Chapter 32 The Child with a Communicable Disease Objectives
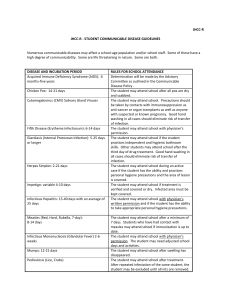
advertisement
• • • • • • • • • • • • • • • • • • • Chapter 32 The Child with a Communicable Disease Objectives Define each key term listed. Interpret the detection and prevention of common childhood communicable diseases. Discuss the characteristics of common childhood communicable diseases. Discuss three principles involved in standard precautions used to prevent the transmission of communicable diseases in children. Objectives (cont.) Discuss national and international immunization programs. Describe the nurse’s role in the immunization of children. Demonstrate a teaching plan for preventing sexually transmitted infections (STIs) in an adolescent. Formulate a nursing care plan for a child with acquired immunodeficiency syndrome (AIDS). Communicable Disease Prevention and control are the key factors in managing infectious disease HIV, hepatitis, TB, and STIs are infections continue to occur worldwide The incidence of common childhood communicable disease has decreased with the use of appropriate immunizations The nurse must know and be alert to signs and symptoms of communicable disease because air travel enables rapid transmission around the world Review of Terms Communicable disease—can be transmitted from one person to another • • • • • • • • • • • • • Incubation period—time between exposure to pathogen and onset of clinical symptoms Prodromal period—time between earliest symptom and appearance of typical rash or fever Vector—an insect or animal that carries and spreads disease Review of Terms (cont.) Pandemic—a worldwide high incidence of a communicable disease; i.e., H1N1 influenza Epidemic—sudden increase of disease in localized area Endemic—an expected continuous incidence of disease in a localized area Opportunistic infection—caused by organism normally present in the environment that the immune-suppressed person cannot fight Health care–associated infection—an infection acquired after admission to a health care facility Virulence of Infection Host resistance to disease is influenced by – – – – – – – – Age Sex Genetic makeup Nutritional status Physical/emotional health Phagocytes in blood to attack/destroy pathogens Intact skin and mucous membranes Functioning immune system Types of Immunity Natural—resistance is inborn • • • • • • • • • • • • • • • • Acquired—not born with it; as a result of having disease or receiving vaccines or immune serum Active immunity—when a person produces his or her own immunity Passive immunity—provides the antibody to the person; does not last as long Transmission of Infection Direct—transmitted by contact with an infected person Indirect—transmitted by contact with objects that have been contaminated by an infected person (fomites) Medical Asepsis, Standard and Transmission-Based Precautions Preventing the Spread of Infection Aseptic technique—used with all patients Standard precautions—involve hand hygiene and the use of appropriate personal protective equipment (PPE) based on the tasks to be performed or known infectious disease status of the patient Transmission-based precautions—designed according to the method of spread of a specific organism Airborne Infection Isolation Precautions Airborne particles <5 microns in size float in the air and contaminate anything within the room – – Particles can remain airborne for several hours Used for conditions such as TB and varicella Use of negative pressure room and an N95 particulate respirator mask is required whenever in the room with the patient N95 mask is removed only upon exiting the room and hand hygiene is performed Contact Precautions • • • • • • • • • • • When contamination is likely to occur skin to skin or through contact with a contaminated fomite – Private room or cohorting of patients with same type of infection is recommended Fluid-resistant cover gown and disposable gloves should be donned prior to entering the patient’s room and removed upon leaving Hand hygiene is required Droplet Precautions Droplets (>5 microns in size) from coughing or sneezing can contaminate surrounding environment up to 3 feet around the patient – • Droplets do not stay suspended in the air, they immediately “fall” Use of a regular mask is required. A cover gown and gloves may also be required such as when caring for a child with RSV PPE is removed upon exiting the room and hand hygiene is performed Expanded Precautions (Protective Isolation) Used for patients who are not communicable but have high susceptibility to infection, such as a neutropenic patient or bone marrow transplant recipient Strict adherence to standard/transmission-based precautions are required at all times, this includes any visitors – • Used in conditions such as RSV, MRSA, VRE, or Clostridium difficile infections NOTE: If a disease has more than one mode of transmission, then more than one precaution technique is used Hand Hygiene Nurse performs hand hygiene between patients and after removal of gloves – – – Only hospital-approved antibacterial soaps, lotions, and sanitizers are to be used Self-contained liquid soap dispensers, no bar soap Alcohol-based hand sanitizers • • • • Artificial nails, tips, wraps, and nail jewelry are not to be worn as they increase the risk of infection Caregivers with lesions on exposed body parts should not give patient care until all lesions have healed Safety Alert Alcohol-based hand sanitizers should not be used when caring for a patient diagnosed with Clostridium difficile diarrhea – • • • • • • Alcohol cannot penetrate the exterior wall of the spore-forming organism, therefore it cannot kill it Soap and warm, running water should be used after every contact with this type of patient – Running water helps rinse the spore-forming organism off of the hands Family Education to Prevent the Spread of Infection Should include – – – – – – – – Hand hygiene Necessity of immunizations Proper food storage Use of pasteurized milk Proper defrosting/cooking of meat Avoid using community towels Control of insects Avoid use of sandboxes in the yard Rashes of the Skin Erythema—diffuse and reddened Macule—circular reddened area • • • • • • • Papule—circular reddened area that is elevated Vesicle—circular reddened area that is elevated and contains fluid Pustule—circular reddened area that is elevated and contains pus Scab—dried pustule that is covered with a crust Pathognomonic—term used to describe a lesion or symptom that is characteristic of a specific illness (i.e., Koplik spots are seen in measles) Worldwide Immunization Programs Healthy People 2020 – The USPHS goal for 2020 is to have 95% of all children in the U.S. immunized against childhood communicable diseases • • • • • • • • • • • Increase education Accessibility to health clinics Reduce the cost of immunizations Follow-up and track immunizations CDC provides advice concerning vaccinations needed when traveling (www.cdc.gov) Types of Immunization Agents Vaccines Multiple doses at predetermined intervals may be needed to achieve an immunity Used to prevent disease, cannot be used to treat disease Route of administration – Important to achieve immunization Proper storage and handling will ensure potency – – Do not store in refrigerator door Store in center of shelves, away from vents • • • • • • • • • • • • • • • • • – Store at 35-46° F (1.6° to 7.7° C) Nursing Tip The earliest age a vaccine should be administered is the youngest age at which the infant’s body can respond by developing antibodies to that illness Allergies and Toxicities Epinephrine should be available in unit where immunizations are given Child should be observed for 20 minutes after immunization Do not administer the following vaccines if patient is allergic to – – – Baker’s yeast: avoid recombinant hepatitis B vaccine Eggs: avoid influenza vaccine, MMR Neomycin: avoid IPV, MMR, and varicella vaccine Allergies and Toxicities (cont.) Varicella must be given same day as MMR or no less than one month later A tuberculin skin test should not be given within 6 weeks of MMR or varicella Thimerosal: a mercury-containing preservative in some vaccines can cause toxicity Some vaccines can be given on the same day but must be in different syringes and administered in different sites Serious adverse events must be reported to the national VAERS Contraindications to Immunizations Immunocompromised state Pregnancy (with certain vaccines) Bacteremia or meningitis Immunocompromised caregiver in the home • • • • • • • • • • • • • • • • • – Requires individual evaluation by the health care provider Corticosteroid therapy – Requires individual evaluation History of high fever or other reaction after previous immunization Nursing Tip An interrupted vaccination series can usually continue without restarting the entire series The Future of Immunotherapy Refining and combining vaccines continues Transcutaneous immunization through intact skin Recombinant DNA technology is developing vaccines for use with rheumatic fever and malaria Development of RNA and DNA viruses to be used as vectors (carriers) of antigens The Future of Immunotherapy (cont.) Development of “gene gun” to blast vaccine through intact skin Development of immunotherapy for non-communicable diseases such as mucosal administration of myelin for multiple sclerosis Development of tumor antigens Bioterrorism and the Pediatric Patient Children are more vulnerable as immune system is not fully developed Children are closer to the ground so heavy particles from aerosol-propelled agent reaches them in higher doses than adults Safety of new drugs developed may not yet be available for children • • • • • • • • • • • • • • • • • • Bioterrorism and the Pediatric Patient (cont.) Routine “HazMat” decontamination procedure may not be suitable for pediatric patient who is prone to hypothermia (due to large head and body surface area; low fat content of body) A small blood volume makes child more susceptible to fluid losses from GI toxins Gas masks may not be available in children’s sizes TV coverage of terrorist attacks can affect child’s feeling of safety in the home and can alter behavior Triage Categories Common Diseases Spread Through Bioterrorism Emergency Preparedness Family should keep several days supply of food, water, pet food, warm clothing, blankets, medicines, copies of vital documents and toiletries Battery-powered radio, basic first aid supplies Hold disaster drills in the home Have out of state family contact numbers to call in case the family is separated Children should be taught to keep personal ID with them and how to call for help when needed Initial Observations During Disasters Assess the “ABCs” and mental status Heightened awareness by health care personnel plays critical role in facilitating early recognition of bioterror attack Work with emergency department, Infection Control staff, and the local public health department to help coordinate actions that are needed NOTE: It is imperative to follow your chain of reporting at your facility • • • • • • • • • • • • • • • • • • • • • The Pediatric Patient in a Disaster Setting Has a proportionately larger body surface area, thinner skin May have increased pulmonary problems compared to the adult Children are closer to the ground and may be exposed to more toxins Immature blood-brain barrier and increased CNS receptor sensitivity increases their sensitivity to nerve agents Use of Broselow-Luten color-coded, water-resistant tapes for drug calculations decreases risk of medication errors Can also use the Pediatric Antidotes for Chemical Warfare for dosage calculations Sexually Transmitted Infections Infections spread through sexual activity Can be spread from pregnant mother to fetus Can be spread through sexual abuse of child Can be spread by use of contaminated needles or exposure to blood Nurse required to report STIs to the local Public Health Department Contacts of infected person will also need to be tested Nursing Care and Responsibilities Create environment where patient feels safe and at ease Listen, be nonjudgmental, and provide emotional support Provide privacy during examinations Encourage questions Assure confidentiality Assess level of knowledge and understanding • • • • • • • • • • • • Help patient formulate positive self-attitude Nursing Tip Sex education is not limited to mechanics of intercourse, but rather includes the feelings involved in sexual experience, expectations, fantasies, fulfillments, and disappointments HIV/AIDS in Children Children usually contract HIV by – – – Contact with infected mother at birth Sexual contact with infected person Contact with infected needles or blood Cause of HIV/AIDS in Children HIV-1 attacks lymphocytes and causes imbalance in helper T-cells (CD4+) that support immune system and suppressor T-cells that shut it down Diagnosis of HIV/AIDS in Children CD4+ cell count is measure of damage to the immune system caused by HIV and guides treatment options ELISA test and Western Blot test to diagnose HIV are not reliable in children under 15 months of age HIV/AIDS in Children (cont.) Manifestations – – – – Failure to thrive Lymphadenopathy Chronic sinusitis Failure to respond to treatment of infections • • • • • • • • • • • • • • Thrush Pneumocystis jiroveci (formerly, carinii) pneumonia Herpes infection Cytomegalovirus (CMV) HIV/AIDS in Children (cont.) Treatment – – – – – – – Supportive No cure available for HIV/AIDS Education regarding drug therapy compliance Support growth and development of the child Psychological support of child and family Referral to available resources within the community Update routine immunizations Question for Review What type of immunity is given to infants and children through routine vaccinations for common childhood communicable disease? Review Objectives Key Terms Key Points Online Resources Review Questions