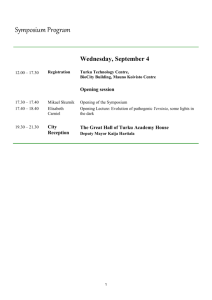
Yersinia pseudotuberculosis outbreak: Summary of ESR case
advertisement

Yersinia pseudotuberculosis Yersinia pseudotuberculosis Outbreak: Summary of ESR case control studies The ESR studies identify foods eaten more often by people who became ill than by people who didn’t become ill. The ESR studies do not identify any affected or contaminated food nor its source. The ESR studies say the information is not definitive, but provides direction for further investigation. MPI investigations to identify an affected or contaminated food are ongoing. The Ministry of Health (MoH) and Ministry for Primary Industries (MPI) became aware on 23 and 24 September 2014, respectively, of an outbreak of enteric illness (gastroenteritis) caused by Yersinia pseudotuberculosis. These bacteria cause a notifiable disease, which is uncommon in New Zealand with just 13 cases notified during 2013. Outbreak investigations employ several procedures to identify directions for inquiry and ultimately the cause. These include: Routine evaluation of information collected from persons with a notifiable disease (cases). Review of literature on the causative organism and its disease. Enhanced questions of cases to narrow the focus for investigation. Additional detailed and targeted surveys of persons with illness. Case-control studies (comparison of information from cases and similar individuals that have not been unwell). Epidemiological and microbiological/toxicological analyses of implicated foods. Initial case information presented by ESR and the Public Health Units (PHU) associated illness with a range of fresh produce with those most frequently recalled as consumed being lettuce, carrots, tomatoes, apples, cold ready-to-eat meats and dairy products. Affected persons had generally purchased these foods from supermarkets or shops. A wide range of other ready-to-eat foods and food settings such as fast food outlets and restaurants were ruled out as the majority of cases had not eaten those foods raw, or visited those establishments. While MOH and MPI considered the identified foods to be possible sources of infection, it was noted that they were foods commonly consumed by the general population. Because the possible food sources were commonly eaten, an ESR case-control study was commissioned to provide additional clarification of possible avenues for further investigation. The initial report of the case-control study (dated 6 October 2014) identified that cases were more likely to have purchased or eaten raw lettuce, lettuce from a supermarket or shop, Pam’s Fresh Express bagged lettuce, carrots from a supermarket or shop, bagged carrots and Pam’s bagged carrots than those that were not ill. The second report of the case-control study (dated 8 October 2014) again showed that lettuces and carrots were commonly consumed by both cases and controls. However, cases were more likely to have eaten the identified foods than controls. The report listed several lettuce and carrot sources that were more likely to be associated with illness. These were then ranked “in descending order of magnitude of association”. ESR noted that the associations in the report were large and statistically significant. However, they also stated in the report that this information is not definitive and should lead to further investigations. MPI and MOH considered the evidence supporting the associations between human cases and specific food products, and their ranking, to have a level of uncertainty. While the findings did give a clear steer for further investigation, in themselves they were insufficient to clearly identify specific products that were contaminated. Therefore, investigations into the following areas have commenced and are ongoing. Any common growing, processing and consumption of lettuce and carrots. The level of exposure of possible food sources. Possible contamination of different sub-categories of lettuce and carrots. Supply or processing in supermarkets. Reports Institute of Environmental Science and Research Results of Case-Control Studies into Yersinia pseudotuberculosis outbreak – 6 October 2014 (PDF, 2.4 MB) Institute of Environmental Science and Research Results of Case-Control Studies into Yersinia pseudotuberculosis outbreak – Second interim report as at 8 October 2014 (PDF, 4.2 MB) MPI investigating source of Yersinia pseudotuberculosis Ministry for Primary Industries (MPI) has been notified by Environmental Science and Research of a cluster of human illnesses linked to the bacteria Yersinia pseudotuberculosis. While cases are reported each year, there has been an increase in cases in September 2014. Symptoms Yersinia pseudotuberculosis causes stomach cramps and can present symptoms that mimic appendicitis. Diarrhoea can occur but is rare. It has a 3 to 21 day incubation period. Outbreak source MPI is working to determine the source of the outbreak. We believe there is a credible link that food is the likely source, but it is too early to be certain about the source of this pathogen and direct people away from foods that have no proven risk for consumers. The people who have become ill with Yersenia have been interviewed on what foods they have been eating and this information has been cross-referenced, giving us sources to investigate further. It is important to note that MPI’s investigation is over a range of foods. Person to person spread is uncommon. More information For more information on this illness visit http://www.health.govt.nz/your-health/conditionsand-treatments/diseases-and-illnesses/yersinia-pseudotuberculosis Advice for consumers Yersinia pseudotuberculosis causes stomach cramps and can present symptoms that mimic appendicitis. Diarrhoea can occur but is rare. It has a 3 to 21 day incubation period. Please apply normal food safety practice. If it looks off or smells off, throw it out. Otherwise keep fresh food chilled and wash fruit and vegetables before eating.