Reflection Paper: Ethical and Legal Aspects of Health Care and the
advertisement
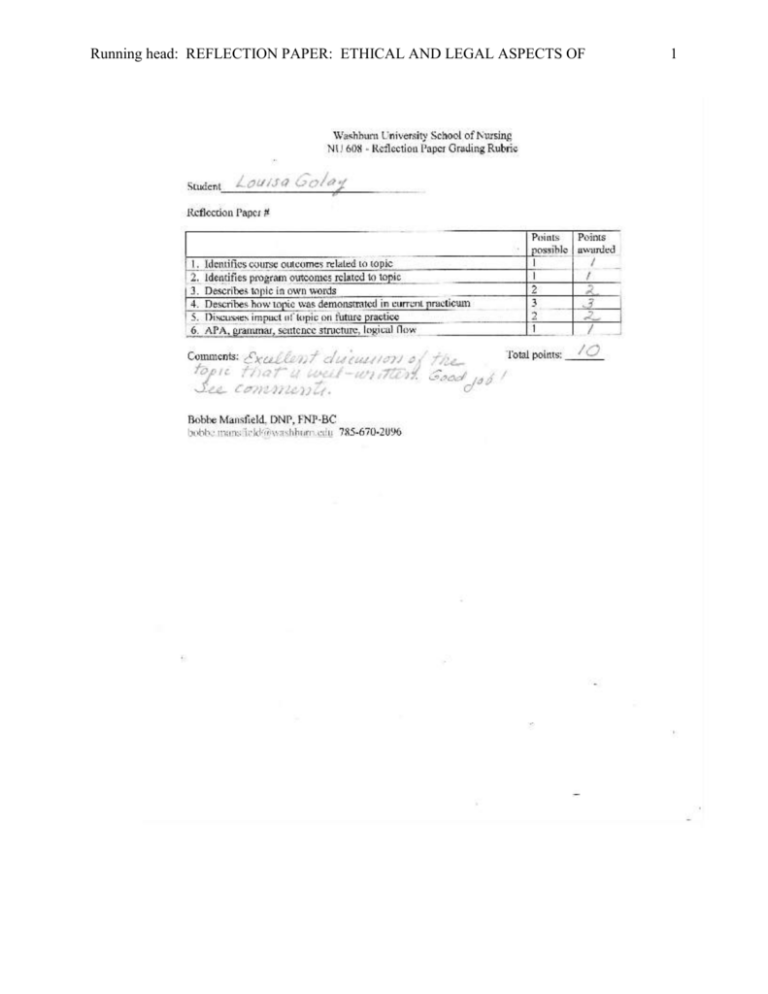
Running head: REFLECTION PAPER: ETHICAL AND LEGAL ASPECTS OF 1 REFLECTION PAPER: ETHICAL AND LEGAL ASPECTS OF Reflection Paper: Ethical and Legal Aspects of Health Care and the Role of the Advanced Practice Nurse LOUISA GOLAY WASHBURN UNIVERSITY NU 608 September 19, 2012 2 REFLECTION PAPER: ETHICAL AND LEGAL ASPECTS OF 3 Reflection Paper: Ethical and Legal Aspects of Health Care and the Role of the Advanced Practice Nurse Ethical and legal aspects of health care present challenges for many providers. When reviewing both the program and course outcomes that pertain to this topic, I felt Program Outcome #6: “Incorporate ethical and legal principles in health care polices” outlined each subject the best. Additionally, I felt as though Course Outcomes, #3: “Exhibit advanced communication skills in interdisciplinary settings” also pertained to the aspects of ethical and legal issues related to the advanced practice nursing role. As the complexity of issues intensifies, the role of the APN (Advanced Practice Nurse) becomes particularly important in the identification, deliberation, and resolution of ethical problems. Clinical reasoning is inextricably linked to ethical reasoning. For example, clinical reasoning generates possibilities of what could be done in a situation, whereas ethical reasoning adds the dimension of what should be done in the situation. The first theme encountered in many ethical dilemmas is the erosion of open and honest communication. Clear communication is an essential prerequisite for informed and responsible decision making. The literature regarding how to resolve ethical issues is extensive. One approach, the incorporation of preventive or prospective ethical considerations into clinical thinking and decision making. This approach places an emphasis on preventing ethical conflicts from developing rather than waiting until a conflict arises; it does so by shaping the process of clinical care so that potential valued conflicts are anticipated and discussed before outright conflict occurs (Hamric, 2009). In the clinic setting, disagreements between a patient and their family member, friend, significant other, etc. can be rooted in faulty communication, which can then lead to ethical conflict. REFLECTION PAPER: ETHICAL AND LEGAL ASPECTS OF 4 Additionally, the skill of listening is just as crucial in effective communication because listening well allows others the necessary time to form and present their thoughts and ideas. In my current specialty practicum, I have encountered several “disagreements” between patients and their family members. Whether it is arguing over the last time they took their medication or what their diet regimen consists of, family members tend to argue with their loved ones! Regardless of the disagreement, I try to effectively listen and engage in the conversation by redirecting and simply saying “if you aren’t sure when you last took your medication, either yesterday or today, I can note in your chart that you are still taking the medication; however unsure if taking the medication as prescribed due to the fact a few doses may have been missed. Does this sound okay to you?” Typically re-directing the conversation, but still involving the patient in the overall statement, calms the mood and we can then continue through the assessment and reason for their visit in a timely manner all while providing clear, concise and adequate documentation. As illustrated in the approve scenario, the preventative approach has the potential to avoid conflicts as APNs integrate ethical reasoning into clinical reasoning at an earlier point in time. As illustrated in the literature, I feel this example accurately reflects one of my ability’s to prevent ethical dilemmas from occurring. In addition to emphasizing early communication between the patient and provider in hopes to prevent ethical dilemmas from occurring, it is equally important for APNs to create and preserve trust and understanding with their patients (and families, significant other, etc.). One example of clear communication includes the “teach-back” method that ensures a patient truly comprehends what the APN has said. In this method, you ask the patient to “teach” you the information. In my specialty practicum setting, I have used the teach-back method REFLECTION PAPER: ETHICAL AND LEGAL ASPECTS OF 5 several times especially when prescribing medications. When prescribing antibiotics for example, I simply say: “I want to be sure that I explained your medication correctly. Can you tell me how you are going to take this medicine and when to call me if further complications or change in symptoms arise?” By developing trust and promoting open communication, APNs can address health literacy, prevent ethical dilemmas from occurring, and build relationships with their patients in an attempt to create the best possible outcomes (NSO, 2012). Upon graduation and becoming an APN, I plan to utilize both the preventative approaches mentioned above in hopes to avoid ethical dilemmas from occurring. I believe that placing an emphasis on preventing ethical conflicts from developing, rather than waiting until one arises, is the best answer. As evidenced in the two scenarios above, potential patient harm and/or a malpractice lawsuit could have been an outcome from either case if the preventative approach was not employed initially. When addressing the legal aspects of the advance nurse practitioner role, the most pressing issues that come to mind are those involving the legal aspects of licensing and credentialing. APNs have been practicing in various capacities for years; however, a consensus on the components involved in the regulation of APNs has been argued for some time. Disagreements on uniform state regulations are limiting the accessibility of the high quality, cost-effective care APNs can provide. Much of the debate involved in defining the APN profession has involved credentialing, education, scope of practice, and the actual title of APNs (Hamric, 2009). At no time has it been more important for APNs to understand and value the important relationships among groups that control the complex processes and systems that regulate practice. New models of health care and varying configurations of how APNs practice in interdisciplinary teams escalate the importance of regulatory considerations. REFLECTION PAPER: ETHICAL AND LEGAL ASPECTS OF 6 Currently, there is a lack of uniformity across states in defining the APRN role, including advanced practice education, licensing, and credentialing requirements. Credentialing can be defined as the requirements that a state uses to assess minimum standards of competency for APNs to be authorized to practice in an APN role. The purpose of credentialing is to protect the health and safety of the public, whereas certification provides validation of the APN’s knowledge in a particular specialty. Certification is used by most states as one component of second licensure for APN practice. In my future practice as an APN, I plan to obtain Kansas licensure and maintain credentialing through the American Academy of Nurse Practitioners. In 2007, the Alliance APRN Consensus Work Group met with the APRN Advisory Committee to produce complementary recommendations that would together guide future regulation, thus giving rise to the Consensus Model for APRN Regulation: Licensure, Accreditation, Certification & Education (LACE). The LACE Consensus Model recognizes four APRN roles: certified registered nurse anesthetist (CRNA), clinical nurse specialist (CNS), certified nurse-midwife (CNM), and certified nurse practitioner (CNP) (Hamric, 2009). The model also states that all APNs will be educated in one of these four roles, in addition to at least one of six population foci: family, adult-gerontology, pediatrics, neonatal, women’s health, or mental health (Stanley, 2009). The proposed APRN Regulatory Model outlines an understandable framework for making decisions in regards to advanced practice nursing and LACE issues. From an ethical standpoint, it is imperative for the public to trust that any APN providing care is educated, certified, and licensed within his/her scope of practice. This will ensure patients that they are receiving safe and equitable care from providers with the title of APN. REFLECTION PAPER: ETHICAL AND LEGAL ASPECTS OF 7 Creating and implementing a timely consensus for APNs is critical to assure the public about the consistency and quality of their healthcare providers (Hamric, 2009). In conclusion, it is clear that organizations are engaged in a more active dialogue about the nature of advanced practice and have begun a concerted effort to address LACE issues. Although the nature of advanced practice nursing is amplified and clarified by the role-specific documents published by these organizations, the level of conceptualization is more complex than is usually associated with conceptual models. This complexity illustrates the breadth and depth of advanced, specialized practice in the four APN roles and may be one reason why it has been difficult to identify a unified and coherent view of advanced practice nursing (Stanley, 2009). Essentially, APNs have dual legal liability including nurse adherence to the state nurse practice act and the APN’s requirement to national specialty certification and/or secondary licensure requirement. If APNs continue to expand practice roles, there will likely be an increase in the APNs level of accountability and liability. REFLECTION PAPER: ETHICAL AND LEGAL ASPECTS OF References Hamric, A. (2009). Advanced Practice Nursing An Integrative Approach (4th ed.). St. Louis, MO: Saunders Elsevier. Nurses Service Organization. (2012). Improving health literacy improves patient outcomes. Retrieved from http://www.nso.com/newsletter12 Stanley, J. (2009). Reaching consensus on a regulatory model: what does this mean for APRNs?. The Journal for Nurse Practitioners, 99-104. 8