Lecture 18
advertisement

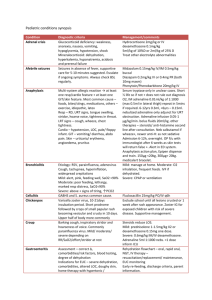
Infections of Skin and Wounds Abscesses Abscess - a localized collection of pus Abscess formation localizes an infection and prevents spread Microorganisms in abscesses are difficult to treat with antimicrobial agents because: 1.microbes aren’t multiplying - many antimicrobial agents only work against actively growing cells. 2.chemical nature of pus interferes with action of some antibiotics 3.antibiotics have difficulty reaching the site because of lack of vessel penetration Abscesses are a potential source of infection for other sites, can seed microbes into the blood or lymph I. Bacterial Infections of Skin, Soft Tissue, Muscle All acute (24-48h) A. By skin layer involved 1. infections of hair follicles – usually S. aureus a. folliculitis - involves only the hair follicle - small red bump of inflammation b. furuncles = boil – intense inflammation spreads to surrounding tissue – abscess w/localized redness, swelling, tenderness, pain, pus - 1.5 mil/yr - S. aureus food poisoning c. carbuncles - larger - several sites of draining pus - usually on neck or upper back - systemic symptoms (fever) 2. Stratum corneum Impetigo - a highly contagious pyoderma caused by group A -streptococci (GAS)- almost exclusively in children - spread by contact 3. Epidermis Ecthyma – untreated impetigo 4. Dermis a. Erysipelas = St. Anthony’s fire – usually GAS - blockage of dermal lymphatics – welldefined edges. Pain and fever. 5% develop bacteremia with high mortality. b. Lymphangitis – inflammation of the lining of lymphatic vessels 5. Subcutaneous fat layer Cellulitis – usually S. aureus or S. pyogenes. Initial superficial skin trauma. inflammation, enlarged lymph, malaise, chills, fever. Diffuse 2 B. By specific strains of S. aureus or S. pyogenes 1. Scalded skin syndrome Caused by certain exotoxin producing strains of S. aureus infected by lysogenic phages Exotoxin is exfoliatin - carried in bloodstream to the epidermis where it causes a split in deep layers - 40% of outer layers of skin are lost - loss of body fluid, high fever, bacteremia. Rapid txt is necessary to prevent death. Txt with antibiotics - remove dead skin and tissue Most common in children under 2, esp. newborns. Also assoc. with w/late stages of STSS (60% mortality) 2. Necrotizing fasciitis - "flesh-eating strep" – GAS infected by phage - infection is secondary to minor ski trauma Involves the subdermal tissues produces 2 toxins: 1. Pyrogenic toxin A - a superantigen, stimulates excessive IL-2 production 2. Exotoxin B - destroys tissues by breaking down protein, rate of 1 inch/hr. Similar clinical picture induced by Methacillin Resistant Staphylococcus aureus (MRSA) II Viral diseases resulting in skin rashes = exanthems Several childhood diseases are characterized by distinctive skin rashes caused by viruses that are carried to the skin by the blood from sites of infection in the upper respiratory tract. All spread by inhalation of respiratory droplets. 1 - Rubeola virus – measles (61 reports in 2009) High fever and rash that starts head & neck, then arms, upper trunk, back, finally legs Koplik's spots are diagnostic Extremely contagious – 90% Rash is caused by the reaction of Tc cells with virus-infected cells in the small vessels of the skin. More than 15% of children infected with measles die of measles complications pneumonia, encephalitis - major ww killer In U.S. in children less than 15 months because of vaccination program (2 – Scarlet fever – phage infected S. pyogenes – produces an erythrogenic toxin that is distributed systemically scarlet fever rash) 3 3 - Rubella virus - German measles = 3 day measles - one of the mildest of the viral diseases that cause rashes (4 reports in 2009, 1 congenital) Low grade fever, eye pain - rash first on face then spreads downward Seriousness - maternal infection in 1st trimester serious fetal damage 4 – Scarlatina - ?? 5 - Fifth Disease = Erythema infectiosum - Parvovirus B19 6 - Sixth Disease = Roseola infantum - Human Herpesvirus 6 (HHV-6) Others un-numbered Varicella-Zoster - chickenpox and shingles (16,944 U.S. / 1,857 MI) Chickenpox - highly contagious Spread by coughing, sneezing, direct contact, aerosolization Highest incidence in March and April Generally mild in 5-9 year olds, 1in 10 experience complications Fatal in infants, adolescents, adults, immunocompromised of any age (10-30% mortality) due to __________________________________________ Deaths every year in unvaccinated individuals Dorsal root ganglion near spine - Shingles, reactivation, over 45. Kawasaki Disease III. Fungal Skin Diseases - Read in your text 4 IV. Infections of Wounds A. Infections of Trauma Induced Wounds Many type wounds result in anaerobic conditions in the tissues: 1. Dirty 2. Crushed 3. Puncture wounds (including little puncture wounds from nails, tacks, thorns, splinters) 4. Projectile (bullets, fireworks) - battlefields, especially cavalry - tetanus EX. Gas gangrene - Clostridium perfringens and C. septicum - many trauma wounds Onset 12-48 hrs after injury - tissues become anoxic spores germinate bacteria grow & ferment carbohydrates of muscles prod gases (carbon dioxide & hydrogen), gas bubbles destroy tissue. Foul odor, high fever, shock, massive tissue destruction, blackening of the skin, rapidly spreading Txt - Debridement, amputation, hyperbaric chamber - pressurized oxygen-rich atmosphere - oxygen saturates the infected tissue, prevents growth of clostridia. EX. Pasteurella multocida - GNR, ox +, grows on MAC. - animal bite wounds B. Infections of Surgical Wounds 5-12% of all surgical patients develop post-operative infections. Role of sutures - usually 10,000 S. aureus needed to establish infection but sutures down to 100. Also IV catheters, artificial valves & joints. The pathogens: S. aureus - highest single agent, about 20% all surgical wounds BUT Infections caused by coagulase (-) staphylococci, Enterobacteriaceae, and Pseudomonas together cause 60% of surgical wound infections. They are less invasive than S. aureus but more antibiotic resistant. C. Infections of Burn Damaged Skin Burned areas with damaged skin are ideal sites for infection by bacteria from the environment or normal flora. Almost any opportunistic pathogen can infect wounds but the most serious is Pseudomonas aeruginosa - very antibiotic resistant - major cause of death in burn patients. GNR, oxidase +, characteristic blue-green pigment called pyocyanin- can color tissues green as well. 5 Staphylococcus aureus virulence factors Factor 1. Leukocidin 2. Coagulase 3. Exfoliative toxin (exotoxin) 4. Toxic Shock Syndrome toxin (exotoxin) 5. Protein A secreted 6. Capsule 7. Lipase 8. Protease 9. Hyaluronidase 10. Penicillinase Effect Kills WBC by producing holes in their cytoplasmic membranes (also kill RBC). May impede the progress of WBC into the infected area by causing plasma to clot in the surrounding capillaries. Also disguises staph antigens with self material (antigenic mimicry). Separates the layers of epidermis, aids in invasion. Superantigen - stimulates TH to over produce IL-2. Causes rash, diarrhea, falling blood pressure resulting in shock Binds to Fc portion of antibody so antibody can’t bind to Fc receptors on phagocytes (antiopsonic). Inhibits phagocytosis of nonopsonized bacteria. Breaks down lipids, aids in colonization of oily hair follicles. Degrades collagenase, aids in spread. Breaks down hyaluronic acid in connective tissue, aids in spread. Destroys the beta-lactam ring of penicillin. 6 Streptococcus pyogenes virulence factors Factor 1. Hemolysins = streptolysins 2. Streptokinase 3. DNase 4. Hyaluronidase 5. Erythrogenic toxin 6. Proteases 7. Hyaluronic acid capsule 8. M-protein Effect Kill WBC by producing holes in their cytoplasmic membranes (also kill RBC). Converts plasminogen to plasmin, promotes lysis of fibrin clots, aids in spread. Breaks down the viscous DNA in pus to facilitate spread. Breaks down hyaluronic acid (the cement that holds cells together) in connective tissue, allows rapid spread (also eventually breaks down their own capsule). Produced by lysogenic strains (virus infected), responsible for rash. Break down proteins. Same as hyaluronate of connective tissue. Inhibits phagocytosis of nonopsonized bacteria, also disguises strep antigens. Interferes with phagocytosis and blocks complement action. The major virulence factor.