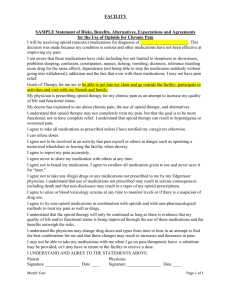
ADVANCED INTERVENTIONAL PAIN CONSULTANTS Follow Up
advertisement
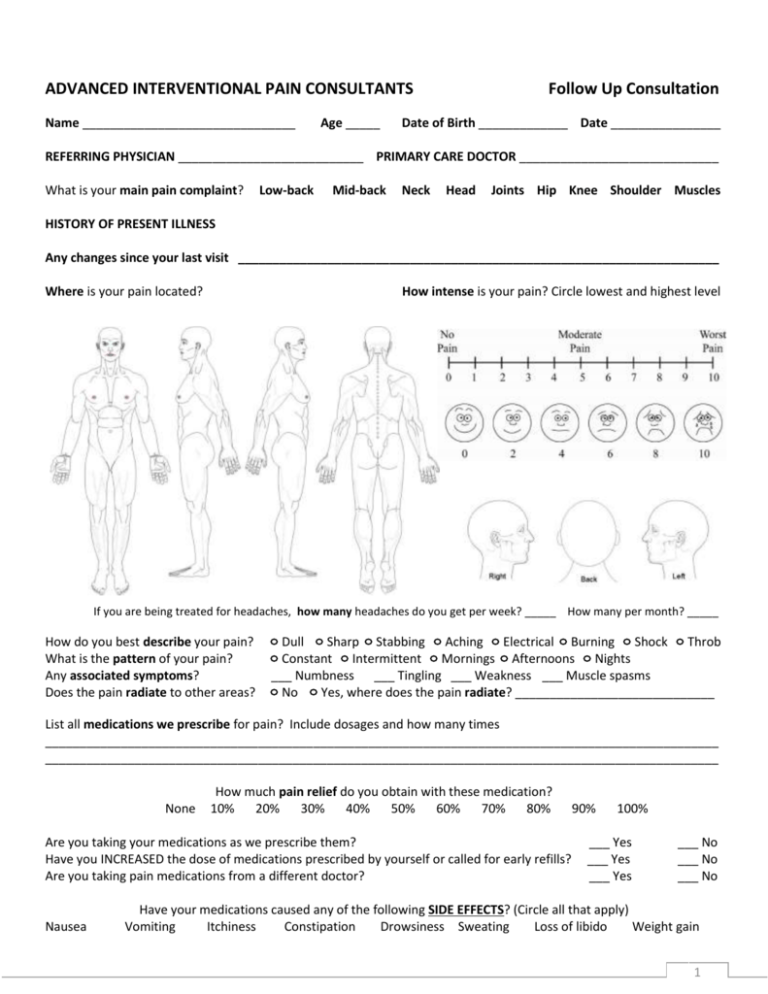
ADVANCED INTERVENTIONAL PAIN CONSULTANTS Name _______________________________ Age _____ Follow Up Consultation Date of Birth _____________ Date ________________ REFERRING PHYSICIAN ___________________________ PRIMARY CARE DOCTOR _____________________________ What is your main pain complaint? Low-back Mid-back Neck Head Joints Hip Knee Shoulder Muscles HISTORY OF PRESENT ILLNESS Any changes since your last visit ______________________________________________________________________ Where is your pain located? How intense is your pain? Circle lowest and highest level If you are being treated for headaches, how many headaches do you get per week? _____ How many per month? _____ How do you best describe your pain? What is the pattern of your pain? Any associated symptoms? Does the pain radiate to other areas? Dull Sharp Stabbing Aching Electrical Burning Shock Throb Constant Intermittent Mornings Afternoons Nights ___ Numbness ___ Tingling ___ Weakness ___ Muscle spasms No Yes, where does the pain radiate? _____________________________ List all medications we prescribe for pain? Include dosages and how many times __________________________________________________________________________________________________ __________________________________________________________________________________________________ None How much pain relief do you obtain with these medication? 10% 20% 30% 40% 50% 60% 70% 80% Are you taking your medications as we prescribe them? Have you INCREASED the dose of medications prescribed by yourself or called for early refills? Are you taking pain medications from a different doctor? Nausea 90% 100% ___ Yes ___ Yes ___ Yes ___ No ___ No ___ No Have your medications caused any of the following SIDE EFFECTS? (Circle all that apply) Vomiting Itchiness Constipation Drowsiness Sweating Loss of libido Weight gain 1 Since your last visit, have you had a pain injection? ___ Yes ___ No If yes, how much pain relief did you obtain with the injection? None 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% Has your treatment improved any of the following aspects of your life? Activities of daily living Ability to work Family life ___ Yes ___ Yes ___ Yes ___ No ___ No ___ No Relations with people Sleeping /rest Depression/anxiety Overall, has the treatment you are receiving made a positive change in your condition? ___ Yes ___ Yes ___ Yes ___ No ___ No ___ No ___ Yes ___ No Opioid Attestation I attest and certify that all of the following statements are true and factual: ___ I have used all medications prescribed to me exactly as prescribed. ___ I have reported all side effects to my physician. ___ I have not sold, given to someone else, or otherwise transferred my medications to anyone. ___ I have safeguarded my medications from theft. ___ I have not received, accepted, taken, or otherwise used any other opioid medications (narcotics) from any other source, including from other physicians. ___ I have not received, accepted, taken, or otherwise used any illegal drugs. ___ I have not used alcohol while taking my opioid medications (narcotics). ___ All of the answers provided on this form are true and factual. Patient‘s Signature _________________________________ List all your drug allergies _______________________________ List all other MEDICATIONS FOR PAIN you currently taking. Include PAIN CREAMS. Include dose and times per day taken 1) 2) 3) 4) 5) ______________________________________________ ______________________________________________ ______________________________________________ ______________________________________________ ______________________________________________ ___ Digabatran (Vigabatin) Do you take any of the following blood thinners? ___ Plavix ___ Alteplase (Aclilyse) ___ Coumadin ___ Ticlopidine (Ticlid) ___ Lovenox ___ Apixoban (Elquis) ___ Heparin ___ Aspirin ___ Rivaroxaban (Xarelt ___ Edoxaban (Lixiana) Are you currently enrolled in PHYSICAL THERAPY? ___ No ___ Yes If yes, when will you complete it _______________ PAST MEDICAL HISTORY Has your medical history changed since your last visit? ___ No ___ Yes, explain __________________________________________________________________________________________________ __________________________________________________________________________________________________ PAST SURGICAL HISTORY Since your last visit, have you had any new surgery(ies)? ___ No ___ Yes If yes, write the type of surgery(ies) _____________________________________________________________________ __________________________________________________________________________________________________ 2 REVIEW OF SYSTEMS Circle all that apply 1. General 2. Eyes/ Ears/Nose/Throat Weight gain or loss, unexplained hair loss, fever or chills, low energy, too sleepy Eye pain, vision problems (blurred vision, loss of vision), hearing loss, swollen glands in neck, sore throat/pain when swallowing, dental problems Chest pain (sharp, crushing, or heaviness), heart racing (palpitations), fainting spells, shortness of breath, swelling of legs (edema) Shortness of breath, cough/coughing up blood Increased appetite, decreased appetite, stomach pain, nausea/vomiting, diarrhea, constipation Pain when passing water (urination), blood in urine, urinating more than usual (day and/or night), bladder Infection, pain during sex, changes in sex drive (libido) Limited motion of arms or leg, joint pain, swelling/redness, numbness, tingling, or weakness in arms or legs Arm/leg weakness, new headaches, problems with memory or speech, tremors Sadness, stress, seeing or hearing things, suicidal thoughts, feeling down, insomnia, anxiety Weight gain/loss, thirsty all the time, cannot stand temperature changes (heat/cold) Swollen glands (armpits or groin) Rash (palm of hands, sole of feet), changes in skin, sores or rash on skin Hives/skin rashes, allergic reaction to foods 3. Cardiovascular 4. Respiratory 5. Gastrointestinal 6. Genitourinary 7. Musculoskeletal 8. Neurological 9. Psychiatric 10. Endocrine 11. Lymph 12. Skin 13. Allergies ____ No new problems I attest that information I have provided is accurate and factual, and I can provide supporting information to its veracity. Patient‘s Signature __________________________________ Date _____________________ DOCTOR’S NOTES MRI: _ Reviewed XRAY: ___Reviewed CT SCAN: ___Reviewed EMG: ___ Reviewed SOAAP-R Score: ____ PMQ-R Score: ____ DEPRESSION Score: ____ Medical Records: ___ Reviewed ___ Not Available DPS REPORT: ___ Reviewed Inclinometry and muscle strength test: ___ Done today ___ Reviewed UDS REPORT: ___ Reviewed 3