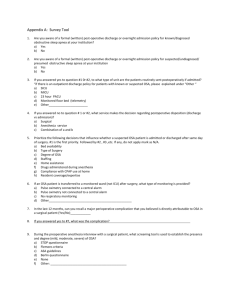
ONLINE APPENDIX Methods Long-term OSA-model Twelve
advertisement
1 ONLINE APPENDIX Methods Long-term OSA-model Twelve-week male Sprague-Daley rats were intubated and ventilated with 2%isoflurane/room-air. Volume-controlled ventilation was delivered with tidal volume and respiratory rate of 2.5 ml and 72 cycles/minute, respectively. OSA was mimicked by closing the airway at end-expiration for 40 seconds, followed by 80-second recovery periods, 20 consecutive times/day (Figure 1). After OSA-cycles, rats were ventilated with room air during recovery from anesthesia. They were then extubated after confirming spontaneous respiration. No complications resulted from anesthesia, ventilation and OSA. OSA-cycles were repeated daily, 5 days/week for 4 weeks. Two control groups were studied: 1) openairway rats subjected to the same ventilator-arrest cycles but without airway-closure; 2) sham rats ventilated with isoflurane/room-air throughout the procedure. Animals in all 3 groups were subjected to daily oropharyngeal intubation for ventilation. No animal showed signs of complications of intubation such as stridor or tachypnea. After 4 weeks, in vivo electrophysiological studies and AF-induction assessments were performed, and tissueprocurement was obtained. A 3-Fr pressure-transducer catheter (Scisense P-catheter) was introduced into the esophagus close to the LA posterior-wall to monitor intrathoracic pressure in 6 OSA-rats and 5 open-airway rats. For blood-pressure monitoring, a 2-Fr pressure-transducer catheter (Scisense P catheter-RAT) was introduced into the ascending aorta through the left internal carotid artery. In-vivo electrophysiological study Programmed right-atrial (RA)-stimulation was performed at a cycle length of 150 ms (pulse-width 2 ms, 2×threshold-current) to measure effective refractory periods (ERPs). Atrial and atrioventricular (AV) conducting-system ERPs were defined as the longest S1-S2 coupling interval failing to generate a propagated beat. To assess atrial-tachyarrhythmia inducibility, 25-Hz burst-pacing (pulse-width 2 ms, 4×threshold current) was applied for 3 seconds, with six 3-second burst-cycles separated by 1-second intervals. AF was defined as 2 a rapid (>800 bpm) irregular atrial rhythm, and AF-inducibility was defined as AF lasting for at least 1 sec immediately following the 6-burst cycle protocol. If AF was induced after fewer than 6 burst-pacing cycles, burst-pacing was suspended so as not to interfere with the evolution of the AF. Mean AF-duration was determined in each rat as the average duration of all AF-episodes. If AF was not induced by burst pacing at baseline, the same pacingprotocol was repeated during acute-OSA. Wenckebach cycle length was defined by failure of 1:1 AV conduction, determined by RA-pacing with decremental steps of 5 msec. Sinus-node recovery time was determined by 30-sec RA-pacing with a cycle-length of 150 msec. Echocardiography Transthoracic echocardiographic studies were performed at baseline and after 4-week study with a phased-array 10 S-probe (4.5-11.5 Megaherz) in a Vivid 7 Dimension system (GE-Healthcare Ultrasound, Horten, Norway), under sedation with 2%-isoflurane. M-mode echocardiogram was obtained in parasternal long-axis views to measure LA-diameter (LAD) at end-systole, RV anterior-wall thickness (RVAW) and RV-diameter (RVD) at end-diastole. M-mode images were obtained in parasternal short-axis view at the level of papillary muscles to measure LV-diameter at end-systole (LVDs) and diastole (LVDd), and the thickness of LV anterior-wall (LVAWd) and posterior-wall (LVPWd). LV-mass was calculated using the Reffelmann formula. RA major diameter (RAD) was measured in apical 4chamber view. Pulsed-wave Doppler was used to study transmitral and left pulmonary-vein (PV) flow (TMF, PVF) in apical 4-chamber view. Peak velocity of early-filling E-wave, atrialfilling A-wave in TMF, and systolic (S) and diastolic (D) wave in PVF were measured. The average of 3 consecutive cardiac-cycles was used for each measurement. Similar imagingplanes were used for follow-up studies and LAD-monitoring during acute OSA-testing. The effects of acute OSA on cardiac output (CO) were evaluated by echocardiography. LV end-systolic and end-diastolic volume (LVVs and LVVd) were measured by Simpson’s method in 4 chamber view. LV stroke volume (SV) was calculated by LVVd-LVVs; CO was calculated by multiplying SV by heart rate (HR). Long-term effects of 4-week OSA on SV and CO were calculated by the Doppler method: SV=(DLVOT/2)2xπxTVILVOT), CO=SVxHR; where DLVOT=orifice diameter at the LV outflow tract (LVOT) and TVI=time-velocity integral. 3 Protein-extraction and Western-blot Freshly-isolated LA-samples were snap-frozen in liquid nitrogen and mechanically homogenized in TNE-buffer containing: Tris 25-mmol/L, EDTA 5-mmol/L, EGTA 5-mmol/L, NaCl 150-mmol/L, NaF 20-mmol/L, Na3VO4 0.2-mmol/L, -glycerophosphate 20-mmol/L, AEBSF 0.1-mmol/L, leupeptin 25-µg/mL, aprotinin 10-µg/mL, pepstatin 1-µg/mL, microcystin-LR 1-µmol/L, pH 7.34, HCl. Homogenized samples were centrifuged at 1,000xg for 10 minutes, supernatant collected and ultracentrifuged at 100,000xg for 1 hour. The resulting cytosolic-fraction supernatant was kept for mitogen-activated protein-kinase (MAPK) study. The membrane-fraction pellet was incubated in TNE buffer containing 1% Triton-X100 for connexin-43 analysis. The protein-concentration was determined with Bradford assay (BioRad). All steps were carried out on ice at 4-5°C. Protein-samples (20µg) were separated on 8%-poly-acrylamide SDS-PAGE and transferred electrophoretically onto PVDF-membranes. The PVDF-membranes were blocked in a PBS-solution containing 0.05% (v/v) Tween-20 and 5% (w/v) non-fat dried milk (NDM) and incubated overnight at 4°C with primary antibodies diluted in PBS containing 0.05% Tween-20 and 1%-NDM. After washing with PBS-Tween solution/1%-NDM, membranes were hybridized with HRPconjugated secondary antibody. Immunoreactive bands were detected by electrochemiluminescence using BioMax MS/MR films. Protein-quantification was performed with Quantity-One software (Biorad). All expression-data are relative to GAPDHstaining for the same samples on the same gels. Antibodies Primary antibodies (1/2000) included polyclonal rabbit anti-connexin-43 (AB1727; Millipore), polyclonal rabbit anti-phospho-connexin-43 (ser368) (#3511; Cell Signalling Technologies), monoclonal mouse anti-phospho-p38-MAPK (Thr180/Tyr182) (#9216; Cell Signalling Technologies), monoclonal mouse anti-p38-MAPK (#9217; Cell Signalling Technologies), monoclonal mouse anti-p44/42-MAPK (3A7) (#9107; Cell Signalling Technologies), polyclonal rabbit anti-phospho-p44/p42-MAPK (#9101; Cell Signalling Technologies) and monoclonal anti-GAPDH (10R-G109a) from Fitzgerald. Peroxidaseconjugated AffiniPure donkey anti-rabbit IgG (111-035-152) and Affinipure donkey antimouse IgG (715-035-151) from Jackson ImmunoResearch were used as secondary 4 antibodies (1/10000). Histology Sections (5-μm thickness) were cut at room temperature and stained with Masson’s Trichrome. Stained images were digitized and fibrosis-area analyzed with Image-J 1.45s software. Fibrosis was quantified by a blinded observer and expressed as %cross-sectional area, excluding blood vessels and perivascular tissue. Confocal Imaging Cryosections (14-μm) were fixed with PBS-solution containing 4%-paraformaldehyde (pH 7.34), blocked, and permeabilized with PBS-solution containing 2%-normal donkey serum and 0.5%-Triton X-100. Primary antibodies (mouse anti-Cx43, Chemicon; rabbit anti-Cx40, Zymed) were diluted 1/200 in PBS-solution containing 2% normal donkey serum and 0.1% Triton X-100 for overnight incubation with cryosections. Alexa Fluor–conjugated donkey anti-rabbit (488 nm, Invitrogen) or donkey antimouse (555 nm, Invitrogen) were used as secondary antibodies (1/600 dilution). Alexa Fluor-conjugated phalloidin (647 nm) was used as an actin filament marker (1/600 dilution). Slides were imaged in Z-series every 1μm with an Olympus FV-1000 confocal microscope. The 10 middle layers of the z-stack were used to obtain aggregate 2-dimensional images of phalloidin and connexin-43 fluorescence. Connexin-43 lateralization was analyzed as described previously (12). Detailed Optical Mapping Methods The heart was excised and coronary-artery perfused with Krebs solution (mM: 120 NaCl, 4 KCl, 1.2 MgSO4 0.7, 1.2 KH2PO4, 25 NaHCO3, 5.5 glucose, 1.25 CaCl2, 95% O2/5% CO2) at 10 mL/min and 37°C (1). After 30 minutes for stabilization and electrical-mechanical decoupling with blebbistatin (15-µM), the heart was loaded with di-4-ANEPPS (Biotium, CA). A charge coupled device-camera (CardioCCD, Redshirt Imaging) was used to record RA-free wall fluorescence at 2 kHz. Bipolar electrodes were used to pace the superior RA. Optical maps were obtained during 1.5×threshold-current 2-ms stimulation. Data were analyzed with custom-written algorithms. 5 Data Processing for Optical Mapping The recorded data were processed using custom-made optical mapping analysis software written in Matlab (version 7.11, MathWorks). The statistical analysis was done by using IBM SPSS software (version 20). The data were processed as follows: 1) Wavelet filtering was used to smooth the fluorescence intensity signal of each pixel (2). The symlet sym8 wavelet was used to decompose the signal into 3 levels. Coefficients for filtered signal reconstruction were selected using the minimax thresholding method (3). 2) The series of activation maps corresponding to the atrial activations were obtained by detection and timing of the action potential spikes from the filtered signal of all the pixels in the region of interest. The pattern of action potential (AP) propagation was characterized by the final isochronal activation map. A five point Gaussian filter was applied to filter the calculated isochronal activation map. 3) The conduction velocity was calculated from the gradient of the scalar field of the isochronal activation map using the algorithm proposed by Bayly et al. (4) and Barnette et al. (5). Local velocity vectors were composed of horizontal and vertical components corresponding to the magnitude and direction of propagation. The conduction velocity was obtained from the average of magnitudes of the local velocity vectors. Statistical analysis Data are expressed as mean±SEM except for AF-duration, which is expressed as median and interquartile range (25%-75%). The Fisher's exact test was applied to compare AF-inducibility. Multiple-group comparisons were obtained with ANOVA (for details, see Figure and Table legends). Bonferroni-corrected t-tests were applied to evaluate individual mean-differences when ANOVA revealed significant group effects. All data satisfied statistical criteria for normal distribution except for AF-duration, which satisfied normaldistribution criteria after logarithmic transformation. Two-tailed p<0.05 was considered significant. 6 References 1. Nishida K, Qi XY, Wakili R, et al. Mechanisms of atrial tachyarrhythmias associated with coronary artery occlusion in a chronic canine model. Circulation 2011;123:13746. 2. Crowe JA, Gibson NM, Woolfson MS, Somekh MG. Wavelet transform as a potential tool for ECG analysis and compression. J Biomed Eng 1992;14:268-72. 3. Luo G. Wavelet Denoising, Advances in Wavelet Theor and Their Application in Engineering, Physics and Technology. D. D. Baleanu, InTech Open Science, 2012. 4. Bayly PV, KenKnight BH, Rogers JM, Hillsley RE, Ideker RE, Smith WM. Estimation of conduction velocity vector fields from epicardial mapping data. IEEE Trans Biomed Eng 1998;45:563-71. 5. Barnette AR, Bayly PV , Zhang S, Walcott GP, Ideker RE, Smith WM. Estimation of 3-D conduction velocity vector fields from cardiac mapping data. IEEE Trans Biomed Eng 2000;47:1027-35. 7 Table 1. Arterial blood gases during conditioning procedure pH Baseline (n=4) Open (n=4) OSA (n=5) 7.401±0.010 7.405±0.011 7.315±0.025 pCO2 (mmHg) 47±1 49±3 66±5**,## pO2 (mmHg) 102±7 84±14** 26±3***,### Sat O2 (%) 97±1 92±5 36±5***,### Na+ (mEq/L) 139.8±0.5 139.8±0.8 141.4±0.5 K+ (mEq/L) 4.0±0.2 4.0±0.1 4.3±0.2 BE (mEq/L) 4.3±0.2 5.6±0.8 6.1±0.3 HCO3- (mEq/L) 28.8±0.3 30.8±1.1 31.4±1.5 Mean±SEM. **p<0.01, ***p<0.001 vs. Baseline, ## p<0.01, ### p<0.001 vs. Open airway. Baseline measurements were made prior to ventilator arrest. One-way ANOVA/Bonferroni-adjusted t-tests. BE = base excess. 8 Table 2. ECG parameters Baseline 4-week P (msec) PQ (msec) QRS (msec) P (msec) PQ (msec) QRS (msec) Sham 28.1±1.4 52.0±1.3 29.1±1.5 26.0±0.8 50.3±1.6 30.3±1.4 Open 26.4±0.8 46.6±2.5 28.4±1.2 26.1±0.8 47.8±2.3 29.4±0.9 OSA 28.1±1.2 50.9±2.8 27.7±1.3 28.7±1.7 50.9±3.0 27.4±1.0 Mean±SEM. Sham (n=7), Open (n=8), OSA (n=7). Statistical comparison was by two-way ANOVA for repeated measures. There were no significant differences. 9 Table 3. Blood pressure at end study Sham (n=6) Open (n=6) OSA (n=8) Systolic blood pressure (mm Hg) 114±6 108±2 110±2 Diastolic blood pressure (mm Hg) 88±4 82±2 82±2 One-way ANOVA; no significant differences were found.