H. pylori term paper - Sites at Penn State
advertisement

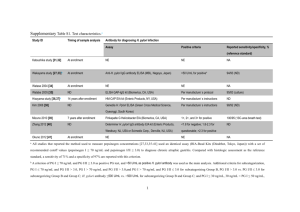
Amy Ketcham Microbiology 201H April 15, 2013 H. pylori and the controversial effect of its cytotoxin-associated gene A Introduction The gram negative bacterium Helicobacter pylori is a prominent member of humans’ microbiota, and the consequences of such a colonization are numerous. One of the adaptations of H. pylori that make this bacterium well-suited for colonization of the stomach is its ability to produce a specific virulence factor, cytotoxin-associated gene A, referred to as cagA (1). This virulence factor originates on the pathogenicity island of H. pylori, which are large genomic regions, present only on pathogenic strains of certain bacteria (6). Pathogenicity islands are reproduced in bacteria by horizontal gene transfer (6). Upon H. pylori attachment on the human epithelial, the CagA virulence factor is released and is the factor directly injected into a host cell’s cell membrane (8). It is there that CagA facilitates interaction with host cell proteins involving growth and cell motility (8). The effect of CagA on the human epithelial is controversial, and many studies suggest CagA is the virulence factor that leads to gastric carcinoma (8). H. pylori is also commonly accepted in the scientific community as the cause of peptic ulcers (4). However, in a time long past, H. pylori was a bacteria present in nearly every adult human, and when present, it is the single most dominant species in the stomach (4). On the other hand, H. pylori is cited as a helpful microbe in preventing gastro-esophageal reflux disease (4). Whatever the effect of H. pylori, its intimacy with its host cells allows an interaction between the host and microbe that may either benefit or harm the host. Whether this microbe causes more harm than good is up for debate. Nevertheless, there has been much discussion in the news recently over one of the effects of H. pylori colonization. This debate centers around the epidemic of Type II Diabetes Mellitus. A few studies suggest that H. pylori exacerbates the glucose homeostasis of the human blood, while a more recent study done by a collaboration of researchers at Virginia Tech and other universities shows that the injection of a strain of H. pylori that carries the cag pathogenicity island (PAI) significantly improves glucose homeostasis (1). The overwhelming evidence in support of H. pylori in regards to regulation of obesity and Type II Diabetes suggests that this microbe may be more beneficial than harmful, but the decreasing prevalence of H. pylori may be another detrimental factor in the ongoing obesity epidemic. H. pylori fighting against obesity This study done by researchers suggests that the growing obesity epidemic coincides with the recent decrease in H. pylori colonization of human epithelial (1). They suggest that the bacterium, with the effects of CagA, may induce “anti-obesity and anti-diabetic actions” (1). The researchers state, “obesity is characterized by insulin-resistance and low-grade chronic inflammation in white adipose tissue with the accumulation of macrophages” (1). Macrophages are responsible for the inflammation, and their involvement leads to insulin resistance (1). However, the results of the study have shown that H. pylori “down-modulates” the resistance by inducing apoptosis of macrophages (1). These actions of H. pylori may suggest an anti-diabetic role that could increase resistance to dangerous blood glucose levels. Additionally, H. pylori assists in weight control and has anti-obese effects (1). The bacterium interacts with many gastric neuroendocrine secreting cells that regulate appetite and weight gain (1). For example, H. pylori interacts with cells secreting ghrelin, a hormone that helps regulate energy homeostasis (1). The microbe maintains the ghrelin production to a decreased level, so that energy homeostasis may be better maintained (1). Another study found that complete eradication of H. pylori led to an increase in body mass index in adult males, and they hypothesized that presence of H. pylori leads to a decrease in leptin and ghrelin levels in circulation (11). The researchers gave possible explanations for the correlation between H. pylori colonization and ghrelin levels, suggesting that H. pylori may modulate gastric cytokine function. The study also provides another explanation: H. pylori may affect the balance of leptin and ghrelin release into circulation (11). However, there have not been many studies in response done to lead to an accepted explanation for H. pylori’s effect on ghrelin and leptin release. The study done by Virginia Tech went on further to comment on the restraints of H. pylori in its role of ameliorating obesity and insulin-resistance in diet-induced obese mice. The mice in the study that had a loss of their Peroxisome proliferator-activated receptor gamma (PPAR gamma-responsive) gene were unable to feel the beneficial effects of H. pylori on glucose metabolism. Furthermore, the strains of H. pylori that carried the cag pathogenicity island were more intimately attached to the epithelial, and therefore, these strains are more likely to cause the negative effects of H. pylori, such as gastric cancer. Alternatively, the researchers were able to determine the proportions of macrophages and regulatory T cells (Treg), the cells which suppress the function of macrophages, in samples of the mice blood (1). Using the stromal vascular fraction and counting for surface expression of glycoproteins associated with each type, the researchers found that there was a lower proportion of adipose tissue macrophages and a higher proportion of Treg cells in the mice infected with cag pathogenicity island mutant 99-305 (1). In figure 1, this correlation is clearly shown. This figure identifies some of the major effects that this increase in Treg cells and decrease in macrophages would have on the white adipose tissue. The significant increase of Treg cells of H. pylori mutant strains would prevent the increase of macrophages that is a main component of Type II Diabetes Mellitus inflammation of white adipose tissue. Figure 1. Mice infected with H. pylori strain 99-305 had significant differences in adipose tissue macrophages and Treg cell counts, even when compared to non-infected and mice infected with wild-type strain 98-325. (1). Although the mechanism for the increase in Treg cells and adipose tissue macrophages remains unknown, the correlation is significant and shows the advantage that people infected with H. pylori might have over type II Diabetes Mellitus and obesity in general. Other consequences of infection Since its discovery, H. pylori has been the blame for a multitude of diseases in the human body, beginning with ulcers. In antral predominant gastritis, there is an increase in serum gastrin levels, which in turn leads to increased gastric acid secretion and volume (10). This condition results in ulcerations of the stomach, all of which is stimulated by the presence of H. pylori (10). Duodenal ulcer cancer and cancer of the gastric antrum and corpus are both directly related to colonization of this microbe (10). On the other hand, severe gastritis occurs with a decrease in acid production, and this severe atrophic gastritis is enhanced by the activity of H. pylori, thereby decreasing acid production due to its presence (10). This arises because atrophy of the stomach causes destruction of gastric glands. In turn, this improves the conditions of the gastro-esophageal reflux disease patients (10). When the microbe is then eradicated from the stomach, acid levels increase. In recent times, the use of antibiotics and increased sanitation are fighting against H. pylori infection, but this fight may be leading to an increase in GERD. In relation to this, the increase of GERD in the United States is often explained by the increase in obesity (2). However, H. pylori, as discussed previously, may be an indicator of a resistance to obesity and to type II Diabetes Mellitus. Additionally, GERD may lead to adenocarcinoma, a type of cancer that is similarly inversely correlated with H. pylori colonization of the stomach (10). Figure 2. Number of antibiotics taken in correlation with risk of diseases such as GERD . (2). Why the benefits may be null As mentioned earlier, H. pylori had been a primary inhabitant of humans’ gastrointestinal tract in years past, but what about in modern times? Recent studies have shown that H. pylori colonization has been decreasing in developed countries due to the overuse of antibiotics (3). This decrease is seen in a positive light by many because of the risks associated with carrying H. pylori cag+ strains in the stomach, such as cancer and ulcers (3). However, based on the results of the Virginia Tech research, eradication of H. pylori cag- strains may be detrimental for people in an environment prone to obesity, which the United States is often cited as being. Furthermore, Martin Blaser writes in an article about the damaging effects of the overuse of antibiotics. He states that in his lab and other labs the use of antibiotics has been irreversible, and the bacteria may never recover, including those who are beneficial to the human body (2). He writes, “Overuse of antibiotics could be fuelling the dramatic increase in conditions such as obesity, Type II Diabetes, inflammatory bowel disease, allergies and asthma, which have more than doubled in many populations,” (2). Less than 6% of children in the United States, Sweden, and Germany were infected by H. pylori around the beginning of the twenty-first century (2). However, it is clear from research that the regulation of the hormones ghrelin and leptin are intimately connected to the activity of H. pylori, and without the organism present, obesity and other diseases, such as GERD, dramatically increases. The questions remains, therefore, whether eradicating H. pylori from the gastrointestinal tract is more harmful than beneficial and whether the trend towards sterilization, in regards to H. pylori, can be reversed. Researcher Eric Harvill at Penn State University has developed his own theory for managing the negative consequences of a bacterium that also provides benefits, saying that management rather than antibiotics may be the answer (7). He writes that there has been a continuous focus on pathogens in regards to treatments, rather than a focus on the beneficial microbes that reside inside the body (7). This focus on pathogens does not make much logical sense due to the mechanisms the human body uses to protect against pathogens that additionally prevent harm of the microbiome in the body (7). For example, a protein IgA is released as an immune response against pathogens, but this protein does not have antimicrobial effects yet is able to target pathogens (7). This type of immunity might be the human body recognizing the benefits of a “healthy microbial flora” (7). In a country where obesity is one of the leading causes of health problems, his thoughts can be applied to H. pylori. In a study in Kure Kyosai Hospital, Japan, only 2.9% of the subjects infected by H. pylori had developed gastric cancer, one of the possible risks of being infected (12). However, obesity is associated with increased risks of having cancer of the esophagus, breast, endometrium, colon and rectum, kidney, pancreas, thyroid, gallbladder, and other possible cancer types (9). Furthermore, H. pylori had infected nearly the entire population of the world in years past, and this prevalence shows that its colonization of the intestinal tract may have had benefits (4). Therefore, having H. pylori as a part of the intestinal flora may be more beneficial than risky, but its benefits may be useless if the overuse of antibiotics provides an impossible environment for H. pylori to colonize. Implications for the future There are many issues that H. pylori faces in its future. Because of the benefits that H. pylori provides, many are wondering if children should be inoculated with certain strains of H. pylori in the United States. However, this depends on socioeconomic status and chances of obtaining gastric carcinoma in the area in which a child lives. In the United States, especially areas of high chances of obesity and Type II Diabetes Mellitus, this may prove beneficial and may help decrease the negative consequences of obesity, including other types of cancer. In regards to the question of inoculation for fighting certain diseases, there remains an additional question wondering which strain or combination of strains should be used. Microbiologist Blaser writes, “To best understand our future association with H pylori, we must be thinking in biological terms rather than merely in terms of patients’ symptoms or of the hyperbole in drug advertisements and the lay press” (5). A change in the thoughts of people in regards to this microbe, as it is mainly regarded in negative connotations, may improve the fight against obesity and help the health status of thousands of sufferers from diseases such gastro-esophageal reflux. However, the research available is still limiting and it may be years before a strain is capable of being inoculated in a beneficial way. Literature Cited (1) Bassaganya-Riera, J., Dominguez-Bello, M.G., Kronsteiner, B., Carbo, A., Lu, P.,Viladomiu, M., ... Hontecillas, R. (2012). Helicobacter pylori Colonization Ameliorates Glucose Homeostasis in Mice through a PPAR γ-Dependent Mechanism. PLoS ONE, 7. (2) Blaser, M. J. (2011). Antibiotic overuse: stop the killing of beneficial bacteria. Nature, 476, 393-394. (3) Blaser, M. J. (2008). Disappearing Microbiota: Helicobacter pylori Protection against Esophageal Adenocarcinoma. Cancer Prevention Research, 1, 308. (4) Blaser, M. J. (2006). Who are we? Indigenous microbes and the ecology of human diseases. EMBO reports, 7, 956-960. (5) Blaser, M. J. (1998). Science, medicine, and the future: Helicobacter pylori and gastric diseases. BMJ: British Medical Journal, 316, 1507. (6) Hacker, J., & Kaper, J.B. (2000). Pathogenicity islands and the evolution of microbes. Annual Review of Microbiology, 54, 641-679. (7) Harvill, E. T. (2013). Cultivating our “Frienemies”: Viewing immunity as microbiome management. mBio, 4(2). (8) Hatakeyama, Masanori, & Higashi, Hideaki. (2005). Helicobacter pylori CagA: a new paradigm for bacterial carcinogenesis. Cancer Science, 96, 835-843. (9) National Cancer Institute. (2012). Obesity and Cancer Risk. National Cancer Institute at the National Institutes of Health. Retrieved from www.cancer.gov/cancertopics/factsheet/Risk/obesity (10) Richter, J. E. (2001). H pylori: the bug is not all bad. GUT: An International Journal of Gastroenterology and Hepatology, 49. (11) Roper, J., Francois, F., Shue, P. L., Mourad, M. S., Pei, Z.,. Olivares de Perez, A.Z., ... Blaser, M. J. (2008). J Clin Endocrinol Metab, 93, 2350-2357. (12) Uemura N, Okamoto S, Yamamoto S, Matsumura N, Yamaguchi S, Yamakido M, Taniyama K, Sasaki N, Schlemper RJ. (2001). Helicobacter pylori and the development of gastric cancer. New England Journal of Medicine, 11, 784-789.