World Cafe. AMOC. Structure. Notes. 0309.2014
advertisement

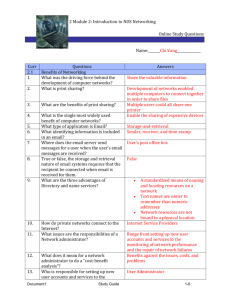
Page 1 of 5 Feedback from table 4 on the outcomes of the World Cafe exercise. STRUCTURE was the topic of this group; the group had 3 questions, see below 1. How are we organised and connected? What does not work at present? (in black) What does work or would work if it were in place ? (in red) - Silos NGO 1o clinical across and within Funding ! Competition - Geographic boundaries - Developmental – youth / elderly / adult - Collocation – Whitiora / Te Awhi Whanau, shared process - Interagency meetings – some areas 2. How do we operate? - Lack of knowledge of different services - Broken fishnet - Other agencies – fragmentation – WINZ, housing 3. Lines of communication - Issues disseminating information - Between clinical staff and NGOs – based clients ad hoc - Trish coordinating – NGO, PHO connections and iwi Document1 Page 2 of 5 - Stakeholder network Organisation and connection - Strength of personal relationships - Difference between fee for service and free service - Fragmentation between physical and mental health needs - Specialisation versus generic services Health mentally – versus mental illness What would it look like? - Shared IT system e.g. portals - Person owns their plan - Health of older person – ability and model - Coordinating of services, continuity of care with staff – navigator - Skill base for practitioners, professional, can perform - 90% things peer level support, TWON, keeping well - Good communication – staff - Must grow peer support - Good model TWON and Arataki, good benefit - Respectful partnerships Document1 Page 3 of 5 - Peer support worker navigator role - Integrated plan - Look at models of peer support - Looking at increasing options – vocation and employment STRUCTURE What would it look like? - Good relationships between staff - No gaps child & youth / adult - Structure of all services – good knowledge services - Knowledge pathways - Better alignment of clinical teams and NGOs, explore model - “One stop shop” with location of clinical/GP/NGO - Being creative – prepared to do differently - Understanding workforce and roles required - One plan between services - Range of models in CMHC - More groups - Self management early Document1 Page 4 of 5 STRUCTURE What would it look like? - Models of primary care engagement for youth, serious mental illness (barriers cost, lack of consistency, short time consultations, not seen as needed) - Maori mental health services through region - Shared information primary / secondary - Client holding information - Deeper than communication – attitude, inclination, will to work together - Diagram of services - Intersectorial forums – who meets? Review - Roles – core skills – non regulated workforce - Silos influenced by contracting – contract security and climate of collaboration - Service without professional jealousy / snobbery What would it look like? - Breakaway silos - Flexibility - One point entry - Not expecting people fitting into services - Affordable - Easily accessible - Birth - Solid blanket, not fishnet – permeable, not constricting - Try everyone GP identified - Client centred - Holistic care - Are our services in the right place? Document1 death Page 5 of 5 - Whanau centred care, outreach - Issues of Whakama STRUCTURE What would it look like? - * Social inclusion - Not stigmatising - Skills for staff in different agencies - Range of housing options to account for people who have enduring disability versus intensive short term support - More flexibility for L3/4 - Flexible respite - Less gaps between adult / C&Y services - Emphasis on whanau ora philosophy of care - No respite children – need options - Collaborative plans with whanau not inclusive agencies - Earlier access - Interagency strengthening families Our group identified that all of the above ideas could be encapsulated in the 5 areas below, this was also evident in the feedback from the 4 other groups. Everything we need to do over the life of this project should sit within these five areas. 1. 2. 3. 4. 5. Alignment Communication Models of Care Values Skills Document1