Rheumatic Conditions
advertisement

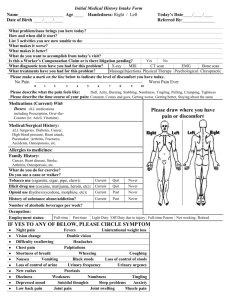
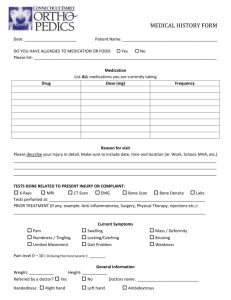
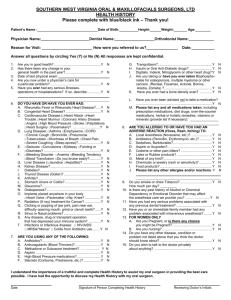
Rheumatic Conditions General competencies 1. Perform diagnostic, therapeutic and rehabilitative examination and treatment of the rheumatologic patient. 2. Optimize treatment plans a. Consult rheumatologist and arthritis resources 3. Culturally competent communication to provide understanding of the diagnosis, treatment and rehabilitation. 4. Identify multidisciplinary needs of rheumatologic patients. 5. Practice a multidisciplinary approach for rheumatologic patients including a. Mental health professionals b. Physical therapist c. Patient self- management skills 6. Provide urgent care or referrals when needed 7. Preventative medicine to decrease disability a. Recognize and emphasize its importance b. Physical activity prescriptions Topic Areas 1. Arthralgia a. Osteoarthritis (OA) i. Primary and secondary b. Rheumatoid arthritis (RA) i. Manifestations 1. Articular, extra-articular, juvenile c. Spondyloarthritis i. Ankylosing spondylitis ii. d. e. Reiter's disease iii. Psoriatic arthritis iv. Arthritis associated with inflammatory bowel disease Infections i. Directly causing arthritis 1. Septic Arthritis ii. Indirectly causing arthritis 1. Acute rheumatic fever, sub-acute bacterial endocarditis, postdysenteric Crystal-induced arthropathies 2. i. Gout ii. Acquired iii. Calcium pyrophosphate dihydrate (pseudogout) iv. Hydroxyapatite deposition f. Neoplasms g. Drug-induced Connective tissue disorders a. Lupus erythematosus (LE) i. Various presentations 1. Systemic, discoid, drug-induced b. Scleroderma i. Various presentations 1. Localized, systemic, drug/toxin-induced c. Polymyositis and dermatomyositis i. 3. ii. Distinguish from drug-induced myositis d. Sjögren's syndrome (primary and secondary) e. Polymyalgia rheumatica f. Antiphospholipid syndrome Vasculitis a. Polyarteritis nodosa b. Microscopic polyangiitis c. Hypersensitivity angiitis i. ii. d. Serum sickness Henoch-Schönlein purpura Granulomatous arteritis i. 4. Relationship to connective tissue disorders Wegener's granulomatosis ii. Giant Cell (temporal) arteritis e. Kawasaki disease f. Behcet's disease Regional rheumatic pain syndromes a. Bursitis b. Tendinitis and tendinosis c. Low back pain d. Costochondritis e. Chondromalacia patellae f. Compression i. Peripheral entrapment (e.g., carpal tunnel) ii. Radiculitis and radiculopathy iii. Spinal stenosis 5. g. Raynaud's phenomenon h. Complex regional pain syndrome Other a. Osteopenia and osteoporosis b. Osteomalacia c. Paget’s disease d. Avascular necrosis e. Relapsing panniculitis (Weber-Christian disease) f. Erythema nodosum g. Sarcoidosis h. Goodpastures disease i. Adult Still's disease j. Fibromyalgia and chronic fatigue syndrome For each topic area 1. Epidemiology 2. Anatomy 3. Pathophysiology/Etiology 4. Risk factors 5. History and physical exam 6. Clinical presentations 7. Diagnostic Tests 8. Diagnostic criteria 9. Differential diagnosis 10. Management 11. Psychosocial implications Highlighted teaching points 1. Pathophysiology/etiology a. Immunologic processes that contribute to the pathogenesis of rheumatic disease 2. Risk Factors a. For listed rheumatic conditions b. For poor prognosis 3. History and physical exam a. Basic elements of a rheumatic assessment i. Focused history 4. 5. 6. 1. For joint and soft tissue symptoms 1. For screening ii. A complete musculoskeletal physical examination iii. Functional assessment b. Use history and physical (in conjunction with laboratory tests) to monitor: i. Disease progression ii. Treatment efficacy Diagnostic tests: a. Laboratory tests i. Indications and contraindications b. Joint and bursal aspirations i. Technique ii. Interpretation of results 1. Identify crystal, inflammatory or infectious causes c. Radiographic Tests i. Order appropriate views of involved joints ii. Interpretation of results 1. Emphasis on soft tissue changes and early erosive changes d. Urgent joint conditions (e.g. “the red hot joint”) i. Recognition ii. Performing appropriate synovial fluid aspiration and analysis e. Use of laboratory test (in conjunction with clinical findings) to monitor: i. Disease progression ii. Treatment efficacy iii. Potential side effects of treatment f. Arthrocentesis i. Indications ii. Interpretation g. Tissue biopsy i. Indications ii. Interpretation h. Indications for arthroscopy Differential Diagnosis a. Development of a differential diagnosis based on i. Pattern of joint and soft tissue involvement such as symmetrical small joints, non-symmetrical large joints, axial skeleton Management a. Treatment of listed rheumatologic conditions i. Monitoring of the laboratory, physical exam and potential side 7. effects in collaboration with a rheumatologist b. Pain control modalities: i. Oral pharmacologic agents ii. Physical therapy iii. Acupuncture iv. Intra-articular and soft tissue aspirations and injections. c. Pharmacologic agents: mechanisms, indications, contra-indications, and side effects i. Analgesic medications 1. Acetaminophen 2. COX 2 inhibitors 3. Tramadol 4. Narcotics ii. Disease modifying agents 1. Anti-malarials 2. Sulfasalazine 3. Minocycline 4. Gold salts iii. Immunosuppressive agents 1. Penicillamine 2. Cytotoxic agents (methotrexate, and biologic agents) d. Osteoporosis as a side effect of treatment i. Medications causing osteoporosis ii. Treatment of osteoporosis in patients with rheumatic conditions e. Rehabilitation services i. Joint mobilization ii. Physical conditioning iii. Promote function and prevent physical disability f. Use of multidisciplinary teams: i. Rheumatologist, physiatrist, physical and occupational therapist, orthopedic surgeon and mental health provider g. Complementary therapies i. Supplements, chiropractic and acupuncture h. Disability prevention i. General health maintenance (necessary vaccinations, weight maintenance, nutrition and exercise counseling, and controlling comorbid medical conditions) Psychosocial implications a. Evaluation of limitations in activities of daily living: i. Effect on social status ii. Effect on psychological status References: 1. American Academy of Family Physicians. (2008). Recommended Curriculum Guidelines for Family Medicine Residents, Rheumatic Conditions (Reprint No. 278), Leawood, Kansas.