Epidemiology of Periodontal Disease
advertisement
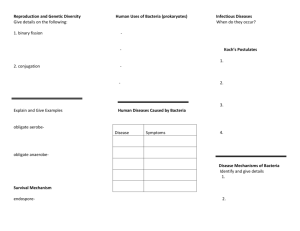
Epidemiology of Periodontal Disease This handout is provided by the CLR. Epidemiology- the study of health and disease in human populations and associated factors - Prevalence » number of cases - Incidence » rate of occurrence - Severity » level of disease - Risk Factors Local » environmental (bad dentistry, overhangs) Systemic » medical conditions Host » influences of ones own body Determinants » risk factors one can not change Periodontal disease is a complex interaction of bacterial infection, host response, and patient behavior Types of Experimental Designs - Cross-Sectional » presence or absence of disease at a particular point in time Entire population or a subset Determines the prevalence of disease - Cohort » examines a population over time Generally disease free at start and monitored for the onset of disease Asses the incidence of disease and risk factors - Case Control » compares those with and without disease Identify characteristics but cannot asses prevalence or incidence Indices- measurement systems used for collecting the necessary data - Periodontal disease Plaque Calculus Gingival inflammation Periodontal attachment level Bleeding Mobility - Index- tool which collects objective data, numerical expressions Can be quantified, tabulated and used in comparisons Predict disease patterns, progression and trends - Plaque- the major etiologic agent in the initiation and progression of inflammatory periodontal disease Plaque Index of Silness and Loe - 0-3 (no plaque at margin to heavy plaque at margin) Must be present for disease, but not all plaque causes disease - Amount, virulence, bacteria and host response/defense matters - Gingival Bleeding This handout is provided by the CLR. Gingival Index of Loe and Silness (GI) - Measure inflammation and bleeding - 0-3 Sulcus Bleeding Index (SBI) - 0-5 - Differentiates more severe signs of inflammation » significant swelling and color change - Gingival Crevicular Fluid Identifies early inflammation As inflammation increases » so does gingival fluid flow First measurable change in the inflammatory process of the periodontium Periotron calibrates filter strips - Mobility Miller Index of Tooth Mobility 0-3 ( no movement to >1mm in any direction, or tooth is depressible or can be rotated in its socket) not all movement is pathologic - Calculus- not an etiologic agent Irritant to gingival tissues which causes inflammation Can cause progression of disease Calculus Index (of Simplified Oral Hygiene Index) - Amount of calculus covering what portion of the tooth - 0-3 (no calculus to covering more than 2/3) Plaque is a dense, nonmineralized, complex mass of bacterial colonies living in a gel-like intermicrobial matrix - Readily adheres to the surface Material Alba is a loosely adherent mass of bacteria and cellular debris - Can be removed by a strong water spray Key difference: strength of adherence Accumulation of bacteria is not random - Specific, complex - Based on bacterial characteristics Five criteria make species or groups of bacteria important in the etiology of perio disease - High numbers in advancing lesions or sites » low numbers in healthy or nonprogressing sites - Clinical healing occurs upon removal - Present prior to evident clinical changes - Create a tissue reaction - Produce disease in experimental animals or humans Gram positive have a thick glycocalax capsule (slime layer) and a thin peptidoglycan layer - Lysozyme can split these units and cause lysis Gram negative have a thin capsule and a lipopolysacharides(LPS) (outer membrane) - This handout is provided by the CLR. Contains endotoxins that release upon cell lysis and directly affect host tissues or activate a host response Fimbriae or pili- small protein aqueous projections that mediate adhesion Flagella- long fine wavy structure used for motility Aerobes- require oxygen Faculative anaerobes- can use oxygen but use anaerobic fermentation when not present Aerotolerant anaerobes- can not use oxygen but can tolerate Obligate anaerobes- cannot survive in the presence of oxygen Fermentative or saccharolytic- obtain energy by breaking down complex organic compounds (carbs) such a sugars, to smaller products (lactic acid) Nonfermentative or asaccharolytic- use amino acids, simple petides and proteins for energy Bacteria Important to Periodontal Disease - P. gingivalis - T. forsynthensis - F. nucleatum - A. actinomycetemcomitans Stage 1:Pellicle Formation - Pellicle formation; membranous film that serves a nutrient source for bacteria Polishing removes Forms within minutes after cleaning teeth Forms from glycoproteins in saliva - Supragingival plaque has a salivary based nutrition, it is very organized and has the ability to adhere to the pellicle - GR + bacteria, mainly cocci Stage 2: Initial Adherence and Colonization - Hours afters pellicle formation GR –bacteria begin to proliferate - GR + rods and numerous filaments - Only bacteria with specific binding sites for pellicle constituents, and occurring in sufficient numbers can bind Lectins are adhesions that allow Secretory IGa can prevent attachment of bacteria Saliva plays a facilitative and inhibitory role in plaque formation Stage 3: Growth and Maturation - Shifts to predominately GR – - Can take anywhere from 4-7 to 7-14 days - Plaque mass accomplished by the adhesion of bacteria to one another - Bacterial coaggregation- direct interaction between surface components of different bacteria - Filaments at the salivary or external plaque become coated with cocci » corncob appearance - Bacteria can bridge for bacteria that cannot interact - This handout is provided by the CLR. Shifts from predominantly aerobic to mostly anaerobic Facultative organisms use all the oxygen so “healthy” GR + die GR – obligate anaerobes takeover due to lack of oxygen - Mature plaque has the ability to invade the gingival space Supragingival cause inflammation » gingival less tight so bacteria invades crevice Subgingival plaque is more anaerobic, more GR – ad more motile and more asaccharolytic than supragingival plaque Gingival Health vs. Disease - Health Sparse bacterial flora Mostly GR + cocci, facultatively anaerobic Some GR + rods such has Actinomyces - Gingivitis Plaque accumulation for 10-21 days Initial flora of GR + cocci and rods and GR – cocci becomes more complex Increase in anaerobic GR – rods F. nucleatum, P, intermedia, and an increase in Actinomyces - Periodontitis Domination by GR – rods P. gingivalis most important P. intermedia, T. forsynthensis, F. nucleatum Localized Juvenile Periodontitis - First molars and sometimes incisors - A. actinomycetemcomitans is main agent - Familial pattern of defective PMN’s - Less GR – than periodontitis HIV Associate Periodontitis Conditions - Differ than other infections because of reduced host response and ability to fight infection