6 Optimization Strategies for Clinical Practice Guidelines
advertisement

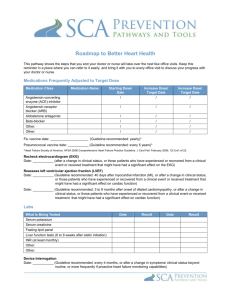
Section 6.5 Optimize Optimization Strategies for Clinical Practice Guidelines Use this tool to incorporate clinical practice guidelines and clinical quality measures into electronic health record (EHR) systems and other health information technology (HIT). Time needed: 8 – 12 hours Suggested other tools: NA How to Use 1. Review the descriptions below of clinical practice guidelines. 2. Identify the guidelines currently in use in your organization. These may be standing order sets, specific algorithms, or charting instruments. 3. Identify where other guidelines/pathways may be helpful, based on clinician experience, quality collaboratives, health plan recommendations, etc. Engage stakeholder groups to review and approve additional guidelines for use. 4. Determine the source of guidelines/pathways used by the EHR or other HIT vendor. Engage stakeholder groups to compare these to guidelines you currently use, or plan to use. Select guidelines/pathways. Clinical Practice Guidelines Clinical practice guidelines are statements developed to support provider and client decisions about therapies and treatments for specific conditions. Although guidelines have traditionally focused on ensuring a perceived standard of care among local practitioners, the focus is shifting to patient safety and quality of care—supported by the best available clinical evidence—to support decisions about what treatments are best for individual clients. The Agency for Healthcare Research and Quality (AHRQ) has compiled nationally recognized guidelines from many sources. The National Guideline Clearinghouse (at: http://www.guideline.gov/browse/by-topic.aspx) is a repository for these guidelines. Guidelines may also be developed by your facility or specialty society (see resources for such guidelines from the American Psychiatric Association at: http://www.psych.org/practice/clinical-practice-guidelines). Guideline formats vary greatly. Some are relatively straightforward sets of statements that can clearly direct template development in an EHR or other HIT. Such statements are relatively easy to incorporate into an assessment or care planning process. Guidelines with complex algorithms may best be used in an automated environment, as they provide the structure for clinical decision support (CDS) rules. Guidelines in the form of lengthy articles describing the history of the research about a disease or a differential diagnosis challenge may be difficult to incorporate into a structured data collection form. Clinical Quality Measures (CQMs) Clinical quality measures (CQMs) are related to clinical practice guidelines. They are tools that help measure and track the quality of health care services. AHRQ also maintains a repository of CQMs at http://www.qualitymeasures.ahrq.gov/browse/nqf-endorsed.aspx. Section 6 Optimize—Optimization Strategies for Clinical Practice Guidelines - 1 The Centers for Medicare & Medicaid Services (CMS) uses CQMs in a variety of quality initiatives, including quality improvement and public reporting. CQMs must be reported to earn incentives through the CMS program for meaningful use (MU) of EHRs. The Office of the National Coordinator for Health Information Technology (ONC) certifies EHRs for their ability to accurately calculate CQM results (for Stage 1) and directly report the e-CQMs from EHRs (for Stage 2) of the MU incentive program. (For additional information see: http://www.healthit.gov/policy-researchersimplementers/clinical-quality-measures.) Clinical Practice Guidelines/CQMs Usage Use the following tool to help track review of clinical practice guidelines and/or clinical quality measures for inclusion in EHR or other HIT. Guideline/Measure (Current/ Proposed) Social anxiety disorder: recognition, assessment, and treatment guideline (http://www.guideline.g ov/content.aspx?id=462 34) Date of Review December Applicability Extent of Usage Review Against EHR or Other HIT Clients exhibiting persistent fear of or anxiety about one or more social or performance situations that is out of proportion to the actual threat posed by the situation Therapists and psychiatrists Assessment template not available Action Modify generic template to support this guideline Clinical Practice Guidelines/CQMs Challenges You will encounter a number of challenges in implementing using clinical practice guidelines and CQMs: 1. Clinical practice guidelines are often based on logic, which means they may be overlooked because of their routine nature. As an example, colorectal cancer screening for patients over age 50 has been demonstrated to reduce mortality, yet these screening tests are not always ordered for all eligible patients. Reasons may include things as simple as the lack of a reminder system. 2. Clinical practice guideline development is costly, with potential for harm if not done properly. Clinical practice guidelines must be kept up-to-date. In some cases, this may require responding to new findings. For example, in April 2007, Avandia, used to control diabetes, was reported to increase risk for heart attacks and death. Although the drug was not pulled from the market and the findings were questioned, orders immediately dropped. Health care delivery organizations need to monitor this type of information and engage the clinical community in making appropriate decisions. 3. To be most widely adopted, clinical practice guidelines need to be incorporated into an EHR or other HIT. A key element of clinical practice guideline adoption is requiring accurate and complete data entry. A given guideline may require more data collection than current documentation reflects. In a busy environment, making the case for the additional Section 6 Optimize—Optimization Strategies for Clinical Practice Guidelines - 2 documentation time can be difficult. Consideration must be given to downstream time savings and client benefits. 4. Clinical quality measures may be even more difficult to implement and it may be more difficult to gain provider acceptance. Ideally, measures should be derived from clinically accepted guidance. Measurement is impacted by co-morbidities—some of which may not be known by the provider being measured. For instance, depression is now understood to be an underlying cause of hospital readmissions for patients who have heart failure or chronic obstructive pulmonary disease. It is both unhealthy and costly not to follow a depression screening guideline for such patients. Clinical quality measures require structured data entry into an EHR, or time-consuming, error-prone, and costly abstraction is required to report on the measures. For this reason, Stage 2 of the MU incentive program requires use of e-CQMs (electronic-CQMs). Copyright © 2014 Stratis Health. Section 6 Optimize—Optimization Strategies for Clinical Practice Guidelines - 3 Updated 01-01-14