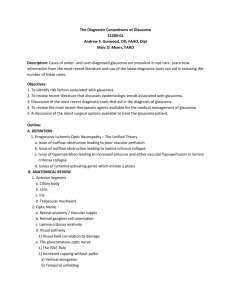
Post-review manuscript (MMPs in retina en ON - Lirias
advertisement

Invest Ophthalmol Vis Sci. 2014 Mar 28;55(3):1953-64. doi: 10.1167/iovs.13-13630. MMPs in the neuroretina and optic nerve: modulators of glaucoma pathogenesis and repair? Lies De Groefa, Inge Van Hovea, Eline Dekeystera, Ingeborg Stalmansb, Lieve Moonsa a Laboratory of Neural Circuit Development and Regeneration, Animal Physiology and Neurobiology Section, Department of Biology, KU Leuven, Leuven, Belgium b Laboratory of Ophthalmology, Department of Neurosciences, KU Leuven, Leuven, Belgium Corresponding author: Prof. Dr. Lieve Moons Research Group Neural Circuit Development and Regeneration Animal Physiology and Neurobiology Section Department of Biology KU Leuven Naamsestraat 61, Box 2464 B-3000 Leuven, Belgium Tel: (32)-16-32.39.91 Fax: (32)-16-32.42.62 Email: lieve.moons@bio.kuleuven.be 1 Abstract Multiple studies in glaucoma patients and in animal models of spontaneous and experimentally induced glaucoma, reported changes in the expression and activity of several matrix metalloproteinases (MMPs) in the retina, optic nerve, aqueous humor and trabecular meshwork. These data have led to the hypothesis that MMPs might be involved in glaucoma onset and/or disease progression. However, reports are conflicting and research aiming at providing a clear definition of their causative role is lacking. In glaucoma, MMPs are thought to act at two different levels. In the trabecular meshwork, they fine-tune the aqueous humor outflow rate and intraocular pressure, in the neuroretina and optic nerve, however, their role during glaucoma disease progression is much less clear. This review provides a comprehensive overview of the research conducted on the expression and function of MMPs in the retina and optic nerve, and on the elucidation of their potential involvement during glaucoma pathogenesis. Additionally, we describe the insecure balance between detrimental and potential beneficial MMP activities during central nervous system recovery and how MMP-based therapies could help to overcome the current pitfalls in the development of retinal ganglion cell neuroprotection and axon regeneration approaches for the treatment of glaucoma. 2 1. Introduction 1.1. MATRIX METALLOPROTEINASES At present, more than 20 human matrix metalloproteinases (MMPs) have been identified and divided into collagenases (MMP-1, -8 and -13), gelatinases (MMP-2 and -9), stromelysins (MMP-3, -10 and -11), and a heterogeneous group of MMPs (MMP-7, MMP-12, MMP-20, MMP-26 and MMP-28), based on their preferential substrates. The membrane-type or MTMMPs (MT1- to MT6-MMP) are considered a separate class, regardless of their substrate preference 1. All of these zinc (II)-dependent proteases are characterized by a conserved domain structure, including a catalytic domain, which is shielded by an auto-inhibitory pro-domain to keep the MMP in an inactive state 2-4. Besides activation of MMPs via cleavage/disruption of this prodomain, also transcriptional, posttranscriptional and epigenetic mechanisms contribute to a strict control of MMP activity, as do compartmentalization, substrate availability and inhibition of the MMPs 4, 5 . The latter is ensured by -amongst others- the TIMPs (tissue inhibitors of MMPs, TIMP1-4), that effectuate a local, reversible inhibition of MMPs in tissues 2, 5. MMPs were named after their ability to cleave and remodel the extracellular matrix (ECM), however, they clearly have a much broader degradome, also comprising proteinases, growth factors, cytokines, cell surface receptors, cell adhesion molecules, and even DNA repair enzymes and mediators of apoptosis. Essentially all MMPs have been linked to disease development, including neurodegenerative disorders such as multiple sclerosis, Huntington’s disease, Alzheimer’s disease, Parkinson’s disease, etc. 4, 6-8 . Despite their detrimental impact during central nervous system (CNS) pathology, MMPs are increasingly recognized as essential players during CNS development and in the healthy adult brain. Indeed, a well3 balanced MMP/TIMP expression has been shown to confer to neurogenesis, neurite outgrowth, myelinogenesis, angiogenesis, cell survival and adult neural progenitor migration 7-13 . Importantly, these processes do not only occur during development, but also after CNS injury, thus promoting a reparative role for MMPs during recovery from CNS injury. Taken together, there is ample evidence corroborating MMPs as fine regulators of CNS physiology and pathology, and any disturbance of their activity may result in profound implications on cell-cell and cell-ECM interactions. 1.2. GLAUCOMA Worldwide, more than 60 million people are affected by glaucomatous optic neuropathies, making this multifactorial neurodegenerative disease the second most important cause of irreversible blindness 14 . Glaucomatous neurodegeneration, characterized by progressive degeneration of the optic nerve and apoptosis of retinal ganglion cell (RGC) somata, is thought to be inflicted by a combination of genetic predisposition and age-related and environmental stressors 15, 16. The most prevalent and important risk factor, as well as the sole target for clinical intervention, is elevated intraocular pressure (IOP). Although many patients benefit from IOP lowering therapies, some patients continue to lose vision in spite of all current treatments 17, 18 . Furthermore, despite intensive research efforts, the precise cellular and molecular events translating elevated IOP and other contributing stressors into progressive RGC death, and the time course of glaucoma pathogenesis, still remain largely elusive. Expansion of our knowledge about glaucoma pathogenesis and new insights into contributing molecules/processes, seem of utmost importance for the development of innovative therapies that can preserve or restore vision. The complex etiology of the disease is reflected in the divergent array of glaucoma models, both genetic and experimentally induced, that are available to study its pathogenesis in 4 laboratory animals 19, 20 . Although each of these models mimics only a certain aspect of the disease, they do provide valuable insights in the underlying causes and mechanisms leading to RGC degeneration. While ocular hypertension-induced glaucoma models and optic nerve crush/transection are representative for the large cohort of patients with axonal damage inflicted by elevated IOP (or trauma), N-methyl-D-aspartate (NMDA)- and kainic acid (KA)mediated models and ischemia-reperfusion injury represent excitotoxicity-induced RGC damage and RGC death caused by vascular insufficiency, respectively. Of note, although covering the variety in initial insults contributing to glaucoma pathogenesis, this richness of models might also be (partially) responsible for the seemingly contradicting results that are sometimes emerging from different studies investigating glaucoma pathology. 2. Current knowledge on MMP expression and activities in the posterior segment of the glaucomatous eye In many cases, glaucomatous damage to the optic nerve and retina is caused by a pathological IOP elevation. MMPs are the major matrix degrading enzymes and have been described as important modulators of IOP in the healthy human eye, functioning in a feedback mechanism that continuously remodels the trabecular meshwork ECM composition in order to maintain a stable aqueous humor outflow resistance and IOP 21 . However, IOP homeostasis is only one aspect of glaucoma in which MMPs are involved. Regardless of the primary cause of the retinal damage, glaucomatous optic neuropathies share a common endpoint involving progressive atrophy of the optic nerve and apoptosis of RGC somata. Both in the retina and optic nerve, MMPs are known to be expressed by various glial as well as neuronal cell types (Tables 1 and 2). It is therefore very likely that MMPs, besides their role as trabecular ECM remodelers in the anterior segment of the eye, also contribute to the degenerative events 5 manifesting in the posterior segment. 2.1. MMP EXPRESSION AND ACTIVITIES IN THE GLAUCOMATOUS RETINA The gelatinases, and notably MMP-9, are by far the best studied MMPs in the retina. This might be largely due to the fact that gelatin zymography allows straightforward quantification of gelatinase activity, as such circumventing sensitivity and specificity issues related to antiMMP antibodies required for Western blot. Limited research has also been performed on the expression of MMP-1, MMP-3, MT1-MMP and TIMP-1 in the healthy and glaucomatous retina, but data about other MMPs/TIMPs are virtually absent, as apparent from Table 1. MMP expression in the retina of glaucoma patients Thus far, no more than 4 studies have investigated MMP localization in the human retina 22-25 (Table 1). These failed to detect any MMP-3 or MMP-9 expression in the healthy retina 24, yet found MMP-2 to be expressed in RGC somata and their axons 23. MMP-1 was observed both in nuclear and plexiform layers outer segments 25 24 , while MT1-MMP was only present in the photoreceptor and TIMP-2 expression was observed within the inner and outer nuclear layers of the healthy retina 24. In contrast, TIMP-1 expression, which was undetectable in the healthy retina, appeared to be upregulated in RGC somata and axons of POAG patients 23. MMP expression in the retina in animal models of glaucoma In the retina, like in any other tissue, the status and composition of the ECM is believed to modulate the synthesis and release of MMPs, and vice versa. This MMP-ECM interplay affects cell-cell and cell-ECM interactions, which may ultimately determine cell survival versus death 26 . Several studies in rodent models of glaucoma, induced by ischemia- reperfusion injury 27-31, NMDA- and KA-mediated excitotoxicity 32, 33, optic nerve transection 6 34 , or ocular hypertension 26, revealed a positive correlation between RGC death and MMP-9 activity in the RGC layer (Table 1), whereas MMP-9 activity negatively correlated with laminin immunostaining in the inner limiting membrane. Increased MMP-9 activity in the RGC layer plays a key role in the promotion of RGC death, as it induces degradation of laminin, resulting in abrogation of integrin-mediated survival signalling pathways and detachment-induced apoptosis of RGCs (‘anoikis’) 26, 28, 35 (Figure 1). Indeed, MMP-9 deficient mice subjected to an ischemia-reperfusion injury model are protected from RGC 27 death and laminin degradation , providing the ultimate evidence for MMP-9 as a crucial regulator of RGC death. In contrast, MMP-2 deficiency did not protect from RGC death after ischemia-reperfusion injury 27 and MMP-2 activity/expression was reported to remain unchanged after excitotoxic injury, ischemia-reperfusion injury or optic nerve transection 22, 30, 32-34 . However, the latter is still under debate, as others revealed increased MMP-2 activity within the first hours post ischemia-reperfusion or excitotoxic injury 31, 33 (Table 1). Co-localization studies by means of immunohistochemistry confirmed reactive astrocytes as the major source of MMP-9 expression after retinal ischemia-reperfusion injury or KAmediated excitotoxicity in mice 29, 33 , and excluded endothelial cells, microglia and RGCs 29. In contrast, in situ zymography pointed out that RGCs exhibit increased MMP-9 activity after ischemia-reperfusion injury or NMDA-mediated excitotoxicity in rats 28, 32 , while the equine retina revealed MMP-9 expression localizing to the RGC layer, inner plexiform layer and photoreceptor segments 24, 36 (Table 1). The cellular source(s) of the observed MMP-9 elevation in the glaucomatous retina thus remain obscure and more research with carefully validated anti-MMP-9 antibodies is required. For MMP-2, constitutive expression has been located to many cell types. In mice, MMP-2 was found in RGCs, Müller cells and astrocytes 33 . Also in the monkey retina, MMP-2 has been detected in RGC somata and their axons, whereas MMP-2-positive astrocytes were only found in the optic nerve head 22. In the equine 7 retina, MMP-2 expression was observed in both the inner and outer segments of the photoreceptors and in the adjacent outer limiting membrane 36 (Table 1). Notably, while MMP-9 expression is low in the healthy retina, prominent expression of its major inhibitor, TIMP-1, is seen in RGC somata and their axons in the nerve fiber layer 26 22, 23, (Table 1). Moreover, the increase in MMP-9 activity in response to elevated IOP was repeatedly reported to be accompanied by an increased TIMP-1 expression, which was found to display a positive correlation with the degree of IOP exposure 26, 32, 37, 38. While constitutive TIMP-1 expression was suggested to support synaptic plasticity at the RGC terminals and maintenance of an intact ECM (i.e. by keeping MMP activity within limits) 22, the increase in TIMP-1 levels might facilitate its neuroprotective effects on RGCs, either via inhibition of detrimental MMP-9 activity, or via MMP-independent anti-apoptotic actions 26 , as shown elsewhere in the CNS 39, 40 (Figure 1). Expression of TIMP-2, which seems rather confined to the outer retina, was reported to remain unchanged 24, 31, 33, 36 (Table 1). Several theories, that have in common the inflammatory cytokine interleukin-1 (IL-1), exist about how MMP-9 activity is induced in experimental models of RGC degeneration (Figure 1). Glaucomatous injury in the retina stimulates the production of IL-1β by astrocytes, which could upregulate MMP-9 synthesis in astrocytes (and/or RGCs) increases nitric oxide production 30, 33, 41 30 . In addition, IL-1 also , which may activate extracellular pro-MMP-9 via S- nitrosylation and oxidation of the enzyme’s cysteine switch 32, 33, 42 . Alternatively, MMP-9 expression might be augmented directly or indirectly, via IL-1 signalling cascades, by increased retinal glutamate levels, which can be induced by various stimuli, including injury, ischemia and elevated IOP 26, 33 . Finally, in addition to IL-1, other cytokines such as TNF-α and TGF-β2 are likely to contribute to the upregulation of MMP expression in the glaucomatous retinas as well. In rodent models for glaucoma, as well as in human patients, elevated levels of TNF-α and decreased levels of TGF-β2 have been repeatedly noted in the 8 glaucomatous retina, and these cytokines are well known as, respectively, inducer and inhibitor of MMP transcription 26, 43-46 . However, in contrast to reported observations in the optic nerve (head) (see below), a causal relationship between altered TNF-α or TGF-β2 expression and increased MMP transcription has not yet been described in the glaucomatous retina. Of note, alternative/additional mechanisms of action of MMP-9, besides anoikis, have never been excluded. These could comprise a direct contribution of MMP-9 to apoptotic signalling cascades, MMP-9-dependent cleavage of precursors of neurotoxic proteins, MMP-9-mediated increases in Ca2+ influx or dysfunctional retrograde transport of cell survival factors secondary to the loss of ECM attachment 27, 32, 47. Limited attention has been devoted to expression of other MMPs, i.e. MMP-3 and MT1-MMP, in the healthy and glaucomatous retina so far. A microarray analysis on the retina of rats subjected to an ocular hypertension glaucoma model, revealed 3.5-fold upregulated MMP-3 mRNA levels at 35 days post induction of ocular hypertension 37 . Likewise, MMP-3 mRNA levels were strongly increased after optic nerve crush and optic nerve transection in rats, i.e. over 50-fold and over 250-fold, respectively 43. The cellular origin of MMP-3 expression has not yet been discovered. Nevertheless, these data, suggesting MMP-3 to be an important player during glaucomatous damage, together with the described pro- and anti-apoptotic actions of MMP-3 in the CNS 48, 49 , indicate that MMP-3 is worthwhile investigating. For MT1-MMP, knowledge is restricted to expression studies in the healthy retina, where MT1MMP has been reported in the nerve fiber layer of newborn (P0) mice and adult rabbits 50, 51 and in the photoreceptor segments of equine retina36. Overall, the expression of MMP-2, -3, and -9 in the healthy and glaucomatous retina hints that MMPs might be important players in retinal health and disease. However, largely due to a 9 lack of functional studies, it is currently impossible to define their exact or causative role. Whereas MMP-9 has a clear negative impact on RGC survival, the role of MMP-2 in glaucomatous damage in the retina remains obscure. Although MT1-MMP, MMP-1 and MMP-3 were shown to be expressed in the retina, the latter even being upregulated upon axonal damage, we can only speculate about their function. For TIMP-1, a neuroprotective role in the CNS has been suggested, both via modulation of MMP activity as well as via MMP-unrelated pathways, but whether a similar function exists in the retina remains currently elusive. 2.2. MMP EXPRESSION AND ACTIVITIES IN THE GLAUCOMATOUS OPTIC NERVE (HEAD) As RGC axons exit the primate (or canine) eye to the optic nerve, their sole support and protection is the lamina cribrosa, making the optic nerve head (ONH) a fragile site in an otherwise rigid corneoscleral shell 52 and the major site of impact of the mechanical stress generated by elevated IOP. The lamina cribrosa is composed of cribriform plates that are aligned to form channels for the RGC axons, and an ECM with collagenous columns, to which glial cells (GFAP+ astrocytes and GFAP- lamina cribrosa cells) are anchored by a basement membrane 53. Upon exposure to excessive mechanical stress, characteristic changes take place in the lamina cribrosa: the cribriform plates collapse and the glial cells shift their production of ECM components to those that are characteristic for the glaucomatous phenotype and increase their secretion of MMPs 22, 53-57 . As a consequence, the ECM is remodeled, which adversely affects the capacity of the lamina cribrosa to support RGC axons and predisposes RGCs to axonal compression, arrest of axoplasmic flow and apoptosis 53, 55, 56. Although the rodent ONH only has a rudimentary lamina cribrosa, it does possess a glial 10 lamina with a collagenous composition and a ultrastructural organisation that closely resembles that of the primate. Indeed, the ONH still appears to be the site of early pressureinduced optic nerve injury in rodents, and the above mentioned mechanisms of pathological remodelling seem conserved 58. MMP expression in the ONH of glaucoma patients Despite the restricted number of studies investigating in vivo MMP/TIMP expression and activities in the human glaucomatous optic nerve, we do have some basic indirect insights into the actions of MMPs that contribute to optic nerve axonal degeneration in glaucoma patients. Human ONH glia were reported to increase their secretion of cytokines, such as transforming growth factor-β1 (TGF-β1) 53, 57, 59 and tumor necrosis factor-α (TNF-α) 44, 45, 54, 60, in response to glaucomatous damage, which may act in an auto- or paracrine way to promote other stretch-induced reactions, including stimulation of MMP-2 secretion, leading to progressive ECM remodeling (Figure 2). Indeed, increased immunoreactivity for MMP-2 has been observed in the lamina cribrosa of glaucomatous patients and in vitro in ONH glial cells undergoing mechanical stretching, corroborating ONH glial cells -next to the RGC axons- as the source of MMP-2 53, 54, 57, 60 (Table 2). In addition to MMP-2, also MT1-MMP and TIMP3 were reported to be upregulated in an in vitro culture of human lamina cribrosa cells exposed to cyclic mechanical stretching 57. In the healthy human optic nerve, quiescent astrocytes express low levels of MMP-1, -2, and MT1-MMP, as well as TIMP-1 and -2 23, 60 . In the glaucomatous optic nerve, astrocytes undergo a transition from a quiescent to a reactive phenotype, which involves increased expression of MMP-1 and MT1-MMP, changes in cell shape and relocation in the nerve bundles 23, 60 . The increased expression of MT1-MMP on their plasma membrane was suggested to allow astrocytes to detach and migrate from the underlying basement membrane, 11 by cleavage of ECM and cell surface adhesion molecules at their migration front and/or by altering their cytoskeleton (Figure 2). Of note, the membrane-bound MT1-MMP can not only directly exert these actions, but can also indirectly activate MMP-2 expressed by RGC axons and ONH glial cells, assuring that MMP-2 is activated at the cell-ECM interface 23 . Subsequently, MMP-1 is believed to permit migration of astrocytes throughout the ECM of the lamina cribrosa into the nerve bundles, where MMP-1, if not counterbalanced by TIMP-1, will continue to degrade the ECM around the axons and consequently interfere with neuronal survival 23 (Figure 2). Notably, a similar neurotoxic effect of MMP-1, released by astrocytes, was observed in organotypic rat spinal cord and human brain astrocyte cultures, via destruction of the ECM and/or activation of cytokines 61. MMP expression in the OHN in animal models of glaucoma Several lines of evidence, obtained from research in various animal models of glaucoma, support the above-mentioned modes of action of MMPs in the glaucomatous ONH. TGF-β1 receptor, MMP-2 and TIMP-1 were shown to be augmented in the optic nerve during the onset stage in an IOP-induced glaucoma model in rats 62 , and in the healthy monkey optic nerve, low levels of MMP-1, -2, and MT1-MMP, as well as TIMP-1 and -2, expressed by quiescent astrocytes, were revealed 22 . In the latter study, Agapova et al. confirmed their previous work on human samples. In addition, by comparing MMP expression in the optic nerve of monkeys with ocular hypertension-induced glaucoma to monkeys subjected to optic nerve transection, they were able to prove that the observed ECM remodeling and elevated MMP-1 and MT1-MMP expression in the optic nerve during glaucoma, occur in response to elevated IOP and are not secondary to axonal loss 22. In addition to these animal studies, Hughes et al. investigated the involvement of MMPs in Wallerian degeneration induced by ONC in rats and found MMP-9 expression in optic nerve 12 astrocytes, which is in contrast to the expression pattern found in the glaucomatous monkey ONH, where MMP-9 was expressed by oligodendrocytes 22, 63 . MMP-3, in accordance to expression studies in monkey, was observed in glial cells and blood vessels and upregulated in glia upon glaucomatous damage to the optic nerve 22, 63 . MMP-7 and MMP-12, finally, are both expressed by astrocytes upon optic nerve crush in rats 63 (Table 2). Overall, even when integrating the findings from human and animal studies, the available data about the expression of MMPs in the glaucomatous optic nerve are sparse and puzzling (Table 2). There is a general consensus that elevated IOP induces an increase in MMP-1 and MT1MMP expression levels, which might in turn negatively impact on the optic nerve microenvironment. However, reports disagree on the effect of ocular hypertension-induced mechanical stretching on MMP-2 and TIMP expression in the optic nerve head: while some describe an increase in MMP-2 and TIMP-1 levels expression of MMP-2, TIMP-1 and TIMP-2 22, 23, 63 53, 57, 60, 62 , others note constitutive , or even decreased levels of TIMP-1 and TIMP-2 due to axon loss 22. 3. Can MMP modulation facilitate neuroprotective and regenerative glaucoma therapies? Current glaucoma therapies are all directed towards a sustained reduction of IOP, and slow down or halt glaucomatous disease progression in many but not all patients 17, 18. Nonetheless, glaucoma typically leads to irreversible loss of vision because of the inability of adult mammals to repair or regenerate damaged RGCs. An effective treatment for glaucoma, able to restore vision, would involve neuroprotection and/or replacement of damaged RGCs in the retina, as well as induction of their axonal regenerative capacity in the optic nerve 64. Here, we 13 review current evidence for a carefully balanced MMP activity as crucial modulator of the receptiveness of the retinal and optic nerve extracellular environment to neuroprotection, stimulation of axon regeneration and cell transplantation therapy. 3.1. CAN MMPS MODULATE RGC NEUROPROTECTION IN THE RETINA? MMP-9 deficiency was already mentioned earlier in this review for its neuroprotective effects in a rat ischemia-reperfusion model for glaucoma 27 (Figure 1). In retinal excitotoxicity models in rats and mice, the broad-spectrum MMP inhibitor GM6001 prevented pathological remodeling of the inner limiting membrane and detachment-induced apoptosis of the RGCs, confirming that MMPs, most likely MMP-9, indeed contribute to RGC death 28, 32, 33. Specific MMP-9 inhibitors, or agents acting on downstream targets in the MMP-9-induced RGC apoptotic pathway, might thus serve as neuroprotective agents in retinal neurodegenerative diseases, including glaucoma, retinal artery/vein occlusion and ischemic optic neuropathy 32 . Also TIMP-1 expression has been shown to be upregulated in the retina of rats exposed to ocular hypertension26, 37, 38 . This TIMP-1 elevation is likely to reflect the canonical co- regulation of MMPs and TIMPs, designed to keep pro-apoptotic MMP-9 activity within limits 26 , but, in addition, TIMP-1 might also promote RGC survival by directly suppressing apoptosis signalling pathways, in an MMP-independent manner 26, 39, 40 (Figure 1). 3.2. CAN MMPS MODULATE AXONAL REGENERATION IN THE OPTIC NERVE? Upon injury in the mammalian CNS, the ECM transforms from a growth-permissive to an inhibitory environment, thereby largely preventing CNS neurons from regenerating axons to their former targets. This failure of the mammalian CNS to regenerate axonal projections is multifactorial. In addition to the diminished intrinsic growth capacity of adult CNS neurons 65, 14 the injured CNS becomes deprived of neurotrophic factors and/or their receptors 66, and glial scar- and myelin-derived inhibitory molecules form a physicochemical barrier for regenerating axons 67, 68. MMPs have been suggested as key facilitators of successful axonal regeneration for several reasons (Figure 3). First of all, MMPs add to the clearance of cellular and matrix debris at the site of injury. Second, all major constituents of the glial scar are substrates of at least one MMP 68, 69 and increased MMP activity reduces glial scarring and associated inhibitory molecules. In particular, the chondroitin sulphate proteoglycans (CSPGs) have been denoted for their strong inhibitory impact on axonal regeneration 67 and are subject to cleavage by MMPs. Indeed, the repulsion of neurite growth cones and ‘masking’ of neurite-promoting laminin by CSPGs, can be (partially) abrogated by MMPs 68, 70, 71. Third, MMPs are also able to degrade myelin-derived inhibitory ligands released by degenerating CNS axons, such as neurite outgrowth inhibitor (Nogo), myelin associated glycoprotein (MAG), oligodendrocyte myelin glycoprotein (OMgp) and myelin basic protein (MBP) 8, 67, 68, 72, 73 . Forth, besides disarming inhibitory ECM and signalling molecules, MMPs can also unmask, activate or release others that have a beneficial effect on CNS repair. As such, they can indirectly provide neurotrophic support to regenerating axons via the release of sequestered growth factors (e.g. release of basic fibroblast growth factor (bFGF) from ECM heparin sulphate proteoglycans) or the conversion of inactive pro-growth factors to their active forms (e.g. nerve growth factor (NGF), brain-derived neurotrophic factor (BDNF)) 8, 68 . Finally, as the directed outgrowth of axons requires extensive motility and infiltration within the nervous tissue, MMPs can invoke ‘focalised’ proteolysis at the growth cone 74 thereby reorganizing the ECM to facilitate attachment and motility of the growing axon 75 (Figure 3). Although thus far only described in the brain and spinal cord, it can be assumed that these MMP actions can be extrapolated to the entire CNS, including the retina and optic nerve. 15 Indeed, stimulation of axonal regeneration after optic nerve transection in rats, by intravitreal transplantation of a peripheral nerve segment, coincides with significantly enhanced MMP activity in the regenerating optic nerve as compared to the non-regenerating optic nerve 67 . More specifically, MMP-2 and MMP-9, and to a lesser extent also MMP-1 and MMP-3, are upregulated in the proximal optic nerve stump and at the site of the optic nerve injury, while TIMP-1 and -2 are suppressed. This immediate local upregulation (coinciding with post injury inflammation) of MMP-2 and -9 by reactive astrocytes is thought to clear tissue debris, in concert with invading macrophages (Figure 3). The later burst in gelatinase activity (i.e. 8 days post injury), which co-localizes with ECM compounds of the glial scar, might serve to break down and dissolve the glial scar, thereby clearing the path for regenerating axons 67, 76 (Figure 3). Remarkably, gelatinase activity only rarely co-localizes with regenerating optic nerve axons, in contrast to regenerating peripheral nerves, where growth cones secrete MMP2 (and MMP-3) to facilitate the progression of dorsal root ganglia cell axons on the peripheral nerve basal lamina 74, 77. Instead, reactive astrocytes at the site of injury appear to be the major source of gelatinases in the CNS 67, 76. Ahmed et al. hypothesized that the numerous collateral sprouts in the proximal stump of the transected optic nerve and the growth cones at the front of the regenerating axons, release a -thus far unknown- factor that conditions the surrounding astrocytes to increase MMP and downregulate TIMP expression 67 (Figure 3). The result is a resolution of glial- and myelin-derived growth inhibitory ligands, and RGC axon regeneration is less hampered 67 . Also other experimental approaches that succeeded to induce axonal regeneration in the optic nerve, attributed at least part of their success to MMP-related activities. Transplantation of neural tube-derived chicken embryonic stem cells at the site of optic nerve transection in rats induced the activation of MMP-2 and MT1-MMP in optic nerve astrocytes and resulted in regrowth of axons across the lesion site due to degradation of CSPGs 16 78 . Similarly, transplantation of olfactory ensheating cells was reported to promote neurite outgrowth in vitro in a rat retinal cell culture, via secretion of MMP-2 and degradation of CSPGs 79 . Moreover, endogenous MMP-2, produced by retinal astrocytes, seems to be essential to neurite outgrowth in an in vitro mouse retinal explant model 80. Taken together, MMPs can potentially play part in many different aspects of successful axonal regeneration. In the optic nerve, it is already evident that they can add to the conversion of the nerve environment from a repressive to a facilitative substratum for axon growth. However, many other aspects of RGC axon regeneration to which MMPs could theoretically contribute, remain unexplored. Recently, substantial progress was made in initiating robust axonal regeneration of RGCs in rodents via induction of controlled ocular inflammation and PTEN (phosphatase and tensin homolog) deletion 81-85 . Given these new insights, it might be a good time to re-assess the potential involvement of MMPs in these models of RGC axonal regeneration. 3.3. CAN MMPS MODULATE CELL THERAPY IN THE RETINA? Besides the prevention of neurite outgrowth, glial scar-derived growth-inhibitory molecules also hamper successful cell transplantation therapies by blocking donor-host integration in the retina 86-89 . However, increased MMP expression and subsequent decreased deposition of inhibitory ECM molecules in the retina, was reported to create a more permissive environment for regeneration and cell integration. Indeed, elevated expression of MMP-2, -9 and MT1-MMP in the mouse retina, decreases glial barrier formation at the outer limiting membrane and facilitates incorporation of grafted photoreceptor sheets 89 . Accordingly, controlled release of MMP-2 directly at the site of injury, enhances progenitor cell integration and retinal repopulation after subretinal transplantation in rodents 86, 90-93 . Unfortunately, focus has been on cell therapies for the ‘outer’ retina, i.e. for photoreceptor degeneration 94-98, and little evidence has been provided thus far that intravitreally transplanted stem/progenitor 17 cells can survive and integrate in the ‘inner’ retina. Of note, transplantation of progenitor/stem cells in the inner retina could be used to replace lost RGCs and ultimately, but rather unlikely, to rewire the entire complex retinotopic circuit. But, alternatively, progenitor/stem cells could also be delivered to provide neuroprotection to the remainder RGCs or to transform the host retina into a state that is more permissive to endogenous attempts of repair. Anyway, regardless of the envisioned strategy, the improvement of the integration efficiency of the transplanted cells is one of the many challenges for the successful development of cell therapy in the glaucomatous retina 87 . Nonetheless, given the modest successes with human Müller stem cell and rat oligodendrocyte precursor cell transplantations in rat glaucoma models 99, 100, the recent insights in the nature of the barriers to inner retinal engraftment 87, 88 and the lessons learned from research in the outer retina, it might be worthwhile to explore whether MMPs could be facilitators of host-donor integration in the inner retina. 4. Concluding remarks and future directions Overall, our knowledge on the involvement of MMPs during the onset and disease progression of glaucoma is limited. While MMPs are recognized beneficial players in IOP homeostasis in the anterior segment of the eye 21 , we are still in the dark about their nature and the processes they contribute to, in the posterior segment. In the optic nerve, MMP-1 and MT1-MMP are believed to be involved in the onset of glaucoma, and upregulated MMP-3 and -9 expression in the retina hints that MMPs might be important players in glaucoma pathogenesis as well. However, because of the shortage of functional studies, it is currently impossible to define their exact or causative role. Nevertheless, the scientific community progresses to understand the complex spatial and temporal regulation of beneficial and detrimental effects of MMPs during and after CNS 18 injury and is starting to explore the potential of MMP-based approaches to facilitate CNS repair. In the retina and optic nerve, in particular the gelatinases are emerging as modulators of the receptiveness to neuroprotection, stimulation of axon regeneration and cell transplantation therapy. However, more in-depth studies of MMP activity in time and space are imperative to disentangle the complex ‘protease web’ of which they are part and to identify the myriad of functions fulfilled by MMPs 101. Such studies should consist of systemwide, in vivo approaches, including conditional and/or cell-specific MMP gene deletion, MMP downregulation via RNAi, highly specific inhibitors or blocking antibodies/nanobodies, or alternatively, MMP upregulation via cell-specific viral vector-mediated gene delivery or recombinant MMP, all in combination with high-content proteomic profiling techniques. Indeed, essential to the design of future MMP-based therapies, is the identification of direct MMP substrates and downstream pathways underlying time and space restricted MMP functions. This can be achieved by means of degradomics studies after genetic or pharmacological MMP inhibition, mice deficient in particular MMP substrates, in vitro cleavage, cleavage site protection/mutagenesis or yeast-two-hybrid assays. These approaches should point out MMP drug targets exacerbating pathology as well as anti-targets that provide protection or resolution, and will not only allow the development of a novel generation of highly specific MMP inhibitors and MMP inducers/activators, but more likely, they will result in alternative therapies targeting upstream or downstream factors of MMP-modulated networks. 19 Conflicts of interest statement The authors have no conflict of interest. Acknowledgements The authors acknowledge the Research Foundation Flanders (FWO-Vlaanderen, Belgium, G.05311.10) and the KU Leuven Research Council (KU Leuven, Belgium, BOF-OT/10/033). Lies De Groef is a research fellow of the Flemish government agency for Innovation by Science and Technology (IWT-Vlaanderen, Belgium), Eline Dekeyster is a research fellow and Ingeborg Stalmans is a senior clinical research fellow of FWO-Vlaanderen. 20 References 1. Klein T, Bischoff R. Physiology and pathophysiology of matrix metalloproteases. Amino Acids 2010. 2. Ethell IM, Ethell DW. Matrix metalloproteinases in brain development and remodeling: synaptic functions and targets. J Neurosci Res 2007;85:2813-2823. 3. Page-McCaw A, Ewald AJ, Werb Z. Matrix metalloproteinases and the regulation of tissue remodelling. Nat Rev Mol Cell Biol 2007;8:221-233. 4. Rosenberg GA. Matrix metalloproteinases and their multiple roles in neurodegenerative diseases. Lancet Neurol 2009;8:205-216. 5. Sternlicht MD, Werb Z. How matrix metalloproteinases regulate cell behavior. Annu Rev Cell Dev Biol 2001;17:463-516. 6. Miller JP, Holcomb J, Al-Ramahi I, et al. Matrix metalloproteinases are modifiers of huntingtin proteolysis and toxicity in Huntington's disease. Neuron 2010;67:199-212. 7. Rivera S, Khrestchatisky M, Kaczmarek L, Rosenberg GA, Jaworski DM. Metzincin proteases and their inhibitors: foes or friends in nervous system physiology? J Neurosci 2010;30:15337-15357. 8. Yong VW. Metalloproteinases: mediators of pathology and regeneration in the CNS. Nat Rev Neurosci 2005;6:931-944. 9. Fujioka H, Dairyo Y, Yasunaga K, Emoto K. Neural functions of matrix metalloproteinases: plasticity, neurogenesis, and disease. Biochem Res Int 2012;2012:789083. 10. Milward EA, Fitzsimmons C, Szklarczyk A, Conant K. The matrix metalloproteinases and CNS plasticity: an overview. J Neuroimmunol 2007;187:9-19. 11. Tonti GA, Mannello F, Cacci E, Biagioni S. Neural stem cells at the crossroads: MMPs may tell the way. Int J Dev Biol 2009;53:1-17. 12. Zhang H, Adwanikar H, Werb Z, Noble-Haeusslein LJ. Matrix metalloproteinases and neurotrauma: evolving roles in injury and reparative processes. Neuroscientist 2010;16:156170. 13. Verslegers M, Lemmens K, Van Hove I, Moons L. Matrix metalloproteinase-2 and -9 as promising benefactors in development, plasticity and repair of the nervous system. Prog Neurobiol 2013;105:60-78. 14. Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol 2006;90:262-267. 15. Calkins DJ, Horner PJ. The cell and molecular biology of glaucoma: axonopathy and the brain. Invest Ophthalmol Vis Sci 2012;53:2482-2484. 16. Leske MC, Heijl A, Hyman L, Bengtsson B, Dong L, Yang Z. Predictors of long-term progression in the early manifest glaucoma trial. Ophthalmology 2007;114:1965-1972. 17. Heijl A, Leske MC, Bengtsson B, Hyman L, Hussein M. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol 2002;120:1268-1279. 18. Iwase A, Suzuki Y, Araie M, et al. The prevalence of primary open-angle glaucoma in Japanese: the Tajimi Study. Ophthalmology 2004;111:1641-1648. 19. Bouhenni RA, Dunmire J, Sewell A, Edward DP. Animal models of glaucoma. J Biomed Biotechnol 2012;2012:692609. 20. Johnson TV, Tomarev SI. Rodent models of glaucoma. Brain Research Bulletin 2010;81:349-358. 21. De Groef L, Van Hove I, Dekeyster E, Stalmans I, Moons L. MMPs in the Trabecular Meshwork: Promising Targets for Future Glaucoma Therapies? Investigative Ophthalmology & Visual Science 2013;54:7756-7763. 21 22. Agapova OA, Kaufman PL, Lucarelli MJ, Gabelt BT, Hernandez MR. Differential expression of matrix metalloproteinases in monkey eyes with experimental glaucoma or optic nerve transection. Brain Res 2003;967:132-143. 23. Agapova OA, Ricard CS, Salvador-Silva M, Hernandez MR. Expression of matrix metalloproteinases and tissue inhibitors of metalloproteinases in human optic nerve head astrocytes. Glia 2001;33:205-216. 24. Webster L, Chignell AH, Limb GA. Predominance of MMP-1 and MMP-2 in epiretinal and subretinal membranes of proliferative vitreoretinopathy. Exp Eye Res 1999;68:91-98. 25. Smine A, Plantner JJ. Membrane type-1 matrix metalloproteinase in human ocular tissues. Curr Eye Res 1997;16:925-929. 26. Guo L, Moss SE, Alexander RA, Ali RR, Fitzke FW, Cordeiro MF. Retinal ganglion cell apoptosis in glaucoma is related to intraocular pressure and IOP-induced effects on extracellular matrix. Invest Ophthalmol Vis Sci 2005;46:175-182. 27. Chintala SK, Zhang X, Austin JS, Fini ME. Deficiency in matrix metalloproteinase gelatinase B (MMP-9) protects against retinal ganglion cell death after optic nerve ligation. J Biol Chem 2002;277:47461-47468. 28. Santos ARC, Corredor RG, Obeso BA, et al. Beta1 Integrin-Focal Adhesion Kinase (FAK) Signaling Modulates Retinal Ganglion Cell (RGC) Survival. PLoS One 2012;7:e48332. 29. Zhang X, Cheng M, Chintala SK. Optic nerve ligation leads to astrocyte-associated matrix metalloproteinase-9 induction in the mouse retina. Neurosci Lett 2004;356:140-144. 30. Zhang X, Chintala SK. Influence of interleukin-1 beta induction and mitogen-activated protein kinase phosphorylation on optic nerve ligation-induced matrix metalloproteinase-9 activation in the retina. Experimental Eye Research 2004;78:849-860. 31. Zhang X, Sakamoto T, Hata Y, et al. Expression of matrix metalloproteinases and their inhibitors in experimental retinal ischemia-reperfusion injury in rats. Exp Eye Res 2002;74:577-584. 32. Manabe S, Gu Z, Lipton SA. Activation of matrix metalloproteinase-9 via neuronal nitric oxide synthase contributes to NMDA-induced retinal ganglion cell death. Invest Ophthalmol Vis Sci 2005;46:4747-4753. 33. Zhang X, Cheng M, Chintala SK. Kainic acid-mediated upregulation of matrix metalloproteinase-9 promotes retinal degeneration. Invest Ophthalmol Vis Sci 2004;45:23742383. 34. Sun MH, Chen KJ, Tsao YP, et al. Down-regulation of matrix metalloproteinase-9 by pyrrolidine dithiocarbamate prevented retinal ganglion cell death after transection of optic nerve in rats. Curr Eye Res 2011;36:1053-1063. 35. Halfter W, Willem M, Mayer U. Basement Membrane-Dependent Survival of Retinal Ganglion Cells. Investigative Ophthalmology & Visual Science 2005;46:1000-1009. 36. Hofmaier F, Hauck SM, Amann B, Degroote RL, Deeg CA. Changes in matrix metalloproteinase network in spontaneous autoimmune uveitis model. Invest Ophthalmol Vis Sci 2011. 37. Ahmed F, Brown KM, Stephan DA, Morrison JC, Johnson EC, Tomarev SI. Microarray analysis of changes in mRNA levels in the rat retina after experimental elevation of intraocular pressure. Invest Ophthalmol Vis Sci 2004;45:1247-1258. 38. Guo Y, Cepurna WO, Dyck JA, Doser TA, Johnson EC, Morrison JC. Retinal cell responses to elevated intraocular pressure: a gene array comparison between the whole retina and retinal ganglion cell layer. Invest Ophthalmol Vis Sci 2010;51:3003-3018. 39. Magnoni S, Baker A, Thomson S, et al. Neuroprotective effect of adenoviral-mediated gene transfer of TIMP-1 and -2 in ischemic brain injury. Gene Ther 2007;14:621-625. 40. Tan HK, Heywood D, Ralph GS, Bienemann A, Baker AH, Uney JB. Tissue inhibitor 22 of metalloproteinase 1 inhibits excitotoxic cell death in neurons. Molecular and Cellular Neuroscience 2003;22:98-106. 41. Kido N, Inatani M, Honjo M, et al. Dual effects of interleukin-1beta on N-methyl-Daspartate-induced retinal neuronal death in rat eyes. Brain Res 2001;910:153-162. 42. Gu Z, Kaul M, Yan B, et al. S-Nitrosylation of Matrix Metalloproteinases: Signaling Pathway to Neuronal Cell Death. Science 2002;297:1186-1190. 43. Agudo M, Perez-Marin MC, Lonngren U, et al. Time course profiling of the retinal transcriptome after optic nerve transection and optic nerve crush. Mol Vis 2008;14:1050-1063. 44. Tezel Gln, Li LY, Patil RV, Wax MB. TNF-α and TNF-α Receptor-1 in the Retina of Normal and Glaucomatous Eyes. Investigative Ophthalmology & Visual Science 2001;42:1787-1794. 45. Tezel Gln, Carlo Nucci LCNNO, Giacinto B. TNF-α signaling in glaucomatous neurodegeneration. Progress in Brain Research: Elsevier; 2008:409-421. 46. Nakazawa T, Nakazawa C, Matsubara A, et al. Tumor necrosis factor-alpha mediates oligodendrocyte death and delayed retinal ganglion cell loss in a mouse model of glaucoma. J Neurosci 2006;26:12633-12641. 47. Chintala SK. The emerging role of proteases in retinal ganglion cell death. Exp Eye Res 2006;82:5-12. 48. Kim EM, Hwang O. Role of matrix metalloproteinase-3 in neurodegeneration. J Neurochem 2011;116:22-32. 49. Kim E-M, Shin E-J, Choi JH, et al. Matrix Metalloproteinase-3 Is Increased and Participates in Neuronal Apoptotic Signaling Downstream of Caspase-12 during Endoplasmic Reticulum Stress. Journal of Biological Chemistry 2010;285:16444-16452. 50. Gariano RF, Hu D, Helms J. Expression of angiogenesis-related genes during retinal development. Gene Expr Patterns 2006;6:187-192. 51. Takano A, Hirata A, Inomata Y, et al. Intravitreal plasmin injection activates endogenous matrix metalloproteinase-2 in rabbit and human vitreous. Am J Ophthalmol 2005;140:654-660. 52. Sigal IA, Ethier CR. Biomechanics of the optic nerve head. Exp Eye Res 2009;88:799807. 53. Kirwan RP, Crean JK, Fenerty CH, Clark AF, O'Brien CJ. Effect of cyclical mechanical stretch and exogenous transforming growth factor-beta1 on matrix metalloproteinase-2 activity in lamina cribrosa cells from the human optic nerve head. J Glaucoma 2004;13:327-334. 54. Akhter N, Nix M, Abdul Y, Singh S, Husain S. Delta-Opioid Receptors Attenuate TNF-alpha-Induced MMP-2 Secretion from Human ONH Astrocytes. Invest Ophthalmol Vis Sci 2013. 55. Dahlmann-Noor AH, Vijay S, Limb GA, Khaw PT. Strategies for optic nerve rescue and regeneration in glaucoma and other optic neuropathies. Drug Discov Today 2010;15:287299. 56. Hernandez MR. The optic nerve head in glaucoma: role of astrocytes in tissue remodeling. Progress in Retinal and Eye Research 2000;19:297-321. 57. Quill B, Docherty NG, Clark AF, O'Brien CJ. The Effect of Graded Cyclic Stretching on Extracellular Matrix–Related Gene Expression Profiles in Cultured Primary Human Lamina Cribrosa Cells. Investigative Ophthalmology & Visual Science 2011;52:1908-1915. 58. Morrison JC, Cepurna Ying Guo WO, Johnson EC. Pathophysiology of human glaucomatous optic nerve damage: Insights from rodent models of glaucoma. Experimental Eye Research 2011;93:156-164. 59. Zode GS, Sethi A, Brun-Zinkernagel AM, Chang IF, Clark AF, Wordinger RJ. Transforming growth factor-beta2 increases extracellular matrix proteins in optic nerve head 23 cells via activation of the Smad signaling pathway. Mol Vis 2011;17:1745-1758. 60. Yan X, Tezel G, Wax MB, Edward DP. Matrix metalloproteinases and tumor necrosis factor alpha in glaucomatous optic nerve head. Arch Ophthalmol 2000;118:666-673. 61. Vos CM, Sjulson L, Nath A, et al. Cytotoxicity by matrix metalloprotease-1 in organotypic spinal cord and dissociated neuronal cultures. Exp Neurol 2000;163:324-330. 62. Johnson EC, Jia L, Cepurna WO, Doser TA, Morrison JC. Global Changes in Optic Nerve Head Gene Expression after Exposure to Elevated Intraocular Pressure in a Rat Glaucoma Model. Investigative Ophthalmology & Visual Science 2007;48:3161-3177. 63. Hughes PM, Wells GM, Perry VH, Brown MC, Miller KM. Comparison of matrix metalloproteinase expression during Wallerian degeneration in the central and peripheral nervous systems. Neuroscience 2002;113:273-287. 64. Bull ND, Martin KR. Optic nerve restoration: new perspectives. J Glaucoma 2007;16:506-511. 65. Yang P, Yang Z. Enhancing intrinsic growth capacity promotes adult CNS regeneration. Journal of the Neurological Sciences 2012;312:1-6. 66. Goldberg JL, Barres BA. The Relationship between Neuronal Survival and Regeneration. Annual Review of Neuroscience 2000;23:579-612. 67. Ahmed Z, Dent RG, Leadbeater WE, Smith C, Berry M, Logan A. Matrix metalloproteases: degradation of the inhibitory environment of the transected optic nerve and the scar by regenerating axons. Mol Cell Neurosci 2005;28:64-78. 68. Pizzi MA, Crowe MJ. Matrix metalloproteinases and proteoglycans in axonal regeneration. Exp Neurol 2007;204:496-511. Epub 2006 Dec 2020. 69. Muir EM, Adcock KH, Morgenstern DA, et al. Matrix metalloproteases and their inhibitors are produced by overlapping populations of activated astrocytes. Molecular Brain Research 2002;100:103-117. 70. Cua RC, Lau LW, Keough MB, Midha R, Apte SS, Yong VW. Overcoming neuriteinhibitory chondroitin sulfate proteoglycans in the astrocyte matrix. Glia 2013;NA. 71. Ferguson TA, Muir D. MMP-2 and MMP-9 increase the neurite-promoting potential of schwann cell basal laminae and are upregulated in degenerated nerve. Mol Cell Neurosci 2000;16:157-167. 72. Chantry A, Gregson N, Glynn P. Degradation of myelin basic protein by a membraneassociated metalloprotease: neural distribution of the enzyme. Neurochem Res 1992;17:861867. 73. Gijbels K, Proost P, Masure S, Carton H, Billiau A, Opdenakker G. Gelatinase B is present in the cerebrospinal fluid during experimental autoimmune encephalomyelitis and cleaves myelin basic protein. J Neurosci Res 1993;36:432-440. 74. Zuo J, Ferguson TA, Hernandez YJ, Stetler-Stevenson WG, Muir D. Neuronal matrix metalloproteinase-2 degrades and inactivates a neurite-inhibiting chondroitin sulfate proteoglycan. J Neurosci 1998;18:5203-5211. 75. Murphy G, Gavrilovic J. Proteolysis and cell migration: creating a path? Curr Opin Cell Biol 1999;11:614-621. 76. Duchossoy Y, Arnaud S, Feldblum S. Matrix metalloproteinases: potential therapeutic target in spinal cord injury. Clin Chem Lab Med 2001;39:362-367. 77. Demestre M, Wells GM, Miller KM, et al. Characterisation of matrix metalloproteinases and the effects of a broad-spectrum inhibitor (BB-1101) in peripheral nerve regeneration. Neuroscience 2004;124:767-779. 78. Charalambous P, Hurst LA, Thanos S. Engrafted chicken neural tube-derived stem cells support the innate propensity for axonal regeneration within the rat optic nerve. Invest Ophthalmol Vis Sci 2008;49:3513-3524. 79. Pastrana E, Moreno-Flores MT, Gurzov EN, Avila J, Wandosell F, Diaz-Nido J. 24 Genes associated with adult axon regeneration promoted by olfactory ensheathing cells: a new role for matrix metalloproteinase 2. J Neurosci 2006;26:5347-5359. 80. Gaublomme D, Buyens T, De Groef L, et al. Matrix metalloproteinase 2 and membrane-type 1 matrix metalloproteinase co-regulate axonal outgrowth of mouse retinal ganglion cells. J Neurochem 2013;(in revision). 81. Ahmed Z, Aslam M, Lorber B, Suggate EL, Berry M, Logan A. Optic nerve and vitreal inflammation are both RGC neuroprotective but only the latter is RGC axogenic. Neurobiol Dis 2010;37:441-454. 82. Kurimoto T, Yin Y, Omura K, et al. Long-distance axon regeneration in the mature optic nerve: contributions of oncomodulin, cAMP, and pten gene deletion. J Neurosci 2010;30:15654-15663. 83. Lorber B, Berry M, Douglas MR, Nakazawa T, Logan A. Activated retinal glia promote neurite outgrowth of retinal ganglion cells via apolipoprotein E. J Neurosci Res 2009;87:2645-2652. 84. Lorber B, Guidi A, Fawcett JW, Martin KR. Activated retinal glia mediated axon regeneration in experimental glaucoma. Neurobiol Dis 2012;45:243-252. 85. Yin Y, Cui Q, Gilbert HY, et al. Oncomodulin links inflammation to optic nerve regeneration. Proc Natl Acad Sci U S A 2009;106:19587-19592. 86. Jiang C, Klassen H, Zhang X, Young M. Laser injury promotes migration and integration of retinal progenitor cells into host retina. Mol Vis 2010;16:983-990. 87. Johnson TV, Bull ND, Martin KR. Identification of barriers to retinal engraftment of transplanted stem cells. Invest Ophthalmol Vis Sci 2010;51:960-970. 88. Kinouchi R, Takeda M, Yang L, et al. Robust neural integration from retinal transplants in mice deficient in GFAP and vimentin. Nat Neurosci 2003;6:863-868. 89. Tucker B, Klassen H, Yang L, Chen DF, Young MJ. Elevated MMP Expression in the MRL Mouse Retina Creates a Permissive Environment for Retinal Regeneration. Invest Ophthalmol Vis Sci 2008;49:1686-1695. 90. Suzuki T, Mandai M, Akimoto M, Yoshimura N, Takahashi M. The simultaneous treatment of MMP-2 stimulants in retinal transplantation enhances grafted cell migration into the host retina. Stem Cells 2006;24:2406-2411. 91. Tucker BA, Redenti SM, Jiang C, et al. The use of progenitor cell/biodegradable MMP2-PLGA polymer constructs to enhance cellular integration and retinal repopulation. Biomaterials 2009;31:9-19. 92. Yao J, Tucker BA, Zhang X, Checa-Casalengua P, Herrero-Vanrell R, Young MJ. Robust cell integration from co-transplantation of biodegradable MMP2-PLGA microspheres with retinal progenitor cells. Biomaterials 2011;32:1041-1050. 93. Zhang Y, Klassen HJ, Tucker BA, Perez MT, Young MJ. CNS progenitor cells promote a permissive environment for neurite outgrowth via a matrix metalloproteinase-2dependent mechanism. J Neurosci 2007;27:4499-4506. 94. Bartsch U, Oriyakhel W, Kenna PF, et al. Retinal cells integrate into the outer nuclear layer and differentiate into mature photoreceptors after subretinal transplantation into adult mice. Exp Eye Res 2008;86:691-700. 95. Klassen H, Kiilgaard JF, Zahir T, et al. Progenitor cells from the porcine neural retina express photoreceptor markers after transplantation to the subretinal space of allorecipients. Stem Cells 2007;25:1222-1230. 96. Lamba DA, Gust J, Reh TA. Transplantation of human embryonic stem cell-derived photoreceptors restores some visual function in Crx-deficient mice. Cell Stem Cell 2009;4:7379. 97. MacLaren RE, Pearson RA, MacNeil A, et al. Retinal repair by transplantation of photoreceptor precursors. Nature 2006;444:203-207. 25 98. Gonzalez-Cordero A, West EL, Pearson RA, et al. Photoreceptor precursors derived from three-dimensional embryonic stem cell cultures integrate and mature within adult degenerate retina. Nat Biotech 2013;31:741-747. 99. Bull ND, Irvine KA, Franklin RJ, Martin KR. Transplanted oligodendrocyte precursor cells reduce neurodegeneration in a model of glaucoma. Invest Ophthalmol Vis Sci 2009;50:4244-4253. 100. Bull ND, Limb GA, Martin KR. Human Muller stem cell (MIO-M1) transplantation in a rat model of glaucoma: survival, differentiation, and integration. Invest Ophthalmol Vis Sci 2008;49:3449-3456. 101. Morrison CJ, Butler GS, RodrÃ-guez D, Overall CM. Matrix metalloproteinase proteomics: substrates, targets, and therapy. Current Opinion in Cell Biology 2009;21:645653. 26 Figures Figure 1. 27 Figure 2. 28 Figure 3. 29 Legends to figures Figure 1. Schematic representation of known MMP and TIMP activities in the glaucomatous retina. Proposed MMP-9 working mechanisms (depicted in blue): Various insults, including elevated IOP and ischemia, result in the elevation of retinal glutamate levels and stimulate the production of IL-1 by astrocytes, inducing an upregulation of MMP-9 synthesis in astrocytes and/or RGCs. In addition, IL-1 also increases the production of nitric oxide, which can activate extracellular pro-MMP-9. Finally, MMP-9 expression increases as elevated IOP results in a diminished deposition of TGF-β2, a known MMP inhibitor, in the ECM. This increased MMP-9 activity in the RGC layer abrogates laminin-integrin signalling, mediated by FAK, PI3K and PKB kinases, resulting in decreased expression of the anti-apoptotic protein Bcl-xL and detachment-induced apoptosis of RGCs. Proposed TIMP-1 working mechanisms (depicted in red): Ocular hypertension-induced elevation of MMP-9 activity in the RGC layer, is accompanied by elevated TIMP-1 expression in RGCs. This TIMP-1 elevation is likely to act in a dual way: first of all, TIMP-1 will inhibit MMP-9 and as such keep pro-apoptotic MMP-9 activity within limits, second, TIMP-1 might also promote RGC survival by directly suppressing pro-apoptosis signalling in an MMP-independent manner. NFL: nerve fiber layer, GCL: ganglion cell layer; IPL: inner plexiform layer, INL: inner nuclear layer; OPL: outer plexiform layer, ONL: outer nuclear layer, PRL: photoreceptor layer, FAK: focal adhesion kinase, PI3K: phosphatidylinositide 3-kinase, PIP2: phosphatidylinositol 4,5-bisphosphate; PIP3: phosphatidylinositol 3,4,5-triphosphate; PKB: protein kinase B, Bcl-xL: B-cell lymphoma-extra large; NO: nitric oxide; IL-1: interleukin-1; 30 TGFβ2: transforming growth factor-β2. 31 Figure 2. Schematic representation of suggested MMP and TIMP activities in the glaucomatous optic nerve. In response to the mechanical stress generated by elevated IOP, lamina cribrosa cells and astrocytes increase their secretion of TGF-β1 and TNF-α, which act in an auto- or paracrine manner to induce MMP-2 expression and ECM remodeling in the optic nerve head (1). Moreover, astrocytes also express MMP-1 and MT1-MMP while undergoing a transition from a quiescent to a reactive phenotype. This transition involves detachment from the basement membrane and relocation throughout the axon bundles, processes which are both facilitated via proteolysis of the ECM and cell surface adhesion molecules by MMP-1 and MT1-MMP (2). If not counterbalanced by TIMP-1, expressed in RGC axons and astrocytes, MMP-1 will continue to degrade the ECM, resulting in a lamina cribrosa extracellular environment that is no longer able to support axonal/neuronal survival (3). 32 Figure 3. Schematic representation of suggested MMP and TIMP activities in the regenerating optic nerve. MMP-2, -9, and to a lesser extent MMP-1 and -3, are upregulated at the site of injury and in the proximal stump of the optic nerve, presumably by (an) unknown factor(s), released by the numerous collateral axonal sprouts that stimulate astrocytes to increase their MMP expression. Initially, MMP-2 and -9 contribute to the removal of tissue debris during early post-injury inflammation (1). Later on during the recovery phase, a well-balanced MMP activity might promote axonal regeneration via degradation of glial scar-inhibitory ligands, such as CSPGs (2); via degradation of myelin-derived inhibitory ligands, such as Nogo, MAG, OMgp and MBP (3); via unmasking, release and/or activation of growth-promoting molecules such as bFGF, pro-NFG and pro-BDNF (4); and/or via focalized ECM proteolysis at the growth cones of regenerating axons (5). 33 Legends to tables Table 1. MMP expression and activity in the healthy versus glaucomatous retina. This table provides an overview of reported MMP expression/activity in the healthy and glaucomatous retina, reported from in vivo studies, with corresponding references. Expression data in human patients and data obtained in animal models of glaucoma are categorized under different subheadings, with the latter being subdivided according to the type of initial insult leading to the glaucomatous retinal damage. Of note, optic nerve ligation has been grouped under the subheading ‘ischemia-induced animal models for glaucoma’, however, as not only the ophthalmic artery but also the optic nerve is ligated during this procedure, RGC degeneration in this model is likely due to a combination of ischemia and axonal compression. NFL: nerve fiber layer, OLM: outer limiting membrane, GCL: ganglion cell layer, IPL: inner plexiform layer, OPL: outer plexiform layer, INL: inner nuclear layer, IHC : immunohistochemistry, ISZ: in situ zymography, ISH: in situ hybridisation, WB: western blot, qRT-PCR: quantitative RT-PCR, POAG: primary open angle glaucoma. 34 Table 2. MMP expression and activity in the healthy versus glaucomatous optic nerve. This table provides an overview of MMP expression/activity in the healthy and glaucomatous optic nerve, reported from in vivo studies, with corresponding references. It illustrates the variety in species, glaucoma models and experimental details that have contributed to a very rich data set about MMP expression/activity, but that have also hampered a straightforward interpretation of these data due to conflicting outcomes. Expression data in human patients and data obtained in animal models of glaucoma are categorized under different subheadings. IHC : immunohistochemistry, ISH: in situ hybridisation, qRT-PCR: quantitative RT-PCR, POAG: primary open angle glaucoma, NTG: normal tension glaucoma. 35 Table 1. Expression/activity in the retina Species/glaucoma model Technique(s) Reference Human patients MMP-1 nuclear and plexiform layers human IHC 24 MMP-2 RGCs and their axons in the NFL human IHC 23 MMP-3 no detectable immunoreactivity human IHC 24 MMP-9 no detectable immunoreactivity human IHC 24 MT1-MMP photoreceptor outer segments human WB 25 TIMP-1 no detectable immunoreactivity human IHC 24 ► glaucoma: human (POAG) IHC 23 human IHC 24 rat (hypertonic saline episcleral vein injection) microarray, qRT-PCR 37 increased MMP-9 expression in apoptotic cells in GCL, correlating with the degree of IOP exposure rat (hypertonic saline episcleral vein injection) IHC 26 ► glaucoma: rat (hypertonic saline episcleral vein injection) microarray, qRT-PCR 38 GCL ► glaucoma: increased immunoreactivity, correlating with the degree of IOP exposure rat (hypertonic saline episcleral vein injection) IHC 26 ► glaucoma: increased TIMP-1 expression rat (hypertonic saline episcleral vein injection) qRT-PCR 32 ► glaucoma: increased TIMP-1 expression rat (hypertonic saline episcleral vein injection) microarray, qRT-PCR 37 ► glaucoma: increased TIMP-1 expression rat (hypertonic saline episcleral vein injection) microarray, qRT-PCR 38 WB, IHC 34 microarray, qRT-PCR 43 WB, IHC 34 WB 30 zymography 31 TIMP-2 RGC somata and axons, no immunoreactivity in astrocytes inner and outer nuclear layers Ocular hypertension-induced glaucoma models in rodents MMP-3 ► glaucoma: MMP-9 ► glaucoma: TIMP-1 increased MMP-3 expression decreased MMP-9 expression Optic nerve injury-induced glaucoma models in rodents MMP-2 ► glaucoma: MMP-2 expression remains unchanged rat (optic nerve transection) MMP-3 ► glaucoma: increased MMP-3 expression rat (optic nerve crush, optic nerve transection) MMP-9 ► glaucoma: increased MMP-9 expression in RGC layer rat (optic nerve transection) Ischemia-induced glaucoma models in rodents MMP-2 MMP-9 36 ► glaucoma: MMP-2 expression remains unchanged mouse (optic nerve ligation) ► glaucoma: increased pro-MMP-2 expression rat (ischemia-reperfusion injury) dot-like staining pattern in GCL ► glaucoma: increased eGFP+ area and intensity mouse (optic nerve ligation) MMP-9-eGFP reporter mice 27 ► glaucoma: increased MMP-9 expression in RGCs mouse (ischemiareperfusion injury) IHC, ISZ 28 ► glaucoma: increased MMP-9 expression in reactive astrocytes mouse (optic nerve ligation) WB, IHC 29, 30, 33 TIMP-1 TIMP-2 ► glaucoma: increased pro-MMP-9 expression in interphotoreceptormatrix rat (ischemia-reperfusion injury) zymography, IHC 31 ► glaucoma: TIMP-1 expression remains unchanged rat (ischemia-reperfusion injury) reverse zymography 31 ► glaucoma: TIMP-1 expression remains unchanged mouse (optic nerve ligation) WB 33 ► glaucoma: TIMP-2 expression remains unchanged mouse (optic nerve ligation) WB 33 ► glaucoma: TIMP-2 expression remains unchanged rat (ischemia-reperfusion injury) reverse zymography 31 rat (intravitreal NMDA injection) zymography 32 RGCs, Müller glia, astrocytes ► glaucoma: slightly increased MMP-2 protein levels measured via WB, yet no change in activity levels measured via zymography mouse (intravitreal KA injection) WB, zymography, IHC 33 ► glaucoma: rat (intravitreal NMDA injection) zymography, ISZ 32 Excitotoxicity-induced glaucoma models in rodents MMP-2 MMP-9 ► glaucoma: MMP-2 activity remains unchanged increased in expression of pro- and active MMP-9 in RGCs Miscellaneous RGCs and their axons in the NFL monkey IHC 22 photoreceptor inner and outer segments; weak immunoreactivity in OLM horse IHC 36 MMP-9 GCL, IPL and photoreceptor segments horse IHC 36 MT1-MMP photoreceptor inner segments horse IHC 36 NFL mouse (P0) ISH 50 inner retinal layer rabbit IHC 51 TIMP-1 RGC somata and axons in NFL, no immunoreactivity in astrocytes in NFL monkey IHC, ISZ 22 TIMP-2 photoreceptor inner and outer segments horse IHC 36 MMP-2 37 Table 2. Expression/activity in the optic nerve Species/glaucoma model Technique(s) Reference Human patients cytoplasm of few glial cells; faint staining of glial processes around axons and in pial septae ► glaucoma: increased number of MMP-1+ glial cells human (PAOG, NTG) IHC 60 few astrocytes ► glaucoma: increased immunoreactivity in astrocytes and ECM in cribriform plates; axons; small vessels and pial septae human (POAG) IHC 23 few glial cells; faint staining of glial processes around axons increased intensity of immunostaining and number of MMP-2+ cells; increased intensity of immunostaining of glial processes around axons and along pial blood vessels ► intracytoplasmatic immunostaining of glial cells is more intense in areas with preserved axons human (POAG, NTG) IHC 60 astrocytes; axons, higher immunoreactivity in unmyelinated (pre)laminar regions than in myelinated postlaminar region ► glaucoma: MMP-2 expression remains unchanged human (POAG) IHC 23 few glial cells; faint staining of glial processes around axons ► glaucoma: increased immunoreactivity in astroglial cells, glial processes around axons and along pial septae ► immunoreactivity is more intense in areas with preserved axons human (POAG, NTG) IHC 60 perivascular cells human (POAG) IHC 23 MMP-7 no detectable immunoreactivity human (POAG) IHC 23 MMP-9 no detectable immunoreactivity human (POAG) IHC 23 MMP-12 no detectable immunoreactivity human (POAG) IHC 23 MT1-MMP few astrocytes; granular immunostaining associated with blood vessels; no immunoreactivity detected in axons or ECM ► glaucoma: increased immunoreactivity in astrocytes human (POAG) IHC 23 TIMP-1 astrocytes and axons ► glaucoma: TIMP-1 expression remains unchanged human (POAG) IHC 23 TIMP-2 astrocytes and axons ► glaucoma: TIMP-2 expression remains unchanged human (POAG) IHC 23 MMP-1 MMP-2 ► glaucoma: MMP-3 Ocular hypertension-induced glaucoma models in monkey MMP-1 few astrocytes; small blood vessels ► glaucoma: increased immunoreactivity in reactive astrocytes and ECM; many quiescent astrocytes in myelinated nerve express mRNA monkey (laser scarification of trabecular meshwork) ISH, IHC 22 MMP-2 few astrocytes; axons ► glaucoma: decreased MMP-2 immunoreactivity in nerve bundles due to loss of axons; MMP-2 expression in astrocytes remains unchanged monkey (laser scarification of trabecular meshwork) ISH, IHC 22 MMP-3 small bloodvessels monkey (laser scarification of trabecular meshwork) IHC 22 MMP-9 some oligodendrocytes in the nerve bundles in the myelinated nerve ► glaucoma: MMP-9 expression remains unchanged monkey (laser scarification of trabecular meshwork) IHC 22 MT1-MMP low immunoreactivity/mRNA in few astrocytes and around small blood vessels ► glaucoma: increased immunoreactivity/mRNA in reactive astrocytes monkey (laser scarification of trabecular meshwork) ISH, IHC 22 TIMP-1 astrocytes and axons ► glaucoma: decreased immunoreactivity due to loss of axons monkey (laser scarification of trabecular meshwork) ISH, IHC 22 TIMP-2 astrocytes and axons ► glaucoma: decreased immunoreactivity due to loss of axons monkey (laser scarification of trabecular meshwork) ISH, IHC 22 38 Ocular hypertension- and axonal injury-induced glaucoma models in rodents MMP-2 MMP-3 ► glaucoma: increased MMP-2 expression rat (hypertonic saline episcleral vein injection) microarray, qRT-PCR 62 ► glaucoma: MMP-2 expression remains unchanged rat (optic nerve crush) qRT-PCR, zymography 63 ► glaucoma: increased MMP-3 expression, primarily associated with GFAP+ rat (optic nerve crush) qRT-PCR, IHC 63 increased MMP-7 expression, primarily associated with GFAP+ rat (optic nerve crush) qRT-PCR, IHC 63 increased pro-MMP-9 expression, primarily associated with GFAP+ rat (optic nerve crush) qRT-PCR, IHC, zymography 63 increased MMP-12 expression, primarily associated with GFAP+ rat (optic nerve crush) qRT-PCR, IHC 63 increased TIMP-1 expression rat (hypertonic saline episcleral vein injection, optic nerve transection) microarray, qRT-PCR 62 astrocytes MMP-7 ► glaucoma: astrocytes MMP-9 ► glaucoma: astrocytes MMP-12 ► glaucoma: astrocytes TIMP-1 39 ► glaucoma: