Background information - Group B Strep Support
advertisement
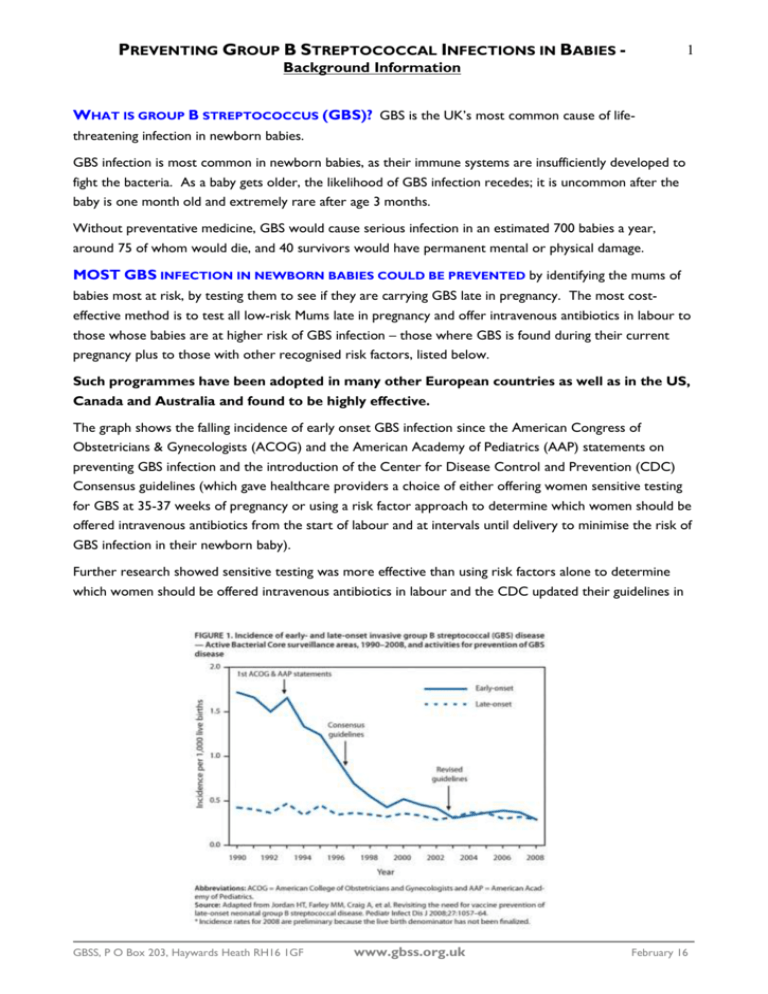
PREVENTING GROUP B STREPTOCOCCAL INFECTIONS IN BABIES - 1 Background Information WHAT IS GROUP B STREPTOCOCCUS (GBS)? GBS is the UK’s most common cause of lifethreatening infection in newborn babies. GBS infection is most common in newborn babies, as their immune systems are insufficiently developed to fight the bacteria. As a baby gets older, the likelihood of GBS infection recedes; it is uncommon after the baby is one month old and extremely rare after age 3 months. Without preventative medicine, GBS would cause serious infection in an estimated 700 babies a year, around 75 of whom would die, and 40 survivors would have permanent mental or physical damage. MOST GBS INFECTION IN NEWBORN BABIES COULD BE PREVENTED by identifying the mums of babies most at risk, by testing them to see if they are carrying GBS late in pregnancy. The most costeffective method is to test all low-risk Mums late in pregnancy and offer intravenous antibiotics in labour to those whose babies are at higher risk of GBS infection – those where GBS is found during their current pregnancy plus to those with other recognised risk factors, listed below. Such programmes have been adopted in many other European countries as well as in the US, Canada and Australia and found to be highly effective. The graph shows the falling incidence of early onset GBS infection since the American Congress of Obstetricians & Gynecologists (ACOG) and the American Academy of Pediatrics (AAP) statements on preventing GBS infection and the introduction of the Center for Disease Control and Prevention (CDC) Consensus guidelines (which gave healthcare providers a choice of either offering women sensitive testing for GBS at 35-37 weeks of pregnancy or using a risk factor approach to determine which women should be offered intravenous antibiotics from the start of labour and at intervals until delivery to minimise the risk of GBS infection in their newborn baby). Further research showed sensitive testing was more effective than using risk factors alone to determine which women should be offered intravenous antibiotics in labour and the CDC updated their guidelines in GBSS, P O Box 203, Haywards Heath RH16 1GF www.gbss.org.uk February 16 PREVENTING GROUP B STREPTOCOCCAL INFECTIONS IN BABIES - 2 Background Information 2002, recommending that all women should be offered sensitive testing. The also shows how the incidence fell further after the introduction of the CDC’s universal screening guideline (on graph as “revised guidelines”) and that this lower level has been maintained. WHAT IS THE CURRENT SITUATION IN THE UK? There is no national testing programme for GBS in the UK. Sensitive tests for diagnosing GBS carriage (Enriched Culture Method or ECM tests) are only available privately and from a handful of NHS hospitals, despite being the method recommended by the Health Protection Agency’s Bacteriology Standard Operating Procedure No 58 – Processing Swabs for Group B Streptococcal Carriage. Almost all testing for GBS carriage currently done on the NHS uses a method inferior to the ECM test, which misses up to 50% of the women carrying GBS when the swabs are taken, giving unacceptable levels of falsely negative results. Historically, the cost of an antenatal testing programme for all pregnant women in the UK was not seen as justifiable because the incidence if GBS infection in newborn babies born in the UK was relatively low compared for example in the USA, although the moral argument has always been persuasive. In November 2003, the Royal College of Obstetricians & Gynaecologists (RCOG) introduced guidelines directing clinicians to use a series of risk factors to determine which women should be offered antibiotics in labour to prevent early onset GBS infection in babies. Unfortunately, whilst maternity hospitals increasingly have policies on preventing GBS infection in babies, these vary considerably, which causes confusion. Moreover, most have a ‘reactive’ approach, only responding to actual infections or requests for advice – and you need to know about GBS to ask about it! As a result, many pregnant women never hear about GBS and consequently don’t know what preventative measures are available. Because of this inappropriately low level of concern, many health professionals working in maternity care are not fully informed themselves. This graph shows data from the Health Protection Agency and the voluntarily reported proven cases of GBS infection in babies up to age one week in England and Wales between 2000 and 2008. Clearly the RCOG guidelines have not been as effective as had been hoped and, since 2005, the incidence has been increasing and sadly, there is no reason to suppose this trend will have stopped in 2009. In the USA, the incidence per 1,000 live births has fallen from more than 1.5 during the early 1990s, to 0.28 in 2008 (a fall of 80%). Many other countries have seens similar falls in the incidence of GBS infection in their babies. Tragically, the incidence in the UK has been rising for some time and in 2008 reached 0.66 per 1,000 live births, more than twice the rate now seen in the USA. At what point will policy makers act to prevent these unnecessary deaths and disabilities? GBSS, P O Box 203, Haywards Heath RH16 1GF www.gbss.org.uk February 16 PREVENTING GROUP B STREPTOCOCCAL INFECTIONS IN BABIES - 3 Background Information Cost benefit studies of UK practice published in 2007 and 2010 have shown clearly that sensitive testing is more cost effective than using risk factors alone to determing which women should be offered antibiotics in labour. Moreover, the reducing costs of sensitive testing mean that this cost-effectiveness is increasing. Research estimates put the savings to the NHS and UK government at £37 million a year. Therefore GBSS considers that now is the time to introduce sensitive testing for all low-risk women late in their pregnancy, with intravenous antibiotics being offered in labour to all women whose babies are at higher risk of developing GBS infection. WHAT GROUP B STREP SUPPORT WANTS: All relevant health professionals to be fully informed about GBS and every pregnant Mum to be given clear and accurate information on GBS as a routine part of her antenatal care. Sensitive Enriched Culture Medium (ECM) testing for GBS colonisation (recognised as optimal by the Health Protection Agency and the Royal College of Obstetricians & Gynaecologists) to be freely available in the NHS, both on request by health professionals and pregnant Mums Every low-risk woman to be offered a sensitive test for GBS colonisation at 35-37 weeks of pregnancy free of charge (and, until these tests are freely available, all pregnant women should be told that these tests are available privately or directed to the GBSS website where they can find out about them). Every high-risk pregnant woman (those who have had a baby with GBS disease, those with GBS found in the urine during the current pregnancy and/or 2 or more of: GBS carriage, maternal fever in labour, preterm labour, preterm rupture of membranes, prolonged rupture of membranes) to be recommended to have intravenous antibiotics from the start of labour until delivery. Every higher-risk pregnant woman (those with only one of: GBS carriage or maternal fever in labour or preterm labour or preterm rupture of membranes or prolonged rupture of membranes) to be offered intravenous antibiotics from the start of labour until delivery. Research estimates this could prevent 80-90% of GBS infection in newborn babies in the UK. UNTIL SENSITIVE GBS TESTING IS ROUTINELY & FREELY AVAILABLE TO HEALTH PROFESSIONALS & PREGNANT WOMEN, GBSS WANTS: The Royal College of Obstetricians & Gynaecologists’ GBS guidelines to be fully implemented in all maternity units, and for policy and practice to be regularly audited against these guidelines. All pregnant women to be given information on the availability of the sensitive ECM test in their area, whether that’s in the NHS or privately. The ‘standard’ test currently used within the NHS not to be used to detect GBS carriage in pregnancy. LONGER TERM? Vaccination could prevent more cases of GBS infection than anything else, potentially preventing preterm labour and stillbirths caused by GBS infection, post-delivery GBS infection in the mother and late-onset GBS infection in the baby. Vaccination would avoid allergic reactions to antibiotics and concern about the emergence of antibiotic resistant bacteria. Moreover, there are no indications of hazard in this approach. However, a suitable vaccine candidate is not yet available –more research is GBSS, P O Box 203, Haywards Heath RH16 1GF www.gbss.org.uk February 16 PREVENTING GROUP B STREPTOCOCCAL INFECTIONS IN BABIES - 4 Background Information urgently needed to develop a safe and effective GBS vaccine. In the decade or so until an effective and safe vaccine is available, we should prevent preventable GBS infection in newborn babies using sensitive testing and risk factors – we must not just wait until we have a vaccine. Number of babies affected: Without preventative medicine, approximately 700 babies in the UK develop serious GBS infection each year (one in every 1,000 babies born), usually septicaemia, pneumonia and/or meningitis It’s estimated that around 75 babies die as a result of their GBS infection and 40 survive with long term problems (typically brain damage) At least 60 deaths and 400 serious GBS infections in babies aged up to 3 months could be prevented every year Group B Strep Support (GBSS) The UK charity Group B Strep Support (GBSS) was set up in 1996 with the objective of preventing preventable GBS infection in newborn babies. It has an active medical advisory panel, comprising recognised experts in their fields. UK GROUP B STREP PREVENTION – WHAT’S THE PROGRESS SO FAR? September 1996 The Group B Strep Support charity was founded, with the overall objective of preventing preventable GBS infection in newborn babies in the UK, supported by a medical advisory panel, comprising recognised experts in their fields. February 2000 A 13-month enhanced surveillance study of the incidence GBS infection in babies 0-90 days in the UK and Republic of Ireland started. The research established a minimum rate of culture-proven GBS infection in the UK of 0.7 per 1,000 babies born, and looked at the risk factors associated with these infections. June 2001 The Public Health Laboratory Service issued the UK’s first national recommendations on preventing GBS infection in newborn babies, describing them as Interim Good Practice Recommendations. May 2003 A sensitive enriched culture medium (ECM) test for GBS carriage is made available privately in the UK. The standard NHS test (a vaginal swab) only detects up to half of GBS carriers. Sensitive ECM tests are not available as a routine part of antenatal care, although they are available routinely in other countries. June 2003 UK research showed a much higher incidence of early-onset GBS infection (3.6 cases per 1,000 births) by looking at culture-proven and probable cases. “This estimate indicates a much greater disease burden in the UK than that suggested by figures of culture-proven sepsis, and lends support to the need for prevention strategies.” (Lancet. 2003 Jun 7;361(9373):1953-4. Estimated earlyGBSS, P O Box 203, Haywards Heath RH16 1GF www.gbss.org.uk February 16 PREVENTING GROUP B STREPTOCOCCAL INFECTIONS IN BABIES - 5 Background Information onset group B streptococcal neonatal disease. Luck S, Torny M, d'Agapeyeff K, Pitt A, Heath P, Breathnach A, Russell AB.) July 2003 David Cameron held an Adjournment Debate on GBS and has since 2003 tabled 3 EDMs - 254 MPs from all parties signed one or more of the EDMs (EDM 1211 in 2003, EDM 973 in 2004 and EDM 538 in 2005/6). October 2003 The National Institute for Clinical Excellence (NICE) issued “Antenatal Care – Routine care for healthy pregnant women” guidelines stating “pregnant women should be offered evidence based information and support to enable them to make informed decisions regarding their care … addressing women’s choices should be recognised as being integral to the decision making process.” Yet pregnant women aren’t routinely informed about GBS. The guideline doesn’t recommend testing for GBS, saying, “evidence of its clinical effectiveness and cost effectiveness remains uncertain.” All the currently available evidence clearly demonstrates the clinical effectiveness of testing pregnant women for GBS and offering intravenous antibiotics in labour to higherrisk women: this dramatically reduces GBS infections in newborn babies. The cost effectiveness issue has been addressed in a recent paper in the BMJ (see later). November 2003 The Royal College of Obstetricians & Gynaecologists (RCOG) issued their first guidelines for GBS prevention in newborn babies. GBSS endorsed these risk-based guidelines as, if implemented throughout the UK, they would prevent most fatal GBS infections in newborn babies. However, more GBS infection in newborn babies can be prevented by testing low-risk women using sensitive tests to detect GBS at 35-37 weeks of pregnancy and offering intravenous antibiotics in labour to those where GBS has been detected during the current pregnancy, plus to those with other recognised risk factors, than by using risk factors alone. November 2003 The National Screening Committee held a workshop on preventing GBS infection in newborn babies. This agreed the priority should be to ensure women at increased risk receive consistent advice and appropriate clinical management, and that a project group be established to keep prevention of GBS infection in newborn babies under review. May 2004 The National Screening Committee GBS Research Workshop established the key research priorities for preventing GBS infection in newborns – all experts at the meeting supported a randomised control trial to establish the relative effectiveness of a risk-based versus a testbased prevention strategy; and a cost/benefit modelling project. November 2004 A meeting with Health Minister, Dr Stephen Ladyman, was organised by David Cameron, at which families affected by GBS called on the Minister to introduce national testing. The Minister said that if it is achievable and workable, he will make sure it is made available. In the absence of reliable tests being freely available, he agreed the Royal College of Obstetricians & Gynaecologists’ riskbased guidelines should be implemented nationally and that pregnant women and their health professionals must be educated about GBS. August 2005 The Health Protection Agency issue their Bacteriology Standard Operating Procedure No 58 – Processing swabs for Group B Streptococcal Carriage describing the optimum method of detecting GBS carriage in pregnant women, which is not the standard method used in the vast majority of NHS hospitals. September 2005 The UK’s first Group B Strep Awareness Week was organised by Group B Strep Support. Volunteers around the country met health professionals, providing information packs containing materials on GBS for reading, distribution and display. Almost half of all the UK's maternity were visited and the rest received information packs by post. October 2005 A survey of 1000 pregnant women & new mothers found 9 out of 10 had never heard of GBS, only 2% had been informed about GBS at an 'antenatal class' and 3% 'by their GP'. Twothirds of these 'had no idea how dangerous GBS can be'. 100% said 'all pregnant women should be automatically told about GBS by their GP or midwife and be offered a free reliable test on the NHS during the last few weeks of pregnancy.’' (source: Pregnancy & birth magazine) GBSS, P O Box 203, Haywards Heath RH16 1GF www.gbss.org.uk February 16 PREVENTING GROUP B STREPTOCOCCAL INFECTIONS IN BABIES - 6 Background Information November 2005 David Cameron & GBSS delivered a petition of 5060 names to 10 Downing Street, asking the Government to ensure sensitive testing for GBS carriage is routinely & freely available for all pregnant women in the UK and that health professionals are fully informed about GBS so they can advise families in their care. May 2006 - The UK National Screening Committee launched their GBS online learning package. Based on the RCOG’s current UK guidelines, this was developed to raise awareness of GBS amongst health care professionals and provides a multidisciplinary interactive teaching resource. January 2007 The Royal College of Obstetricians & Gynaecologists’ Patient Information Leaflet on preventing GBS infection in newborn babies was finalised and made available from their website. February 2007 The Royal College of Obstetricians & Gynaecologists’ audit evaluating practice in UK obstetric units against the recommendations of their GBS guideline was published. The Audit showed that, even after 3 years, only a minority of units had protocols which were entirely consistent with the guidelines. Sept 2007 Two research projects commissioned in 2005 by the Health Technology Assessment (HTA) Programme reported. The BMJ reported on an economic modelling study that testing women for Group B Strep during pregnancy could save the Government £37million a year. The article stated that most GBS infection in newborn babies could be prevented by changing current practice and that the most cost-effective approach is treating all high risk groups. The best combination of clinical and cost effectiveness is treating all high risk groups and testing low risk mothers with the sensitive test. A proposal for a feasibility study of a large trial comparing testing with risk factor management to support decision making about a future trial was turned down by the HTA, which stated that in its current design the trial should not be commissioned. November 2007 The Health Protection Agency reported a 19.6% increase in the overall incidence of culture-proven, voluntarily-reported GBS infections in babies in England, Wales & Northern Ireland aged 0-90 days to 0.61 per 1000 live births in 2006 from 0.51 in 2005. The increase in the preventable early-onset GBS infections was 19.4% in the same period (Health Protection Report Vol 1 No 46 Bacteraemia Routine Data Reports Pyogenic and non-pyogenic streptococcal bacteraemia, England, Wales and Northern Ireland: 2006). December 2007 The UK’s second Group B Strep Awareness Week was sponsored by Group B Strep Support - all maternity units throughout the country were sent up to date information materials for both at health professionals and at expectant parents. There were lots of fundraising and media appearances, including in The Mirror and many local and regional newspapers. January 2008 With Pregnancy & birth magazine, Group B Strep Support submitted a petition of 11,340 names to the Prime Minister asking that all women are provided with information about GBS and offered a sensitive test for GBS as a routine part of their antenatal care. Nicholas Soames MP, together with a number of other MPs from England, Wales and Northern Ireland, including Jeffrey Donaldson, Nia Griffith, Philip Hollobone and Theresa May, escorted a delegation of parents and supporters to present the petition. February 2008 Jeffrey Donaldson MP MLA & Alasdair McDonnell MP MLA jointly hosted an event to raise awareness of GBS and to campaign to save babies lives by making sensitive testing for GBS available to pregnant women on the NHS in Northern Ireland. Representatives of Group B Strep Support and its medical advisory panel addressed an audience of MPs, MLAs, health professionals and families affected, GBS providing information about measures which can be taken which will prevent most of these infections in newborn babies. March 2008 The review of the National Institute of Clinical Excellence’s Antenatal Care guidelines was published. Hugely disappointingly, there was no review of the sections relating to GBS, despite this being suggested by a variety of clinicians, health professionals’ organisations and by GBSS. This guideline is not due for review until March 2010. GBSS, P O Box 203, Haywards Heath RH16 1GF www.gbss.org.uk February 16 PREVENTING GROUP B STREPTOCOCCAL INFECTIONS IN BABIES - 7 Background Information March 2008 The Royal College of Obstetricians & Gynaecologists started its review of the Green Top Guideline on GBS issued in November 2003 (due for review November 2006). The review should be completed within approximately two years. April 2008 With Philip Hollobone MP, GBSS met with Dawn Primarolo, Minister of Public Health to discuss the issues around preventing GBS infection in newborn babies. May 2008 GBSS met with Dr Anne Mackie, the new Screening Programmes Director of the National Screening Committee to discuss the issues around preventing GBS infection in newborn babies. November 2008 The UK National Screening Committee held a workshop for stakeholders to consider the most recent evidence on testing pregnant women for carriage of group B Streptococcus. The outcome of the workshop will be made available through the NHS specialist screening library, and via GBSS’s website as soon as it’s available. November 2008 The Health Protection Agency reported a 27.1% increase in the overall incidence of culture-proven, voluntarily-reported GBS infections in babies in England, Wales & Northern Ireland aged 0-90 days to 0.61 per 1000 live births in 2007 from 0.48 in 2003. The increase in the preventable early-onset GBS infections was 15.6% in the same period (Health Protection Report Vol 2 No 47 Bacteraemia Routine Data Reports Pyogenic and non-pyogenic streptococcal bacteraemia, England, Wales and Northern Ireland: 2008). Spring 2009 On 11 March, a petition of almost 3200 names was submitted to the Prime Minister asking him to ensure all women are offered the chance to be tested for group B Strep during pregnancy. On 4 June 2009, the Government stated they would not offer routine screening for GBS to all pregnant women. Summer 2009 The National Screening Committee reviewed its policy on testing for group B Strep in pregnancy and decided against any change. November 2009 The Health Protection Agency reported a 51% increase in the incidence of culture-proven voluntarily-reported GBS infections in babies in England, Wales & Northern Ireland since the RCOG Guidelines were introduced in 2003. January 2010 GBSS met with Anne Milton MP, the Parliamentary Under Secretary of State for Public Health to discuss the issues around preventing GBS infection in newborn babies. Spring 2010 On 20 March, a petition of almost 1300 names was submitted to the Prime Minister asking him to ensure all women are offered the chance to be tested for group B Strep during pregnancy. In August, the Government confirmed they would not offer routine sensitive screening for GBS to all pregnant women. June 2010 The Health Protection Agency held a GBS Symposium in London, bringing together international experts in the subject of current advances in the diagnosis, management and treatment of neonatal group B streptococcal infections. GBSS attended and spoke at the meeting. November 2010 Incidence of preventable GBS infection in babies in the UK remains unchanged. The incidence of GBS infection in babies unchanged in 2009 - Data on how many group B Strep infections in newborn babies reported in 2009 in England and Wales were published in November 2010. The incidence has been rising – by over 28% between 2003 and 2008 for early-onset GBS infections. (http://www.hpa.org.uk/hpr/archives/2010/hpr4610.pdf) December 2010 More research shows a testing strategy is more cost effective than a risk factor strategy. Research suggests that the NHS could actually make significant cost savings by introducing ECM testing for all pregnant women at 35-37 weeks and offering antibiotics in labour accordingly. The research was published in BJOG at http://www.ncbi.nlm.nih.gov/pubmed/21078057, and found that the risk factor approach currently used in the UK costs GBP50,000 per infection prevented, but GBSS, P O Box 203, Haywards Heath RH16 1GF www.gbss.org.uk February 16 PREVENTING GROUP B STREPTOCOCCAL INFECTIONS IN BABIES - 8 Background Information that this would fall to GBP45,000 if routine screening were introduced (screening is more efficient because it prevents more cases). This is a purely financial advantage, without taking into account the savings from fewer babies needing intensive care, and without considering the distress to parents who lose their baby when this could easily have been prevented. August 2011 e-petition for better prevention of group B Strep infections in babies started. GBSS is asking the Government to ensure sensitive testing for GBS carriage is routinely & freely available for all pregnant women in the UK and that health professionals are fully informed about GBS so they can advise families in their care. Petition due to close 15 August 2012, it currently has 15,000 signatures. September 2011 Northern Ireland Assembly Health Committee. Evidence session on Group B Streptococcus – the committee took evidence on GBS from Group B Strep Support and thanked them for attending. Minutes at http://www.niassembly.gov.uk/Assembly-Business/Committees/HealthSocial-Services-and-Public-Safety/Minutes/14-September-2011/ December 2011 Nothern Ireland Assembly Health Committee. Following up on the meeting in September, the Committee noted correspondence from Group B Strep Support and agreed to write to the Department about the issues raised. The Committee also agreed to hold a further evidence session with departmental officials on Group B Streptococcus. December 2011 A poll held by ComRes found that while 54% of the women aged between 2035 surveyed had heard of group B Strep, only 20% knew what it was. 92% of those surveyed believe that information on group B Strep should be given to all pregnant women and would welcome the opportunity for pregnant women to be screened for group B Strep in the later stages of pregnancy and believe this should be offered to women routinely. 95% believe antibiotics should be offered in labour to women with group B Strep and that they themselves would definitely or probably accept the offer (89%) January 2012 Jane Plumb, joint founder of GBSS was awarded an MBE for services to Child Healthcare in the 2012 New Year Honours List in recognition of her work to prevent group B Streptococcal infection in newborn babies. May 2012 Mark Durkan MP and Mike Hancock MP tabled individual Early Day Motions ((EDMs) are formal motions submitted by MPs for debate in the House of Commons. However, very few are actually debated. EDMs allow MPs to draw attention to an event or cause and they register their support by signing individual motions.) June 2012 Thursday 28th June, in the House of Commons a new report into infant death and disability caused by group B Streptococcus (GBS) infection was launched. The reception was hosted by Alison Seabeck MP and heard from Professor Philip Steer, Emeritus Professor at Imperial College, consultant obstetrician at the Chelsea and Westminster Hospital & Chair of the GBSS Medical Advisory Panel, Charlotte Cheshire, whose son Adam suffered from GBS infection and Jane Plumb MBE, Chief Executive of GBSS, who prepared the new report .July 2012 On 2nd July 2012, Novartis Vaccines hosted a daylong meeting about developing a vaccine against group B Strep infection. Still in the development phase, a safe and reliable vaccine when available will revolutionise GBS prevention. Gina Burns from the US Group B Strep Association and Chief Executive of GBSS, Jane Plumb MBE chaired a group called GBS Public Awareness, Advocacy. October 2012 The UK National Screening Committee opened a public consultation on routine screening for group B Strep. The consultation closed on the 23rd October. GBSS raised awareness of the consultation and encouraged responses from the public and health professionals. December 2012 The UK National Screening Committee decided to not introduce routine screening for group B Strep. GBSS was very disappointed by the decision, especially the fact that to date the NSC has failed to respond to any of the questions raised in the comments on the public consultation. GBSS, P O Box 203, Haywards Heath RH16 1GF www.gbss.org.uk February 16 PREVENTING GROUP B STREPTOCOCCAL INFECTIONS IN BABIES - 9 Background Information GBSS, P O Box 203, Haywards Heath RH16 1GF www.gbss.org.uk February 16