Appendix Qualitative evaluation of barriers and facilitators for hand
advertisement
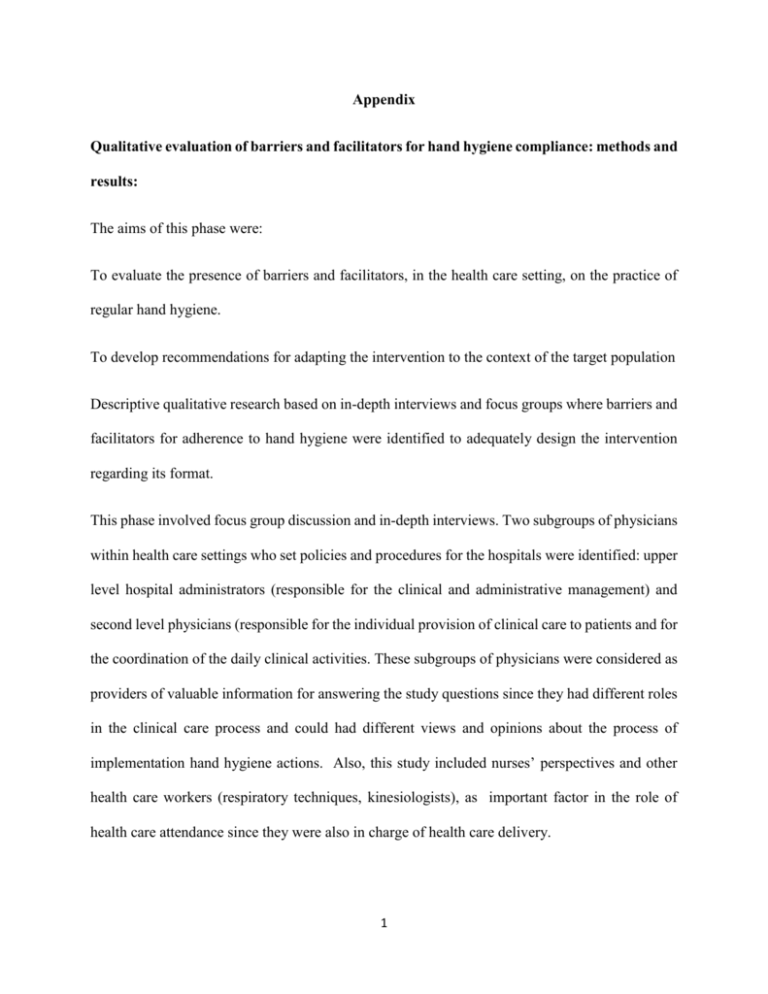
Appendix Qualitative evaluation of barriers and facilitators for hand hygiene compliance: methods and results: The aims of this phase were: To evaluate the presence of barriers and facilitators, in the health care setting, on the practice of regular hand hygiene. To develop recommendations for adapting the intervention to the context of the target population Descriptive qualitative research based on in-depth interviews and focus groups where barriers and facilitators for adherence to hand hygiene were identified to adequately design the intervention regarding its format. This phase involved focus group discussion and in-depth interviews. Two subgroups of physicians within health care settings who set policies and procedures for the hospitals were identified: upper level hospital administrators (responsible for the clinical and administrative management) and second level physicians (responsible for the individual provision of clinical care to patients and for the coordination of the daily clinical activities. These subgroups of physicians were considered as providers of valuable information for answering the study questions since they had different roles in the clinical care process and could had different views and opinions about the process of implementation hand hygiene actions. Also, this study included nurses’ perspectives and other health care workers (respiratory techniques, kinesiologists), as important factor in the role of health care attendance since they were also in charge of health care delivery. 1 Participants from the eleven sites were invited to participate. They were contacted by letter and by phone to explain the aim of the activity and confidentiality aspects. Once they accepted to participate, they signed an informed consent were they could read the aim again and confirm the ethical and confidentiality aspects that were considered. Focus Groups and in depth interviews Focus groups Four focus groups with intensive care units healthcare workers (26 nurses or technical personnel and 12 physicians). Two focus groups included only physicians and the others two groups included nurses and technical personnel. The physician groups involved a total of 12 (one group of 7 and one group of 5 ) including 9 of the 11 sites and the non-physicians groups involved 26 participants from 10 of the 11 sites. The groups of physicians were explored separately from others health care workers assuming that different perspective of medical activities, roles and authorities could bias the answers of participants. The focus groups lasted one and a half hours and they were deployed in a selected place not related to any of the sites included. A trained moderator (one at the time) covered a series of questions using a pre-established discussion guide. In addition to the facilitator, one recorder also attended each group to take notes on participants’ comments, any unspoken language and group dynamics. Focus groups were audio taped and transcribed. The main topics to discuss were: Concepts and symbolic aspects of hand hygiene Self-referencing 2 Reflection about himself and the other Hospital Policy The everyday process of care Skin Care Preferences about hand hygiene products Gloves wearing No compensation was offered for participating. Snacks and refreshments were provided to facilitate a comfortable environment. In depth interviews A trained interviewer (a social scientist) conducted eight in-depth interviews with to infection control practitioners, hospitals directors, intensive care units chiefs and other healthcare worker from eight of the eleven sites. The aim of the in-depth interviews was the same as for the focus group, but they were seeking for individual opinions with physicians and nurses. All interviewees were asked to provide informed consent. A semi-structured topic guide was used, beginning with general open-ended questions and gradually moving to more detailed focused questions. Interviews were audio taped for subsequent transcription. Qualitative data analysis followed the following steps: 3 1) Reviewing of the material to identify items and wording to produce a coding system by two different coding systems one for interviews and one for focus groups; 2) Qualitative data analysis software (Ethnograph) was used to code the transcripts; 3) After displaying and reducing the coded data the information was organized looking for shared and contrasting meanings, emerging patterns, differences and similarities, connections between attitudes/opinions and pre-existing knowledge; 4) Global interpretation of the material. Identifying emergent themes A social Scientist read the transcripts to identify emergent themes associated with each focus group question and draft written definitions of each theme. Two social scientists coded text segments independently using those emergent themes definitions and identifying new possible categories for comments that do not fit the existing ones. The coding triangulation assured the analysis reliability. After the first transcript of one target group was coded, social scientist discussed and resolved problems related to the use of established coding categories and decided on the relevance of emergent categories. During these discussions, social scientist decided the categories and the coding system. If the decision was made to alter any coding category, both social scientist reviewed their work and, if necessary, recoded the relevant sections of text. Coding procedures 4 Data codes were developed using a grounded theory-based approach to identify emergent themes, a “constant comparison” strategy to ensure internal consistency. A second social scientist reviewed what was already coded in order to confirm the first hand analysis. Data Analyses of Focus Groups A computer program –Ethnograph-, was used to analyze focus group transcript texts. This program allowed data analysts to code sections of text in more than one way and to compile selected portions that met search criteria without destroying the integrity of the original transcripts. These features enabled the different levels of analyses described below. Analytic Strategies Contextual factors. Descriptive statistics was used to characterize hospital characteristics and participant sociodemographic characteristics. Thematic analyses was used to characterize the context in which each session occurred, in-country conditions that could have affected the perspectives of hospital staff, and the social circumstances in which the group came together. Within-session analyses. Content and thematic analyses were conducted for each focus group session. Content analyses examined how often a topic had been mentioned, the emotional tone of member interactions, and how many members talked about a given topic. Thematic analyses were conducted to identify the types and range of participants’ focal concerns related to the research questions. As part of this analysis, direct quotations 5 was identified to be used in the report as representative examples of participants’ opinions. Cluster comparisons. In this stage, the findings from the within-session thematic analyses from all the administrator interviews and both sessions of the physicians’, nurses groups was compared to identify convergent and divergent responses to each question. Findings from this phase This phase showed the following barriers for compliance with hand hygiene 1) Unequal decision power between doctors and nurses 2) Segmented assistance process 3) Doctors overestimate complex practice and technology 4) To be unaware of being the carrier of microorganisms (knowledge) 5) To be overcrowded and feeling uncomfortable with reminding peers 6) The lack of an incentive or punishment result after complying with politics. The following facilitators were founded: 1) Institutional commitment with policy and leadership 2) Institutional empowerment to remind peers 3) To be aware of being the carrier of microorganisms (knowledge) 4) Team spirit and open institutional culture. 5) Data feedback and communication Seventy seven percent of the healthcare workers, mentioned that they had received some training about hand hygiene three years or less before the study. 6 Hand Hygiene Knowledge Questionnaire for Health-Care Workers results The aim of the application of this questionnaire was to identify those aspects less known about hand-hygiene among the health care workers in order to adapt the reminders and information to be reinforced by coordinator during the intervention. The questionnaire was done only for those health care workers that accepted to participate with an informed consent. This questionnaire was answered by 371/383 health care workers (97% response rate) from nine out of the eleven sites. The range of number of respondents per sites was 49 (14 to 63). Sixty eight percent of participants were nurses, 22% were physicians and 10% were other type of healthcare worker (technical personnel). Seventy seven percent of participants received some training about hand hygiene in the last three years and 98% utilize alcohol hand rub for hand hygiene. Adequate knowledge of appropriate hand hygiene practice was seen in 28.3% (Median: 64 points; maximum: 92; minimum: 32; SD: 9.7). No difference on adequate knowledge was found between physicians and nurses (p: 0.49). The domains that showed differences favoring nurse knowledge were related to transmission to patients, knowledge about hand rub/hand washing moments and elements to avoid for hand hygiene. Physicians showed a higher score in one of the questions related to transmission to personnel. A smaller proportion of adequate answers were observed in knowledge about reservoir. Sixty four percent of participants considered the environment more important than patient flora as a reservoir for transmission. 7