Gordon Robson GOGS
advertisement

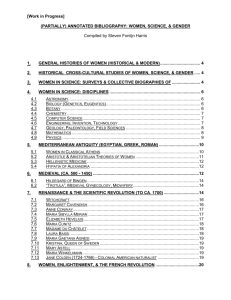
OGILVIE’S SYNDROME Abstract Ogilvie’s Syndrome characterizes the occurrence of acute colonic pseudo-obstruction with progressive dilatation of the colon without an evident mechanical cause.1,2 Of rare incidence, it has been reported in patients post caesarean section with complications of bowel perforation and ischaemia.2 Various medical and surgical conditions are associated with Ogilvie’s Syndrome. Over half of known cases are preceded by trauma or surgical procedure, most often caesarean section.1 Little is known about this condition, which poses diagnostic as well as therapeutic challenges in patients following Caesarean section. Therefore I describe a case of Ogilvie’s Syndrome following an elective repeat caesarean section necessitating emergency hemicolectomy to avoid colonic perforation, review cases of similar presentations in the literature, and discuss features of Ogilvie’s syndrome and its management. Introduction Ogilvie’s Syndrome describes acute massive colonic dilatation in the absence of any distinct cause of organic obstruction of the distal colon.1,2 Despite accurate descriptions since then, this Syndrome with mortality rates as high as 36-50% when complicated by bowel perforation remains hard to diagnose.3 Case Report A healthy non-smoker thirty year old para 2, with a past surgical history of two previous caesarean sections was admitted for an elective third repeat caesarean section. Her previous obstetric history included one emergency caesarean section for no progress at 8cm, followed by an elective caesarean section 3 years later. Her antenatal care in the third pregnancy was uneventful with no placental abnormalities demonstrated. The procedure was completed under spinal anaesthesia with findings of fibrotic rectus sheath with moderate adhesions between the sheath and anterior abdominal wall upon entry. There were no other features of concern. Neonate was delivered with good apgar scores. Her immediate post operative recovery was reasonable. Four days post operatively surgery she developed generalised abdominal pain associated with mild nausea and vomiting, becoming pyrexial at 38.1 degrees. Her abdomen was grossly distended with sluggish bowel sounds. The inflammatory markers were elevated. Plain abdominal X-ray showed generalised dilated loops of large bowel, followed by a CT scan demonstrating significant gaseous distension of transverse and ascending colon as well as caecum. Radiologically caecal dilatation was as high as 12 cm and had been commented on at being at risk of perforation whereby urgent laparotomy was undertaken by general surgeons. Right colon had ischaemic appearances and distension of caecum extended upto transverse colon. This was decompressed and a right hemicolectomy and primary end to end anastomosis was carried out. The patient made good post operative recovery subsequently. Histopathological investigation of resected bowel specimen showed thin atrophic necrotic caecal wall with patchy areas of ischaemia, mucosal ulceration and necrosis. Discussion Ogilvie’s syndrome, or acute colonic pseudo-obstruction, is a functional disorder characterised by massive dilatation of the colon in the absence of any mechanical obstruction,1 first described by Sir Heneage Ogilvie in 1948.2 Though exact data on prevalence is unknown,3 Ogilvie’s syndrome is relatively rare. It has also been reported as isolated case reports and small case series.2,3 The exact pathophysiology of Ogilvie’s syndrome is not completely understood, but it is believed to be due to an imbalance between sympathetic and parasympathetic colonic innervation, leading to massive dilatation of the colon.4 The causes for this imbalance are likely multifactorial, but can occur as a consequence of caesarean section (the most common cause), pregnancy (including following preterm labour, vaginal delivery and preeclampsia), sepsis, spinal trauma, and spinal, pelvic, cardiothoracic and abdominal surgery. In the case of Ogilvie’s syndrome following an obstetric or gynaecological event (such as caesarean section), it is thought that damage to the nerves of S2-4 lying close to the cervix, vagina and broad ligaments during the procedure may play a role, where the normal parasympathetic outflow from sacral segments S2-4 suffer disruption causing this functional obstruction where proximal and distal nerve supplies to the colon overlap.1 It has a clinical and radiological picture of acute large bowel obstruction without an obvious mechanical cause.2 Without appropriate treatment, it may lead to progressive colonic dilatation resulting in necrosis and perforation typically of the caecum with high mortality rates of 35% to 72%.1 Through searching the literature, 24 cases of Ogilvie’s syndrome following Caesarean section were identified, the characteristics of which are details in Table 1. Patient’s ages ranged from 21-47 years (mean= 33.1 years), with 6 patients having a multiple pregnancy (5 patients pregnant with twins, 1 with triplets). 5 patients experienced operative complications. Table 1: Characteristics of patients found on literature search Patient Patient Age Single/multiple Pregnancy Weeks Gestation at C/S Indication for C/S A 32 Single 37 Placenta previa + 2 previous C/Ss B 30 Single 39 Failure to progress C 28 Single 32 D 29 Single 37 Antepartum massive haemorrhage Breech, previous myomectomy E 40 Single 39 Severe pre-eclampsia + high multiparity F 40 Single 39 G 29 Multiple (twins) N/A Severe pre-eclampsia, previous C/S Breech presentation of first twin H 22 Multiple (triplets) 32 Pre-eclampsia, multiple pregnancy I 38 Single At term J 47 Multiple (twins) 29 (+6) weeks K 28 Single 39/40 L 35 Single 33 2 weeks past expected date of delivery Abruptio placentae M 26 Single Not recorded Elective C/S for narrow pelvis N 21 Single Not recorded Abruptio placentae O 41 Single Term P 42 Single Term Q 31 Multiple (twins) 25 (+6) weeks R 33 Single 40 Failure to progress S 28 Multiple (twins) 36 Atypical pre-eclampsia T 32 Single 41 Elective, for previous C/S U 39 Single 35 Obstructed labour V 29 Single 28 Breech presentation, low fetal size W 44 Multiple (twins) 35 Failure to progress (pregnancy induced due to pre-eclampsia) Suspected fetal distress Pre-eclampsia Emergency C/S for prolonged 2nd stage of pregnancy Elective C/S for narrow pelvis Fetal bradycardia in twin 2 Among the cases we reviewed, abdominal pain was the most common presenting symptom (83.3%, n=20) often being described as colicky and initially poorly localised, and distension (83.3%, n=20). Vomiting and constipation were frequently experienced. Nausea and tachypnoea have also been reported. Bowel sounds were frequently absent or sluggish, though occasionally hyperactive or high-pitched (“tinkling”), corresponding to what is stated in the literature.5 Pyrexia and peritonitic or shoulder-tip pain may indicated perforation, and patients may become acutely ill with dehydration and oliguria.5 While differential diagnoses include mechanical bowel obstruction, volvulus, 5 bowel perforation and peritonitis, the most difficult step is often distinguishing Ogilvie’s syndrome from paralytic ileus, a relatively frequent complication of abdominal surgery. There are, however, a number of key differences exist between the two: paralytic ileus often involves generalised impairment of the whole gut, while Ogilvie’s syndrome is specific to the colon Ogilvie’s syndrome often presents with hyperactive or high-pitched bowel sounds, while bowel sounds are usually absent in paralytic ileus patients with Ogilvie’s syndrome often continue to pass flatus and loose stool nausea and vomiting are more common in paralytic ileus The most important considerations when investigating possible Ogilvie’s syndrome are exclusion of mechanical obstruction and assessing for possible ischaemia or perforation. Abdominal x-ray is the most important diagnostic test and, in the case of Ogilvie’s syndrome, will reveal either pancolonic dilatation or segmented colonic dilatation. 1 Indeed colonic dilatation was observed on abdominal x-ray in 100% of patients found in the literatures. A caecal diameter greater than 9-12cm indicates a high risk of impending perforation. Air seen under the diaphragm suggests perforation. Water-soluble contrast enema can be used to rule out mechanical obstruction. Early detection is important, as it allows more conservative management and improves prognosis. Management is individualised depending on degree of bowel dilatation and risk of ischaemia and perforation. Of the patients identified in the literature, 8 (33.3%) were managed conservatively (including 1 patient requiring decompression via flexible sigmoidoscopy) while 16 (66.6%) required surgical intervention, ranging from tube caecostomy to right hemi-colectomy. Initial conservative management of Ogilvie’s syndrome may involve measures such as correcting any fluid or electrolyte imbalance, nasogastric suction, and avoiding any drugs which might impair colonic motility.5 Maintaining mobility, and avoiding keeping the patient in a supine where possible, can help. Pharmacological management often includes the use of the parasympathomimetic drugs increasing gastro-intestinal motility, neostigmine and cisapride.1 Surgical intervention is necessary when conservative methods fail, symptoms worsen, and/or caecal diameter exceeds 12 cm (which indicates impending perforation). Colonic decompression is often the first step in invasive treatment, though symptoms often recur and serial decompression may be necessary.5 Caecostomy may be the next procedure of choice, but failing these options, laparotomy will be mandatory, usually bowel resection with primary anastomosis or temporary diversion and 2nd stage closure.5 However, surgery is associated with a high mortality.1 This syndrome is serious because it is possible for the caecum to burst causing faecal peritonitis which carries a heavy mortality. OS is an established post-operative complication, but since it occurs rarely it may be overlooked or treated as an adynamic ileus because of the similarity in symptoms. The diagnosis is particularly difficult in puerperium since mild pyrexia, leucocytosis and some lower abdominal tenderness is generally present following CS. The hallmark symptom is development of marked abdominal distension over a short period of time and therefore a diagnostic abdominal X- ray should not be delayed even if the bowel sounds are normal.1 CONCLUSION This case highlights the need for a greater awareness, amongst obstetric practitioners, of this potentially lethal syndrome, since it may be successfully treated if identified early. 1 If a postoperative patient presents with features consistent with a bowel obstruction, prompt imaging should be performed in order to aid timely diagnosis.4 Reference 1) De M, Mandal A & Cooper JC; “A case of Ogilvie’s syndrome after caesarean section”; J Obstet Gynaecol (2002); 22:686-687 2) Ogilvie H; “Large intestine colic due to sympathetic deprivation. A new clinical syndrome”; BMJ (1948); 2:671-673 3) Srivastava G, Pilkington A, Nalla D, Polson Dw & Holt E; “Ogilvie’s syndrome: a case report”; Arch Gynecol Obstet (2007); 276:555-557 4) Rawlings C; “Management of postcaesarean Ogilvie’s syndrome and their subsequent outcomes; Aus and New Zeal J of Obstet and Gynaecol (2010); 50:573-581 5) Kakarla A, Posnett H, Jain A, George M & Ash A; “Acute colonic pseudo-obstruction after caesarean section”; The Obst and Gynecol (2006); 8:207-213