transfersomes based transdermal drug delivery
advertisement

TRANSFERSOMES BASED TRANSDERMAL DRUG DELIVERY: AN
OVERVIEW
Prasurjya Jyoti Sarmah 1*, Bhupen Kalita1, Anil Kumar Sharma2
1
Girijananda Chowdhury Institute of Pharmaceutical Science, Guwahati, Assam-781017.
2
Kemwell Biopharm Pvt. Ltd., Bangalore, Karnataka-560022.
Corresponding Author:
Prasurjya Jyoti Sarmah
Email: bblsarmah@gmail.com
Ph no. +91-88764-53189
INTRODUCTION:
Transdermal drug delivery systems can be described as topically administered medicaments
in the form of patches or semisolids, which can be applied to the intact skin to deliver the
drug through the skin at a controlled rate to the systemic circulation. Now a days , various
newer Transdermal Drug Delivery System (TDDS) have been developed , which can
considered to be helpful in rate controlled delivery of various drugs.Transdermal systems
have been designed to provide controlled continuous delivery of drugs via the skin to the
systemic circulation. Transdermal delivery can improve both therapeutic efficacy and safety
of drugs by more precisely, but it required spatial and temporal placement within the body to
reduce both the size and number of doses necessary to achieve the objective of systemic
medication through topical application to the intact skin surface. (1) .In the last two decades
transdermal controlled drug delivery system have been developed in order to avoid hepatic
first-pass effect and to improve drug bioavailability and to overcome the side-effects
associated with oral route. The transdermal route has become one of the most successful and
innovative focus for research in drug delivery, with around 40% of the drug candidate being
under clinical evaluation related to transdermal or dermal systems. The first transdermal
patch was approved in 1981 by FDA. (2)
ADVANTAGES OF TRANSDERMAL DRUG DELIVERY:
Transdermal drug delivery systems has the following advantages (3)
a. It provides constant blood level in the plasma for drugs with narrow therapeutics
index; as a result they minimize the risk of toxic effects. Transdermal drug delivery
system provides a steady infusion of a drug over an extended period of time.
b. It leads to improve patient compliance and reduced intra-patient variability
c. By avoiding hepatic first pass metabolism, it improves bioavailability.
d. It can be used for a long-term duration and can be utilized for drugs with a very short
half- life, narrow therapeutic window, and poor oral absorption.
e. It is preferable for unconscious patients as comparing to the oral route.
f. No interference with gastric and intestinal fluids.
g. Self-administration is possible and easy elimination of drug delivery in case of
toxicity.
The success of transdermal delivery system in Pharma market is evident as currently more
than 35 transdermal drug delivery products are approved in the USA for wide variety of
patho physiological conditions including hypertension, angina pectoris, motion sickness,
female menopause, male hypo-gonadism and approx 40% of drugs are under investigations to
validate the feasibility for transdermal drug delivery .The market share for transdermal
delivery was $12.7 billion in the year 2005 and is expected to increase to $31.5 billion in the
year 2015.
But the big hurdle in transdermal delivery of drug is the skin, the stratum corneum, & the
outermost envelop of the skin contributing to less permeability and lower systemic
availability. Recently, various strategies have been used to augment the transdermal delivery
of bioactive. Mainly, they include iontophoresis, electrophoresis, sonophoresis, chemical
permeation enhancers, micro needles, and vesicular system (liposomes, niosomes, elastic
liposomes such as ethosomes and transfersomes. (4)
TRANSFEROSOMES:
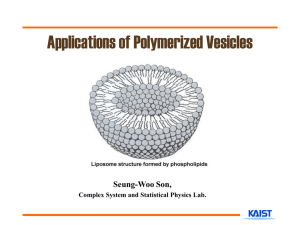
Transferosomes mainly composed of phospholipids like phosphatidyl choline which self
assembles into lipid bilayer in aqueous environment and closes to form a vesicle. The main
component in transfersome formulation is edge activator. It consists of single chain surfactant
that causes destabilization of the lipid bilayer thereby increasing its fluidity and elasticity.
Transfersomes are efficient in delivering the low molecular weight and as well as high
molecular weight drugs through skin, consisting of hydrophobic and hydrophilic moieties
together and has a result wide range of solubility. This high deformability gives better
penetration of intact vesicles. (5)
The drug loaded with transfersomes transfer across the skin from the epidermis into the
dermis and finally into lymphatic vessels and blood vessels, and possess a therapeutic effect.
Due to their more elasticity as comparing to standard liposomes, transfersomes are well
suited for the skin penetration. Transfersomes were developed in order to take the advantage
of phospholipids vesicles as transdermal drug carrier. Transfersomes overcome the skin
penetration difficulty by squeezing themselves along the intracellular sealing lipid of the
stratum corneum. (6)
German company IDEA AG registered the term Transfersome as a trademark to refer to its
drug delivery technology. The name means “carrying body”, and it is derived from the Latin
word 'transferre', which means ‘to carry across’, and the Greek word ‘soma’, means for a
‘body’.
Advantages of transfersomes :(7)
Transfersomes can deform and pass through narrow constriction without measurable loss.
They have the following advantages:
a. Trasfersomes have high entrapment efficiency,in case of lipophilic drug their
entrapment efficiency is up to 90%.
b. Transfersomes can act as a carrier for both low and high molecular weight drugs
such as analgesic, insulin, protein, anaesthetic, corticosteroids, sex hormone,
anticancer and albumin.
c. Transfersomes can accommodate drug molecules with wide range of solubility; they
have an infrastructure consisting of both hydrophobic and hydrophilic moieties.
d. They can release their contents slowly and gradually, because they act as depot.
e. They are made from natural phospholipids similar to liposomes, as a result they are
biocompatible and bio- degradable.
f. They can be used for both systemic and topical drug delivery.
g. They protect the encapsulated drug from metabolic degradation.
h. They are easy to scale up, as procedure is simple, do not involve lengthy procedure.
The clinical effectiveness of transferosomes was found in many randomized trial both on
hauman and animal. In various clinical trial stages, when Transfersulin (insulin-loaded
transfersome) were applied on alloxan diabetic mice for hypoglycaemic effect. The
penetration of Transfersulin could result in a decrease in blood glucose level in alloxaninduced diabetic rabbits with a simultaneously increased blood insulin level. (8)
Limitations of transfersomes:
1. Transfersomes are chemically unstable because of their predisposition to oxidative
degradation.
2. Lack of purity of the natural phospholipids comes in the way of adoption of
transfersomes as drug delivery vehicles.
3. Transfersomes formulations are expensive.
TRANSFERSOMES v/s OTHER CARRIER SYSTEMS: (9-10)
Transfersomes are generally differ from the mixed micelles .They are as following
1. In size,a transfersomes is greater than the standard lipid micelles.
2. Each vesicular transfersomes contains a water filled core whereas a micelle is just a
simple fatty droplet. As a result, transfersomes can carry water as well as fat-soluble agent in
comparison to micelles that can only incorporate lipoidal substances.
3. Transfersomes are different from commonly used liposomes as they are much more
flexible and adaptable.
4. Confocal Scanning Laser Microscopy (CSLM) can be used to differentiate the penetration
ability of all these carrier systems in the intact murine skin. In all these vesicles the highly
deformable transfersomes transverse the stratum corneum and enter into the viable epidermis
in significant quantity.
KINETICS OF PENETRATION OF TRANSFERSOMES:
After penetration of Transfersome through the outermost skin layers, transfersomes reach the
deeper skin layer. From this latter skin region they are normally washed out, via the lymph,
into the blood circulation and through the latter throughout the body. Transfersomes can thus
reach all such body tissues that are accessible to the subcutaneously injected liposomes. The
kinetics of action of an epicutaneously applied agent depends on the velocity of carrier
penetration as well as on the speed of distribution of the drug and the action after this
passage.
Transfersomes when applied to skin under suitable condition, they can transfer 0.1 mg of
lipid per hour and cm2 area across. The mechanism for penetration is the generation of
“osmotic gradient” due to evaporation of water while applying the transfersomes on the skin
surface. The transport of these elastic vesicles is thus independent of concentration. The
trans-epidermal hydration provides the driving force for the transport of the vesicles. (11)
Fig 1 : Penetration Pathway of Transfersomes
Table 1: Comparison of different approaches for permeation enhancement (12)
Method
Liposomes
Advantage
Disadvantage
Phospholipid vesicle, they Less skin penetration and
are biocompatible and
less stable.
Biodegradable. Suitable for
controlled release.
Proliposome
Phospholipid vesicle, more They cause aggregation and
fusion of vesicles.
stable than liposomes
Iontophoresis
(Physical methods)
Increase
penetration
of Applicable only for charged
intermediate size charged drug. Transfer efficiency is
molecule.
low.
Niosomes
Non-ionic
surfactants
vesicles. They improve oral
bioavailability of poorly
absorbed drugs and enhance
skin penetration of drugs and
delayed clearance from body.
More stable, high penetration
due to high deformability,
biocompatible and
biodegradable, suitable for
both low and high molecular
weight and also for lipophilic
as well as hydrophilic drugs
and reach up to deeper skin
layers.
Transfersomes and
Protransfersomes
Less skin penetration easy
handling But will not reach
up to deeper skin
layer
They are chemically unstable
because
of
their
predisposition to oxidative
degradation.
OPTIMIZATION OF FORMULATION CONTAINING TRANSFERSOMES:
Optimization techniques are abundant in pharmaceutical industry. Optimization techniques
provide both a depth of understanding and an ability to explore and defend ranges for
formulation and processing factor. There are various process variables which could affect the
preparation and properties of the transfersomes.
The preparation procedure for transfersomes was first optimized and validated. The process
variables in formulation depend upon the procedure involved for manufacturing of
formulation. The preparation of transfersomes involves various process variables such as,
1 .Lecithin: surfactant ratio
2. Effect of various solvents
3. Effect of various surfactants
4. Hydration medium
Optimization was done by selecting entrapment efficiency of drug. During the preparation of
a particular system, the other variables were kept constant. (13)
Fig 2: Process Variables affecting Optimization Technique in Transfersomes
Formulation
MATERIALS REQUIRED FOR PREPARATION OF THE TRASNSFEROSOMES:
1. Phospholipids – (Vesicles forming component) Ex. - Soya phosphatidyl choline, egg
phosphatidyl choline,
2. Surfactant – (Providing flexibility). Ex. - Sod.deoxycholate, Tween-80, Span-80
3. Alcohol – (As a solvent) .Ex. - Ethanol, methanol
4. Buffering agent – (As a hydrating medium) Ex. - Saline phosphate buffer (pH 6.4)
5. Dye - {for Confocal scanning laser microscopy (CSLM)} Ex. – Rhodamine.
METHOD OF PREPARATION OF TRANSFERSOMES:
1. Thin film hydration technique: (12-13-14)
For the preparation of transfersomes thin film hydration technique is used, which comprised
of mainly three steps.
(a) At first, the vesicle forming ingredients phospholipids and surfactant were dissolved in
volatile organic solvent. The organic solvent evaporated above the lipid transition
temperature using rotary evaporator. Final traces of solvent were removed under vacuum for
overnight. The deposited lipid films were hydrated with buffer by rotation at 60 RPM/min.
(b)The thin film is hydrated with buffer solution (pH 6.5) by rotation at 60 rpm for 1 hr at the
corresponding temperature. The resulting vesicles were swollen for 2 hr at room temperature.
(c)To prepare small vesicles, resulting vesicles were sonicated at room temperature or 50°C
for 30 min, using a bath sonicator or probe sonicator. The sonicated vesicles were
homogenized by manual extrusion 10 times through a sandwich of 200and 100 nm
polycarbonate membranes (Fig: 1).
2. Modified hand shaking (lipid film hydration technique):
The method comprise of the following steps
(a) Drug, Phosphatidyl choline and Edge activator (Surfactant) were dissolved in ethanol:
chloroform (1:1) mixture. Organic solvent was removed by evaporation while hand shaking
above lipid transition temperature (43°C). A thin lipid film was formed inside the flask wall
with rotation. The thin film was kept overnight for complete evaporation of solvent.
(b)The film was then hydrated with phosphate buffer (pH 7.4) with gentle shaking for 15
minute at corresponding temperature. The transfersomes suspension further hydrated up
to1hour at 2-8°C.
Fig 3: Method of Preparation of Transfersomes
CHARACTERIZATIONS OF TRANSFERSOMES: (15-16-17)
The characterization of transfersomes is generally similar to liposomes, niosomes and
micelles.
(a) Entrapment Efficiency:
Using centrifugation method entrapment efficiency of un-entrapped drug was determined.
The amount of drug entrapped (Total amt. of drug- unentrapped drug) in the vesicles was
then determined by disrupting the vesicles using phosphate buffer, followed by filtration and
amount of drug was quantified spectrophotometrically.
Entrapment efficiency = (Amount entrapped / Total amount added) ×100
(b)Vesicle Shape and Type: Transfersomes vesicles can be visualized by Transmmision
Electron Microscopy, with an accelerating voltage of 100 kV. Transfersomes vesicles can be
visualized without sonication by phase contrast microscopy by using an optical microscope.
(c) Number of Vesicle per Cubic mm: For optimizing the composition and other process
variables in the formulation, it is an important parameter. Transfersomes formulations
(without Sonication) can be diluted five times with 0.9% of sodium chloride solution and
studied with optical microscopy by using haemocytometer.
(d)Penetration Ability: Fluorescence microscopy is used to evaluate the penetration ability of
transferosomes .
(e) Surface Charge and Charge Density: Zetasizer is used to determine surface charge and
charge density of transferosomes.
(f) Confocal Scanning Laser Microscopy (CSLM) Study:
Conventional light microscopy and electron microscopy both face problem of fixation,
sectioning and staining of the skin samples. Often the structures to be examined are actually
incompatible with the corresponding processing techniques; these give rise to
misinterpretation, but can be minimized by Confocal Scanning Laser Microscopy
(CSLM).Different fluorescence markers such as Fluorescein- DHPE, Rhodamine-DHPE used
in CSLM study.
(g) Degree of Deformability or Permeability Measurement:
In the case of transfersomes, the permeability study is one of the important and unique
parameter for characterization. The deformability study is done against the pure water as
standard. Transfersomes preparation is passed through a large number of pores of known size
(through a sandwich of different microporous filters, with pore diameter between 50 nm and
400 nm, depending on the starting transfersomes suspension). Particle size and size
distributions are noted after each pass by dynamic light scattering (DLS) measurements
(h) In vitro drug release study: For determining the permeation rate in vitro drug release study
is performed. For determining drug release, transfersomes suspension is incubated at 320ºC
and samples are taken at different times and the free drug is separated by centrifugation
method .The amount of drug released is then calculated indirectly from the amount of drug at
zero times as the initial amount (100% entrapped and 0% released).
Fig 4-Electron micrograph images of Transfersomes.{Zheng et al (2012)
List of Drugs used for Transfersomes:
Transfersomes
Clotrimazole transfersomes
Curcumin transfersomes
Method
Rotary evaporation method
Modified
hand
shaking
method
Quercetin transfersomes
Modified
hand
shaking
method
Indinavir
sulfate Conventional
rotary
transfersomes
evaporation method
Valsartan
Conventional
rotary
nanotransfersomes
evaporation method
Ibuprofen transfersomes
Rotary evaporation method
Itraconazole transfersomes
Film dispersion method
Reference
R Kumar et al (2012)18
R.Patel et al (2009)19
B.K Sarkar et al (2012)20
Maurya et al (2010) 21
Ahad et al (2010)22
Irfan M etal (2012)23
Zheng et al (2012)24
Patent Reports on Transfersomes as carriers for the delivery of therapeutic agents:
Application no of patent
Applicant
Results
US 20020048596A1 (2002)
Gregor Cevc.
US 7175850 B2 (2007)
IDEA AG, Munich (DE)
The patent claims the use of
NSAID in transfersomes for
transport through natural
barriers and constriction of
skin.25
Described the administration
of
corticosteroids
via
transfersomes on mice skin
for oedema suppression
activity .They were tested
against commercial reference
cream.26
US 20070042030 A1 (2007)
IDEA AG, Munchen (DE)
It is
non invasive and
painless therapy, resulted in
>90% of the applied drug
dose reaching the destined
organ of the body.27
US 7591949 B2 (2009)
IDEA AG, Munich (DE)
Claimed
the
penetrant
capability of transfersomes
because these deformable
complex droplets adapt the
pore of the skin. They
deform and penetrate the skin
along the natural moisture
gradient
rather
than
28
coalescing locally.
CONCLUSION:
Transdermal drug delivery system though have many advantages over oral route, still not
explored to high extent and it necessitates the newer technological addition to the existing
methods and practices in transdermal delivery system design.
Transfersomes are highly deformable particles, which can be used to bring drugs across the
biological permeability barriers, such as skin. Transferosomes are complex lipid molecules
that can increase the transdermal flux, prolonging the release and improving the site
specificity of bioactive molecules.Therefore enhanced delivery of NSAIDS, herbal drugs,
anticancer drugs, protein, peptides and insulin through the skin by means of an ultradeformable vesicular carrier open new challenges and opportunities for the development of
novel improved therapies. This technology is best suited for non-invasive delivery of
therapeutic molecules across open biological barriers.
Transferosomes facing approval problem due to non-availability of pure phospholipid and is
a matter of concern in developing these carrier. Stability related issues can be addressed by
the approaches available for liposomes and nanoparticles which include surface modification,
combining polymeric segment, modifying the manufacturing process for week chemical bond
formation, etc.
The fewer drugs loading tag to transdermal system must be challenged using novel
transferosomes carrier.
REFERENCES:
1. Kumar R, Philip A, Modified Transdermal Technologies: Breaking the Barriers of Drug
Permeation via the Skin, Tropical Journal of Pharmaceutical Research, March 2007; 6 (1):
633-644.
2. Kundlik G, Pal R, Potential Role of Transfersomes in Transdermal Drug Delivery, World
Journal of Pharmaceutical Research, Vol 1(1), 21-38.
3. Prausnitz M.R, Langer S.R, Current status and future potential of transdermal drug
delivery. Nat. Rev. Drug Discov., 2004, 3: 115-124.
4. Modi CD, Bharadia PD. Transferosomes: New Dominants for Transdermal Drug Delivery.
American Journal of PharmTech Research 2012, 2(3): 72-91.
5. Sivannarayana P, Parmeela A Rani, Saikishore V, Venubabu Ch and Sri Rekha.
Transfersomes: Ultra Deformable Vesicular Carrier System in Transdermal drug delivery
system. Research Journal of Pharmaceutical Dosage forms and Technology. 2012; 4(5): 243245.
6. Pirvu C.D, Hlevca C, Ortan A, Prisada R: Elastic vesicles as drugs carriers through the
skin. Farmacia 2010; 58 (2): 128
7. Kaushik A,Dwivedi A, Sunda M,Transfersomes: The Drug loaded ultradeformable vesicles
for Transdermal Delivery,International Research Journal of Pharmacy,2011 2(11), 40-42.
8. Kumar A, Pathak K, Bali V: Ultra–adaptable Nanovesicular Systems: A carrier for
systemic delivery of therapeutic agents, Drug Discovery Today, 2012(17), 21-22.
9. Cevc G, Isothermal Lipid Phase,Transitions Chemistry and Physics of Lipids,1991; 57:
293-299.
10. Vinod K.R, Kumar M.S, Anbazhagan S, Sandhya S, Saikumar P, Rohit R.T, Banji D,
2012, Critical issues related to transfersomes– novel vesicular system. Acta Sci. Pol.,
Technol. Aliment. 1(11), 67-82.
11. Prajapati S.T, Patel C.G , Patel C.N, Transfersomes: A Vesicular Carrier System For
Transdermal Drug Delivery, Asian Journal of Biochemical and Pharmaceutical Research
Issue 2 (Vol. 1) 2011.
12. Sachan R, Parashar T, Soniya, Singh V, Sing G, Tyagi S, Patel C, Gupta A, Drug Carrier
Transfersomes: A NovelTool For Transdermal Drug Delivery System,International Journal of
Research and Development in Pharmacy and Life Sciences, February - March, 2013, Vol.
2(2), 309-316.
13. Sheo DM, Shweta A, Vijay KT, Ram CD, Aklavya S, Ghanshyam M, “Enhanced
Transdermal delivery of Indinavir Sulfate via transfersomes”, Pharmacie
Globale (IJCP), 2010, 1 (06), 1-7.
14. Anand P,Samnani A, Bhoumick M, Dubey B.K , Ultra Deformable Elastic
VesiclesTransfersomes For Enhanced Skin Delivery,World Journal of Pharmaceutical
Research 2012 ,Vol 1(2), 10-21.
15. Walve J.R, Bakliwal S.R, Rane B.R, Pawar S.P, Transfersomes: A Surrogated Carrier For
Transdermal Drug Delivery System, 2011, 2(1).204-213.
16. Parashar B, Kaur A, Gupta N, Singh B,Maurya B, Yadav
approach for Vesicular Drug Delivery System 2012, Vol 2(2), 86-91.
V, Transfersomes-An
17. Bhardwaj V , Shukla V, Singh A, Malviya R , Sharma P.K, Transfersomes ultra
flexible vesicles for transdermal delivery, Indian Journal Of Pharmaceutical Sciences and
Research, (2010), Vol 1(3),12-19.
18. Kumar R, Rana A.C, Rajni Bala, Seth N, “Formulation and Evaluation of
Elastic Liposomes of Clotrimazole” Int. J. Drug Dev. & Res., July-September 2012, 4(3):
348-355.
19. Patel R, Singh. S.K,Sheth. N.R,Gendle. R, Development and Characterization of
Curcumin Loaded Transfersome for Transdermal Delivery, J. Pharm. Sci. & Res. Vol.1(4),
2009, 71-80.
20.Sarkar B.K, Maharshi A, Baniwal A, Kumar S,Sachan M,
Formulation and
Characterization of Quercetin Transfersome for Transdermal Delivery, International Journal
of Pharmaceutical and Medical Sciences Vol. 1(1), June 2012.
21. Maurya S.D, Aggarwal S , Tilak V.K, Dhakar R.C, Singh A.K, Enhanced Transdermal
Delivery of Indinavir Sulphate Via Transfersomes, Pharmacie Globale (IJCP) 2010, 1 (06).
22. Ahad A, Aqil M, Kohli K, Sultana Y, Mujeeb M, Ali A,Formulation and optimization
of Nanotransfersomes using experimental design technique for accentuated transdermal
delivery of Valsartan, Nanomedicine: Nanotechnology, Biology, and Medicine 2012 (8) 237–
249.
23. Irfan M, Verma S, Ram A, Preparetion and Characterization of Ibipropen loaded
Transfersomes as a novel carrier for Transdermal drug delivery, Asian Journal of
Pharmaceutical and clinical Research, 2012:5(3): 162-165.
24.Zheng W.S , FangX.Q ,Wang L, Zhang Y, Preparation and quality assessment of
Itraconazole transfersomes, International Journal of Pharmaceutics 436 (2012) 291– 298.
25. Cevc, G. Preparation for the transport of an active substance across barriers, US
20020048596A1, (2002).
26. Cevc G. IDEA AG, Munich. Formulation for topical non-invasive application in vivo,
US007175850B2,(2007).
27. Cevc G. IDEA AG, Munchen, Preparation for the application of agents in mini-droplets,
US20070042030A1, (2007).
28. Cevc G. et al (2009) IDEA AG, Munich,Method for the improvement of transport across
adaptable semipermeable barriers, US007591949B2.