2012 Physician Services Agreement: Overview
advertisement
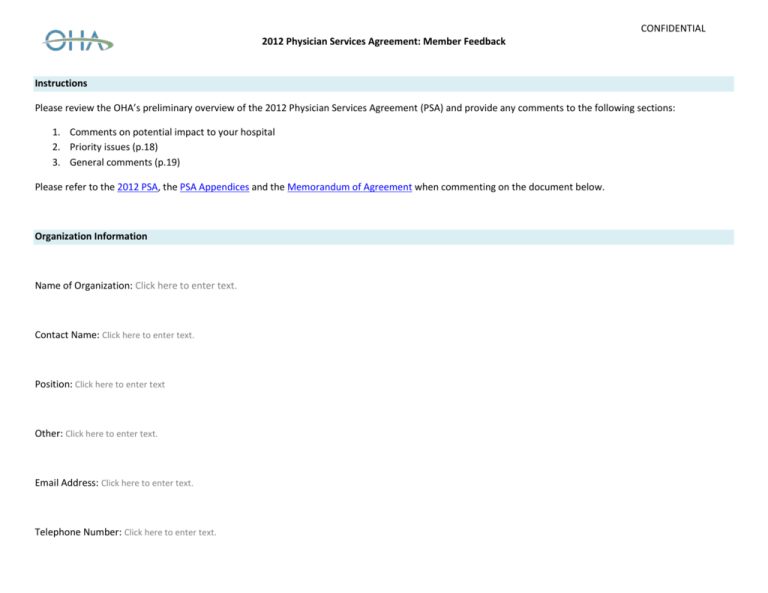
CONFIDENTIAL 2012 Physician Services Agreement: Member Feedback Instructions Please review the OHA’s preliminary overview of the 2012 Physician Services Agreement (PSA) and provide any comments to the following sections: 1. Comments on potential impact to your hospital 2. Priority issues (p.18) 3. General comments (p.19) Please refer to the 2012 PSA, the PSA Appendices and the Memorandum of Agreement when commenting on the document below. Organization Information Name of Organization: Click here to enter text. Contact Name: Click here to enter text. Position: Click here to enter text Other: Click here to enter text. Email Address: Click here to enter text. Telephone Number: Click here to enter text. CONFIDENTIAL 2012 Physician Services Agreement: Overview Key Issues Impacting Hospitals Reference format in ‘Agreement Initiatives/ Strategies’ column: Section Payments Section 1 Appendix A Review of Changes to Schedule of Benefits (April 2012) Section 2 Appendix B Agreement Initiatives/ Strategies Payment Discount (1.1) 0.5% ‘across the board discount’ applied to all physician payments Application of Payment Discount (1.2) 0.5% discount applied to all fee-for-service payments, primary care models, Alternate Funding Plans/ Alternate Payment Plans, physician programs (i.e. Hospital On-Call Coverage Program) OMA/MOHLTC will continue to work on evidence-based initiatives Phase ll Review (1.3; Section A, Appendix A) Physician Services Committee (PSC) to establish a working group to conduct a Phase ll Review that promotes the use of evidence and best practices for the appropriate provision of health care resources Review will investigate the overuse, misuse, underuse of resources Recommendations from the Review will focus on 15 tests, treatments and services 1 that are currently underused Appropriate Prescribing (1.3; Section B, Appendix A) PSC to develop a program that reviews prescribing practices among physicians Targeted education strategies and mechanisms for improving the tracking of prescriptions will be recommended Narcotics and controlled substances will be initial focus of the program Program will be voluntary and data used to identify physicians will be kept confidential to the physician and the PSC Review of Payment Discount (1.4) PSC to conduct a review of the savings associated with the Phase ll and Appropriate Prescribing Reviews 100% of any savings realized will be applied to the 0.5% payment discount Amendments to Schedule of Benefits (2.1; Appendix B - #1-9) The following changes made to the Ontario Health Insurance Plan (OHIP) Schedule of Benefits in April 2012 will be amended: o Optical Coherence Tomography (OCT): codes for unilateral/ bilateral retinal disease and glaucoma to be increased from $25 to $35. o After-hours procedure premiums: restored from 40% to 50% (evenings), 65% to 75% (midnight) Effective Date (1.3; Section A, Appendix A) Physician Services Appendix to Physician Agreement Services Agreement (1) Comments on Potential Impact April 1, 2013 April 1, 2013 October 1, 2012 April 1, 2013 October 1, 2013 April 1, 2013 1 Phase II recommendations include: Limitation of self-monitoring and blood glucose tests, Investigations in the work-up of dementia, Appropriate sleep lab testing, Anesthesia requirements for vasectomies, cataracts and endoscopy, Lipid testing, Serum protein electrophoresis, Appropriate ultrasound imaging, Vitamin B12, Funding for pre-operative cardiac testing for asymptomatic patients, Genetics strategy, Companion diagnostics, Schedule of Benefits for Bond Mineral Testing by DXA, Relevancy of pre-dental/ pre-operative assessments with the services provided by hospital-based pre-operative assessment clinics, Utilization and relevancy of preoperative consultations, Changes in practice patterns for the provision of cardiac services and impact on utilization arising from changes in PSA (Physician Services Agreement, 2012, S. 1.3 Appendix A) 2 Last Revised: 2/9/2016 CONFIDENTIAL 2012 Physician Services Agreement: Overview Key Issues Impacting Hospitals Reference format in ‘Agreement Initiatives/ Strategies’ column: Section Agreement Initiatives/ Strategies Effective Date (1.3; Section A, Appendix A) Physician Services Appendix to Physician Agreement Services Agreement (1) Comments on Potential Impact o Anesthesia flat fee for procedural sedation: increased from $60 to $75 when anesthesiologist providing one-on-one care o Laparoscopic surgical fee premiums: restored from 10% to 25% o Intensive and coronary care premium: complete restoration of premium applied for each patient seen on visit to ICU or CCU claimed by a physician who was not the Most Responsible Physician (MRP) o Lumbar spine: removal of requirement for physicians to repay X-ray or CT studies of the lumbar spine if found not to be medically necessary Development of New Billing Codes and Payment Rules (2.1, Appendix B - #1-9) The following fee codes and/ or payment rules will be developed: o Optical Coherence Tomography (OCT) 1. Code for patients receiving active treatment for unilateral/ bilateral retinal disease/ glaucoma ($35) 2. Code for active management of retinal disease ($25) 3. Code for OCT related to treatment of children ($35) o Fees for anesthesia 1. Consider the development of supervisory code for anesthesiology 2. Develop code to provide anesthesia for cataracts, colonoscopy, cytoscopy, sigmoidoscopy in low volume/ rural settings 3. Recommendation of a solution to move procedures out of hospitals and into out of hospital facilities that have access to care provided by Anesthetic Care Teams o Cataracts: Ontario Health Technology Advisory Council (OHTAC) to review objective criteria for cataract extractions. o Assessment with surgical procedures: restriction imposed on physicians from billing a higher paying assessment/ consultation on the day of a surgical procedure when a previous assessment/ consultation had already been billed will be reviewed. Physicians will be permitted to submit rejected codes for manual review. o Pediatric consults: April 1, 2012 changes clarified that pediatricians should not be paid as specialists when providing care to adult patients aged 18+ Pediatricians may be exempted to charge specialist fees to adult patients (a) when such patients are developmentally delayed and (b) when pediatrician has specialty training (i.e. allergist) and treats an adult patient requiring this care OMA Section on Pediatrics will be solicited to determine whether exemption process is creating problems in providing pediatric-specific services to adult patients April 1, 2013 3 Last Revised: 2/9/2016 CONFIDENTIAL 2012 Physician Services Agreement: Overview Key Issues Impacting Hospitals Reference format in ‘Agreement Initiatives/ Strategies’ column: Section Agreement Initiatives/ Strategies Self Referral Regulation (2.1, Appendix B - #10) Removal of regulation reducing self-referrals and referrals within physician/ hospital groups for diagnostic services by 50%2 The Expert Panel on Appropriate Utilization of Diagnostic and Imaging Studies will continue to make recommendations to the PSC April 1, 2012 Flow Though (3.1) April 1, 2012 decreased to the Schedule of Benefits will be flowed through to the payments as outlined in this section. April 1, 2012 Flow Through Section 3 Appendix C Reverse Flow Through (3.1, Appendix C) 1. Specialist Alternative Payment Plans (APPs) and Physician Programs Changes to specialist payments in April 2012 (i.e. reduction of fees for electrocardiograms by 50%) will be applied to specialist AFP/APP agreements and Academic APPs o Changes (increase or decrease) will be applied to the clinical contract value of each plan (excluding administrative and non-clinical payments) o Where possible, flow through will be implemented as an adjustment to the Service Encounter Premium3 o Clinical physician payments that received positive flow through4 (i.e. fee increase) from the 2008 PSA will be subject to a reverse flow through Primary Care Specialty Models Reverse flow through arising from the April 2012 changes to family physicians (i.e. fee reduction for intermediate assessments) will be applied to the clinical base of 16 primary care specialized models (e.g. Aboriginal Health Access Centres, Rural-Northern Physician Group Agreements 1 and 2, Community Health Centres) Equivalent Flow Through (3.1, Appendix C) The fee code for an Intermediate Assessment was reduced by $1.00 (fee-for-service) and by $0.15 (primary care models) in April 2012 o The GP Psychotherapy premium will be reduced from 15% to 12% in alignment with this decrease Professional fees5 for diagnostic radiology, MRI and diagnostic ultrasound were reduced by 5% in April 2012. The following professional fees will be reduced by 5% in alignment with this decrease: Effective Date (1.3; Section A, Appendix A) Physician Services Appendix to Physician Agreement Services Agreement (1) Comments on Potential Impact April 1, 2012 January 1, 2013 2. January 1, 2013 January 1, 2013 January 1, 2013 2 Nuclear Medicine, Diagnostic Radiology, MRI, Diagnostic Ultrasound, Pulmonary Function Studies, Diagnostic and Therapeutic Procedures (MOHLTC, 2012) Non-fee-for-service physicians practising under alternative payment plans or primary care arrangements in Ontario are required to submit Service Encounter Reporting (shadow-billing) in accordance with the Schedule of Benefits. Under some arrangements (i.e. AFPs), shadow-billed claims generate a Service Encounter Premium that represents a percentage of the full value of the claim. (Health Force Ontario, 2010) 4 Mental Health Sessionals, Sessional Fee Supplement, Psychiatric Stipend, Physicians compensation in Divested Provincial Psychiatric Hospitals, Physicians compensation in Assertive Community Treatment Teams, OPOP sessionals, Visiting Specialist Program and Urgent Locum Tenens Program for Specialists sessionals, and the Hospital Pediatric Stabilization Program (Physician Services Agreement, 2008, S. 3.3) 3 4 Last Revised: 2/9/2016 CONFIDENTIAL 2012 Physician Services Agreement: Overview Key Issues Impacting Hospitals Reference format in ‘Agreement Initiatives/ Strategies’ column: Section Primary Care Section 4 Appendix D Agreement Initiatives/ Strategies o Nuclear medicine o Sleep studies o Radiation oncology treatment planning codes Primary Care (4.1) All primary health care initiatives are continued and amended as outlined in this section Primary Health Care Committee (PHCC) (4.1, Appendix D, #1) PHCC to be reconstituted; mandate/ terms of reference to be developed by PSC: 1. Oversee implementation of initiatives outlined in this section of the PSA 2. Responsible for review/ evaluation prior to end of PSA Personalized Health Visit (4.1, Appendix D, #2) Annual health exam to be replaced by a personalized bi-annual health visit for adult patients aged 18-64 o New fee code will be established ($50) o Patients in other age groups will be unaffected o Capitation rates will not be adjusted (fee-for-service only) Alignment with Excellent Care for All Act (ECFAA) (4.1, Appendix D, #3) Expansion of primary health care quality agenda to Family Health Teams, Aboriginal Health Access Centres, Community Health Centres PHCC to coordinate rollout and implementation of: o Annual Quality Improvement Plans (QIPs) o Development of indicators o Development of patient experience surveys o Public reporting Daytime Access (4.1, Appendix D, #4.1) PHCC to investigate daytime access to primary care physicians participating in patient enrolment models (PEMs)6 PHCC to make recommendations on guidelines to inform PEM physicians on operating during daytime hours (i.e. standards for group size, strategies and support for advanced access) Effective Date (1.3; Section A, Appendix A) Physician Services Appendix to Physician Agreement Services Agreement (1) Comments on Potential Impact October 1, 2012 January 1, 2013 April 1, 2013 By April 1, 2013 5 Diagnostic tests and other procedures often have two fees. Professional fees are paid to the physician who performs and interprets the test, and technical fees are paid to the facility (e.g., the hospital) to offset the costs associated with providing the services (e.g., technicians’ salaries, overhead expenditures, capital outlays and amortization). (ICES, 2012) 6 PEMs are of two main types: (1) Harmonized models, such as the Family Health Network (FHN) and the Family Health Organization (FHO), are blended capitation models and (2) Non-harmonized models, such as the Family Health Group (FHG) and the Comprehensive Care Model (CCM), are enhanced fee-for-service (FFS) models (OMA, 2012) 5 Last Revised: 2/9/2016 CONFIDENTIAL 2012 Physician Services Agreement: Overview Key Issues Impacting Hospitals Reference format in ‘Agreement Initiatives/ Strategies’ column: Section Agreement Initiatives/ Strategies Effective Date (1.3; Section A, Appendix A) Physician Services Appendix to Physician Agreement Services Agreement (1) Comments on Potential Impact Enhanced After-hours Access (4.1, Appendix D, #4.2) Family Health Networks (FHNs), Family Health Organizations (FHOs), Family Health Groups (FHGs)will be required to provide the following after-hours service blocks7 based on size of the group: Number of physicians in group 10-19 20-29 30-74 75-100 100-199 200 + Total number of after-hours service blocks (per week) 7 8 10 15 20 25 Northern FHO and FHG groups who require 50% of its physicians to maintain active inpatient hospital privileges are exempt from after-hours coverage requirements above FHO and FHN agreements will be amended to ensure the staffing of additional physicians after-hours may be necessary if the group determines that the volume and needs of their patients require additional staff House Calls (4.1, Appendix D, #4.3) Primary care physicians will be incented to provide more house calls with a focus on homebound, frail/ elderly patients: o New fee code for housecalls to homebound, frail/elderly patients to be developed by the PHCC o A 20% premium will be applied to Comprehensive Care Model (CCM), FHG, FHN physicians who provide 68+ house calls per year to more than 17+ patients, if 75% of these calls were to homebound, frail and elderly patients o Additional bonus to all family physicians and PEM physicians will be applied on an increasing scale for up to 32 patients served with more than 128 encounters Termination of THAS Obligation (4.1, Appendix D, #5) All PEM agreements will be amended to delete service requirements and payment terms for the Telephone Health Advisory Service (THAS) PEM groups will be permitted to provide THAS on a voluntary basis Termination of Access Bonus Rebate (4.1, Appendix D, #6.1) Access bonus rebate ($237.91 per eligible physician) established in 2008 PSA that compensated capitated PEM physicians (FHO, FHN) for enrolled patient use of focused practice GPs will be cancelled 7 April 1, 2013 April 1, 2013 January 1, 2013 October 1, 2012 A service block refers to a 3-hour period in which one physician within the group is available. Blocks are after 5pm on weekdays or anytime on weekends (MOHLTC, 2010) 6 Last Revised: 2/9/2016 CONFIDENTIAL 2012 Physician Services Agreement: Overview Key Issues Impacting Hospitals Reference format in ‘Agreement Initiatives/ Strategies’ column: Section Agreement Initiatives/ Strategies Review of Access Bonus (4.1, Appendix D, #6.2) PHCC to conduct a policy review of the access bonus payment in FHO/FHN arrangements to review intent and current application of outside use. The review will consider: o Value of negative access bonuses o Impact on emergency departments o Exemptions for Urgent Care Centres and GP focused practices o Impact from walk-in clinics Premium and Payment Changes (4.1, Appendix D, #7) Elimination of service premiums in PEM agreements o In-office service bonus8 ($10 Million annually) o Out-of-office service bonus9 o Preventative care management services enhancement fee (code - $6.86) Effective Date (1.3; Section A, Appendix A) Physician Services Appendix to Physician Agreement Services Agreement (1) Comments on Potential Impact March 31, 2014 Oct 1, 2012 April 1, 2013 April 1, 2013 Capitation and Long-Term Care Patients o Residents in LTC will be required to be rostered as an LTC patient or seen on a feefor-service basis o LTC patients should not be rostered as non-LTC patients and billed the monthly management fee in addition to that o MOHLTC to revise LTC patient enrolment process to make it administratively easier for physicians to enroll such patients. Comprehensive Care Management Fee Reduction for Large Rosters o PHCC to develop methodology in which CCM capitation payment will be reduced by 50% for each patient a physician enrolls above 2500 April 1, 2013 Diabetic Management Fee o Fee code reduced from $75 to $60 April 1, 2013 Acuity Modifier o $40 Million will be set aside to develop and implement a premium for PEM agreements (for high acuity patients) 2013 (Year 1) will involve selecting an acuity adjustment tool, testing it against OHIP data and designing the payment system October 1, 2012 Interim ToolMarch 31, 2013 8 The In Office Service Bonus Payment is intended to recognize PEM physicians and PEM physician groups who provide a broad range of in-office services. These services fall under the categories of complex procedures, mental health, minor office procedures and reproductive health. Initial payment of $5 million paid in 2010/ 11 (MOHLTC, 2010) 9 Out-of-office bonus reflects the extent to which rostered patients reflect population demographics in the physician’s community. In 2011/12, it rewarded top performing groups who provided the broad range of out of office services which meet the needs of their rostered patients (i.e. aging at home/ end of life care, maternity/ newborn care) (Physician Services Agreement, 2008, S. 5.2) 7 Last Revised: 2/9/2016 CONFIDENTIAL 2012 Physician Services Agreement: Overview Key Issues Impacting Hospitals Reference format in ‘Agreement Initiatives/ Strategies’ column: Section Agreement Initiatives/ Strategies Effective Date (1.3; Section A, Appendix A) Physician Services Appendix to Physician Agreement Services Agreement (1) Comments on Potential Impact 2014 (Year 2) will involve conducting systems testing, adjusting the tool to MOHLTC payment systems, providing physician education and developing a communications plan o PHCC will report back to OMA/MOHLTC with recommendations for the tool that will be selected as the Acuity Modifier Managed Entry Process (4.1, Appendix D, #8) 1. Family Health Groups No limit will be applied to physicians joining FHG groups 2. Virtual Care Section 5 Appendix E Family Health Organizations/ Family Health Networks Registration of 40 new physicians into FHN and FHO models each month in two streams: 1) 20 physicians in prioritized stream for new graduates and physicians seeking to practice in high need areas, and 2) 20 physicians in regular stream- first come, first serve Unused spots from one stream will shift to the other stream and/or rolled-over to subsequent months Replacement physicians (i.e. for deceased/ retiring physicians) will be processed outside of managed entry process Interprofessional Health Provider (IHP) Funding (4.1, Appendix D, #9) Expansion of availability of IHPs for patients in community with primary care needs Full salary funding made available to support full integration of IHPs (i.e Physician Assistants) into non-Family Health Team affiliated PEM groups (i.e. FHNs, FHOs) of three of more physicians (i.e. not CCMs) PHCC will oversee implementation and establishment of criteria which will examine (a) community need, (b) roster size, (c) involvement in quality improvement initiatives, (d) integration with other providers in region to support population-based planning Family Health Group Governance Agreements (4.1, Appendix D, #10) Amendment of FHG agreement to require each group to establish and maintain a written governance agreement between the physician members to formally set out the terms of their relationship Virtual Care (5.1) OMA/MOHLTC have committed to the virtual care initiatives outlined this section. Northern Health Travel Grant (NHTG) (5.1, Appendix E, #1) Modification of NHTG approval process (i.e. increased difficulty) Replacing face-to-face visits with virtual equivalents Final Tool – January 1, 2013 October 1, 2012 April 1, 2013 April 1, 2013 By April 1, 2013 April 1, 2013 8 Last Revised: 2/9/2016 CONFIDENTIAL 2012 Physician Services Agreement: Overview Key Issues Impacting Hospitals Reference format in ‘Agreement Initiatives/ Strategies’ column: Section Agreement Initiatives/ Strategies Specialist to Primary Care Virtual Follow-Up (5.1, Appendix E, #2) Establishment of a Working Group to evaluate existing programs to recommend a comprehensive provincial business and technology model for hospital to primary care communications. Patient eConsults(5.1, Appendix E, #3) Funding for an evaluation project to enable patient-initiated patient to primary care provider eConsultations Evaluations to beginning in capitated sites (i.e. FHO, FHN) followed by fee-for-service setting Primary Care to Specialist eReferral (5.1, Appendix E, #4) eReferral fee codes will be developed for ophthalmology and dermatology Eventual expansion to other specialties Evidence and Appropriateness – Phase I Review Section 6 Appendix F Realignment of Telemedicine Premium (5.1, Appendix E, #5) Ontario Telemedicine Network working group will be established to evaluate personal video conferencing (PVC) deployment, utilization, and volume and workflow trends. Working group will ensure: o PVC utilization targets that signal a diminishing need for full telemedicine premium o Establishment of new premiums for northern/ non-northern telemedicine consultations based on adoption requirements Evidence and Appropriateness (6.1) Use of evidence and best practice to ensure provision of healthcare is relevant to and appropriate for the clinical needs of patients. OMA/MOHLTC has agreed to: o Changes to Schedule of Benefits o Inclusion of ‘comments’ on fee codes to ensure appropriate provision o Removal of selected tests from the MOHLTC’s requisition form o Recommendations for further analysis and/or consultations Revised Laboratory Requisition Form (Appendix F, Section A, #1) Due to oversuse/ misuse, the following tests are recommended to be removed from from the Ontario laboratory requisition forms: o Ferritin o Thyroid stimulating hormone o Vitamin B12 Asparate Aminotransferase (AST) (Appendix F, Section B, #1) AST testing in community laboratories is recommended to be restricted to patients under the care of a specialist at a hospital. o Aligned with OHTAC recommendation Effective Date (1.3; Section A, Appendix A) Physician Services Appendix to Physician Agreement Services Agreement (1) Comments on Potential Impact April 1, 2013 November 1, 2012 January 1, 2013 9 Last Revised: 2/9/2016 CONFIDENTIAL 2012 Physician Services Agreement: Overview Key Issues Impacting Hospitals Reference format in ‘Agreement Initiatives/ Strategies’ column: Section Agreement Initiatives/ Strategies Chloride (Appendix F, Section B, #2) Chloride testing recommended to be removed from the Ontario laboratory requisition form based on limited utility in community setting. o Aligned with OHTAC recommendation Creatine Kinase (Appendix F, Section B, #3) Due to inappropriate ordering as a screening agent creatine kinase recommended for removal from the laboratory requisition form. o Aligned with OHTAC recommendation Folate (Appendix F, Section B, #4) Restriction of folate ordering to red blood cell folate when ordered on advice of physicians with expertise in hematological, inflammatory, or gastrointestinal orders. o Aligned with OHTAC recommendation Reflexive Testing (Appendix F, Section B, #5) Reflexive testing can be used to increase efficiency of ordering, as it allows the physician to indicate the condition and the laboratory to run the necessary tests based on this. Thyroid Scans (Appendix F, Section B, #6) Language will added to the OHIP schedule of benefits under which specific circumstances thyroid scans should be ordered (i.e. adult hypothyroidism) Diagnostics Ordered by Other Practitioners (Appendix F, Section B, #7) Appropriateness of diagnostic studies (i.e. x-rays) ordered by non-physicians (i.e. chiropractors) will be reviewed; referring provider number will now have to be included. Colon Cancer Screening Intervals (Appendix F, Section C, #1) Colorectal cancer follow-up screening intervals will be increased. Recommendations for colonoscopy follow-up are 1 every 5 years or 1 every 10 years based on individual patient indications. o Aligned with recommendation from Cancer Care Ontario (CCO) Cervical Cancer Screening (Appendix F, Section C, #2) Revision of the cervical cancer screening bonuses to reflect CCO’s guidelines on cervical cancer screening o Bonus for PEMs (i.e. FHO, FHN) o Schedule of Benefits changes Interval for screening recommended to increase from 2 years to 3 years, and for those within 21-70 age group Annual Stress Tests (Appendix F, Section C, #3) De-listing of annual stress tests for asymptomatic patients at low risk for heart disease o Aligned with recommendation from American College of Cardiology and the American College of Physicians Effective Date (1.3; Section A, Appendix A) Physician Services Appendix to Physician Agreement Services Agreement (1) Comments on Potential Impact January 1, 2013 January 1, 2013 10 Last Revised: 2/9/2016 CONFIDENTIAL 2012 Physician Services Agreement: Overview Key Issues Impacting Hospitals Reference format in ‘Agreement Initiatives/ Strategies’ column: Section System Savings and Sustainability Section 7 Appendix G Agreement Initiatives/ Strategies Pre-operative Cardiac Testing (Appendix F, Section C, #4) De-listing of pre-operative cardiac testing for patients undergoing low/moderate risk noncardiac surgery (i.e. echo, ECG, nuclear imaging, routine chest x-rays) o Aligned with recommendation from American College of Cardiology and the American College of Physicians Chest X-Rays (Appendix F, Section C, #5) De-listing of routine chest x-rays for screening and routine pre-admission for ambulatory and in-patients with unremarkable history/ physician exam Arthoscopic Lavage (Appendix F, Section D, #1) De-listing of arthoscopic lavage for osteoarthritis of knee o Aligned with OHTAC recommendation Injection of Hyaluronic Acid (Appendix F, Section D, #2) De-listing of the injection of hyaluronic acid o Aligned with OHTAC recommendation System Savings and Sustainability (7.1) Measures outlined in this section ensure sustainability in health care system and promote efficiency of resources. Annual Consecutive Consultations (7.1, Appendix G, #1) Fee for annual consecutive consultations by the same specialist on same patient for same clinical diagnosis will be reduced to a limited/ repeat consult fee or a specific assessment fee Multiple Consultations (7.1, Appendix G, #2) Language to be clarified in the OHIP Schedule of Benefits to limit patient to one second opinion consultation when patient requests Group Appointments (7.1, Appendix G, #3) Creation of group care codes to promote shared medical appointments for diabetes, congestive heart failure, asthma, chronic obstructive pulmonary disease. Hospital Supplies and Equipment (7.1, Appendix G, #4) The OMA/MOHLTC to establish a province-wide product/supplies standard for specific procedures to reduce variation among vendors and cost. OMA will encourage physicians to standardize use of hospital supplies and equipment (i.e. technology, prosthetics). Areas of initial focus: o Hip/ knee replacements o Spine o Cataracts/ cataract lenses o Vascular/ cardiac stents Effective Date (1.3; Section A, Appendix A) Physician Services Appendix to Physician Agreement Services Agreement (1) Comments on Potential Impact January 1, 2013 April 1, 2013 11 Last Revised: 2/9/2016 CONFIDENTIAL 2012 Physician Services Agreement: Overview Key Issues Impacting Hospitals Reference format in ‘Agreement Initiatives/ Strategies’ column: Section Bilateral Monitoring and Accountability Process Section 8 CPSO Complaints Process Section 9 CMPA Section 10 Appendix H 10 Agreement Initiatives/ Strategies Medically Complex Patients (7.1, Appendix G, #5) $10 Million will be reserved for October 1, 2013 – October 1, 2014 in order to develop demonstration projects for medically complex patients (post-discharge, on-going) to measure results, to be evaluated after one year. Bilateral Process between OMA/MOHLTC PSC to develop a bilateral monitoring and accountability process to monitor and evaluate initiatives within this PSA. Specific components include: o MOHLTC/OMA Responsibilities (8.1) o Measurement and Evaluation Process (8.2) o Workplan (8.3): o Development of a Sub-Committee (8.4): o Assessment of Bilateral Monitoring and Accountability Process (8.5): o Amendments to Data-Sharing Agreement (8.6) CPSO Complaints Process (9.1) Request by the OMA to the MOHLTC for the amendment of the Health Professions Procedural Code such that CPSO will not be tied to a full investigation into complaints about matters outside their jurisdiction Increase Contribution of CMPA Payments (10.1, Appendix H) OMA/MOHLTC to enter into negotiations with the CMPA to replace the current agreement (2013 expiry) with a new agreement (2022 expiry) OMA/MOHLTC will request across-the-board increases of 2.1% between 2015-23, based on the average of the Consumer Price Index10 between 2001-2011 In 2014, physician contribution will increase the greater of $200 or 22% o Interns and residents, clinical fellows exempted from increase Increases will be revised if Ontario’s CPI exceeds 4%. Tort Reform Measures (10.2) OMA/MOHLTC to review and update tort reform measures recommended by the OMA/MOHLTC/CMPA Medical Malpractice Coverage Committee in 2001, including reforms for: o OHIP subrogation o Prejudgment interest o Family Law Act awards o Limitation of general damages Effective Date (1.3; Section A, Appendix A) Physician Services Appendix to Physician Agreement Services Agreement (1) Comments on Potential Impact October 1, 2013 October 1, 2012 Recommendations for legislative amendments (March 2014) October 1, 2012 June 2013 Measures changes in the price level of consumer goods and services purchased by households in a particular period 12 Last Revised: 2/9/2016 CONFIDENTIAL 2012 Physician Services Agreement: Overview Key Issues Impacting Hospitals Reference format in ‘Agreement Initiatives/ Strategies’ column: Section Physician Programs Section 11 Appendix I Committees Section 12 Appendix J 11 Agreement Initiatives/ Strategies Continuance of Physician Programs (11.1, Appendix I, Section 1) 22 total physician programs will be continued, as outlined in Appendix I. Of interest to hospitals may include: o Emergency department coverage demonstration project o Hospital pediatric stabilization program o Hospital on-call coverage program (HOCC) o Divested psychiatric physician hospital funding o Northern physician locum initiative Modified Programs (11.1, Appendix I, Section 2) Modification of the ED Summer Incentive to restrict access to the Summer Incentive to highest need hospitals, including: o Rural-Northern Physician Group Arrangement hospitals with 2 physicians and 24hour emergency coverage o ED Coverage Demonstration Project (EDCDP) participating hospitals o EDCDP Regional Referral Centres o Fee For Service (FFS) physicians practicing in hospitals with total volumes of 30,000 or less no longer eligible Discontinued Programs (11.1, Appendix I, Section 2) 1. Service Recognition Program: funding to remain in Physician Services Budget (PSB). 2. HOCC Collaboration Fund: $22 Million fund established to recognize physicians in each LHIN where a comprehensive regional on-call coverage program is in place and aligned to the community needs. $22 M will be repurposed in the PSB. 3. Technical Fee Payment: $15 Million fund established for selected technical fees (t-fees) for eligible diagnostic services11 in the 2008 PSA discontinued, as was always meant to be a one-time payment. $15 M has been paid out. Continued Bilateral Steering Committees (12.1) Bilateral subcommittees in this section will continue under their respective terms of reference, subject to revisions indicated below Joint Forms Committee (12.1, Appendix J, Section 1) The mandate of the Committee is expanded to include: o Fees for Forms (including Out of Country forms) o Review of undervalued and unremunerated government forms o Standardize hospital forms that require physician input o Review of document requirements for the exceptional access program process (S. 16 of Ontario Drug Benefit Act) Effective Date (1.3; Section A, Appendix A) Physician Services Appendix to Physician Agreement Services Agreement (1) Comments on Potential Impact October 1, 2012 October 1, 2012 Discontinuance: October 1, 2012 October 1, 2012 October 1, 2012 October 1, 2012 October 1, 2012 Neurology, allergy testing, gastroenterology, neurology, physical medicine, ophthalmology, pulmonary functions, nuclear medicine, mammograms (MOHLTC, 2011) 13 Last Revised: 2/9/2016 CONFIDENTIAL 2012 Physician Services Agreement: Overview Key Issues Impacting Hospitals Reference format in ‘Agreement Initiatives/ Strategies’ column: Section Agreement Initiatives/ Strategies Non-Fee-For Service Agreements Section 13 Appendix K Primary Health Care Committee (12.1, Appendix J, Section 2) PHCC will be tasked with developing implementation strategies for the initiatives established in Section 4, including: o Expansion of Excellent Care for All Act to primary care (including development of Quality Improvement Plans) o Daytime access o House calls o Review of the access bonus o Payment change: (a) Comprehensive Care Management fee reduction for large rosters and (b) acuity modifier o Interprofessional health provider funding (i.e. Physician Assistants in primary care) Non Fee-for-Service (NFSS) agreements (13.1) Standard agreements will facilitate the negotiation of future NFFS contracts with the MOHLTC. Agreements require physicians to require arbitration to resolve any disputes with the MOHLTC regarding the interpretation and application of the NFFS agreement. Standard NFFS agreements will apply to specialist and primary care NFFS agreements. Specialist NFFS Agreements (13.1) Entered into or renewed after the date of this PSA (with adjustments to the template as needed) Primary Care NFFS Agreements (13.2) OMA/MOHLTC to begin negotiating standard template for primary care NFFS agreements. Terms from the specialist NFFS agreements will apply. Review Existing Primary Care Agreements to Standardize (13.3) OMA/ MOHLTC will review existing primary care agreements to standardize/ update terms Recommendation will be made to PSC OMA request to permit non-voting shares of a Medicine Professional Corporation (MPC) to be held by a family trust (14.1) MOHLTC acknowledges OMA request MOHLTC to lead consultation with CPSO, Ministry of Finance and others by and report back to the PSC with recommendations OMA request that corporations whose voting shares are held by physicians and partnerships of physicians be allowed to hold voting shares of MPC (14.2) MOHLTC consultation to begin in January 2013 MOHLTC to provide status report to PSC by June 2013 Recommendations brought forth by the PSC in 2014 Incorporation Section 14 Effective Date (1.3; Section A, Appendix A) Physician Services Appendix to Physician Agreement Services Agreement (1) Comments on Potential Impact October 1, 2012 October 1, 2012 January 31, 2013 January 31, 2013 Review/ recommendations by June 2013 January 1, 2013 14 Last Revised: 2/9/2016 CONFIDENTIAL 2012 Physician Services Agreement: Overview Key Issues Impacting Hospitals Reference format in ‘Agreement Initiatives/ Strategies’ column: Section Statutory Amendments Section 15 Term and Renewal Section 16 OMA Representation and Negotiation Rights Agreement (Memorandum of Agreement) Agreement Initiatives/ Strategies Statutory Immunity (15.1) MOHLTC to support legislation (upon return of Legislature) providing statutory immunity from litigation against the OMA’s directors, officers, members, employees, agents for ‘acts done in good faith’ Legislation to be applicable when the OMA: 1. Enters into agreements with the MOHLTC/ government (e.g. PSA) 2. Makes recommendations to the MOHLTC/ government regarding fee codes or other matters affecting physician payments Term and Renewal (16.1) PSA to begin on October 1, 2012 and terminate on March 31, 2014 Negotiations to establish next PSA will begin no later than January 1, 2013 OMA/MOHLTC agreed to negotiate in accordance to process identified in the OMA Representation and Negotiation Rights Agreement (OMA Memorandum of Agreement) OMA Representation and Negotiation Rights Agreement (Refer to Memorandum of Agreement) Future negotiations to be conducted in accordance with process set out in OMA Representation and Negotiations Rights Agreement: o OMA recognized as exclusive representative of physicians o Parties agree to negotiate ‘in good faith’ in accordance with Joint Process (below) o Minister will negotiate all template agreements12 (and amendments) with the OMA o Minister may not deal directly with a Physician Group in respect of negotiating ancillary agreements13 if majority of Group elects to have the OMA as its representative o All current and future template and ancillary agreements will include OMA as signatory Physician Services Committee o Will continue to provide broad process for regular liaison between MOHLTC/ OMA o Expanded mandate Dispute Resolution Process o Either party may refer disagreement to PSC for consideration o PSC may enlist support of agreed upon facilitator o Facilitator may issue written recommendations for resolution to parties Effective Date (1.3; Section A, Appendix A) Physician Services Appendix to Physician Agreement Services Agreement (1) Comments on Potential Impact October 1, 2012 October 1, 2012 October 1, 2012 12 Template agreement is a funding agreement that the Minister intends to offer to more than one group of physicians Ancillary agreement is either (a) unique agreement that provides funding to a specific group of physicians in a NFFS basis or (b) template agreement when it is applied to and entered into with a specific group of physicians 13 15 Last Revised: 2/9/2016 CONFIDENTIAL 2012 Physician Services Agreement: Overview Key Issues Impacting Hospitals Reference format in ‘Agreement Initiatives/ Strategies’ column: Section Agreement Initiatives/ Strategies o Physician Services Appendix to Physician Agreement Services Agreement (1) Comments on Potential Impact Matters unresolved within 2 weeks from written recommendations will be made public and affected groups may use any other available dispute resolution process Amending Procedure o OMA/MOHLTC may amend this agreement by providing other party with written notice of proposed amendments o Parties must operate in ‘good faith’ when reviewing proposed amendments o If parties are unable to reach an agreement respecting the proposed amendment within 60 days of the written notice then either party may refer the dispute to a special committee of the PSC for consideration o Special committee will make written recommendations within 30 days of referral o Special committee may then enlist support of agreed upon facilitator to help parties to reach a resolution Term of Agreement o Will come into effect when Minutes of Settlement abandoning OMA Supreme Court Case 344/12 are executed Joint Process o Phase 1: Negotiation and Facilitation Parties to commence negotiations at least 4 months before end of PSA term Parties agree to bilaterally negotiate for no longer than 120 days After 120 days any party may request a facilitator for remainder of negotiations Facilitator will issue written recommendations to both parties if after 14 days of his or her appointment a resolution cannot be reached Parties will reconvene within 14 days of recommendations to continue negotiations o Phase 2: Conciliation Conciliator will issue written recommendations to both parties if after 14 days of his or her appointment a resolution cannot be reached Parties will reconvene within 14 days of recommendations to continue negotiations (negotiations no longer than 10 days) Minister will not advise the government to unilaterally implement decisions unless Joint Process occurs Neither party will seek to end negotiations prior to conclusion of Joint Process Effective Date (1.3; Section A, Appendix A) 16 Last Revised: 2/9/2016 CONFIDENTIAL 2012 Physician Services Agreement: Overview Key Issues Impacting Hospitals Reference format in ‘Agreement Initiatives/ Strategies’ column: (1.3; Section A, Appendix A) Physician Services Appendix to Physician Agreement Services Agreement (2) If you could identify the key issues for the OHA to focus on during the implementation of the 2012 PSA, what would they be? Please list your issues in priority order and be as specific as possible. Priority Issue #1: Priority Issue #2: Priority Issue #3 17 Last Revised: 2/9/2016 CONFIDENTIAL 2012 Physician Services Agreement: Overview Key Issues Impacting Hospitals Reference format in ‘Agreement Initiatives/ Strategies’ column: (1.3; Section A, Appendix A) Physician Services Appendix to Physician Agreement Services Agreement (3) Please list any general comments, concerns, or questions you may have regarding the 2012 Physician Services Agreement: 18 Last Revised: 2/9/2016