Rheumatology - SLE - Oxford Medical Education
Systemic Lupus Erythematosus (SLE, lupus)
Definition of SLE o An inflammatory, multi-system autoimmune disease with a relapsing-remitting course with a wide spectrum of severity of disease
Epidemiology of SLE o Incidence of SLE is5/100,000 in the U.S. o Ethnic incidence: Afro-Caribbean>Asian>Caucasian o Peak age of onset of SLE 20-40 o Females:Males = 9:1
Aetiology of SLE (lupus) o Genetics
Monozygotic twins 25% vs dizygotic 3%
Multiple genes found to be more common in patients with SLE o Hormonal influence
Disparity in incidence between men and women is reduced post-menopause age
Potentially an infectious trigger but uncertain
Anti-TNF therapy can induce lupus o Some drugs can induce a lupus-like syndrome
E.g. Hydralazine, methyldopa, penicillamine, minocycline
Drug induced SLE is associated with HLA DR-4
Pathophysiology of SLE (lupus) o Possibly a defect in apoptosis that upsets immune tolerance mechanisms o T-cell abnormalities o Circulating immune complexes
Presentation of SLE (lupus) o Systemic – fatigue often a prominent feature o Arthritis – usually affecting small joints, may be asymmetrical and pain often out of proportion to swelling
Jaccoud’s arthropathy: A deforming non-erosive polyarthropathy with ulnar deviation and
MCP subluxation, deformities can be reduced o Renal disorder (Lupus nephritis): presents with proteinuria, haematuria, ARF, CKD, hypertension, nephrotic syndrome
1 = sedimented
2 = mesangial
3 = proliferative <50%
4 = proliferative >50% (most are in this category)
5 = membranous
6 = sclerosed o Serositis
Pleuritis – pleuritic chest pain
Pericarditis – often asymptomatic
Peritonitis – recurrent episodes of diarrhoea & abdominal pain o Mucocutaneous
Photosensitivity
Malar rash – fixed erythema over the malar eminences
Oral ulcers
©Oxford Medical Education 2014. All rights reserved.
No part of this document may be reproduced or shared without permission of Oxford Medical Education.
Discoid rash – erythematous, raised patches of keratotic scale, which progress to atrophic, depressed lesions. Affects ears, cheeks, scalp, chest, forehead
Raynaud’s
Livedo reticularis o Pulmonary
Pneumonitis
Interstitial lung disease
PE
Cardiac
Myocarditis
Libman-Sachs endocarditis – atypical sterile clusters of vegetations on posterior mitral valve leaflet o Neurological disorder
Seizures
Psychosis
Psychiatric symptoms e.g. depression anxiety very common and often under-recognised
Headache
Aseptic meningitis
Investigations in SLE (lupus) o FBC
Anaemia, leukopenia, lymphopenia, thrombocytopenia o ESR raised disproportionate to CRP (which is usually relatively normal) o Complement
Low in disease flares
Rising complement implies response to treatment o Immunology
ANA +ve in 99% (some controversy over whether ANA negative SLE really exists)
Anti-Sm (pathognomonic but poor sensitivity)
Anti-dsDNA
Sensitivity 70%
Anti-Ro and anti-La antibodies in about 15% (And increase the risk of neonatal heart block)
Anti-histone Ab in drug induced lupus
Rheumatoid factor – positive in 25%
Anti-cardiolipin/lupus anticoagulant/anti B2 glycoprotein o Biopsy
Renal
Skin - often shows complement and immunoglobulin deposits at dermo-epidermal junction o Imaging dependant on organ involvement
CXR, CT, echo, renal US, MRI can all be appropriate
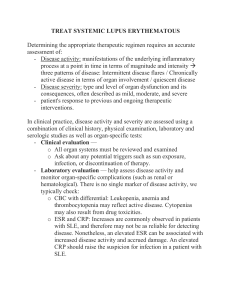
Treatment of SLE (lupus) o Lifestyle
UV protection
Minimise cardiovascular risk factors
Patient education o Hydroxychloroquine - cornerstone of treatment
Reduces flares and improves fatigue
Prolongs life
May be sufficient treatment for mild disease e.g. skin or musculoskeletal o Paracetamol and NSAIDs for analgesia o Steroids
Short term courses for flares
©Oxford Medical Education 2014. All rights reserved.
No part of this document may be reproduced or shared without permission of Oxford Medical Education.
o DMARDS
Dependant on disease manifestations
Consider methotrexate for chronic arthritis
Azathioprine or mycophenolate in moderate disease
CNS or renal involvement requires aggressive treatment o High doses steroids o Azathioprine or mycophenolate o Cyclophosphamide (remember many patients are women of child-bearing age so can be difficult)
Ciclosporin
May require multiple agents o Biologics
Used in refractory disease
Rituximab (anti-CD20)
Belimumab (blocks B lymphocyte stimulator)
Complications of SLE o Cardiovascular disease (x5) o Infection o Antiphospholipid syndrome (APLS) o Osteoporosis
Prognosis in SLE o 5-year survival is 95%
Infection and cardiovascular disease key causes of mortality o Prognostically poor features in SLE:
Multi-system disease
Lupus nephritis
Men o Drug-induced lupus improves once drug stopped
©Oxford Medical Education 2014. All rights reserved.
No part of this document may be reproduced or shared without permission of Oxford Medical Education.