Senior Level: Asthma Management - Center for Health Sciences
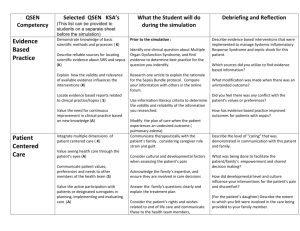
advertisement

Pediatrics - Asthma Management -School Age Child Senior level Program/Curriculum Specific Objectives: 1. The learner will apply health assessment techniques to a school age client 2. The learner will use pharmacology knowledge to provide proper patient education about prescribed medications 3. The learner will demonstrate safe medication administration in a pediatric client 4. The learner will apply principles of coordination of care in considering client referrals 4. The learner will apply principles of management of care in planning for ED discharge 5. The learner will apply appropriate therapeutic communication and interprofessional communication techniques Measurable Objectives 1. Learner completes a school age appropriate intake assessment including information about drug/alcohol use 2. Learner asks child about use of “inhalants” and/or “huffing” frequency 3. Learner administers an IV piggyback medication on a syringe pump using proper technique 4. Learner considers and evaluates child’s need for a referral to social work 5. Learner teaches the child how to administer his home medications using a developmentally appropriate approach 6. Learner addresses inhalant abuse through client/support education and referral Authors: Heather Bissmeyer, Swedish Medical Center; Tiffany Jasperson, Seattle University College of Nursing Date: Spring 2013 Will There Be Any Pre-Simulation Lecture? Yes Duration 15 min Expected Scenario Time: 45 min Expected Debrief Time: 45-90 min Report and Information Provided To Participants Prior To Simulation This is a 10 year old male brought to the ED today by a friend’s parents for a sudden onset of difficulty breathing, wheezing, coughing, dizziness, and a short loss of consciousness. Reportedly, he was with his friend, when symptoms developed suddenly. The client reports that he would normally use his albuterol inhaler, but he didn’t have it with him at his friend’s house. HEET V Grant Simulation Scenario Template 2013. Excerpts adapted and used by permission from National League for Nursing's & Laerdal Medical Corporation's Simulation Design Template (2008), and Northwest Medical Center's Scenario Planning Worksheet (last accessed March 2013). 1 Background This 10 year old male has had multiple clinic and emergency department visits for asthma exacerbation and upper respiratory infections. Asthma diagnosed at age 2yrs. No history of intubations or ICU admissions. Asthma managed at home with pulmicort mdi and albuterol mdi. He has been in the foster care system since birth. Assessment Vital Signs: T 98.6F, HR 90, RR 34, BP 100/80, SPO2 93% on room air General Appearance: Child appears of average height, weight, and nutrition for stated age. He presents as shy, quiet, making little or no eye contact, and in moderate respiratory distress. Cardiovascular: Sinus rhythm, no murmurs Respiratory: Nonproductive cough, tachypnea, subcostal, intercostal, and suprasternal retractions, wheezing in all lung fields GI: Active bowel sounds in all 4 quadrants GU: No reported problems with urination. No current concerns. Extremities: Moving all extremities well and symmetrically, good strength in grips, arms, feet, and legs Skin: Warm, dry, and pale. Flushed cheeks. No clubbing. Good turgor. Neurological: Alert and oriented to person, place, and time; Pupils equal, round, and reactive to light and accommodation. No neurological deficits. Shy and anxious. Shaky. Pain: Reports of pain of 3-4 in his throat and lungs when he coughs Labs: Capillary Blood Gas: pH 7.34, pCO2 49 mm Hg, HCO3 22 mEq Medications: The respiratory therapist started James on Albuterol 9mg continuous neb inhalation x 1 hour per provider orders and it is still running Recommendation: Complete a more detailed history and physical regarding presenting symptoms. Consider inhaled bronchodilator for wheezing and IV corticosteroid to decrease respiratory inflammation Reading Assignments: Review your nursing care of children textbook or the American Academy of Pediatrics website (www.aap.org ) to read about the assessment, nursing care, medications, and patient teaching involved in school-age children with Asthma. HEET V Grant Simulation Scenario Template 2013. Excerpts adapted and used by permission from National League for Nursing's & Laerdal Medical Corporation's Simulation Design Template (2008), and Northwest Medical Center's Scenario Planning Worksheet (last accessed March 2013). 2 Review your nursing care of children textbook or the American Academy of Pediatrics website (www.aap.org ) to read about: Developmental Milestones of the School Age Child Review your nursing care of children textbook, mental health textbook, or X regarding appropriate health screenings for drug/alcohol abuse in the school-age child Review your nursing skills/procedures text on the procedure for IV drug administration Review your pharmacology textbook or online formulary for information on inhaled bronchodilators and inhaled and IV corticosteroids Guiding Questions: 1. What is included in an ED intake assessment for a pediatric client? 2. What are reasons a school-age child might experience an asthma exacerbation? 3. What are current evidenced-based interventions for school-age children with asthma? 4. What interprofessional services might be involved in the care of a school age child with asthma in the ED? What are their roles? 5. What are risk factors associated with drug/alcohol abuse in pediatric clients? Patient Information Patient Name: James Evans Age: 10 yrs. Gender: Male Birth date: April 7 Weight: 30 kg Height: 136 cm Hx. Present Illness: Presents to the emergency department with wheezing, coughing, dizziness, and short loss of consciousness. Was with friend when symptoms developed suddenly. Social History: In foster care since birth – no biological parental involvement, Multiple foster care homes. HEET V Grant Simulation Scenario Template 2013. Excerpts adapted and used by permission from National League for Nursing's & Laerdal Medical Corporation's Simulation Design Template (2008), and Northwest Medical Center's Scenario Planning Worksheet (last accessed March 2013). 3 Religion: None Support System: Brought in to the emergency department by friend’s parents. Lives with foster mom, dad, and two foster siblings Allergies: NKDA Immunizations: Unknown if up to date Attending Physician: Dr. Heather Hill Past medical history: Asthma diagnosed at age 2yrs. multiple emergency department visits for wheezing and upper respiratory symptoms. No history of intubations or ICU admissions. Asthma managed at home with pulmicort mdi and albuterol mdi. Physical description of how you want the manikin to present at start of scenario? Moulage: Manikin dressed in baseball cap, jeans, t-shirt, too big shoes. Have backpack and cell phone at bedside or in bed Assignment of Roles (Color Key) Primary Nurse Physician/ Advanced Practice Nurse Respiratory Therapy Pharmacy Social Services Unlicensed Assistive Personnel/CNA/MA Observer roles Developmental/Communication Focus, Positive Feedback Focus, Constructive Criticism Focus, Safety Focus Other: Friend’s parent or parents Important Information Related To Roles: Primary Nurse: Your role is as manager and coordinator of care. You may delegate tasks to other appropriate personnel on the healthcare team. Physician/ Advanced Practice Nurse: Your role is as the ED provider in this scenario. You are busy, but kind. You know this client from his multiple ED visits, but need a little reminding about his history. Your role in this scenario is to provide proper HEET V Grant Simulation Scenario Template 2013. Excerpts adapted and used by permission from National League for Nursing's & Laerdal Medical Corporation's Simulation Design Template (2008), and Northwest Medical Center's Scenario Planning Worksheet (last accessed March 2013). 4 medication and treatment orders to the nursing staff upon receiving a proper SBAR report. Respiratory Therapy Your role in this scenario is to conduct respiratory assessments and recommendations to the healthcare team when necessary. You may be asked to initiate and manage the respiratory interventions in this scenario. Pharmacy: Your role in this scenario is to provide consultation for other members on the healthcare team regarding medications and medication administration. You also may be asked to provide patient/family education about new or discharge medications. Social Services: Your role in this scenario is to provide consultation on the social needs of this child during a crisis. Your emphasis is on assessing the child and family’s social network and resource strengths and encouraging them to rely on those existing resources. You also assess for areas of social service and network weakness and provide suggestions on available social resources. Unlicensed Assistive Personnel/CNA/MA: Your role in this scenario is to take vital signs on the pediatric client and provide any basic care that is delegated to you. You can provide input to the healthcare team from your perspective. If playing the role of an MA, you can also be delegated to administer medications and/or perform teaching. Other: Observer roles: If you have learners observing the simulation it is helpful to give them active observation foci. These are suggestions and you can always add more: Developmental/Communication Focus: During the simulation, your role is to observe and take notes for feedback on pediatric developmental issues that arise Additionally you will take notes on your observations regarding team communication and communication with the family and child Positive Feedback Focus: During the simulation, your role is to observe and take notes on things that went well during the simulation (e.g. hand washing, working as a team) Constructive Criticism Focus: During the simulation, your role is to observe areas where the participating learners may want to improve in the future (e.g. more detailed SBAR report). For this role, it is helpful to use statements like: “I noticed” and “When I saw you do X, I didn’t understand why. Can you clarify what you were thinking?” Safety Focus: During the simulation, your role is to observe and take notes on safety issues that arise during the scenario (e.g. during medication administration) HEET V Grant Simulation Scenario Template 2013. Excerpts adapted and used by permission from National League for Nursing's & Laerdal Medical Corporation's Simulation Design Template (2008), and Northwest Medical Center's Scenario Planning Worksheet (last accessed March 2013). 5 Friend’s parents: Your role is to be kind and cooperative, but not very knowledgeable or willing to get involved other than to get the child medical help. You are distressed as you can’t get ahold of the foster parents. Your knowledge of the client is that he is “troubled” but you think he is a “good kid who has just had a tough life.” SIM Setup Mannequin IV site : Pediatric simulator or task trainer arm Site _Right hand_______ Gauge _22g___ Fidelity (choose all that apply to this simulation) Setting/Environment ER Medications and Fluids: IVPB: Dexamethasone per IV syringe pump Labs Values: after drawn – capillary blood gas Props: Equipment attached to manikin: O2 via continuous nebulizer ID band Other: IV saline locked with extension tubing Documentation Forms: Physician Orders Flow Sheet MAR Triage Forms Equipment available in room: Crash cart c airway devices and emergency meds Fluids Other: IV syringe pump Other Props: Continuous nebulizer in place on child upon start of scenario Recommended Mode for Simulation Manual/Programmed Hybrid Manikin to be used: high fidelity pediatric manikin or standardized patient Significant Lab Values Capillary Blood Gas pH 7.34 pCO2 49 mm Hg HCO3 22 mEq Physician Orders Dexamethasone 4mg IV x 1 Albuterol 9mg continuous neb inhalation x 1 hour Upon discharge: Albuterol 2 puffs (216 mcg) every 4 to 6 hours as needed Pulmicort flexhaler (budesonide) aerosol, powder 1 puff (180 mcg) twice daily HEET V Grant Simulation Scenario Template 2013. Excerpts adapted and used by permission from National League for Nursing's & Laerdal Medical Corporation's Simulation Design Template (2008), and Northwest Medical Center's Scenario Planning Worksheet (last accessed March 2013). 6 Scenario Progression Outline Stage 1 Initial Amount Time in Initial Stage 0 - 5 mins Baseline Vital Signs T PR 98.6, 90, 34 BP 100/80 SPO2 93% Cardiac Rhythm Sinus Breath Sounds wheeze, stridor Heart Sounds Normal, S1, S2 Abdominal Sounds Normal Other Symptoms: Eyes open, half closed, or closed Trending: VS ↑ or↓ over time Verbalization (Pt/Manikin Cues) Patient is coughing and still a little dizzy and “feels fuzzy” He is quiet and shy but cooperative. If asked, he will admit to “huffing” if not in front of friend’s parents Expected Interventions Wash hands Check patient’s ID band for name and birthdate Incorrect Treatment Choice That Will Affect Outcome Failure to ask about allergies can lead to an allergic reaction or negative side effect to administered medications. Confederate Actions/Additional Role Player Cues Friend’s parents are concerned but visibly uncomfortable. They want the child to be well-cared for, but feel overwhelmed. Ask about the child’s allergies to medications Consider/discuss issues of consent due to parental absence HEET V Grant Simulation Scenario Template 2013. Excerpts adapted and used by permission from National League for Nursing's & Laerdal Medical Corporation's Simulation Design Template (2008), and Northwest Medical Center's Scenario Planning Worksheet (last accessed March 2013). 7 Correct Treatment Choice Stage 2 Timing Sequence Expected Interventions Stage 1: 15 min *1 hour time acceleration from Stage 0 Baseline Vital Signs T PR 98.6, 90, 34 Intake assessment BP 100/80 of school age SPO2 93% child including Cardiac Rhythm Sinus questions about Breath Sounds wheeze, drugs/alcohol stridor (e.g. inhalants and Heart Sounds huffing) Normal, S1, S2 Abdominal Sounds Removal of Normal continuous Other Symptoms: nebulizer and evaluation of the Verbalization effect after it is “I’m dizzy.” “I feel complete. fuzzy.” Coughing. “It’s hard to breathe.” “I’m Provide SBAR feeling better with the report to provider nebulizer.” Admit to the huffing if If proper asked not in the information is presence of the friend’s given to the parents. provider and in SBAR format, the provider should order: Dexamethasone 4mg IV x 1 Incorrect Treatment choice Stage 2a Learners forget to remove nebulizer Timing Sequence Expected Interventions Stage 1: 15 min *1 hour time acceleration from Stage 0 Baseline Vital Signs Learners remove T PR 98.6, 90, 34 nebulizer and BP 100/80 complete and SPO2 93% evaluation of the Cardiac Rhythm Sinus treatment including Breath Sounds wheeze, a full set of vital stridor signs. Heart Sounds Normal, S1, S2 Provide SBAR Abdominal Sounds report to provider Normal Other Symptoms: If proper information is Verbalization given to the “Can I take this off my provider and in face? I think it is done.” SBAR format, the provider should order: Dexamethasone 4mg IV x 1 Consider referral to social work Consider referral to Social Work HEET V Grant Simulation Scenario Template 2013. Excerpts adapted and used by permission from National League for Nursing's & Laerdal Medical Corporation's Simulation Design Template (2008), and Northwest Medical Center's Scenario Planning Worksheet (last accessed March 2013). 8 Correct Treatment Choice Stage 3 Timing Sequence Expected Interventions Stage 2: 5 min Baseline Vital Signs T 98.6 Assessment of IV P 108 site R 26 BP 100/80 Administration of SPO2 96% IV Cardiac Rhythm Sinus dexamethasone Mild expiratory wheeze Heart Sounds Normal, S1, S2 Abdominal Sounds Normal Other Symptoms: Verbalization “What are you doing with my IV?” “Will it hurt.” “That feels cold.” Incorrect Treatment choice Administer IV dexamethasone incorrectly by fast direct IV push Stage 3a Timing Sequence Expected Interventions Stage 2: 5 min Baseline Vital Signs Call provider to T 98.6 report medication P 108 administration R 26 error BP 130/90 SPO2 96% Cardiac Rhythm Sinus Mild expiratory wheeze Heart Sounds Normal, S1, S2 Abdominal Sounds Normal Other Symptoms: Verbalization “Hey can you leave me alone.” Correct Treatment Choice Alternate Treatment choice Learners teach child about dangers of huffers Stage 4 and inhalants Stage 4a Timing Sequence Expected Interventions Timing Sequence Expected Stage 3: 10 min Interventions Stage 3: 10 min T 98.6 P 108 Evaluation of Baseline Vital Signs Learners assess R 26 respiratory T 98.6 child for BP 100/80 symptoms after P 108 background of SPO2 96% previous R 26 using huffers and Cardiac Rhythm Sinus interventions BP 100/80 inhalants Mild expiratory wheeze SPO2 96% Heart Sounds If proper Cardiac Rhythm Sinus Assess readiness to Normal, S1, S2 information is Mild expiratory wheeze change behavior Abdominal Sounds given to the Heart Sounds Normal provider and in Normal, S1, S2 Teach child about Other Symptoms: SBAR format, the Abdominal Sounds the dangers and provider should Normal effects of Verbalization order: Other Symptoms: huffers/inhalants “So I need to do this myself?” “Why do I Albuterol 2 puffs Considers or have to learn this?” (216 mcg) every 4 Verbalization provides resources to 6 hours as “Can I go home now?” to child and or HEET V Grant Simulation Scenario Template 2013. Excerpts adapted and used by permission from National League for Nursing's & Laerdal Medical Corporation's Simulation Design Template (2008), and Northwest Medical Center's Scenario Planning Worksheet (last accessed March 2013). 9 needed Pulmicort flexhaler (budesonide) aerosol, powder 1 puff (180 mcg) twice daily Teaches child about home medication administration at a developmentally appropriate level “I don’t want to come back here.” “But I feel good when I huff.” “This is how my friends and I get away.” “We escape this way.” “It’s not gonna hurt me long term.” “It’s just for fun.” “I could stop if I want.” friend’s parents on prevention and recognition of inhalant abuse What will be discussed in Debrief? Student observers will provide feedback to the group on: o Developmental/Communication Focus; What went well with the developmental approaches of the team to the toddler? What went well with team or foster parent communication? What might you do differently in the future? o Positive Feedback: What went well during your observation of this patient care scenario? o Constructive Criticism Focus: What would you like to see done differently? o Safety Focus: Were there any safety issues that you observed? Please describe what you noticed. When parents aren’t present, how does consent for care work with a pediatric client? What resources did you have available in the ED to you to help you care for this client (i.e. interprofessional team members, teaching materials, etc.)? What referral resources will be appropriate for this child in the community? What did it feel like to approach the child/family about drug, alcohol, inhalant use? Why did you choose your particular approach? (e.g. child alone, friend’s parents in room) HEET V Grant Simulation Scenario Template 2013. Excerpts adapted and used by permission from National League for Nursing's & Laerdal Medical Corporation's Simulation Design Template (2008), and Northwest Medical Center's Scenario Planning Worksheet (last accessed March 2013). 10 Instructor Check List (return to CHESC assistant at the end of class) Pre-Scenario Check List 1. 2. 3. 4. 5. 6. 7. 8. Equipment is staged as requested. The learner has been oriented to the simulator. The learner understands the guidelines/expectations for the scenario. Participants understand their assigned roles. The time frame Expectations for simulation met: Yes No. The time frame Expectations for debrief met: Yes No. Audio/Visual Consent signed and turned into CHESC sheet. Attendance sheet completed and given to CHESC staff. Post Scenario If you could change anything next time, what would it be? Comments: ________________________________________________________ ________________________________________________________ ________________________________________________________ CHESC Assistant Name: Did the person provide excellent support for the scenario? Yes No Comment Instructor signature ________________________________ Date ________________________ HEET V Grant Simulation Scenario Template 2013. Excerpts adapted and used by permission from National League for Nursing's & Laerdal Medical Corporation's Simulation Design Template (2008), and Northwest Medical Center's Scenario Planning Worksheet (last accessed March 2013). 11 Participant Check List (return to Instructor at the end of class) Pre-Scenario Check List 1. 2. 3. 4. 5. I have been oriented to the simulator. I understand the guidelines/expectations for the scenario. I understand the assigned role. My questions about the simulation have been answered. I have all necessary equipment for the simulation. Post Scenario If you could change anything next time, what would it be? Comments: ________________________________________________________ ________________________________________________________ ________________________________________________________ ________________________________________________________ Participant Signature ____________________________________ Date ________________________ HEET V Grant Simulation Scenario Template 2013. Excerpts adapted and used by permission from National League for Nursing's & Laerdal Medical Corporation's Simulation Design Template (2008), and Northwest Medical Center's Scenario Planning Worksheet (last accessed March 2013). 12 Simulation Post-Assessment Methods Checklist Tests Evaluations Turning Point Jeopardy Other Literature References Hockenberry, M. & Wilson, D. (Ed). (2011). Wong’s Nursing Care of Infants and Children, (9th Edition). Mosby Elsevier: St Louis. Hockenberry, M. (Ed.) (2011). Wong’s Clinical Manual of Pediatric Nursing, (9th edition). Mosby: St Louis. INASCL Board of Directors. (2011). Standard III. Participant Objectives. Clinical Simulation in Nursing. 7(4), p. S10-S11, doi: 10.1016/j.ecns.2011.05.007) INASCL Board of Directors. (2011). Standard VI: The Debriefing Process. Clinical Simulation in Nursing. 7(4), p. s16-s17. doi:10.1016/j.ecns.2011.05.010 Jeffries, P. (2012). Simulation in nursing education: From conceptualization to evaluation. (2nd ed.). New York, NY: National League for Nursing. Jones, J. S., Fitzpatrick, J. J., & Rogers, V. L. (2012). Psychiatric mental health nursing: An interpersonal approach. New York, NY: Springer. Martinez, F. (2009). Managing childhood asthma: Challenge of preventing exacerbations. Pediatric, 123(3), p. S146 -S150. doi: 10.1542/peds.2008-2233D National Heart, Lung, and Blood Institute. (2007) National Asthma Education and Prevention Program Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. Bethesda, MD: National Institutes of Health. Retrieved from http://www.nhlbi.nih.gov/guidelines/asthma/ asthgdln.pdf O’Malley, P. (2012). This pretty balloon might kill you: the rise of inhalant abuse and resources for practice. Clinical Nurse Specialist, 26(4), p. 200-202. doi: 10.1097/NUR.0b013e31825d8f86 HEET V Grant Simulation Scenario Template 2013. Excerpts adapted and used by permission from National League for Nursing's & Laerdal Medical Corporation's Simulation Design Template (2008), and Northwest Medical Center's Scenario Planning Worksheet (last accessed March 2013). 13 Debriefing Guidelines (Remember to identify important concepts or curricular threads that are specific to your program) 1. Leave the simulation room and go to a conference room, if possible. It allows for deescalation of emotions. 2. Solicit and validate emotions briefly. Validate simisms (the simulation isn’t 100% accurate due to different equipment, personnel etc.) 3. What went WELL in this simulation? 4. What DID NOT go well in this simulation? 5. If you could do it again, what would you do differently? 6. Summarize: “What I hear you saying is . . .” HEET V Grant Simulation Scenario Template 2013. Excerpts adapted and used by permission from National League for Nursing's & Laerdal Medical Corporation's Simulation Design Template (2008), and Northwest Medical Center's Scenario Planning Worksheet (last accessed March 2013). 14