Carter_Philipp_Abstract_2015
advertisement

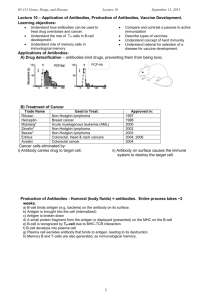
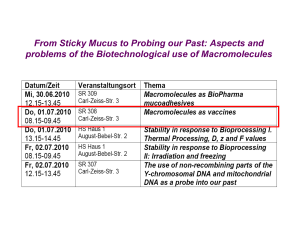
Mechanism-based design of conjugate vaccines against drugs of abuse Philipp Carter1, Megan Laudenbach2, and Marco Pravetoni2,3 1 Graduate program in Pharmacy, University of Basel, Switzerland. 2 Minneapolis Medical Research Foundation, Minneapolis, MN. 3 Department of Medicine and Pharmacology, University of Minnesota, MN. Vaccines may offer a promising therapy for drug addiction. Small molecules, such as oxycodone or nicotine, are made immunogenic by conjugating them to large, foreign carrier proteins to elicit serum antibodies that bind drug in serum, prevent its distribution to brain, and subsequently block drug-induced behavior. However, eliciting high levels of drug-specific serum antibodies has remained one of the biggest challenges in translating these vaccines to human use. Current clinical-stage vaccines showed proof of efficacy only in a small subset (~30%) of immunized individuals that had high antibody titers. Novel strategies are needed to develop more effective addiction vaccines. Understanding the immunological mechanisms involved in generating drug-specific antibodies is critical for improving vaccine efficacy Generation of effective serum antibodies against drugs of abuse is the result of vaccineinduced T cell-dependent B cell activation, which largely occurs via germinal center (GC) formation in secondary lymphoid organs. Our group has previously shown that the number of naïve and activated hapten-specific B cells, before and shortly after immunization, correlates with vaccine efficacy in vivo. Here, we hypothesized that vaccine efficacy may be enhanced by targeting downstream pathways involved in GCdependent B cell responses. To test this, we co-administered a promising candidate oxycodone conjugate vaccine with a series of adjuvants and immunomodulators known to regulate GC formation and compared hapten-specific B cells, oxycodone distribution, and oxycodone-induced antinociception within these groups. Our preliminary data suggests that co-administration of IL-4 and IL-6 modulates vaccine efficacy against oxycodone. Furthermore, IL-2 signaling was blocked by co-administering mAbs directed against the α-chain of IL-2 receptor (also known as CD25), which enhanced the efficacy of our vaccine. In contrast, interference of the programmed death-1 (PD-1) signaling pathway negatively affected vaccines efficacy. Results suggest that modulating specific downstream regulators of GC-dependent B cell responses (and subsequent antibody production) can improve vaccine efficacy, but a better understanding of GC formation is needed to greatly improve antibody response. The long-term goal of these studies is to develop more effective vaccines by combining conjugate immunogens with immunomodulators and polymer-based delivery platforms.