Technology - The Co-Creativity Institute
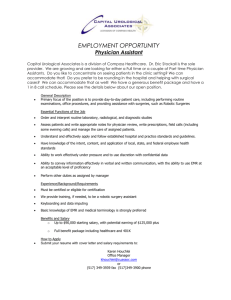
advertisement

UNIVERSITY OF ILLINOIS HOSPITAL & HEALTH SCIENCE SYSTEM MGMT 590 November 29, 2012 Amrita Ghoshal Hongyan Pei Liz Pisney Maggy Tieche Neeta Venepalli 1 BACKGROUND The University of Illinois Hospital & Health Science System (UIHHSS) is one of the largest medical research districts in Illinois, and integrates three university systems, seven health science colleges including the College of Medicine, and two Federally Qualified Health Centers (FQHCs). UIHHSS consists of a 496 bed tertiary hospital, an outpatient facility with multiple diagnostic and specialty clinics and 19 neighborhood clinics through Chicagoi. In 2011, UIHHSS saw the following: 18,201 inpatient admissions; 490,155 outpatient visits; 2,633 births; 6,288 inpatient surgeries; 41,176 emergency department visits. Approximately 360 physicians and 1175 nurses are on staffii. UICHSS’s mission is to “leverage its unique combination of clinical care, health sciences education and biomedical research in providing high quality, cost effective healthcare for the people of the State of Illinois and delivering personalized health in pursuit of the elimination of racial and ethnic health disparities”iii. Important priorities for the UIHHSS are to improve clinical outcomes and quality metrics as measured through criteria established through the Joint Commissioniv, and Centers for Medicare and Medicaid (CMS)v and patient satisfaction as measured through the Press Ganey Surveyvi, while reducing overall expenses. After review of the UIHHSS strategy five specific organizational goals have been selected: 1. Decrease 30 day hospital readmissions and hospital acquired infections 2. Improve patient experience in the inpatient setting 3. Improve CMS core measure objective scores 4. Formalize quality improvement plan with data collection and benchmarking for individual physicians 5. Reduce expenses and improve financial status of organization Through the following situational and resource analysis, we propose strategy recommendations focused on optimization of the current electronic medical record (EMR). We also explore UIHHSS’s uncertainties and how to prepare for them. STRATEGY OVERVIEW In 1995, UIHHSS implemented Cerner’s PowerChart electronic medical record (EMR) to 2 manage patients’ health records electronically. The implementation improved patient care through improved data management and communication. Currently, the EMR links to the inpatient and outpatient setting and is integrated with radiology, laboratory and pharmacy. It includes e-prescribing (eRx), computerized provider order entry (CPOE) and clinical decision support (CDS) assistance. Because of its outstanding performance on infrastructure, business and administrative management, clinical quality and safety and clinical integration; UIHHSS was selected as one of the Most Wired Hospitals in 2012 for the sixth year in a rowvii. Review of the UIHHSS competitive landscape shows that there is more to be gained by continual optimization of Cerner PowerChart with regards to the afore mentioned organizational goals. The following resource analysis shows how this can be achieved by first evaluating the status of UIHHSS’ finances, operations, marketing, design and engineering and information systems. The following situational analysis identifies opportunities for strategic changes. RESOURCE ANALYSIS: FINANCES UIHHSS’s finances are a portion of the entire University of Illinois’ budgetviii. Annual reports list hospital and other medical activities for revenues, expenses and health services’ assets and liabilities (Figure 1) with June 30, 2011 as the most recent fiscal year end. The limited breakout of financial figures and lack of specifics for UIHHSS, such as total equity and inventory, prohibits a complete financial analysis. The hospital and other medical activities have had negative net revenue for the last three fiscal years, with 2011’s at -$86,627 million. A number of factors contribute to the growing expenses, including employee compensation and the rising cost of care. The current ratio of 2.9 shows ability to cover debt with liquid cash, even with negative net revenue. The debt-to-asset ratio is 0.42, showing low risk and the ability to gain financing. There may be fewer liabilities attributed directly to the hospital and it retains valuable land assets that helps keep these ratios in check. Liabilities reduced from 2010 to 2011, which may indicate that even with a negative margin, UIHHSS has the ability to pay down its debt. 96 percent of payment comes from insurance companies, indicating an incoming source of cash for services rendered. In 2011 the hospital provided over $16 million in charity care, which is care provided to patients who are underinsured or are without insurance. 3 (in thousands) 2011 2010 Operating revenue $547,168 $576,852 Operating expense 633,795 597,426 Net revenue -86,627 -20,574 Current assets $259,453 $249,605 Total assets 415,854 406,680 Current liabilities 9,0080 129,698 Total liabilities 173,116 176,605 Figure 1: University of Illinois Annual Reportix RESOURCE ANALYSIS: MARKETING UIHHSS markets to two consumer groups: patients and medical services payers. Patients are encouraged to use UIHHSS’s services while insurance companies cover the cost of these Net margin (net revenue/operating revenue) Current ratio (current assets/current liabilities) Debt-to-assets ratio (total debt/total assets) services. -1.6% -3.6% 2.88 1.92 0.42 0.43 UIHHSS’s slogan is “Changing medicine. For good.” and their message emphasizes providing equal care to all patient types, especially for groups with health disparities. In early 2012, the hospital underwent a rebranding, which reflected the organization change of combining all health related university activitiesx UIHHSS must attract new patients and ensure patients continue to receive ongoing care and services. For some patients, how doctors, nurses and other staff treat them encourages them to continue to seek treatment from UIHHSS. Promoting the patient’s involvement in their overall health creates a consumer base that is knowledgeable and driven. The MyHealth xi website is a resource for patients to participate in their care with news and general health information. Current and recent marketing activity includes traditional print and radio campaignsxii, a YouTube channel featuring patient storiesxiii, an online magazine highlighting stories about the system and emphasizing the quality of care providedxiv and television segments about specific clinical services for news outletsxv. UIHHSS can enhance MyHealth to allow patients to view their patient record, test results, schedule appointments, make payments and consult with health care providers. 4 Since the majority of payment for health services comes from insurance companies and government aid, UIHHSS also has an obligation to seek sufficient payer options. UIHHSS accepts 26 insurance plansxvi, in addition to Medicare and State and Federal programs. RESOURCE ANALYSIS: DESIGN UIHHSS consists of a 496 bed, inpatient hospital with seven specialized intensive care units and an ambulatory facility with multiple sub-specialties. The hospital has 8 floors; 5 dedicated to inpatient care and 3 including radiology, surgery suites, the cafeteria and administration offices. Each floor is divided into two to three units and categorized by sub-specialty (for example: 8W is an oncology area and 8BMT is the stem cell transplant area). Each unit has a central nursing station equipped with computers, a nursing staff room, and hospital beds extending in a line from the nursing station. The hospital has a combination of single and double rooms, and reserves single rooms for patients with hospital acquired infections or those requiring isolation. Computer workstations are located primarily in the nursing station, with two to three computers located in other areas of the unit. The medication carts are located at the nursing stations in close proximity to the computers and the nursing staff rooms. Except for the intensive care unit rooms, inpatient rooms lack computer stations and the hospital has few mobile workstations. The hospital has wireless capabilities that are free to all patients and staff. Cerner PowerChart is a fully integrated system with electronic order entry and charting, clinical decision support, medication alerts and e-prescribing used in inpatient units and ambulatory clinics. Multiple providers can access patient records although only one provider can input orders at any time. Currently, there are no portals connecting patients to their hospital records, or allowing patients to communicate with their providers electronically through Cerner. Although partially paperless, UIHHSS still relies heavily on paper; electronic orders printed by nursing staff after placed by the providers and paper copies of patient imaging/labs/discharge instructions being given to the patient. RESOURCE ANALYSIS: OPERATIONS UIHHSS’s inpatient operations and supply chain management are complex but similar to other tertiary hospital centers and involve multiple ancillary systems that run in parallel. These include laboratory, pharmacy, radiology, housekeeping, food delivery, transport (patients and 5 materials), surgical suite management, admissions and discharge coordination. At the epicenter of operations is the physician-nurse-pharmacy-patient interaction. Currently most of the physicians’ and nurses’ time is spent on the computer rather than face-toface time with patients. Daily work flow in the inpatient setting revolves around three physical foci: computers location, medication room, and patient rooms. Daily workflow is physically centered on areas of the floor with computer stations and medication carts: 1. At shift changes, nurses and residents give verbal reports about overnight events to their counterparts 2. Residents print rounding reports, which include vitals, medications and labs 3. Residents ‘pre-round’ and physically visit every patient and spend about 5-10 minutes examining them and talking with them about their clinical situation 4. Attending physicians then re-round with the residents, either by sitting in the resident room (where there is access to a computer for updated labs) and then visiting each patient’s room or by ‘rounding at the room’ 5. Residents break away from rounds to place electronic orders into the computer as they have time. Residents also break away to place orders requested by the nurses. 6. Nurses receive orders electronically, and then must chart with each order implementation 7. Patients call for nurses through the intercom systems that are answered by a receptionist at each nursing station, who then verbally communicates patient requests to the nurses. 8. Medications are stored in a central medication holding area in each nursing station; each patient has a ‘bin’ in which their medications are stored which are manually delivered by pharmacy technicians. ‘STAT’ medication orders are sent via tube stations. There is no bar code administration closed loop system for medications as of yet, although this is being planned for December 2012. RESOURCE ANALYSIS: INFORMATION SYSTEMS The process of implementing and maintaining a system to facilitate electronic medical records is 6 three-fold: automate, informate and transform.xvii The first level automation was complete with Cerner PowerChart. The system changed some of the clinical workflows. The second order of change, to informate is when the roles of the actors involved within the system have changed as a result of the automation. It is important that UIHHSS continue to have a set plan for training new employees on use of the system as part of an on-boarding process as well as ways to train all users on upgrades or changes. The last type of change, to transform is when information systems and technology permeate to the point that they flatten the organization and have bearing on organizational structure and roles. UIHHSS has not realized many of the transformational changes at this time, but can soon, through the use data harvesting. For example, the EMR has the potential to store more than just prescription and discharge information. Databases could store elapsed time between treatments/visits or provide insight into a patient’s return because of an unresolved complaint. The manual, paper based processes and workstation centric order entry seem to have reduced time actually interacting with the patients. Transformational changes can begin to happen by redesigning the mobility of the technology and further improving the workflow – which will ultimately lead to more time interacting directly with patients. With UIHHSS’s research facility, collected data can drive analytics to identify gaps in care and services. UIHHSS would need to ensure their databases are not only accessible for reporting, but that they have the talent to harvest and in turn, interpret the data. The following value creation framework (Figure 2) demonstrates how value can be added to a customer (in this case patient) relationshipxviii: Figure 2: Value Creation On the left vertical axis is the theoretical repurchase frequency (low to high, bottom to top) and the horizontal axis is the degree of customizability (low to high, left to right), with UIHHSS 7 represented by the star. In this instance, patients at UIHHSS have a substantial “repurchase frequency” as everyone will need healthcare throughout their lives and the opportunity to use data to customize the experience of and care for a patient is high. As described, this data can not only improve healthcare operations, but also benefit the patient by tailoring to their needs. UIHHSS has an opportunity to add value to their patients by providing EMR access along with customized tools and information based on their healthcare needs. Security of patient data is a cornerstone of any EMR system. It is crucial that the UIHHSS ensure not only the patient data is kept securely, but that there is also enough storage space for records and data to be housed. UIHHSS must ensure they have solid planning for server uptime, redundancy and capacity. SITUATIONAL ANALYSIS SWOT ANALYSIS Strengths Strengths of UIHHSS are that it is affiliated with the largest and best medical schools in the country. Care is provided locally in Chicago, across the region and the state of Illinois and is provided regardless of patient ability to pay. Weaknesses Weaknesses of UIHHSS are that it is financed by the state of Illinois, which means that fiscal trouble for the state can translate into funding issues for the system. Traditionally, healthcare has not been a highly profitable business. And finally, population changes move demand for care over time, which makes strategic planning and resource allocation a challenge. Opportunities There are many opportunities for UIHHSS to gain a competitive advantage as the landscape of care is at a transformational stage. Overall, there is a greater focus in the US than ever before on adopting healthy lifestyle choices. Robust employment of an EMR system can help patients make and commit to those changes. Threats 8 Threats also loom large for UIHHSS. With the increased use of technology, competition for healthcare services and information has increased dramatically. This has informed patients more than ever and influences how they select their healthcare provider. As federal funding has shifted and changed, there are more limitations that not only affect how patients care can be funded, but also how aspiring caregivers such as doctors and nurses can fund their education. The latter of the two greatly affects maintaining a knowledgeable staff and recruiting over time. PORTER’S FIVE FORCES ANALYSIS Competitive Rivalry within the Industry (High) UIHHSS has five major competitors (Figure 2): Loyola University Medical Center (LUMC) Rush University Medical Center (RUMC) University of Chicago Medical Center (UCMC) The John H. Stroger, Jr. Hospital of Cook County (CCH) Northwestern Memorial Hospital (NMH) UIHHSS is the smallest of the five hospitals. The affiliation relationship of UIHHSS and University of Illinois at Chicago (UIC) Health Science Colleges does not bring any extra competitive advantage as other hospitals are also affiliated with a medical university or college. As UIHHSS highly relies on government aid, federal policy changes will affect its capital resource. If any organization does not have its initiative to control its capital, it may reduce the flexibility when determining strategy. All hospitals other than UIHHSS have their own specialized care center, something which distinguishes their brand or image. Each comparison hospital uses an EMR. Bargaining Power of Suppliers (High) The main suppliers of UIHHSS are medical equipment, pharmaceuticals, insurers, doctors and nurses. UIHHSS’s state funding creates limitations when compared with private university hospitals. This also limits the hospitals bargaining power. As private hospitals or clinics enter the industry, doctors, nurses and insurers bargaining powers also increase. 9 From suppliers of medical equipment and pharmaceuticals, UIHHSS can get data - storage, consuming, costs, outcomes, and readmission rates associated with those products, then join group-purchasing organizations to increase bargaining power. Doctors and nurses are also suppliers to the hospital and should optimize their services by utilizing products like EMR to improve operational procedures, reduce cost and waste of human resource and time. Threat of new entrants (Low) Two important considerations when evaluating new entrants are the level of attractiveness and barriers to entry. Traditionally healthcare is said to be a local business because providers must deliver services to patients in person. Advances in technology and communication, as well as the ability to recruit providers nationally, some aspect of the physician - patient relationship is no longer true. The challenge of streamlining patient care through digitized medical records, e-prescription programs, and online hospital communication, has gained some momentum, giving younger companies a chance to make inroads. With a $19 billion federal stimulus to develop new health information tracking technology, health IT employment is expected to grow by 18 percent through 2016xix. When considering income as a key indicator of industry growth, it can be concluded that the industry would be moderately attractive to potential entrants. There are a number of complications faced by potential new entrants. The capital cost involved to open a new hospital will be substantial. Long lead times are required to find the actual site, purchase land, gain various approvals and finally build the hospital. Still probably, the most difficult would be to recruit and secure the optimum mix of referring medical practitioners. Therefore, a general conclusion would be that it would be relatively unattractive to enter this industry by way of setting up new facilities. The most likely entry strategy would be through the acquisition of an existing operation. 10 UIHHSSxx LUMCxxi RUMCxxii UCMCxxiiixxiv CCHxxv NMHxxvi Ownership State Government Private Non Profit Public Hospital Number of beds Specialized Care Center 485 569 676 Private Non Profit 532 Private Non Profit 897 Outpatient diagnostic and specialty clinics, two Federally Qualified Health Centers (FQHCs) Cardinal Bernardin Cancer Center, Ronald McDonald Children's Hospital, Heart & Vascular, Orthopedics, Transplantation, Women's Health Cancer, Heart, Neurology, Orthopedic Women’s, Men’s, Senior’s, Pediatric, and Pregnancy. Bernard A. Mitchell Hospital, Comer Children Hospital Chicago Lying-in Hospital, Duchossois Center Level-1 Trauma Center, Hospital-Eye Clinic, the Sable/ Sherer Clinic Profile of Patients Accepts most insurance plans & governmental programs Accepts most insurance plans, including many HMO, PPO and POS plans and Medicare, Loyola also offers financial assistance and charity care. Accepts about 80 participating products and about 40 noncontracted products Accepts more than 100 products. Accepts all major health insurance plans and managed care programs including: Medicare and Medicaid, Blue Cross, Aetna/US Healthcare, Keystone Health Plan East, etc. Usage of Electronic Health Records (EHR) Implemented in 1997, and involved in every aspect of work flow. e-Renewal of prescription medications & e-prescribing Uses an electronic system called Epic The leader in using of EMR from registering, scheduling appointments, diagnosing to prescribing. Epic EMRs Epic EHRs More than 80% of work is done via EMR to including patient chart, prescribing and providers' documents Epic EMRs They upgraded the security of EMR by replacing the traditional “Box” PC to Clear-Cube PC Blades and User Ports. EMRAM scorexxvii ~4 ~4 6 ~4 ~3 6 Figure 3: Academic Hospital Competition in Chicago 11 464 The Bluhm Cardiovascular Institute, The Kovler Organ Transplantation Center, Maggie Daley Center (woman's health-care), The Robert H. Lurie Comprehensive Cancer Center A variety of managed care, Medicare & Medicaid, PPO,HMO and POS insurance plans are accepted Bargaining Power of Buyers (Neutral) Patients are the main buyers in the healthcare industry. As individuals will get sick or suffer from diseases, they will have to choose a certain hospital or insurance company over another. Since there are a limited numbers of insurance companies within a network or limited number of hospitals within an area, it becomes very hard to have much buyer power in this industry. The general population in the United States either has private healthcare insurance or government insurance. Most private healthcare insurance is paid for by the patient’s employer. Hence, it can be said that employer’s with the ability to decide the kind of insurance to include in the employee’s benefit package make most of the buying decisions. Corporate buyers with several choices of managed care organizations can wield a certain bargaining power towards insurance companies and ultimately the healthcare provider. “Large employers engage in competitive bidding processes with the available health plan. In some cases, employers have moved backwards in the industry value chain to contract directly with hospitals and physician, almost completely removing the health plans and insurers from the chain.”xxviii Threat of Substitute products/services (High) Non-traditional healthcare providers, such as alternative and holistic medicine, are increasingly competing with traditional healthcare providers. Treatment offered by these providers is often at a lower cost, reducing hospital stays or need for costly surgeries. With advances in medical imaging and communication, radiologists can outsource x-ray readings for hospitals at lower prices. Most pharmacies have an additional “service/advice” section offering free medical solutions to patients. Today medical advice can also be offered to patients via the internet. STRATEGY RECOMMENDATIONS To achieve the five organizational goals listed above, we propose that UIHHSS direct resources towards optimization of the current EMR system with the following considerations: 1. Breaking a habitxxix: Assigning more resources towards optimizing the EMR system must also mean fewer resources spent towards something else. Because UIHHSS is dependent on state funding, finances are tightly regulated. 2. Blue Oceanxxx: It is difficult to compete with the four other academic hospitals in 12 Chicago in all areas of excellence. One potential area of growth that is relatively dormant is focusing on telemedicine and mobile health applications for underinsured patients. By expanding use of preventive medicine on the high risk patient populations, there are opportunities to study both health disparities and effect positive changes (for example: diagnosing hypertension or diabetes earlier through piloting remote applications, utilizing automated text messaging for appointment reminders and for annual screening exam reminders, using social media as a health literacy tool). 3. Value Disciplinesxxxi: Focusing on operational effectiveness and customer intimacy are vital for UIHHSS to distinguish itself from its competitors. Hospital-patient relationships are ultimately about personal satisfaction of patients, physicians and hospital employees. Product excellence is harder to focus on without a specific area of excellence, such as University of Chicago’s phase 1 study program, or Northwestern’s Prentice Hospital for labor and deliveries. STRATEGY EXECUTION Rather than trying to innovate in the majority of these areas, UIHHSS can take advantage of existing and empirically validated strategies that have shown success for other hospitals. Creation of SMaCxxxii practices for each of the goals below is vital, and we have included specific components. 1a) Decrease 30 day hospital readmissions A national study of 537 hospitals’ practices for hospital readmission rate reductionxxxiii and other articlesxxxivxxxv help base SMaC practices to reduce preventable readmissions: Implement the national guidelines for care into Cerner templates, and update every 6 months to mandate the proper treatment o Expand clinical decision support to ensure appropriate orders and care with physician and RN notifications (for example: automatic electronic notification if a patient weight on admission is over 10 lbs from last visit) o Create order sets and templates within Cerner to standardize care, and give physicians access to order sets and evidence based guidelines if they should choose alternate orders 13 Monitor patient numbers daily and in real time o IT programs to monitor the percent of patients readmitted within 30 days Create a discharge check list for patients including: o Pharmacy conducted medication reconciliation on the day of discharge o RN counseling for new medications o Follow up appointment scheduled for 7 days post discharge o Discharge instructions including a plan for patients for emergencies o Automated IT alerting of physicians within 24 hours of patient discharge Check in with all discharged patients within 72 hours of discharge via pre-specified patient managed technology with 2-3 questions (are you feeling: better/worse/the same; do you have questions about your medications: yes/no) o Patient portal for email o Mobile applications via phone o Responses requiring follow up will be directed to a health intervention team that will personally contact patient via telemedicine Teach patients that technology can be helpful o Inpatient training of portal and mobile applications and telemedicine by health intervention team with RNs, NPs and PAs 1b) Decrease hospital acquired infections a) Mandate hand washing for all providers on entry and leaving patient rooms a. Increase hand-washing compliance through automated monitoring with or without radiofrequency identificationxxxvi. Privacy concerns and expense of automated systems are two challengesxxxviixxxviii. b) Track infections in real time and automatically a. Purchase and implement infection control software for active infection surveillance and injury detection/prevention systems. Examples of vendors include Cardinal Health Med Mined, TheraDoc Infection Control Assist, Premier Safety Surveillorxxxix. University of Pennsylvania hospitals adopted TherapDoc back in 2007 with a subsequent 90% reduction in the rates of their catheter-associated infections over 3 yearsxl. A less expensive alternative is to 14 develop homegrown infection control software given the strength of the informatics department at UIC. c) Monitor bacteria content in mobile devices, ties, buttons, pends, computers, keyboards in real time with weekly random checks Value added: Providing patients with access to their EMR and personalized health care information will add value to the overall patient experience and make the switching costs for the patients higher than they otherwise would have been. Patients can communicate with their health care team more quickly, and address concerns/fears/illness more quicklyxli. Quantifying infections and hand washing hygiene in real time through health IT software provides data and scope for interventions, resulting in reduced risk of infection for patients which potentially reduces recovery time and need for readmission. 2) Improve patient experience in the inpatient setting (as defined by Press Ganey Survey) Patient satisfaction is an emphasized indicator of health care quality, and correlates with the extent to which physicians fulfill patient expectations. Interestingly, a recent study suggested that patients report the highest levels of satisfaction with their physicians are more likely to be hospitalized, accumulate more health care and drug expenditures, and have higher death rates than those who are less satisfied with their carexlii. Given that Medicare incentive payments will be linked to HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems), UIHSS should focus on patient satisfaction in addition to other quality of care measures (and not only as a surrogate). From an IT perspective, we propose the following SMaC practices: Maximize face time with patients o Mandate computer stations in each patient’s room so physicians and nurses spend more time in the room than at their work station o Place automated medication carts in patient rooms to reduce time for medication administration. o Create ‘smart room technology’ in patients’ rooms similar to a model utilized at University of Pittsburg hospitalsxliii including: a patient screen that lists daily tests/imaging, educational materials, and caregivers a caregiver touch screen for nurses, aides and physicians to quickly 15 document vitals, basic tasks, orders while in the room, which would then automatically upload into the EMR a smart board to replace the currently ‘white board’ that is in each patient room, with caregiver information/updated orders Use formulary medications as the default o Reduce costs for patients with installing formulary list of medications into Cerner’s prescription system; patients will be happier to pay $4.00 (without insurance) for available medications. Teach patients that mobile technology can help them o Demonstrate use of mobile devices, get patient acquainted with care givers using devices, reduces potential conflict or hard feelings on the patient’s side. Value added: Increased quality of interaction and communication between patient and caregivers, and reduced cost of medications. 3) Improve CMS core measure objective scores CMS core measures are a set of 35 health care quality measures for Medicaid-eligible patients to enhance quality improvementxliv. Among the 35 core measures are items like adult BMI assessment, flu shots for adults aged 50-64, antidepressant medication managementxlv. New core measures that will be required by 2014 include the following: secure electronic messaging system for patients and providers track medications from order to administration through electronic medical administration provide patients with ability to view and download their records within 4 days of outpatient encounters and within 36 hours of hospital discharge provide summary of care to patients after each visit conduct electronic health information exchange with another health care organization with different EMR systems To improve CMS core measure objective scores, we propose the following SMaC practices: Prioritize specific core measures: UIHHSS must first prioritize specific core measures and identify which to accomplish through optimization of the EMR. Two necessary steps are development of a patient portal (allowing access to health information and secure 16 messaging between patients and providers, including access to labs/imaging tests/physician notes/summaries of care). Incorporate quality care into the culture of UIHHSS: use leadership, internal marketing to educate all staff as to importance of quality care, use of CMS core measures as a necessary and good tool for reduction of morbidity/mortality, and improvement of patient care and safety Value added: Providing patients with access to their EMR and personalized health care information will add value and empowerment to the overall patient experience and make the switching costs for the patients higher than they otherwise would have been. 4) Formalize quality improvement plan with data collection and benchmarking through EMR Two academic hospitals that are currently operating at HIMSS Analytics Stage 7xlvi utilize Cerner software and 38 academic hospitals currently operating at HIMSS Analytics Stage 6xlvii. UIHHSS can optimize its existing IT systems by expanding its use of Cerner’s business intelligence capabilities to collect and analyze data in real time, with the goal of improving patient care quality, safety, staff productivity, and maximize reimbursement management systemsxlviii. Possible SMaC practices include: Gather our data accurately and in real time o Deploy clinical and business intelligence software to gather and report health data o Develop a quality team to analyze results and propose changes or improvements to existing processes proactively, in addition to ongoing analysis of data, and retrospective studies o UIHHSS is affiliated with Vanguard/McNeal hospital, which increases the amount of patient outcomes data. Get our doctors involved in clinical decision template making o EMR systems work best with physician autonomy and access to evidence based data in addition to templates of carexlix. Build internal scoring systems for grading patient care and physician practice, and do internal benchmarking every 2-3 months Reward well performing physicians (through financial or other incentives) in real time 17 Value added: Real time data collection and analysis allows for more rapid detection of errors and problems, and triage issues into those which must be immediately addressed versus those requiring long term planning. 5) Reduce expenses and improve financial status of organization Moving to a paperless system ensures that UIHHSS becomes process and product focused. With medical records and prescriptions all available electronically, costs will ideally be reduced as work flows become streamlined and administrative costs decrease, allowing a higher quality of interaction with the patient. UIHHSS should utilize this opportunity to revamp their reimbursement system, and integrate their billing and reimbursement system with their EMR such that billing is done in ‘real time’ and electronically. Forecast supplies utilized (for example: respiratory masks during the winter) and purchase during slack periods Develop financial derivatives for patients Move to paperless system! o Become process and product focused by moving to a paperless system and ensure properly coded and billing via the EMR. o Utilizing less paper and storage for paper records, and streamlining work flows will result less overhead, and more time to spend with patients rather than finding records/doing paperwork Value added: Reduce labor cost, duplicative tests and more timely accounts receivable and billing. Through implementation of all the goals outlined above, overall patient satisfaction and experience will increase significantly. At the same time, using technology to communicate and provide information to patients in an elegant way will ultimately increase switching costs for existing patients and incent new patients to use UIHHSS. ADDRESSING STRATEGIC UNCERTAINTIES The most difficult aspect of designing a corporate strategy is the unpredictable future events. In order to combat against future uncertainties, we performed a PEST analysis followed by 18 “bullets”l, which are ways UIHHSS can plan for these unpredictable events. Political The U.S. Government has incented or driven recent EMR adoption. The endeavor in and of itself is highly charged with potential regulatory issues. However, those are all predictable and anticipated within the scope of strategy. More extreme events are unplanned and could affect the proliferation of EMR systems and initiatives. For example: Lack of support for health information exchanges at the state level: lack of continuity throughout the system threatens consistency and reliability for patients as well as the greater initiative. Biological warfare or endemics: flooding the system with urgent patient needs may override the systems capabilities. Record keeping would take a back seat to triage and treatment. Change in drug patent laws: potential drug shortages or the movement of consumers to the Canadian drug markets. Lack of control over prescription drugs can threaten patient’s safety and complicate diagnosis and care by physicians. Decreases in Medicare/Medicaid funding: a reduction in support from the government for publicly funded or subsidized healthcare threatens the overall system as less payment would be available for services. Bullets Collaborate with international drug companies to acquire lower cost prescription drugs or promote generic drug use to reduce patient cost. Explore health information exchanges regionally and nationally, starting with sites employing Cerner PowerChart. Infection Surveillance systems are in an early adoption stage and is not realistic in our short term. Instead, we can find other ways to communicate potential outbreaks or illnesses using less sophisticated means. Algorithms can track hospital website and provider search terms in the clinical decision support system and patient portal activity to spot trends. 19 Economic As with any business, economic conditions can strongly influence success. Most EMR initiatives are being implemented during recession conditions (or near to). Further complications to the industry could threaten the EMR initiative as well as the overall healthcare system. Outsourcing of medical care: as costs of healthcare rise in the U.S., more and more patients seek surgical procedures outside of U.S. borders. Not only are medical procedures sought outside of the U.S., but increasingly prescriptions are as well. Lack of control over prescription drugs can threaten patient’s safety and complicate diagnosis and care by physicians, which translates to loss of revenue for the healthcare providers. Increase in insurance costs: as cost of healthcare increases, so does insurance. Also, the new nationalized health care may drive costs up, still yet to be seen. Either of these could leave patients uninsured, which will choose either to go without treatment or force healthcare systems to write off more procedures. Decrease in state funding: as more and more state governments reach a fiscal crisis and one looming for the federal government, much of the funding provided may be at risk. Additionally, all of this culminates in markets where the cost of procuring credit needed for capital investments becomes much more difficult. Mergers/Acquisitions: should revenues and funding become more troublesome, UIHHSS either can merge or become acquired by another healthcare provider, thereby putting its unique project and goals on the back burner. Decreases in Medicare/Medicaid funding: a reduction in support from the government for publicly funded or subsidized healthcare threatens the overall system, as fewer payments would be available for services. Bullets Explore small clinics, through partnerships with drugstores and pharmacies like WalMart, Target, CVS and Walgreen’s. These clinics are staffed by registered nurses and physician assistants who provide a quicker meeting and usually less expensive care. Explore partnerships with academic affiliates internationally to benefit from patients seeking care outside of the U.S. 20 Create medical care futures, derivatives and combinations. The hospital and patient sign a contract for care in the future. The patients who worry about the recurrence of an old illness or a hereditary disease would be interested in these kinds of futures, because it would be cheaper than traditional care. The hospital receives the money in advance, which can fund medical technologies, or improving all equipment. Selling the medicine as a combo, just like a fast-food restaurant. Lists all unit prices of medicine and procedures and patients can choose which suits them best and buy at a discount. For example, before the winter one can purchase a check-up and test for sinus infections and antibiotics before they receive care. Social Social threats are those posed when new norms and trends threaten the strategy or goals of the organization. Trends point towards heavier use of social media and a stronger, faster, more global conversation. Social networks slowing endemics/pandemics: with our greater interconnectedness, there is possibility that social networks can act quicker than viruses, alerting people to take precautions sooner, thereby reducing healthcare needs. Decreased quality of "bedside manner": as physicians incorporate technology into the exam room and clinical settings, there is risk of a loss of personal touch. This in turn could drive patients away to various alternatives healthcare resources. Expectations of care: again, as social media and technology proliferates, patients have greater access to information and known alternatives. If care is not of expected levels, based on new benchmarks provided by friends, wikis and blogs, this may drive patients to various alternatives. Bullets Monitor social media to understand patient conversations and concerns. Have a team in place to respond to questions posed via Facebook, Twitter, etc. If conversations become unfavorable, activate a team to address root causes of the patient dissatisfaction and remediate processes as needed. 21 Generate communication and a social network around the patient portal system both internally and externally to encourage use. Build awareness of the benefits among caregivers by demonstrating and obtaining feedback. Pass this knowledge on to patients. Distribute multi-lingual pamphlets to waiting areas and with discharge summaries. Use demographics of current patients to mail post cards explaining the portal benefits. Start with patients who tend to schedule more appointments or are in the offices more frequently to find early adaptors. Nurses take part by explaining the new system at the beginning and end of patient visits. Build communities around physicians (especially those specializing in an area of care) and their patients both in person and online. Facilitate care and build a support network. For example, a physician specializing in cardiology can create online groups/social networks comprised of their patients with similar/related conditions. Connecting others with similar concerns can give the physician a more streamlined method of communication to the entire group and also facilitate the conversation within the group as well, in which they can communicate with the physician and each other. Create a culture of quality interpersonal relationships and patient care and safety first: use internal team building, marketing, benchmarking and rewarding to clarify to health care providers that technology should not be an impediment to quality interactions with patient care. The intersection of technology and interpersonal patient-physicians relationships is changing, but through education of patients and health care providers both, it should be made clear that the culture at UIHHSS is patient care and safety first. Retraining physicians and nurses how to better interact with patients through integration of mobile technology will be essentialli. Pilot strategies that clarify expectations to patients on provider mobile device use, set up rooms such that computers are arranged in conducive areas for patient interaction, mandate at least 5 minutes of in person interaction with each patient by the attending physician during rounds and utilization of mobile technology for accurate assessment of patient comfort/painlii. 22 Technology Technology can be both a blessing and a wild card for businesses today. There is rapid movement as capabilities grow and new businesses emerge. At the same time, implementing technologies in large organizations needs to be done with great care and planning. Implementing change: as addressed in the Resource Analysis, a large part of employing a strategy heavily relying on technology is how the users within the information system will interact with the technology. Lack of adoption or engagement could be a serious threat to the system’s viability and therefore the hospital’s future. Interoperability failures: as UIHHSS employs new EMR technology, so do the majority of healthcare providers. As these are rolled out independently, interoperability could become a major issue for both patients and doctors alike. Moving between healthcare providers could become incredibly difficult and cumbersome without the collaboration on a clear set of metadata in record keeping. Lack of regulation of IT systems: the need to establish clear guidelines and service level agreements for tool providers may be legislated to protect patient’s data. If healthcare providers do not keep this in mind, it could come at a serious cost to remediate at a later date. Loss of power, natural disasters: with disasters like” super storms” or hurricanes coming more and more prevalent, the reliability of technology may be questioned. Tool providers and adopters in the healthcare system will need a failover plan for accessing data at times when they may need it the most. Bullets Release patient portal in stages with an implementation timeline and schedule for roll out. Start with basic functionality such as bill pay and move to online patient appointment requests. Success here may even reveal shortcomings in the use of patient and physicians’ time. Make patient test and laboratory results retrievable through the portal next. This would eliminate a caregiver having to call the patient with test results; patients see them as they become available. If an additional visit or test is required from the result, the patient can use the system to make such a request. Allow patient access to their complete personal health information. Make a system for physicians in conjunction, so they can 23 access all patient records and communicate with them from any location. This will create a standard to manage expectations and an outline for a 20 Mile Marchliii. While younger patients already tend to access health information electronicallyliv, observing how the market evolves and how other hospitals execute a similar plan provides a longer-term approach. The hospital does not have to try to implement and release all features at once; make shorter-term goals and march towards achieving each one. Develop informatics tools to predict which patients are at highest risk for readmission (elderly, multiple conditions) to intervene more quickly and be prepared for them. Administration spearheads the strategy execution. Study and discuss with peers about what tactics worked for others. By creating the strategy, they give guidance on the objectives for different operating units. They should thoroughly understand their role in the organization and for which horizon they must planlv. Executives must expect that only continued dedication to a plan would reap resultslvi. In UPMC’s “top down, bottom up” approach, executives defined the path the hospital should take but also sought information from day-to-day work on how they might achieve what they set out to dolvii. Adhering to the specific goals helps continue to create the outline of the 20 Mile March. Executives serve as the intermediary between the board and hospital employees, so they must seek board support and link the steps they outline to strategic visionlviii. Outline departmental workflow that guide IT implementation. We can expect workflows to change with the introduction of new technology. Anticipating for these changes will help deal with surprises or changes to routine. Each department can map their workflows and help to integrate their specific needs into the documentation process. As the system rolls out to units, track the challenges and successes to make adjustments. The knowledge creates a toolbox to work from when approaching new issues. Getting providers involved early on in the process helps them to adapt to the changelix and allows them to see how they contributed to the overall success of the processlx. Standards of data sharing and system interoperability – need to ensure the systems are set up so they can talk to each other. Explore any current interoperability standards used in the industry and devise ways in which the hospital can contribute to the creation of standards. These standards will not only ensure that the hospital’s goals are met but will also allow the sharing of data across organizations. This is not only an objective of 24 CMS’s Meaningful Use criterialxi, but it also has the possibility of providing better care to patients. Physicians can share specific patient data to understand one’s history but health care system’s can also track population health to better the entire community. ADDRESSING THE BACK UP PLAN To implement an EMR system successfully, it must be integrated through a well-designed process and into a receptive culture. Successful implementation not only requires strong executive, clinical and leadership support but also an active involvement by all levels of staff in selection, development and peer education. There is still the possibility of an unexpected disaster resulting in an information system crash. During these times there are certain considerations that the hospital should take to shore up its contingency planlxii. Conduct risk assessment and risk value: determine what health IT systems are most critical and absolutely needed to function. For example, the EMR system and other patient safety/quality systems are crucial to daily operations and cannot endure long downtimes. Accounting systems, revenue cycle systems and education systems are not vital to patient safety during times of emergency. Consider different types of back-up systems: design a back-up system in the order of the risk hierarchy. The hospital decides how much bandwidth they need and how much they are willing to spend to secure this data. There are three types of back up sites including cold, warm and hot siteslxiii. Hot sites are more expensive than cold sites since they back up data at intervals that are more frequent. Healthcare organizations report that they are not adequately prepared for data recovery and back uplxiv, where they would suffer significant downtime. Remain focused and ready to work if crash dies occur: It is important for every hospital staff member to know the risk assessment and contingency plans. If the EMR does crash, the hospital should have a pre-designated team to determine which information is critical to treat patients and retrieve it from the back up site. Stay abreast of government incentive and regulations: The United States government is spending approximately $25.9 billion to promote and expand the adoption of health information technology through the Health Information Technology for Economic and Clinical Health Act, 2009lxv. Between this and the Health Insurance Portability and 25 Accountability Act which looks into the patients privacy issues, health IT is not only encouraged to expand into the hospital system but is also being heavily scrutinized. The need to be well prepared during an unforeseen disaster is also constantly increasing along with the increase in regulation groups and government mandates. Develop individual plans for departments: The data recovery plan should not rest solely on the IT department. As the particular data varies for each individual department, the recovery plans needs to be tailored to their level of importance in patient care. Factor this into the disaster recovery plan. For example some departments cannot have any downtime as even a couple of minutes of downtime could be the difference between life and death for a patient! Prepare for the best and the worst: It is important to start with the worst case scenario and work backwards to develop a plan that covers the hospital for everyday user-driven problems. The most common scenarios requiring an immediate back up plan for the EMR are often human errors or machine failures. Have a recovery plan for when an administrator accidently deletes a file and when the hospital's power supply is cut. Test the plan: The back-up plan should be tested. Apart from documenting their plans, hospitals should also frequently test it, as well as run unannounced spot checks. LEADING ABOVE THE DEATHLINE As there is no reliable way to predict future events, hospitals just like any other organizations need to be prepared for any unexpected occasions that could potentially harm or damage the enterprise in such a way that it can no longer continue. “Hitting the Death Line”lxvi, if followed consistently, will help UIHHSS to avoid hitting the death line. Build Cash Reserves and Buffers: Due to the recent economic recession, UIHHSS along with other healthcare providers are facing challenging environments. To survive UIHHSS must set strict financial goals and measure performance against these goals. Maintaining strong liquidity should be a major factor while establishing these goals. Apart from consistently monitoring daily cash reports and point of service collections, UIHHSS should ensure improvement of their overall revenue cycle by following these steps: Implement a revenue cycle that will allow the hospital to track billing, payments received, allowances and other financial data historically by payer. The system should 26 allow UIHHSS to go back over a period of time and see how much they are receiving for every dollar they are charging Implement online bill pay system for the patients and suppliers Provide incentive to the account collection staff based on achievements of targets on a quarterly basis Build a stronger presence in the community through various outreach and volunteerism programs and in turn gain philanthropic support which will facilitate growth Bounding Risk: With rising cost in healthcare and insurance and a decrease in state funding towards hospital operations, UIHHSS will need to take a more conservative and risk adverse approach. The proposed “bullets” could help the hospital overcome the risk associated with those uncertainties. Zoom Out, then Zoom In: It is important for UIHHSS to remain hyper vigilant to sense changing economic condition and be able to respond effectively. To control rising Medicaid costs, states are limiting hospital coverage to as few as 10 days a year. This move will effectually force hospitals to absorb more cost themselves to care for the poor who will now come to the hospital emergency area more and also lead to higher charges for privately insured patients.lxvii A recent study by Premier, a healthcare improvement alliance shows that readmissions cost a community hospital $3.83 million each year – accounting for up to 9.6 percent of a hospital’s budget – and inappropriate lengths of stay add another $2.63 million in costs – accounting for up to 5.4 percent of a hospital’s budget.lxviii Viewing the environment from above lets us spot the areas in which change may occur and we can zoom in on “bullets” and back-up plans to address those changes. i http://hospital.uillinois.edu/About_UI_Health.html http://health.usnews.com/best-hospitals/area/il/university-of-illinois-medical-center-at-chicago-6430553 iii http://hospital.uillinois.edu/About_UI_Health.html' iv http://www.jointcommission.org/core_measure_sets.aspx v http://www.healthit.gov/policy-researchers-implementers/meaningful-use vi http://www.pressganey.com/researchResources/governmentInitiatives/HCAHPS.aspx vii http://hospital.uillinois.edu/News/Most_Wired.html, http://research.uillinois.edu/newsmedia/20120719/ui-hospital-named-most-wired-list viii http://www.uillinois.edu/our/news/budget/budgetupdate.cfm ix http://www.uillinois.edu/our/news/budget/budgetupdate.cfm x Mallen , Cayce - Interim Associate Director, Branding and Communications, University of Illinois Hospital & Health Sciences System. Interview November 5, 2012. ii 27 xi http://uillinoishospital.staywellsolutionsonline.com/ Mallen , Cayce - Interim Associate Director, Branding and Communications, University of Illinois Hospital & Health Sciences System. Interview November 5, 2012. xiii http://www.youtube.com/channel/UCxVdcB-O7AKBIpUd8ET6mYg xiv http://hospital.uillinois.edu/About_UI_Health/Illinois_Health_Magazine.html xv Mallen , Cayce - Interim Associate Director, Branding and Communications, University of Illinois Hospital & Health Sciences System. Interview November 5, 2012. xvi http://hospital.uillinois.edu/Patients_and_Visitors/Accepted_Insurance_Plans.html xvii Information Systems for Managers, Piccoli, Gabriele, John Wiley and Sons, Inc, 2008, p 35-38 xviii Information Systems for Managers, Piccoli, Gabriele, John Wiley and Sons, Inc, 2008, p 242-244 xix http://www.inc.com/ss/best-industries-for-starting-a-business#2 xx http://hospital.uillinois.edu/News/Most_Wired.htmlhttp://hospital.uillinois.edu/Patients_and_Visitors/A ccepted_Insurance_Plans.html xxi http://www.loyolamedicine.org/Patient_Visitor_Info/Insurance_Information/index.cfmhttp://www.loyol amedicine.org/Learn_About_Us/FAQs/index.cfm#q10 xxii http://transforming.rush.edu/Technology/Pages/Electronic-Medical-Records.aspx https://www.rush-health.com/RHAWeb/InsurancePlans/Default.aspx xxiii http://www.uchospitals.edu/index.shtml xxiv http://www.uchospitals.edu/billing/managed-care.html xxv http://www.johnstrogerhospital.org/dom/insurance.html xxvi http://www.nmh.org/cs/Satellite?q=insurance&c=Page&scat=global&cid=1223924265067&pagename =nm%2FPage%2Fnm%2FTemplate%2Fnm_L01_SearchResults&x=0&y=0 xxvii http://www.himssanalytics.org/emram/index.aspx xxviii Managing Healthcare Business Strategy, Moseley B xxix Barlow, Christopher, M., PhD. Strategy: Synergy and Serendipity. Co-Creativity Institute, 2007. xxx Barlow, Christopher M., PhD. Strategy: Synergy and Serendipity. Co-Creativity Institute, 2007. xxxi De Kluyver, Cornelis A. and John A. Pearce II. Strategy: View From the Top. 2006. xxxii Collins, Jim and Morten T. Hansen. Great by Choice. 2011. xxxiii Bradley, E. H., L. Curry, L. I. Horwitz, H. Sipsma, J. W. Thompson, M. Elma, M. N. Walsh and H. M. Krumholz (2012). "Contemporary evidence about hospital strategies for reducing 30-day readmissions: a national study." J Am Coll Cardiol 60(7): 607-614. xxxiv Austin, L. S., C. O. Landis and K. H. Hanger, Jr. (2012). "Extending the continuum of care in congestive heart failure: an interactive technology self-management solution." J Nurs Adm 42(9): 442-446. xxxv Lagoe, R. J., D. S. Nanno and M. E. Luziani (2012). "Quantitative tools for addressing hospital readmissions." BMC Res Notes 5(1): 620. xxxvi Gould, D. J., D. Moralejo, N. Drey and J. H. Chudleigh (2010). "Interventions to improve hand hygiene compliance in patient care." Cochrane Database Syst Rev(9): CD005186. xxxvii Boyce, J. M. (2011). "Measuring healthcare worker hand hygiene activity: current practices and emerging technologies." Infect Control Hosp Epidemiol 32(10): 1016-1028. xxxviii Polgreen, P. M., C. S. Hlady, M. A. Severson, A. M. Segre and T. Herman (2010). "Method for automated monitoring of hand hygiene adherence without radio-frequency identification." Infect Control Hosp Epidemiol 31(12): 1294-1297. xxxix Monnegain, B. (2009). "Infection control software market poised rapid growth." http://www.healthcareitnews.com/news/infection-control-software-market-poised-rapid-growth xl "University of Pennsylvania Health System Selects TheraDoc® to Monitor Infection Control." http://www.infectioncontroltoday.com/news/2007/02/university-of-pennsylvania-health-system-selects.aspx xli http://www.hospitalimpact.org/index.php/2011/10/19/mobile_apps_could_be_key_to_higher_patie. xlii Fenton, J. J., A. F. Jerant, K. D. Bertakis and P. Franks (2012). "The cost of satisfaction: a national study of patient satisfaction, health care utilization, expenditures, and mortality." Arch Intern Med 172(5): 405-411. xliii Cerrato, P. (2011). "Hospital Rooms Get Smart." http://www.informationweek.com/healthcare/clinicalsystems/hospital-rooms-get-smart/231901129 xliv http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Stage_2.html xii 28 xlv Hagland, M. (2012). "CMS Finalizes Set of 35 Core Quality Measures for the Care of Medicaid-Eligible Adults." http://www.healthcare-informatics.com/news-item/cms-finalizes-set-35-core-quality-measures-care-medicaideligible-adults xlvi http://www.cerner.com/About_Cerner/Awards/HIMSS_Stage_6_and_7/?LangType=1033 xlvii http://www.himssanalytics.org/emram/scoreTrends.aspx xlviii http://www.informationweek.com/healthcare/clinical-systems/cerner-to-buy-clairvia-to-boost-bicapab/231900453 xlix http://www.healthdatamanagement.com/issues/2009_71/-39035-1.html l Collins, Jim and Morten T. Hansen. Great by Choice. 2011. li http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3246857 lii http://www.foxbusiness.com/personal-finance/2012/09/25/improving-bedside-manner-with-technology/ liii Collins, Jim and Morten T. Hansen. Great by Choice. 2011. liv http://www.alliedhealthworld.com/visuals/smartphone-healthcare.html lv Barlow, Christopher M., PhD. Levels of Bureaucracy. Co-Creativity Institute, 1995. lvi Fickenscher, Kevin and Michael Bakerman. Change Management in Health Care IT. PEJ IT Insights, March April 2011. lvii http://www.himssanalytics.org/emram/stage7caseStudyUPMC.aspx lviii Hood, M. Michelle. How CEOs Drive the Clinical Transformation and Information Technology Agenda. Frontiers of Health Services Management, Fall 2011. lix Goh, Jie Mein. Evolving Work Routines: Adaptive Routinization of Information Technology in Healthcare. Information Systems Research, September 2011. lx http://www.himssanalytics.org/emram/stage7caseStudyUPMC.aspx lxi http://www.healthit.gov/policy-researchers-implementers/meaningful-use lxii Bob Herman. 4 Things to know in case of a hospital information system crash. August 8, 2011. http://www.beckershospitalreview.com/healthcare-information-technology/4-things-to-know-in-case-of-a-hospitalinformation-system-crash.html lxiii http://en.wikipedia.org/wiki/Backup_site lxiv Kathleen Roney. 5 Guidelines for Hospital Data Recovery Plans. August 15, 2012 http://en.wikipedia.org/wiki/Health_Information_Technology_for_Economic_and_Clinical_Health_Act lxv http://en.wikipedia.org/wiki/Health_Information_Technology_for_Economic_and_Clinical_Health_Act lxvi Collins, Jim and Morten T. Hansen. Great by Choice. 2011. lxvii Phil Galewitz. October 31, 2011 “States are limiting Medicaid Coverage in Search for Savings” http://www.kaiserhealthnews.org/stories/2011/october/24/states-are-limiting-medicaid-hospital-coverage-in-searchfor-savings.aspx lxviii Emily Mullin. May 7, 2012 : “Ten Ways Hospitals can Save Money”. http://www.dorlandhealth.com/case_management/trends/Top-10-Ways-Hospitals-Can-Save-Money-Targeting-CaseManagement-Functions_2242.html 29