Improved cellular specificity of plasmonic nanobubbles
advertisement

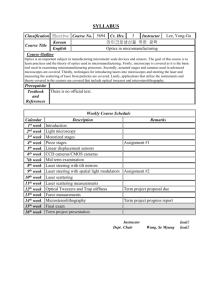
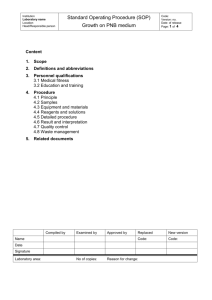
Text S1 for Improved cellular specificity of plasmonic nanobubbles versus nanoparticles in heterogeneous cell systems Ekaterina Y. Lukianova-Hleb, Xiaoyang Ren, Pamela E. Constantinou, Brian P. Danysh, Derek L. Shenefelt, Daniel D. Carson, Mary C. Farach-Carson, Vladimir A. Kulchitsky, Xiangwei Wu, Daniel S. Wagner, Dmitri O. Lapotko 1. Molecular targets and cell models We studied the six cell models representing four molecular targets (Table 1): 1. Epidermal growth factor receptor (EGFR) was studied as specific molecular target in head and neck and lung cancer cell lines. First, we used multi drug-resistant HN31 squamous carcinoma (target) cells (associated with head and neck cancers) with high expression level of EGFR [1, 2] and immortalized normal human oral kerotinocyte NOM9 (non-target) cells. Both cell lines were obtained from The Johns Hopkins Genetic Resoutces Core Facility. The expression level of EGFR was verified with western blot method (Figure S1). The EGFR expression was found to be 2.8 times higher for HN31 target cells compared to non-target NOM9 cells. The NOM 9 cells were cultured in KGM Complete Medium (Cat# CC-3001, Lonza Walkersville Inc, Walkersville, MD) in a 37°, 5% CO2 incubator. The malignant cells were transfected with green fluorescent protein (GFP) to allow identification. The HN31 GFP stable cell line was built by transfecting the EGFP C1 plasmid into HN31 cells. The selecting marker was G418. The transfected cells were cultured in DMEM High Glucose medium (Cat# 10013 CV, Mediatech Inc, Manassas, VA) supplemented with MEM Vitamin Solution (Cat# 11120, Invitrogen Corp., Carlsbad, CA) and MEM NEAA (Cat#11140, Invitrogen Corp., Carlsbad, CA) and penicillin-streptomycin (Cat# 30002 CT), Mediatech Inc, Manassas, VA) in the same incubator. For co-culture, the cells were re-suspended in KGM media and counted after trypsinization and neutralization. NOM 9 was mixed with HN31 cell in 100:1 ratio, seeded at a density of 700,000 cells/ml in 15well chambered slide (µ-Slide Angiogenesis, Ibidi LLC, Martinsried, Germany) and grown 24 hours before NP treatment. The 60 nm hollow gold NSs (2.4*1010 particles/ml) conjugated with Panitumumab antibody were identically targeted to both types of cells in vitro by incubating for 24 hour with a co-culture of HN31/NOM9 cells under physiological conditions (37ºC). After that uncoupled NPs were washed off prior to the generation of PNBs. The viability of the cells was measured after their incubation with NP-conjugates. The viability of cells was found to be 98% for HN31 cells and 96% for NOM 9 cells. In order to determine the role of the targeting vector in cellular specificity of PNBs, we incubated the co-culture of HN31 and NOM9 cells with bare and Panitumumab conjugated 60 nm gold NSP as described above. For combinatorial targeting of cancer surface receptors by the two anti-EGFR body (Panitumumab and C225) we used the 60 nm gold NSP conjugated to Panitumumab antibody and the same NSP conjugated to C225 antibody. The cells were cultivated and treated by NSP conjugates as described above. In the cases of pre-treatment cells by C225 or Panitumumab antibodies alone, the cells were incubated with antibody (30 min, 4°C @ 2µg anitibody/ml), washed off from the uncoupled antibodies and treated by NP conjugates as described above. The viability of cells was more than 98% in all combinations of treatment of cells by NP-conjugates and antibodies. Second, we used the EGFR-positive A549 (target) cells [3-5] (associated with lung carcinoma) and EGFR-negative normal cells, fibroblasts (non-target cells) (cell lines were obtained from the American Type Culture Collection). The cells were grown in RPMI-1640 media for 24-30 hours at 37º C in a CO2 incubator in growth chambers (LabTek II, Thermo Fisher Scientific, Pittsburgh, PA) to 70% confluence. For targeting we used the 60 nm gold 60 nm NSP conjugated with anti-EGFR antibody C225 (BioAssay Works LLC, Ijamsville, MD). The both types of cells were identically incubated with NSP-C225 conjugates (concentration 6*1010 particles/ml) for 30 minutes at 37C in the CO2 incubator. Following incubation, the cells were washed twice by a serum and phenol red free RPMI-1640 media to remove free NPs. Cell viability was measured after NP treatment and was 98% for A549 cells and 98% for fibroblasts and not differed from viability of intact A549 and fibroblast cells (98% and 98%, respectively). 2. Mucin molecule MUC1 was studied as molecular target in HES cells, a derivative of WISH/HeLa cells (kindly provided by Dr D. Kniss, Ohio State University, Columbus, OH). The HES cells with high level of MUC1 expression [6-8] and HS-5 cells with low expression of MUC1 were used as target and non-target cell, respectively. Cells were identically targeted with the gold 60 nm NSP conjugated with 214D4 by BioAssay Works LLC (Ijamsville, MD). HES cells were grown in high glucose DMEM (Life Technologies, Grand Island, NY) supplemented with 5% (vol/vol) FBS (Life Technologies, Grand Island, NY) and 1 mm sodium pyruvate (Sigma-Aldrich, St. Louis, MO). HS-5 cells were grown in low glucose DMEM (Life Technologies, Grand Island, NY) supplemented with 10% (vol/vol) FBS. Cells were seeded in growth chambers (LabTek II, Thermo Fisher Scientific, Pittsburgh, PA) and cultured for 24-48 h before NP treatment. The NSP-214D4 conjugated were re-suspended in phenol red free DMEM media before concentration 2.4*1010 particles/ml. Cell were incubated with the NPcontaining media for 1 h at 37°C in CO2 incubator. After that the cells were washed with fresh DMEM media to remove free NPs. Viability of NP-treated HES and HS5 cells was found to be 90% and 85%, respectively. 3. Prostate Specific Membrane Antigen (PSMA) was studied as a molecular target in C4-2B prostate cancer cells (were obtained from Dr. Leland Chung (MD Anderson Cancer Center, Houston, TX) with high PSMA enzymatic activity [9]. As non-target we used HS5 (human bone stromal cells; were obtained from American Type Culture Collection) with low level of PSMA expression [10]. Both cell lines were grown as described earlier [11]. Both cell cultures were identically targeted with gold NPs using one or two specific cancer surface markers: PSMA that is primarily expressed in prostatic tissues as well as in bone metastases [10, 12] and EGFR that is expressed in prostate cancer and malignancies [13]. Target (C4-2B) and non-target (HS-5) cells were maintained as described previously [14]. Cells were grown to 80% confluence, trypsinized, washed 1 time with PBS, and re-suspended in serum-free low glucose DMEM (Life Technologies, Grand Island, NY). Both cell populations were identically treated (30 minutes at 37 °C in CO2 incubator) with the 60 nm gold spheres conjugated by BioAssay Work LLC (Ijamsville, MD) to PSMA antibodies [15]. After that the cells were washed three times with media, and re-suspended in fresh media before PNBs generation. For combinatorial targeting of two cancer surface receptors we used the 60 nm gold spheres conjugated to PSMA antibodies and the 110 nm silica-gold NSs conjugated to C225 (anti-EGFR antibody) by BioAssay Work LLC (Ijamsville, MD). Cell viability was measured by Trypan Blue staining of intact and NP-treated cells and was found to be 97% and 96% for NP-treated C4-2B and HS5 cells, respectively. 4. Membrane receptor CD3 was studied as molecular target in the two cell models. CD3-positive J32 [16] (target) and CD3-negative JRT3-T3.5 (non-target) clones of Jurkat T-cell leukemia cell lines were purchased from the American Type Culture Collection. JRT3-T3.5 do not express CD3 [17]. Both cell populations were identically treated with the 60 nm gold spheres conjugated with anti-CD3 monoclonal antibody OKT3 (BioAssay Works LLC, Ijamsville, MD). Cells were re-suspended in a serum free RPMI-1640 medium (Invitrogen, Grand Island, NY) containing OKT3-conjugated NPs at a concentration 1.2*1011 particles/ml and incubated with the NP-containing media for 45 minutes at 37°C in CO2 incubator. Following incubation, the cells were washed to remove free NPs and finally suspended in fresh RPMI-1640 medium supplemented with 10% FBS (Atlanta Biologicals, Lawrenceville, GA), 2 mM l -glutamine, 100 units/mL penicillin, and 100 mg/mL streptomycin (Life Technologies, Inc., Grand Island, NY) and placed in growth chambers (Lab-Tek II, Thermo Fisher Scientific, Pittsburgh, PA). Then the cells were treated with laser pulses. The cell viability was tested immediately after treatment of cells by NP conjugates. The viability of J32 and JRT3-T3.5 cells was 96% and 98%, respectively. In another CD3 cell model we used human T-cells. PBMC (peripheral blood mononuclear cells) were isolated from buffy coats (obtained from the Gulf Coast Blood Center, Houston TX), by ficoll gradient. CD3-positive T cells (target) were enriched from PBMC using a Pan T cell Isolation Kit II (Miltenyi Biotec, Inc., Auburn, CA), and CD3negative cells (non-target) were enriched by depletion of CD3-positive cells from PBMC using CD3 microbeads (Miltenyi Biotec, Inc., Auburn, CA) according to the manufacturer’s instructions. The expression levels of CD3 in target and non-target cells were obtained with flow cytometry (Gallios Flow Cytometer from Beckman Coulter) (Figure S2) and showed significant difference: the expression of CD3 in target cells was found to be 25 times higher than in non-target cells. CD3-positive (target) and CD3negative (non-target) cells were incubated at 5*106 cells/ml with the 60 nm gold NSP conjugated (1.2*1011 particles/ml) by BioAssay Works LLC (Ijamsville, MD) with target-specific antibody OKT3 for 30 min at 37ºC, 5% CO2, washed three times with media, and re-suspended in phenol red-free RPMI with 10% FBS for PNB treatment. Cell viability was tested in 72h after NP-treatment and was 98% for CD3+ cells and 97% for CD3- cells. 2. Plasmonic nanobubble generation Optical generation and detection of the PNBs was performed with a photothermal laser microscope that we developed previously [18, 19]. In our work we employed a pulse of length 70ps with wavelength 532 nm or 778 nm (PL-2250, Ekspla, Vilnius, Lithuania) or 500 ps with wavelength 532 nm (STH-01, Standa Ltd, Vilnius, Lithuania) and/or 787 nm (custom made dye laser). Laser beam diameter was 15µm for PNB generation around individual NP clusters and in individual cells and 260 µm for PNB generation in monolayers of co-culture of HN31/NOM9 cells in scanning mode with a covering area of several hundred cells. The laser pulse fluence (10-90 mJ/cm2) was experimentally determined for each pair of the target and non-target cells to exceed the PNB generation threshold in target cells and to be below PNB generation threshold for non-target cells. The fluence of each laser pulse was measured by registering its image and measuring of the beam diameter (at the level of 1/e2 relative to the maximal intensity in the center of the beam) at the sample plane with the imaging device (Luka, Andor Technology, Belfast, Northern Ireland) and by measuring of the pulse energy using a pulse energy meter (Ophir Optronics, Ltd., Jerusalem, Israel). This scheme provided direct and precise measurements of the incident optical fluence at the cell plane for each excitation pulse (Figure S3). Operation of all hardware was controlled by PC through custom software modules developed using the LabView platform. 3. Imaging and metrics for NPs and PNBs To image and quantify the uptake of gold NPs by individual cells we imaged and measured optical scattering by gold NPs in individual cells. As a rule we used laser confocal microscopy (LSM 710, Carl Zeiss Inc, Germany) to obtain the stack of several images per each cell (in case of A549 cells the NP scattering was imaged and quantified with regular inverted microscope). In each population (sample) 30-50 cells were analyzed and the population-average image pixel amplitudes I mean were calculated for each cell sample: 𝐼𝑚𝑒𝑎𝑛 = 𝐾 ∑𝑀 𝑖=1(∑𝑗=1((𝐼𝑠𝑐𝑖,𝑗 −𝐼0 )−(𝐼𝑠𝑐1𝑖,𝑗 −𝐼01 )) 𝑀 (1) where Isc – mean scattering pixel amplitude of individual NP-treated cell as measured in specific region of interest (ROI) with its shape and area being close for those of individual cell, Isc1 - mean scattering pixel amplitude of individual intact cell (obtained under identical settings), I0, I01 – background image amplitude obtained from nanoparticle- and cell-free space in the NP-treated and intact samples, respectively, K – a number of slices in stack obtained for each cell, M – number of analyzed cells. We used previously developed methods and experimental set-up [18, 19] to image, detect and quantify the NP clusters and PNBs in water and individual cells through their optical scattering images and time-responses detected in parallel with two probe lasers. We used the two optical metrics of PNB (Figure S3): optical scattering time-resolved image pixel amplitude and duration of optical scattering time response (measured independently and simultaneously with optical scattering image). First, time-resolved optical scattering was used for imaging of PNBs. Excellent optical scattering properties of a PNB [20] were used for its imaging in water and cells with the second, pulsed probe beam (576 nm, 70 ps, 0.1 mJ/cm2). This beam was directed at the sample under high angle of incidence and with 10 ns delay relative to the excitation laser pulse. Thus only the light scattered by transient PNB was collected by the microscope objective (20x) and detected by the imaging device, a CCD camera (Luka, Andor Technology, Belfast, Northern Ireland) and custom-designed programs developed with LabView platform. For objects whose dimensions are smaller than a wavelength, the size of their image does not represent their actual size. If the image is formed by the light scattered by the object, the maximal brightness of the scattered light correlates to the size of the object. We used this wellknown rule for the quantitative control of the relative size of the gold NP clusters. This allowed us to choose and use in one experiment the NP clusters of similar size. The maximum pixel amplitude that corresponded to the brightest PNB, I, was measured for each individual cell (or NP cluster) and the background signal I0 was measured for a cellfree (or NP-free) space. The PNB scattering pixel amplitude S was calculated: 𝑁 𝑆= ∑𝑛=1(𝐼−𝐼0 ) 𝑁 (2) where N- number of cells or NP clusters (for studies of NP clusters in water). Second, the PNB-specific optical scattering response (Figure 3c) was obtained with additional continuous probe laser (Figure S3). The shape of the time-response signal was PNB-specific, while the duration of the PNB-specific response characterized the PNB lifetime. The maximal diameter of the PNB is proportional to the PNB lifetime [20-24]. The second PNB metric was independently obtained with another, continuous, probe laser (Figure S3). The PNB-induced scattering of a part of the probe beam decreased its axial amplitude, resulting in a dip-shaped output signal of the photodetector that monitored the probe beam (Figure 3c). Thus we registered the time response of the probe laser radiation to the transient scattering effect of the PNB. This mode provided the monitoring of PNB growth and collapse, and delivered the PNB lifetime that characterizes its maximal diameter [19-24]. The lifetime was measured as the duration of the PNB-specific signal at the amplitude level being a half of the maximum of the PNB response. In addition, we measured the probability of the PNB generation at specific fluence of the excitation laser pulse. This allowed us to determine the PNB generation threshold fluence as the excitation laser fluence that provides PNBs generation probability of 0.5. All three described above metrics were used for the relative comparison of the two samples, target and non-target cells, in each cell model. References 1. Sriuranpong V, Park JI, Amornphimoltham P, Patel V, Nelkin BD, et al. (2003) Epidermal growth factor receptor-independent constitutive activation of STAT3 in head and neck squamous cell carcinoma is mediated by the autocrine/paracrine stimulation of the interleukin 6/gp130 cytokine system. Cancer Research 63: 2948-2956. 2. Marshall ME, Hinz TK, Kono SA, Singleton KR, Bichon B, et al. (2011) Fibroblast growth factor receptors are components of autocrine signaling networks in head and neck squamous cell carcinoma cells. Clin Cancer Res 17: 5016-5025. 3. Rachwal WJ, Bongiorno PF, Orringer MB, Whyte RI, Ethier SP, et al. (1995) Expression and activation of erbB-2 and epidermal growth factor receptor in lung adenocarcinomas. Br J Cancer 72: 56-64. 4. Pereboeva L, Komarova S, Roth J, Ponnazhagan S, Curiel DT (2007) Targeting EGFR with metabolically biotinylated fiber-mosaic adenovirus. Gene Ther 14: 627-637. 5. Zhang C, Lv F, Zhou L, Li X, Wu XX, et al. (2009) Effect of verapamil on the expression of EGFR and NM23 in A549 human lung cancer cells. Anticancer Res 29: 2732. 6. Brayman MJ, Dharmaraj N, Lagow E, Carson DD (2007) MUC1 expression is repressed by protein inhibitor of activated signal transducer and activator of transcriptiony. Mol Endocrinol 21: 2725-2737. 7. O'Connor JC, Julian J, Lim SD, Carson DD (2005) MUC1 expression in human prostate cancer cell lines and primary tumors. Prostate Cancer Prostatic Dis 8: 36-44. 8. Wang P, Julian JA, Carson DD (2008) The MUC1 HMFG1 glycoform is a precursor to the 214D4 glycoform in the human uterine epithelial cell line, HES. Biology of Reproduction 78: 290-298. 9. Denmeade SR, Sokoll LJ, Dalrymple S, Rosen DM, Gady AM, et al. (2003) Dissociation between androgen responsiveness for malignant growth vs. expression of prostate specific differentiation markers PSA, hK2, and PSMA in human prostate cancer models. Prostate 54: 249-257. 10. Silver DA, Pellicer I, Fair WR, Heston WD, Cordon-Cardo C (1997) Prostate-specific membrane antigen expression in normal and malignant human tissues. Clin Cancer Res 3: 81-85. 11. Zhang C, Soori M, Miles FL, Sikes RA, Carson DD, Chung LWK, Farach-Carson MC (2011) Paracrine factors produced by bone marrow stromal cells induce apoptosis and neuroendocrine differentiation in prostate cancer cells. The Prostate 71: 157-167. 12. Wright GL, Jr., Haley C, Beckett ML, Schellhammer PF (1995) Expression of prostate-specific membrane antigen in normal, benign, and malignant prostate tissues. Urol Oncol 1: 18-28. 13. Grandis JR, Sok JC (2004) Signaling through the epidermal growth factor receptor during the development of malignancy. Pharmacology & Therapeutics 102: 37-46. 14. O'Connor JC, Farach-Carson MC, Schneider CJ, Carson DD (2007) Coculture with prostate cancer cells alters endoglin expression and attenuates transforming growth factor-beta signaling in reactive bone marrow stromal cells. Mol Cancer Res 5: 585-603. 15. Gregor PD, Wolchok JD, Turaga V, Latouche JB, Sadelain M, et al. (2005) Induction of autoantibodies to syngeneic prostate-specific membrane antigen by xenogeneic vaccination. Int J Cancer 116: 415-421. 16. Tsygankov AY, Kim HW, Pratt JC, Spana C, Class K, et al. (1994) Diminished tyrosine protein kinase activity in T cells unresponsive to TCR stimulation. J Leukoc Biol 55: 289-298. 17. Carmo AM, Castro MAA, Arosa FA (1999) CD2 and CD3 associate independently with CD5 and differentially regulate signaling through CD5 in Jurkat T cells. J Immunol 163: 4238-4245. 18. Wagner DS, Delk NA, Lukianova-Hleb EY, Hafner JH, Farach-Carson MC, et al. (2010) The in vivo performance of plasmonic nanobubbles as cell theranostic agents in zebrafish hosting prostate cancer xenografts. Biomaterials 31: 7567-7574. 19. Lapotko D (2009) Optical excitation and detection of vapor bubbles around plasmonic nanoparticles. Opt Express 17: 2538-2556. 20. Lukianova-Hleb E, Hu Y, Latterini L, Tarpani L, Lee S, Drezek RA, Hafner JH, Lapotko DO (2010) Plasmonic nanobubbles as transient vapor nanobubbles generated around plasmonic nanoparticles. ACS Nano 4: 2109-2123. 21. Lukianova-Hleb E, Lapotko DO (2009) Influence of transient environmental photothermal effects on optical scattering by gold nanoparticles. Nano Lett 9: 2160-2166. 22. Neumann J, Brinkmann R (2007) Nucleation dynamics around single microabsorbers in water heated by nanosecond laser irradiation. J Appl Phys 101: 114701. 23. Vogel A, Noack J, Huttman G, Paltauf G (2005) Mechanisms of femtosecond laser nanosurgery of cells and tissues. Appl Phys B 81: 1015-1047. 24. Vanleeuwen TG, Jansen ED, Motamedi M, Welch AJ, Borst C (1994) Excimer-laser ablation of soft-tissue - a study of the content of rapidly expanding and collapsing bubbles. IEEE J Quantum Electron 30: 1339-1347.