CHAPTER 55- COMPLICATIONS OF PREGNANCY Introduction
advertisement
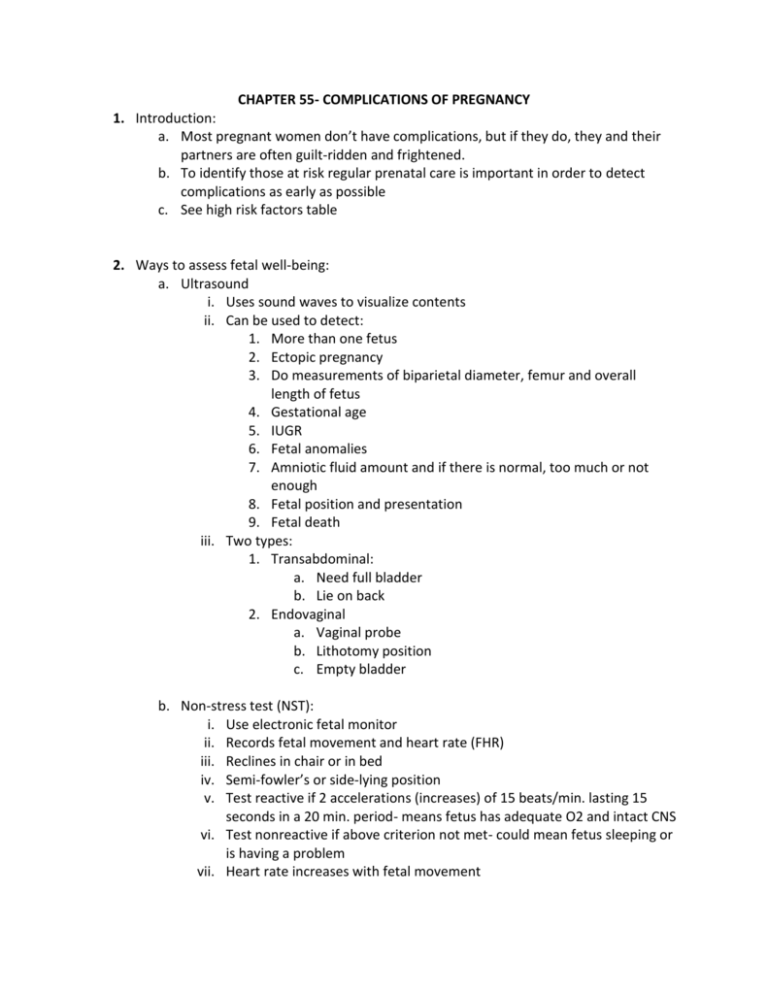
CHAPTER 55- COMPLICATIONS OF PREGNANCY 1. Introduction: a. Most pregnant women don’t have complications, but if they do, they and their partners are often guilt-ridden and frightened. b. To identify those at risk regular prenatal care is important in order to detect complications as early as possible c. See high risk factors table 2. Ways to assess fetal well-being: a. Ultrasound i. Uses sound waves to visualize contents ii. Can be used to detect: 1. More than one fetus 2. Ectopic pregnancy 3. Do measurements of biparietal diameter, femur and overall length of fetus 4. Gestational age 5. IUGR 6. Fetal anomalies 7. Amniotic fluid amount and if there is normal, too much or not enough 8. Fetal position and presentation 9. Fetal death iii. Two types: 1. Transabdominal: a. Need full bladder b. Lie on back 2. Endovaginal a. Vaginal probe b. Lithotomy position c. Empty bladder b. Non-stress test (NST): i. Use electronic fetal monitor ii. Records fetal movement and heart rate (FHR) iii. Reclines in chair or in bed iv. Semi-fowler’s or side-lying position v. Test reactive if 2 accelerations (increases) of 15 beats/min. lasting 15 seconds in a 20 min. period- means fetus has adequate O2 and intact CNS vi. Test nonreactive if above criterion not met- could mean fetus sleeping or is having a problem vii. Heart rate increases with fetal movement c. Fetal Acoustic Stimulation Test (FAST) and Vibroacoustic Stimulation Test (VST): i. Use with NST if nonreactive test ii. Vibrator/buzzer placed over fetal head on abdominal to stimulate fetus. iii. Reactive test is 2 FHR increases of 15 beats/min. lasting 15 secs in a 10 min. period d. Fetal Biophysical Profile (FBPP) assesses: i. Fetal breathing movement ii. Fetal movements of body or limbs iii. Fetal tone –extension/flexion of extremities iv. Amniotic fluid volume v. Reactive NST vi. See table- if score of 8 or more shows probable fetal well-being e. Fetal movement- “quickening” i. Occurs at 16-20 weeks ii. 2 ways to assess: 1. Count fetal movement daily for 10 minutes 3x a day 2. Cardiff method: a. Count fetal movements at the same time each day until 10 movements are felt (note start and stop times) 3.Notify dr. if: a. fewer than 10 movements in 12 hours b. no movements for 8 hours c. sudden, violent movements followed by reduced movements 3. Biochemical Assessments: a. Maternal serum alpha-fetoprotein (MSAFP): i. Identifies birth defects and chromosomal anomalies ii. Done between 16-18 weeks iii. If result hi- can be: 1. Neural tube defect 2. Multiple gestation 3. Maternal diabetes 4. Fetal distress 5. Fetal death iv. If low can be: 1. Down syndrome 2. Maternal hypertensive state b. Estriol: i. Indicates fetoplacental function ii. If gradually increases means placenta functioning properly c. Human Placental Lactogen (PL): i. As fetal weight increases, hPL should increase d. Amniocentesis: i. Needle inserted into amniotic sac thru abdomen and amniotic fluid is withdrawn ii. Never before 14 weeks- do between 14 to 16 weeks iii. Diagnoses genetic diseases and birth defects iv. Can also detect fetal lung maturity v. See safety- amniocentesis vi. Tests done on amniotic fluid: 1. Lecithin/sphingomyelin ratio- determines lung maturity; by 35 weeks if lungs are mature (surfactant present) should be 2:1 ratio 2. Phosphatidylglycerol determines lung maturity 3. Bilirubin- done to see if fetal anemia exists 4. Sex determination e. Chorionic Villi sampling: i. Detects genetic disorders ii. Done at 8-10 weeks gestation f. Contraction Stress Test (CST): i. Evaluates respiratory function of placenta ii. Test done by stimulating uterine contractions by IV oxytocin or nipple stimulation iii. During contractions, O2 of fetus is normally decreased, if healthy fetus, this is tolerated without problems iv. If placenta is not functioning properly, will see fetal hypoxia, myocardial depression and a decreased FHR v. Not to be used in placenta previa, abruption placenta, PROM, history of preterm labor, previous C/S vi. Desired result is a negative CST meaning no late decelerations (decreases in FHR) with uterine contractions vii. Not desired is a positive CST with late decelerations that occur with more than half of the contractions 4. Electronic Fetal Monitoring (EFM): a. Visual record of FHR in relation to uterine contractions- it shows you what happens to the fetal heart rate when a contraction occurs b. 2 types: i. External (indirect) monitoring: 1. A tocodynamometer is placed on mother’s abdomen near the fundus to monitor uterine contractions 2. A Doppler transducer (an ultrasonic device) is placed on the mother’s abdomen to monitor FHR 3. Both held on with an elastic band ii. Internal (direct) monitoring: 1. More reliable- directly monitors FHR 2. EKG electrode is directly attached to fetal presenting part (usually the head) 3. 4 conditions must be met: a. Ruptured membranes b. 2cm dilated cervix c. Presenting part needs to be down near cervix d. Sterile technique iii. Interpretations: 1. Baseline rate: average FHR during a 10 minute period; normal rate 110-160; if rate above 160-tachycardia, below 110- bradycardia 2. Accelerations- short-term increases in FHR usually caused by fetal movement; is normal 3. Early decelerations- reductions in FHR that begin early with the contraction and typically mirror the contraction, caused by head compression during contractions, no intervention needed 4. Late decelerations- reductions in FHR that begin at peak of contraction and increase to baseline level after the contraction has finished, caused by uteroplacental insufficiency (poor blood flow), is abnormal, report STAT, give mother some O2 5. Variable decelerations- reductions in FHR that have no relationship to the contractions, caused by compression of the umbilical cord leading to decreased blood flow to the fetus, is abnormal, report STAT, change mother’s position- to lie on either side, preferably the left HYPEREMESIS GRAVIDARUM: A. B. C. D. Excessive vomiting during pregnancy Cause: unknown but may be hormonal or have a psychological component Can come and go or last entire pregnancy Leads to: a. Dehydration b. Electrolyte and fluid imbalances c. Alkalosis d. Protein and vitamin deficiencies e. Cardiac arrhythmias f. Death of both mother and baby E. Sxs: a. Tachycardia b. Hypovolemia c. Increased Hct and BUN d. Decreased urine output F. Treatment: a. Hospitalize b. IV fluids c. Psychotherapy d. Minimal meds (teratogenic to fetus) e. NPO , then dry foods, then regular diet f. Bedrest g. Emotional support h. Encourage ventilation of feelings i. Quiet environment j. Good oral hygiene k. Antiemetic as ordered l. Assess: i. Skin turgor, mucous membranes ii. I&O iii. Emotional state iv. What triggers it v. Amount and characteristics of emesis vi. FHR vii. For jaundice viii. For vaginal bleeding BLEEDING: A.Abortion: a. induced (purposeful) or spontaneous (natural) termination of pregnancy before 24 weeks of gestation (viability of fetus) b. spontaneous: i. a miscarriage ii. related to: A. chromosomal abnormalities B. faulty implantation C. teratogenic substances D. placental abnormalities E. incompetent cervix F. chronic maternal disease G. maternal infections H. endocrine imbalances iii. TYPES: A. threatened- unexplained bleeding and cramping; cervix closed and membranes intact; treat: bedrest 24-48 hours, avoid stress, strenuous activity, sexual intercourse. B. inevitable- increased bleeding and cramping, cervix begins to dilate, membranes can rupture; treat: D&C or suction evacuation, blood transfusion if needed C. incomplete- some of the products of conception are expelled, bleeding heavy, cramping severe; treat: same as inevitable D. complete- all parts of conception are expelled E. missed- fetus dies but is retained, cervix closed, if not expelled within 6 weeks and fetus is < 12 weeks a D&C is done, if fetus is > 12 weeks induction of labor with oxytocin is used F. habitual- any of the above occurring in 3 consecutive pregnancies, cervix begins to dilate in 2nd trimester- incompetent cervix; treat: cerlageShirodkar procedure is done, internal mouth of cervix is sutured shut, done at 16 weeks of gestation iv. assess: A. amount of bleeding, cramping, presence of clots, for expelled tissue B. do vital signs C. have a calm environment D. provide active listening E. patient may have feelings of guilt/fear ECTOPIC PREGNANCY: A. Fertilized ovum implants outside the uterus, most often the fallopian tube but can be other sites B. Risk factors: PID, Diethylstilbesterol, STDs, medication for infertility, endometriosis C. Ages: 15-45 year old mostly D. Pregnancy appears normal at first, then 3 to 5 weeks after missed period pain starts due to increasing size of fallopian tube, tube ruptures with severe pain then bleeding intrabdominal or vaginal can occur E. Sxs: i. amenorrhea ii. nausea iii.breast tenderness iv.dull ache on one side of pelvis becoming more severe v.when tube ruptures, pt. experiences a single excruciating pain in abdomen- may have referred shoulder pain vi.decreased Hgb, Hct and RBC vii. increased WBC, sed rate viii.slowly rising hCG level ix.rigid, tender abdomen F.Surgical management: i. surgery so bleeding can be controlled ii. NPO iii.Pre and post op care iv.bedrest v.analgesics vi.vital signs HYDATIDIFORM MOLE (TROPHOBLASTIC DISEASE): A.abnormality of the placenta B.can be partial or complete C. uterus fills with fluid filled grapelike clusters called vesicles D.no FHTs E. if partial, fetus is present but not viable F. may have hyperemesis gravidarum G. sxs: i. severe nausea and vomiting ii. brownish vaginal drainage but may be bright red iii.characteristic molar pattern on ultrasound is a snowy appearance iv.PIH sxs H.suspected if PIH occurs before 24 weeks gestation I.diagnose by ultrasound J. medical management: i. follow-up for 1-2 years afterwards due to risk of developing choriocarcinoma ii. do chest x-rays to detect metastasis iii.do pelvic exams iv.do weekly hCG levels v.do NOT become pregnant during this time K.surgical management: i.D&C ii.if older, hysterectomy L.pharmacological: i. if hCG remains high or rises after uterus evacuated- methotrexate is given ii.oxytocin is used to keep uterus contracted to control bleeding iii.blood transfusions if needed PLACENTA PREVIA: A.fertilized ovum is implanted in lower uterine segment with placenta lying over or very near the internal cervical mouth B. cause is unknown C.risk factors: i.multiparity ii.D&C, C/s scarring iii.maternal advancing age iv.smoking D. sxs: i. PAINLESS bleeding in last half of pregnancy ii. relaxed, nontender uterus iii.bleeding-spotting to profuse iv.usually FHR stable E. classified as: i. low-lying or marginal-placenta near internal cervical mouth and not covering any part of the opening ii.partial-placenta covers part of the internal cervical mouth opening iii.complete/total- placenta completely covers internal cervical mouth iv.diagnose by ultrasound F.as cervix thins during labor, placenta pulls away from cervix and bleeding occurs G. effects on fetus/neonate: i. if profuse bleeding, hypoxia to fetus occurs ii. neonate should be checked for anemia H.medical management: i. maintain pregnancy until fetus is viable ii.determine lung maturity by the L/S ratio iii.do H&H q 12 hrs. iv.blood transfusions if needed v.no vaginal exams once diagnosed I. surgical management: i. C/S STAT if fetal duistress or maternal condition worsens J. pharmacological: i. Betamethasone (Celestone) is given to mom to accelerate fetal lung maturity K. treatment: i. bedrest with BRP if no bleeding; bedrest if bleeding ii.monitor vital signs and FHR iii.calm environment iv.Monitor uterine contractions ABRUPTIO PLACENTA: 1. premature separation from the wall of the uterus of a normally implanted placenta 2. cause: unknown 3. risk factors: i. mom has hypertension ii.multiple pregnancies iii.abdomen trauma iv.smoking,alcohol or cocaine use 4. Occurs late in pregnancy or during labor 5. types: i. central- center of placenta separates, blood is trapped between placenta and uterine wall, no apparent bleeding, bleeding is hidden ii.marginal- edge of placenta separates and bright red bleeding vaginally iii.complete- entire placenta separates with profuse bleeding vaginally 6. moderate to severe PAIN, rigid, painful uterus 7. after delivery of the fetus and placenta the uterus contracts poorly with much bleeding 8. may need hysterectomy 9. Can lead to DIC 10. effects on fetus/neonate: i. 1/3rd of cases lead to fetal death ii.complications: a. Preterm labor b. Hypoxia c. Anemia d. Irreversible brain damage e. Fetal death 11.medical management: i. blood tests to include: H&H, PTT, protime, clotting factors, platelets ii.blood transfusions if needed iii.foley catheter iv.if a small separation and near term- induce and deliver vaginally v.if moderate or severe separation, C/S vi.hysterectomy may have to be done to control bleeding 12. medications: i.Rhogam to nonsensitized Rh negative mothers ii.plasma iii.analgesics 13.nursing management: i. NPO if surgery ii.bedrest iii.assess bleeding, pain, vital signs, FHR, fetal activity iv.blood transfusions ineeded v.O2 vi.pre&post-op teaching if C/S vii.lie on left side, not back viii.foley cath care DIC (DISSEMINATED INTRAVASCULAR COAGULATION): 1. Condition in which there is overstimulation of normal clotting process leading to small blood clots (thrombin) forming throughout the circulatory system. In addition, platelets and clotting factors are depleted leading to generalized bleeding causing anemia and ischemia to vital organs. 2. Is a complication of a primary problem 3. Can occur to anyone, not just a pregnant woman 4. Risk factors: a. Abruption placenta b. Placenta previa c. Haydatidiform mole, d. PIH, e. retained products of conception, f. amniotic fluid embolism, g. infections 5. Sxs: a. Onset sudden b. c/o dyspnea/chest pain 6. 7. 8. 9. c. restlessness d. cyanosis e. spitting up frothy blood-tinged mucus f. bleeding gums g. epistaxis h. petechiae under blood pressure cuff i. bleeding from injection sites Effects on fetus/neonate: a. STAT delivery even if preterm b. Fetal hypoxia c. Fetal death Medical management: a. MUST IDENTIFY AND TREAT UNDERLYING CAUSE b. Deliver fetus c. Diagnostic blood work includes: H&H, fibrinogen level, PT, PTT, platelets Medications: a. IV of blood, fibrinogen or cryoprecipitate is started b. Heparin drip on IV pump to prevent microemboli c. O2 Nursing management: a. Have a calm manner b. IV fluids, blood c. Heparin d. O2 e. Vital signs PIH (PREGNANCY INDUCED HYPERTENSION): 1. Also called toxemia, preeclampsia 2. Appears after 20 weeks gestation 3. Classic sxs: a. Hypertension b. Edema c. Proteinuria 4. Usually with 1st babies of mothers <20 or > 35 and poor and with poor nutrition 5. Risk factors: a. Diabetes b. Multiparity c. Family history of PIH 6. SXS: a. Increased BP b. Decreased blood flow to uterus and placenta c. Cerebral edema leading to headaches and visual disturbances d. Liver increase in size leading to epigastric pain 7. Cause: unknown 8. CURE: deliver baby 9. Effects on fetus/neonate: a. Abruption placenta b. Placental infarction c. Acute hypoxia d. Intrauterine death e. Preterm baby 10. Types: a. Mild preeclampsia: i. BP is increased 30 points systolically or 15 points diastolically over baseline on 2 occasions at least 6 hours apart or mother has a BP of 140/90 ii. Facial and hand edema leading to weight gain of >1lb./wk. iii. +1 or +2 albumin in urine b. Severe preeclampsia: i. BP of 160/110 or > on 2 occasions at least 6 hours apart ii. Generalized edema of face, hands, sacral area, lower extremities, abdomen iii. Wt. gain 2 lbs. or more in a few days/wk. iv. +3 or +4 proteinuria v. Urine output < 500ml in 24 hours vi. Hct, uric acid, and creatinine levels increase vii. Other sxs: continuous headache, blurred vision, scotomata (spots before eyes), N&V, irritability, etc. viii. Epigastric pain usually last sx seen before goes into full blown eclampsia c. Eclampsia: i. Seizures tonic clonic- grand mal ii. Coma for few minutes to hours iii. Without treatment- death iv. Seizure activity may trigger uterine contractions d. HELLP syndrome: i. Complication of preeclampsia/eclampsia with liver damage occurring ii. Hemolysis of RBCs iii. Increased liver enzymes- AST/ALT iv. Ischemia of liver v. Platelets decrease to less than 100,000 vi. Causes ischemia, tissue damage, hypoglycemia vii. If blood sugar < 40, maternal mortality high viii. 20% of PIH patients develop HELLP 11. Medical management: a. Goals of treatment: i. Decrease BP ii. Prevent convulsions iii. Deliver healthy baby b. If mild preeclampsia- bedrest with lying on either side c. Lab tests: Hct, Plt, lytes, liver enzymes, estriol level, 24 hour urine for protein and creatinine, serum creatinine 12. Surgical management: a. C/S if mother’s condition deteriorates or fetal distress 13. Medications: a. Magnesium Sulfate (MgSO4): i. A CNS depressant ii. Decrease possibility of convulsions and BP iii. IV or IM (Z-Track) iv. Excreted by kidneys- so if pt. has poor renal function can be toxic and lead to cardiac arrhythmia and arrest v. Given for 24-48 hrs. post-delivery vi. Conditions that MUST be met in order to give MgSO4: 1. Respirations must be 14/min or more 2. Deep tendon reflexes (DTR) have normal response when checked 3. Have at least 30cc urine/hr. output vii. Mag levels need to be monitored- therapeutic level is 4-8 viii. Side effects of toxicity are: flushing, sweating, hypotension, hypothermia, muscle weakness, constipation, N&V ix. Foley catheter inserted x. Mag toxicity antidote is calcium gluconate- keep at bedside for emergency injection b. Antihypertensive- Apresoline except if cardiac disease then Normadyne c. Valium/Phenobarbitol to help rest d. Oxytocin to induce labor- may be used along with MgSO4 14. Diet: a. Well-balanced, hi protein, moderate sodium b. If nauseated or has convulsions, keep NPO 15. Activity: a. Bedrest, left-side lying position, no lying on back 16. Nursing managment: a. Check vs, FHR, edema, weight, for irritability, hyperreflexia (DTR), dyspnea, Proteinuria, headache, blurred vision, cyanosis, nausea, and epigastric pain b. Include family in decisions c. Encourage ventilation of feelings d. Assess for toxicity if MgSO4 is being used e. I&O CHRONIC MEDICAL PROBLEMS: DIABETES MELLITUS: 1. If you have diabetes and want to get pregnant, it is important that your diabetes is well controlled prior to conception. 2. Whether chronic or gestational diabetes, effects same 3. Pregnancy and carbohydrate metabolism: a. Early pregnancy- insulin production increased b. Last half of pregnancy- increased tissue resistance to insulin c. If already a diabetic, pregnancy makes it harder to control it 4. Effects of pregnancy on diabetes: a. 1st trimester, insulin need is decreased b. 2nd trimester insulin need is increased c. 3rd trimester has 4x the insulin need d. After delivery and placenta passed, insulin need decreases 5. Effects of diabetes on pregnancy: a. Higher risk for complications b. Has higher risk for PIH if vascular problems c. Hydramnios (excessive amount of amniotic fluid) may occur d. Death of fetus and mother can occur e. Maternal complications directly related to degree of blood glucose control 6. Effects on fetus/neonate: a. Macrosamia (excessive fetal growth) b. After birth, neonate develops hypoglycemia (2-4 hrs). c. If fetus has a high insulin level, surfactant can be inhibited and fetus can have respiratory distress syndrome d. Fetus also has polycythemia (excessive amount of RBCs) and increased bilirubin leading to hyperbilirubinemia e. Higher risk for fetal anomalies especially heart, CNS, skeletal system 7. Medical management: a. Maintain maternal blood sugar between 70-120 b. Mother seen by OB and endocrinologist monitors own blood sugar and gives self insulin according to sliding scale c. Fetal status: i. Assessed throughout pregnancy ii. AFP screening done as there is a risk for neural tube defects iii. Ultrasound done at 18 weeks then repeated q 4-6 weeks- to determine gestational age and look for congenital anomalies iv. NST done weekly v. CST starting at 32 weeks and then weekly. 8. Surgical management: a. If fetus having trouble, do C/S 9. Medications: a. Humalin used as less allergic reaction b. c. 10. Diet: a. b. c. Daily multiple injections using a sliding scale No oral hypoglycemic Increase calories by 300 daily when pregnant Divide total calories between 3 meals and 3 snacks Eat bedtime snack as late as possible to prevent nitetime hypoglycemiainclude a carbohydrate and a protein d. Do no more than 10 hours between bedtime snack and breakfast 11. Activity: a. Maintain unless contraindicated 12. Nursing management: a. Listen actively to patient b. Answer questions c. Provide support d. Teach glucose monitoring and insulin use if needed e. Monitor fetal status f. Encourage compliance for prenatal visits and testing appointments 13. Assess: a. Diet, activity, medication compliance b. Urine for sugar c. Vital signs d. Weight e. NST f. For infection g. After 28 weeks gestation, record maternal evaluation of fetal activity CHRONIC HYPERTENSION: 1. Definition: BP 140/90 or higher before pregnancy or before the 20th week or that lasts longer then 6 weeks after delivery 2. Can lead to retinal hemorrhage, renal disease, arteriosclerosis, placental infarcts or placenta abruption 3. Effect on neonate/fetus: a. Decreased blood flow leading to IUGR and fetal hypoxia 4. Medical management: a. Prevent preeclampsia development b. Seen prenatally q 2 weeks 5. Medications: a. Aldomet 6. Diet: a. Well-balanced b. No salt restriction 7. Activity: a. Daily rest periods lying on left side 8. Nursing management: a. Educate re: HTN b. Answer questions c. Rest periods d. Stress importance to keep all appointments 9. Assess: a. For headaches and visual disturbances b. Is a silent killer! HEART DISEASE: 1. Someone with preexisting heart disease who gets pregnant may have problems due to increases in blood volume, cardiac output and heart rate 2. Sxs: increased pulse, hypertrophy of ventricle 3. Can lead to CHF 4. Risk factors: rheumatic fever in the past, congenital heart disease, HTN 5. Effects on fetus/neonate: a. IUGR b. Hypoxia 6. Medical management: a. Sees cardiologist and OB b. Chest x-rays, auscultation of heart sounds, EKG, echocardiogram, cardiac cath may be done c. See OB 2-3 times a week d. Hospitalization as needed 7. Medications: a. Antibiotics for prophylaxis b. Heparin if coagulation problems as heparin does not cross placenta c. Thiazide diuretics and Lasix for CHF 8. Diet: a. Hi in iron and protein, lo in Na, caloric intake adequate 9. Activity: a. May be restricted depending on sxs b. 8-10 hours sleep nitely c. Frequent rest periods throughout day d. Side lying position to prevent compression of inferior vena cava 10. Nursing management: a. Vital signs b. Lung and heart sounds c. FHT d. Encourage to keep all scheduled appointments e. Encourage diet as prescribed f. Side-lying position 11. Assess: a. Activity level b. Amount of rest c. For fatigue with activity d. Dyspnea, palpitations e. Cough f. Anxiety g. Support system h. Weight gain i. Edema j. Vital signs k. Signs of infection l. Anemia m. Heart murmurs or crackles in lungs MATERNAL PHENYKETONURIA: 1. Definition: a. an inborn error of metabolism in which a deficiency of the enzyme to metabolize the amino acid phenylalanine 2. genetically inherited by recessive gene 3. if allowed to accumulate can lead to irreversible brain damage 4. since 1997, all newborns are screened for PKU 5. effect on fetus/neonate: a. if poorly regulated mother leads to possible IUGR, mental retardation, microencephaly, heart defects in fetus 6. medical management: a. check mother’s phenylalanine level q 2-4 weeks during 1st half of pregnancy the q week in last half of pregnancy b. check zinc and iron levels 7. diet: a. if mother with PKU she needs to be on a phenylalanine free diet to keep her phenylalanine level < 2.0mg/dl while pregnant- if does outcome of pregnancy is better b. modified protein supplement c. fruits, vegetables, fats d. low-protein cereals 8. nursing management: a. encourage to maintain phenylalanine free diet b. check blood level throughout pregnancy INFECTION: 1. Any infection is a risk factor 2. Early diagnosis and treatment is important 3. If left untreated can cause abortion, congenital anomalies, fetal infection, IUGR, preterm labor, mental retardation, death TORCH GROUP: 1. Toxoplasmosis 2. Rubella 3. Cytomegalovirus 4. Herpes virus type 2 TOXOPLASMOSIS: 1. cause: protozoan Toxoplasma gondii 2. sxs: mild, vague, flu-like, often go unnoticed 3. occurs by eating undercooked, raw or cured meat; working in garden soil without gloves and used cat litter 4. effects on fetus/neonate: a. increased incidence of abortion, preterm birth, stillbirth, neonatal death b. damage to fetus is more severe if disease is acquired before 20 weeks gestation c. if survives: deaf, blind, severely retarded 5. medical management: a. identify patients at risk b. treat disease promptly c. incubation period is 10 days 6. medications; a. sulfadiazine (microsulfon) b. or pyrimethamine (daraprim) 7. diet: a. avoid raw or partially cooked meats b. wash fruits and vegetables before eating 8. risk factors: a. contact with soil while gardening witho0ut gloves b. cat litter c. travel outside okf US, Canada, Europe 9. nursing management: a. encourage to eat only well-done meats b. wash all fruits and vegetables c. wear gloves when gardening d. may have no sxs or may have malaise or myalgia, rash, spenomegalogy, enlarged lymph nodes RUBELLA: 1. 2. 3. 4. 5. 6. Also called German Measles or 3 day Measles Incubation period 14 to 21 days Maculopapular rash appears then vanishes in 3 days Highly contagious Spread by airborne droplets Effects on fetus/neonate: a. Earlier in pregnancy it occurs, more severe the fetal effects b. Effects- congenital rubella syndrome consisting ofd cataracts, deafness, patent ductus arteriosus c. Possible IUGR, mental retardation, hyperbilirubinemia, petechial rash d. Infants contagious and may shed virus for months 7. Medical management: a. Prevention is best cure b. Maternal prenatal screening is done to determine immunity c. A titier of 1:16 or greater is immunity; a titer of 1:8 or less is susceptible to rubella d. If susceptible, avoid exposure during pregnancy e. If gets infected in first trimester, 90% probability of fetal problems 8. Medications: a. All children should be immunized with live attenuated vaccine by age 1 b. Suspectible pregnant women should be immunized immediately after birth and not get pregnant for 3 months afterward 9. Nursing management: a. Identify susceptible clients b. Instruct in avoiding exposure while pregnant c. Encourage to receive immunization after delivery d. Delay pregnancy for 3 months e. Encourage to have children immunized 10. Assessment: a. Sxs: none or may complain of muscle aches and joint pain, increased T, maculopapular rash and lymphadenopathy CYTOMEGALOVIRUS: 1. Found in saliva, breast milk, cervical mucous, urine and semen 2. Spread by close contact 3. Asymptomatic in adults and children 4. Effects on fetus/neonate: a. Death b. If survive- hydrocephaly, microencephaly, mental retardation, CP, or no noticeable damage c. SGA baby 5. Medical management: a. Diagnose by: i. Finding CMV in maternal urine or CMV antibodies in the blood b. No treatment available HERPES GENITALIS (HERPES SIMPLEX VIRUS TYPE 2); HSV-2: 1. Painful, vesicular, genital lesions that appear few hours to 20 days after exposure 2. Primary episode worst 3. Infection can occur to fetus after ROM or during vaginal delivery 4. Mom can breast feed with herpes as the virus not found in breast milk 5. Effects on fetus/neonate: a. If get in 1st trimester, 50% chance that fetus will be born stillborn or a spontaneous abortion will occur b. No sxs at birth c. 2-12 day incubation period d. After incubation period infant will show signs of i. Poor feeding ii. Jaundice iii. Seizures iv. Possible vesicular lesions 6. Medical management: a. Diagnose by active lesions b. Treatment- relieve pain c. No known cure 7. Surgical management: a. C/S if active lesions present 8. Medications: a. Betadine cleansing may prevent secondary infection b. Burrow’s solution may relieve discomfort HIV/AIDS: 1. 2. 3. 4. IF HIV infected, maintenance of weight difficult Instruct in nutritio0on, exercise, rest, sleep Pregnancy- can cause one to go from HIV to AIDS faster Effects on fetus/neonate: a. HIV transmitted: i. Thru placenta ii. Exposed to maternal blood and vaginal secretions at time of birth iii. Thru breast milk b. Infants often have a + antibody titer after birth 5. 6. 7. 8. c. Infants not infected with HIV will seroconvert to a – antibody titer Medical management: a. There is no cure for HIV or AIDS b. Prenatal testing done to include a CD4 lymphocyte count Diet: a. May need nutritional counseling Nursing management: a. Follow standard precautions at all times b. Encourage adequate food intake c. Encourage to follow-up with prenatal visits and tests Assess: a. Client may be asymptomatic or complains of fatigue, malaise, loss of appetite, diarrhea, signs of anemia, cell-mediated immunodeficiency, progressive weight loss, lymphadenapathy, neurologic dysfunctioin, purplish lesions, sores in mouth, delirium OTHER INFECTIONS: 1. May result in: a. spontaneous abortion b. Preterm labor c. Infected infant 2. See table 51-4, pg. 1479