Planning Care and Risk Assessment
advertisement
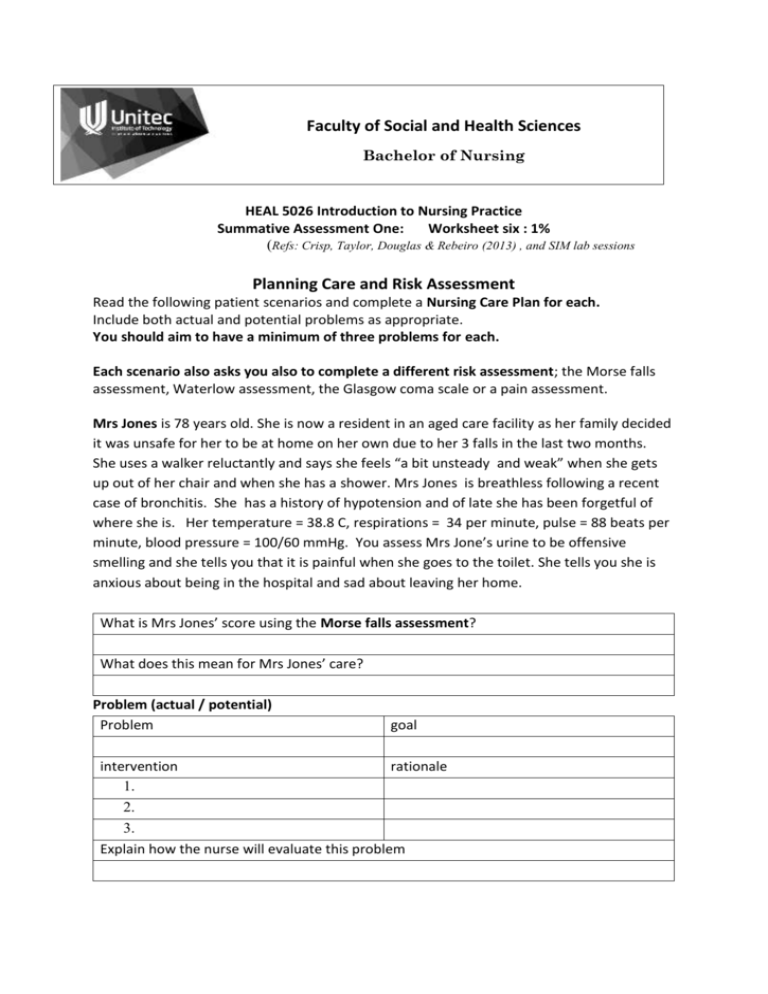
Faculty of Social and Health Sciences Bachelor of Nursing HEAL 5026 Introduction to Nursing Practice Summative Assessment One: Worksheet six : 1% (Refs: Crisp, Taylor, Douglas & Rebeiro (2013) , and SIM lab sessions Planning Care and Risk Assessment Read the following patient scenarios and complete a Nursing Care Plan for each. Include both actual and potential problems as appropriate. You should aim to have a minimum of three problems for each. Each scenario also asks you also to complete a different risk assessment; the Morse falls assessment, Waterlow assessment, the Glasgow coma scale or a pain assessment. Mrs Jones is 78 years old. She is now a resident in an aged care facility as her family decided it was unsafe for her to be at home on her own due to her 3 falls in the last two months. She uses a walker reluctantly and says she feels “a bit unsteady and weak” when she gets up out of her chair and when she has a shower. Mrs Jones is breathless following a recent case of bronchitis. She has a history of hypotension and of late she has been forgetful of where she is. Her temperature = 38.8 C, respirations = 34 per minute, pulse = 88 beats per minute, blood pressure = 100/60 mmHg. You assess Mrs Jone’s urine to be offensive smelling and she tells you that it is painful when she goes to the toilet. She tells you she is anxious about being in the hospital and sad about leaving her home. What is Mrs Jones’ score using the Morse falls assessment? What does this mean for Mrs Jones’ care? Problem (actual / potential) Problem intervention 1. 2. 3. goal rationale Explain how the nurse will evaluate this problem Problem (actual / potential) Problem goal intervention rationale 1. 2. 3. Explain how the nurse will evaluate this problem Problem (actual / potential) Problem intervention 1. 2. 3. goal rationale Explain how the nurse will evaluate this problem Mr Appleby is 74 years old. He has a 2 cm x 2 cm decubitus ulcer on his heel (stage 2) and is in the hospital for respite care. The decubitus ulcer limits his mobility. His medical history shows he is a type two diabetic. Mr Appleby is a smoker, usually having 15 cigarettes per day when at home. He has not passed a bowel motion for 4 days and is feeling “off his food”. He says that he finds it difficult to get to the toilet on time preferring to use a bottle. He notes that he has lost 4 kg in the last month without trying. He is 170cms tall and weighs 72 kgs. Mr Appleby’s skin is dry and bruises easily. He has 5 mosquito bites on his arms which he scratches continuously. Two areas have broken skin. Mr Appleby is worried about his cat Tess and who is feeding her and caring for her. He tells you he can’t sleep at night because of this. What is Mr Appleby’s risk for further decubitus ulcers using the Waterlow Assessment scale? What does that mean for Mr Appleby’s care? Problem (actual / potential) Problem intervention 1. goal rationale 2. 3. Explain how the nurse will evaluate this problem Mr Jacobson is found lying on the floor of the bathroom. He appears to have hit his head on the basin. He answers you only when he hears your voice and he is not sure where he is. When you ask him to move his legs and squeeze your hand he responds appropriately. His vital signs are : B/P= 135/85 mgHg, Temperature = 36.8 C, Respirations =26 beats per minute, heart rate= 88 beats per minute. He is returned to his bed with the assistance of 3 nurses and a hoist and asks if he can just sleep. His mouth is dry, tongue is furry and his lips are cracked. You notice he has had minimal urine output over the last couple of days. Later Mr Jacobson tells you he has pain. Explain how the Glasgow Coma scale assessment might be beneficial in this situation. What was his score at the initial assessment? And how will this impact on his care? Outline a comprehensive Pain assessment to assess Mr Jacobson’s pain. Documentation The nurse makes a mistake by writing about Mr Brown’s care in Mr White’s progress notes. Explain the action the nurse needs to take There are 8 general principles of safe and effective documentation. Identify these principles and show your understanding of how to apply them in the clinical setting. Computerised progress notes and patient records present further responsibilities for health professionals. Explain two of these responsibilities. Outline three reasons why incidents forms are completed in the clinical area.