6. List the risk factors for developing hypertension.
advertisement
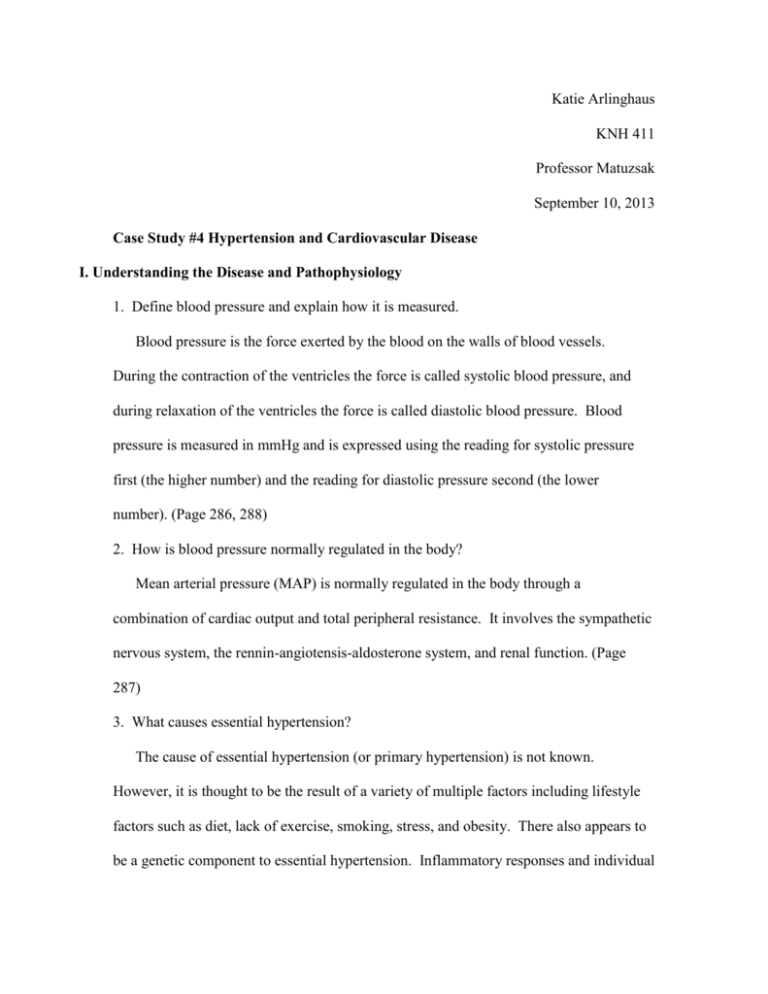
Katie Arlinghaus KNH 411 Professor Matuzsak September 10, 2013 Case Study #4 Hypertension and Cardiovascular Disease I. Understanding the Disease and Pathophysiology 1. Define blood pressure and explain how it is measured. Blood pressure is the force exerted by the blood on the walls of blood vessels. During the contraction of the ventricles the force is called systolic blood pressure, and during relaxation of the ventricles the force is called diastolic blood pressure. Blood pressure is measured in mmHg and is expressed using the reading for systolic pressure first (the higher number) and the reading for diastolic pressure second (the lower number). (Page 286, 288) 2. How is blood pressure normally regulated in the body? Mean arterial pressure (MAP) is normally regulated in the body through a combination of cardiac output and total peripheral resistance. It involves the sympathetic nervous system, the rennin-angiotensis-aldosterone system, and renal function. (Page 287) 3. What causes essential hypertension? The cause of essential hypertension (or primary hypertension) is not known. However, it is thought to be the result of a variety of multiple factors including lifestyle factors such as diet, lack of exercise, smoking, stress, and obesity. There also appears to be a genetic component to essential hypertension. Inflammatory responses and individual differences within the rennin-angiotensin-aldosterone control of blood pressure may also contribute to the development and progression of hypertension. (Page 288) 4. What are the symptoms of hypertension? Hypertension typically has no symptoms and often goes undiagnosed, which is how it got the nickname of the “silent killer.” Hypertenstion can cause congestive heart failure, kidney failure, myocardial infarction, stroke, or aneurysms. (Page 288) 5. How is hypertension diagnosed? People with blood pressure greater than or equal to 140/90mmHg are considered to be hypertensive. However, both systolic and diastolic blood pressures do not need to be elevated for a person to be diagnosed at hypertensive. Stage 1 hypertension is classified as a systolic blood pressure between 140-159mmHg or a diastolic blood pressure 9099mmHg. Stage 2 hypertension is classified as a systolic blood pressure greater than or above 160mmHg or a diastolic blood pressure greater than or above 100mmHg. The diagnosis of hypertension should also include urinalysis, blood glucose, hematocrit and lipid panel, serum potassium, creatinine, and calcium laboratory tests. (Page 288-289) 6. List the risk factors for developing hypertension. Risk factors for developing hypertension include excessive sodium intake, low potassium intake, excessive alcohol intake, lack of exercise, smoking, stress, family history, age (>55 for men, >65 for women), and obesity (BMI>30kg/m2). (Page 289) 7. What risk factors does Mrs. Sanders currently have? According to Mrs. Sanders’s diet recall she has a high sodium intake. She doesn’t exercise very much (although she did recently begin a walking program and has had some weight loss success with the program) and used to smoke two packs of cigarettes a day (fortunately, she quit “cold turkey” a year ago). She also has a family history of hypertension. Her mother died from MI related to uncontrolled hypertension. 8. Hypertension is classified in stages based on the risk of developing CVD. Complete the following table of hypertension classifications. Blood Pressure mm Hg Category Systolic BP Diastolic BP Normal Prehypertension <120 120-139 and or Hypertension Stage 1 Hypertension Stage 2 140-159 ≥ 160 or or <80 80-89 90-99 ≥100 (Page 289) 9. How is hypertension treated? Hypertension is treated through medication, weight reduction, physical activity, and nutrition therapy. The goal of treatment is to reduce the risk of cardiovascular and renal disease and to reduce blood pressure to <140/80mmHg. (Page 290) 10. Dr. Thornton indicated in his note that he will “rule out metabolic syndrome.” What is metabolic syndrome? Metabolic syndrome is a constellation of metabolic risk factors for coronary heart disease including abdominal obesity, insulin resistance, dyslipidemia, hypertension, and prothrombotic state. (Page 302) 11. What factors found in the medical and social history are pertinent for determining Mrs. Sander’s CHD risk category? Mrs. Sanders has a family history of HTN as her mother died from MI due to uncontrolled HTN. Mrs. Sanders is overweight with a BMI of 25.8 (although has recently implemented a walking program to lose weight), has high blood pressure at 160/100mmHg. Although she quit “cold turkey” a year ago, Mrs. Sanders used to smoke two packs a day. From her diet recall, which included items such as canned tomato soup, saltine crackers, and table salt seasoning, it is evident that Mrs. Sanders has a high intake of sodium. She also mentions that she finds low sodium food lacking in flavor. Finally, Mrs. Sanders is African American, which puts her in a higher CHD risk category as HTN is more prevalent among African Americans. (Page 288) 12. What progression of her disease might Mrs. Sanders experience? If her hypertension is uncontrolled, Mrs. Sanders may experience congestive heart failure, kidney failure, myocardial infarction, stroke, or aneurysms. Her vision may be impaired due to blood vessels bursting or bleeding within her eyes. Hypertension can also lead to decreased left ventricular ejection fraction, ventricular arrhythmias, or even sudden cardiac death. (Page 288) II. Understanding the Nutrition Therapy 13. Breifly describe the DASH eating plan. The DASH (Dietary Approaches to Stop Hypertension) eating plan was designed to not only reduce sodium intake, but also increase potassium, magnesium, calcium, and fiber intakes within a moderate energy intake. The eating plan was created after a series of clinical trials in the late 1990s that found that blood pressures were reduced with an eating plan that was low in saturated fat, cholesterol, total fat, and that emphasized 8-9 servings of fruits and vegetables and three servings of low-fat dairy products. The plan emphasizes whole-grain products, fish, poultry, nuts, vegetables, and fruits, and limits red meat, sweets, and sugary beverages. (Page 294-295) 14. Using EAL, describe the association between sodium intake and blood pressure. According to EAL, there is good evidence that high sodium intakes increase blood pressure. “Seventeen studies demonstrate the benefit of reducing dietary sodium intake for lowering blood pressure. A sodium intake of less than 2,300mg per day and further reduction of sodium intake to 1,600mg may have additional blood pressure-lowering effects, especially when combined with the DASH dietary pattern.” (http://andevidencelibrary.com/conclusion.cfm?conclusion_statement_id=250636&highli ght=sodium&home=1) 15. Lifestyle modifications reduce blood pressure, enhance the efficacy of antihypertensive medications, and decrease cardiovascular risk. List lifestyle modifications that have been shown to lower blood pressure. Lifestyle modifications that have been shown to lower blood pressure include increased physical activity, smoking cessation, weight loss, reduced sodium, saturated fat, and alcohol intake, and increased calcium, potassium, and fiber intake. (Page 292) III. Nutrition Assessment 16. What are the health implications of Mrs. Sander’s body mass index (BMI)? Mrs. Sander’s BMI is 25.8kg/m2, which classifies her as overweight, and increases her risk for type 2 diabetes, hypertension, and CVD. (Page 300) 17. Calculate Mrs. Sanders’s resting and total energy needs. Using the Mifflin St. Jeor Equation Mrs. Sanders needs 1,343 kcal resting and her total energy needs are 2,150 kcal. Women: REE = 10 (weight in kg) + 6.25 (height in cm) – 5(age in years) -161 Weight = 160lbs/2.2lb per kg =72.7kg Height = 66in*2.54cm per in =167.6cm REE=10(72.7kg)+6.25(167.6cm)-5(54yr)-161 REE=1,343 kcal Physical Activity Level=1.6 because she does walk 30min 4-5 times a week. Total energy needs=REE*PAL Total energy needs=1,343kcal*1.6 Total energy needs=2,150kcal 18. What nutrients in Mrs. Sanders’s diet are of major concern to you? As a hypertension patient, the nutrients in Mrs. Sanders’s diet that are of major concern to me include saturated fat, sodium, calcium, potassium, fiber, magnesium, and cholesterol. According to her diet recall, Mrs. Sanders is consuming excessive amounts of saturated fat, sodium, and cholesterol. Furthermore, she is not consuming enough magnesium, potassium, or fiber. (Page 292) 19. From the information gathered within the intake domain, list possible nutrition problems using the diagnostic terms. Possible nutrition diagnoses include: Excessive energy intake NI-1.3 Inappropriate intake of fats NI-5.6.2 Excessive sodium intake NI-5.10.2 (7) Overweight/obesity NC-3.3 (1) Food and nutrition-related knowledge deficit NB-1.1 Physical inactivity NB-2.1 20. Dr. Thornton ordered the following labs: fasting glucose, cholesterol, triglycerides, creatinine, and uric acid. He also ordered an EKG. In the following table, outline the indication for these tests (tests provide information related to a disease or condition). Parameter Normal Value Pt’s Value Reason for Abnormality Nutrition Implications Glucose 70-110 mg/dL 92 mg/dL Within normal values Above normal value glucose levels risks for development of type 2 diabetes may be present. BUN 8-18 mg/dL 20mg/dL Creatinine 0.6-1.2 mg/dL 0.9mg/dL Total Cholesterol 120-199 mg/dL 270 mg/dL High, above the normal range Within normal range Too high, Decrease saturated fat and cholesterol above normal intake range Low, below Increase fiber intake normal range High, above Decrease saturated fat and cholesterol normal range intake Low, below Indicates low HDL levels which is normal range higher risk for coronary heart disease High, above Indicates high LDL levels which normal range increases blood pressure Within normal High fat intake range HDLcholesterol LDLcholesterol Apo A Apo B Triglycerides > 55 mg/dL F > 45 mg/dL M <130 mg/dL 101-199 mg/dL F 94-178 mg/dL M 60-126 mg/dL F 63-133 mg/dL M 35-135 mg/dL F 40-160 mg/dL M 30 mg/dL 210 mg/dL 75 mg/dL 140 mg/dL 150 mg/dL 21. Interpret Mrs. Sanders’s risk of CAD based on her lipid profile. When Mrs. Sanders first came in on 6/25 her total cholesterol was 270 mg/dL which gave her more than twice the risk of heard disease compared to someone whose cholesterol is below 200mg/dL. Nine months later Mrs. Sanders is still has a higher risk with borderline high cholesterol of 210mg/dL. Similarly when she first came in her LDL levels were very high at 210mg/dL. Nine months later she still has borderline high levels. Even nine months since her initial visit, however, her HDL levels are still too low at 38mg/dL, which puts her at major risk of heart disease. Finally, her triglyceride levels have decreased from borderline high to normal since her first visit. Mrs. Sanders is still at risk of CAD, however, since her initial visit on 6/25, her risk of CAD has decreased. (Page 301) 22. What is the significance of apolipoprotein A and apolipoprotein B in determining a person’s risk of CAD? An apolipoprotein is the protein portion of a lipoprotein. High levels of apolipoprotein B indicate high levels of LDL, and high levels of apolipoprotein A indicate high levels of HDL. LDL transport cholesterol and lipids to tissues and serum LDL levels are the single strongest indicator of CVD risk. Therefore, the higher the level of apolipoprotein B found, the greater the risk for CAD. Oppositely, since HDL particles are involved in the reverse cholesterol transport (from tissues to the liver) the more apolipoprotein A found, the lower the risk for CVD. (Page 301) 23. Indicate the pharmacological differences among the antihypertensive agents listed below. Medications Diuretics Beta-blockers Calcium-channel blockers ACE inhibitors Mechanism of Action Decreases blood volume by increasing urinary output and inhibits renal sodium and water reabsorption Blocks B-receptors in the heart to decrease heart rate and cardiac output Affect the movement of calcium and cause blood vessels to relax and reduce vasoconstriction Vasodilators that reduce blood pressure by Nutritional Side Effects and Contraindications Potassium supplements may be necessary, avoid natural licorice Calcium may interfere with absorption Avoid natural licorice, limit caffeine, and avoid or limit alcohol Avoid natural licorice, and avoid salt substitutes Angiotensin II receptor blockers Alpha-adrenergic blockers decreasing peripheral vascular resistance by interfering with the production of angiotensin II from angiotensin I and inhibiting degradation of bradykinin Interferes with reninangiotensin system without inhibiting degradation of bradykinin Blocks the vascular muscle response to sympathetic stimulation and reduces stroke volume. Serum potassium may increase; avoid salt substitutes Avoid natural licorice (Page 291) 24. What are the most common nutritional implications of taking hydrochlorothiazide? Hydrocholorothiazide inhibit the resorption of sodium, chloride, and potassium in the loop of Henle of the kidney, which can affect the electrolyte balance. (Page 291) 25. Mrs. Sanders’s physician has decided to prescribe an ACE inhibitor and an HMGCoA reductase inhibitor (Zocor). What changes can be expected in her lipid profile as a result of taking these medications? As a result of taking these medications Mrs. Sander’s blood pressure can be expected to decrease. The ACE inhibitors competitively block the enzyme that converts angiotension I into angiotension II, which results in vasodilation, a decrease in vasopressin release, and a resulting decrease in blood pressure. The HMGCoA reductase inhibitor, Zocor, will lower her LDL cholesterol level by slowing down the synthesis of cholesterol. (Page 292, 217, http://www.ncbi.nlm.nih.gov/books/NBK47273/) 26. How does an ACE inhibitor lower blood pressure? An ACE inhibitor lowers blood pressure by blocking the enzyme that converts angiotension I into angiotension II, which results in vasodilation, a decrease in vasopressin release, and a resulting decrease in blood pressure. Since angiotension I is not able to convert into angiotension II, the blood vessels dialate and relax, which allows less resistance in the blood so that there is a lower blood pressure. (Page 292) 27. How does an HMGCoA reductase inhibitor lower serum lipid? HMGCoA reductase inhibitor lowers serum lipid by inhibiting the production of an enzyme needed to produce cholesterol. The liver responds by producing extra LDL receptors which reduce the amount of LDL in the bloodstream, which consequently lowers blood pressure. (https://provider.ghc.org/open/caringForOurMembers/patientHealthEducation/conditions Diseases/statins.pdf) 28. What other classes of medications can be used to treat hypercholesterolemia? Hypercholesterolemia can be treated through the use of diuretics, aldosterone antagonists, nitrate, digitalis, fibrinolytic therapy, and positive inotropic drugs. (Page 291) 29. What are the pertinent drug-nutrient interactions and medical side effects for ACE inhibitors and HMGCoA reductase inhibitors? Side effects of ACE inhibitors include hypotension (especially in elderly patients), worsening renal function, hyperkalemia, dysguesia, dry/non productive cough, interactions with natural licorice and salt substitutes. Side effects for HMGCoA reductase inhibitors (also called statins) include interactions with grapefruit, and alcohol. They should be taken on a low fat and low cholesterol diet and may cause constipation, stomach pain, nausea, headaches, or memory loss. (Page 291, 217) 30. From the information fathered within the clinical domain, list possible nutrition problems using diagnostic terms. Overweight/obesity NC-3.3 (1) Altered nutrition-related laboratory values: High cholesterol of 270mg/dL NC-2.2 31. What are some possible barriers to compliance? Some possible barriers to compliance include Mrs. Sanders not complying with a low sodium diet because she feels that the food lacks flavor without the salt, and Bingo night. It seems that on bingo night Mrs. Sanders forgoes her exercise and diet program. It would also be helpful for both Mr. and Mrs. Sanders to be on the same page and work together to be healthy. IV. Nutrition Diagnosis 32. Select two nutrition problems and complete the PES statement for each. a. Excessive sodium intake related to frequent consumption of high sodium foods as evidenced by patient’s 24-hour diet recall and high blood pressure of 160/100mmHg. b. High cholesterol related to inappropriate intake of fats as evidenced by patient’s 24-hour diet recall and cholesterol lab results of total cholesterol of 270mg/dL with high LDL levels of 210mg/dL and low HDL levels of 30 mg/dL. V. Nutrition Intervention 33. When you ask Mrs. Sanders how much weight she would like to lose, she tells you should would like to weigh 125, which is what she weighed most of her adult life. Is this reasonable? What would you suggest as a goal for weight loss for Mrs. Sanders? Using the Hamwi Method, Mrs. Sanders’s ideal weight would be 130lbs. 100lbs for the first 5 feet of ht + 5 lbs for every inch over 5 feet: 100 + 5 (6in over 5 feet) =130lbs Therefore, 125 is a pretty reasonable weight goal for Mrs. Sanders, although it would be slightly lower than ideal. I would suggest she have a goal of 130lb as calculated by the Hamwi Method. (Page 48) 34. How quickly should Mrs. Sanders lose this weight? Mrs. Sanders should lose this weight gradually so that she will be more likely to keep the weight off. She could lose 1 to 2 lbs a week and lose the 30lbs in 4-7 months. (Page 264) 35. For each of the PES statements that you have written, establish an ideal goal (based on the signs and symptoms) and an appropriate intervention (based on the etiology). a. Lower blood pressure to <120/80mmHg by educating patient on ways to add flavor to foods without adding salt and implementing the DASH diet with less than 2300mg salt a day. b. Reduce total cholesterol to <200mg/dL, lower LDL level to <130 mg/dL, and raise HDL level to >55 mg/dL by educating patient on the importance of and how to implement the DASH diet plan into her daily life. 36. Identify the major sources of sodium, saturated fat, and cholesterol in Mrs. Sanders’s diet. What suggestions would you make for substitutions and/or other changes that would help Mrs. Sanders reach her medical nutrition therapy goals? According to her diet recall, the major sources of sodium in Mrs. Sanders’s diet include canned tomato soup, saltine crackers, and table salt added to flavor foods. I would advise her to buy low sodium tomato soup or make her own at home, eat lowersodium whole-wheat crackers instead of saltines, and try to add spices and herbs instead of salt to flavor her foods. The saturated fat and cholesterol in her diet comes from salad dressing, donuts, added butter, and ice cream. I would advise her to limit her dessert intake, maybe have either a donut or ice cream in a day instead of both. She could buy lower fat dressings or oil-based dressings for her salad. She could also try to cook with oil instead of butter, or try adding nut butter to her oatmeal instead of margarine. 37. What would you want to reevaluate in three to four weeks at a follow-up appointment? In three to four weeks I would want to reevaluate her efforts to eat lower sodium foods and how she is doing with her walking program. I would check her weight and cholesterol levels. I would also measure her blood pressure. Hopefully her progress will be positive after she has implemented the diet changes. 38. Evaluate Mrs. Sanders’s labs at six months and then at nine months. Describe the changes that have occurred. Mrs. Sanders’s labs at six and nine months illustrate that she had made progress! Her HDL has increased and LDL has decreased so that her total cholesterol level has decreased. Her triglycerides have also decreased. While still not where they need to be, her lipid profile is showing that she has made progress and that the program is working. Mrs. Sanders’s BUN, glucose, Bilirubin, and RBC have all also decreased. These results should help provide encouragement and motivation to help Mrs. Sanders stay with her program. References Academy of Nutrition and Dietetics. (2005). Evidence Analysis Library: What evidence suggests a relationship between sodium intake and blood pressure in healthy and hypertensive adults? Retrieved from http://andevidencelibrary.com/conclusion.cfm?conclusion_statement_id=250636 &highlight=sodium&home=1 Group Health Cooperative. (2011). Statins & ACE Inhibitors. Retrieved from https://provider.ghc.org/open/caringForOurMembers/patientHealthEducation/con ditionsDiseases/statins.pdf. Nelms M, Sucher K, Lacey, K., Habash, D., Roth S. Nutrition Therapy and Pathophysiology. 2nd ed.Belmonte, CA: Thomson Brooks/Cole, 2010. Net Industries Science Encyclopedia. (2013). Hypertension-Prognosis. Retrieved from http://science.jrank.org/pages/3488/Hypertension-Prognosis.html. Smith MEB, Lee NJ, Haney E, et al. Drug Class Review: HMG-CoA Reductase Inhibitors (Statins) and Fixed-dose Combination Products Containing a Statin: Final Report Update 5 [Internet]. Portland (OR): Oregon Health & Science University; 2009 Nov. Retrieved from: http://www.ncbi.nlm.nih.gov/books/NBK47273/ Zelman K. (2012). Salt Shockers. Retrieved from http://www.webmd.com/diet/ss/slideshow-salt-shockers.