SUPPLEMENTAL MATERIAL (Online data supplement) for
advertisement
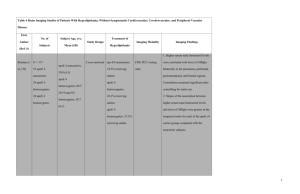
SUPPLEMENTAL MATERIAL (Online data supplement) for “Prevalence and management of familial hypercholesterolemia in patients with acute coronary syndromes” David Nanchen et al. Methods Supplemental Material Table S1 Dutch Lipid Clinic Network criteria for diagnosis of familial hypercholesterolemia (FH) (n=4,778) Table S2 Simon Broome Register criteria for diagnosis of familial hypercholesterolemia (FH) (n=4,778) Table S3 Baseline characteristics of patients with acute coronary syndrome (ACS), by use of lipid lowering drugs before hospital admission (n=4,778) Figure S1 Selection of study sample Figure S2 Venn diagram for agreement between definitions of familial hypercholesterolemia (n=4,778) Figure S3 Prevalence of familial hypercholesterolemia (FH), by use of lipid lowering drugs before hospital admission a) patients not using lipid lowering drugs before hospitalization (n=3,353) b) patients using lipid lowering drugs before hospitalization (n=1,425) Figure S4 Sensitivity analyses for prevalence of familial hypercholesterolemia (FH) among patients hospitalized for acute coronary syndrome (n=4,778) 1 Methods Supplemental material Study population The SPUM-ACS (Special Program University Medicine-Acute Coronary Syndromes) research network included patients hospitalized from September 2009 to September 2014 for an ACS in 4 university medical centers in Switzerland (University hospital of Bern (BE), Geneva (GE), Lausanne (LA) and Zürich (ZH)). Exclusion criteria comprised severe physical disability, inability to participate or severe non-cardiac comorbidities leading to short life expectancy. ACS was defined as the combination of symptoms of angina pectoris and at least one of the following characteristics: ST-segment elevation or depression, T inversion or dynamic ECG changes, evidence of positive troponin and known coronary heart disease (CHD). The final ACS diagnosis was classified as STEMI (ST-segment elevation myocardial infarction), NSTEMI (non STsegment elevation myocardial infarction), or unstable angina. LDL-cholesterol assessment Total cholesterol, HDL-cholesterol and triglycerides were measured from the first blood draw at the emergency department, within 24 hours of admission, and immediately processed locally using standardized and certified dosage methods. LDL-cholesterol was calculated using the Friedewald formula when triglyceride levels were below 4.5 mmol/l. LDL-cholesterol was considered as missing for patients with triglyceride levels of 4.5 mmol/l or above. Because patients with FH can have elevated triglyceride levels explained by genes and environmental interactions, we did not exclude patients with high triglycerides levels (>= 2.3 mmol/l) from our study sample.1 However, only patients with normal triglyceride levels (< 2.3 mmol/l) received scoring for elevated LDL-cholesterol levels as recommended by the Dutch Lipid Clinic Network 2 score for FH diagnosis.2 For patients using lipid-lowering drugs before hospitalization for ACS, we estimated untreated LDL-cholesterol levels based on type and dose of medication used before hospitalization, applying a correcting factor for LDL-cholesterol adapted to the reported efficacy of each drug, as previously done for similar analysis.3 One-year after hospitalization for ACS, LDL-cholesterol levels were measured during the follow-up visit or extracted from laboratory files of the physician in charge of the patient. Use of lipid-lowering drugs HMG-CoA reductase inhibitors (statins) that were taken prior to hospitalisation and prescribed at discharge were systematically collected by trained study nurses. Type and dose of statins were classified in three groups according to their intensity: (1) high-dose statins included atorvastatin 40-80mg or rosuvastatin 20-40mg; (2) moderate-dose statins included atorvastatin 10-20mg or rosuvastatin 5-10 mg or simvastatin 20-40 mg or pravastatin 40-80 mg or fluvastatin 80 mg; and (3) low-dose statins included simvastatin 10 mg or pravastatin 10-20mg or fluvastatin 20-40 mg. Other lipid lowering agents than statins included fibrates, niacin, ezetimibe and bile acid resins. For patients identified with FH, optimal statin management after discharge was defined as the use of high-dose statins, 50% decrease in LDL-cholesterol levels, or a LDL-cholesterol equal or below 1.8 mmol/l, as recommended by lipid guidelines.4 Covariables Personal history of premature CHD was considered positive when men were younger than 55 years old and women younger than 60 years old at the time of ACS.5 Family history of premature atherosclerosis was based on patient reports of a major cardiovascular event in a brother or father 3 younger than 55 years old, or a mother or sister younger than 60 years old. Education status was dichotomized as having followed a high school or university graduation, or lower. Hypertension was defined as a systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg or use of blood pressure lowering drugs. Blood pressure lowering drugs included all medications in the classes of angiotensin converting enzyme inhibitors, angiotensin II receptor blockers, betablockers, calcium-channel blockers, diuretics and nitrates. Smoking status was categorized into current, former and never-smokers. Former smokers were those who smoked at least one cigarette a day during at least one-year, and were non-smokers for more than one month before inclusion. Diabetes, was either self-reported or diagnosed by the use of anti-diabetic medication, or a hemoglobin A1c of 6.5% or greater at admission. Pre-existing cardiovascular disease was defined as a previous diagnosis of CHD, ischemic cerebrovascular disease or periphery artery disease. Attendance rate to cardiac rehabilitation was assessed from administrative data available at discharge. References 1. Hovingh GK, Davidson MH, Kastelein JJ, O'Connor AM. Diagnosis and treatment of familial hypercholesterolaemia. Eur Heart J 2013;34:962-971. 2. Civeira F, International Panel on Management of Familial H. Guidelines for the diagnosis and management of heterozygous familial hypercholesterolemia. Atherosclerosis 2004;173:55-68. 3. Besseling J, Kindt I, Hof M, Kastelein JJ, Hutten BA, Hovingh GK. Severe heterozygous familial hypercholesterolemia and risk for cardiovascular disease: a study of a cohort of 14,000 mutation carriers. Atherosclerosis 2014;233:219-223. 4 4. European Association for Cardiovascular P, Rehabilitation, Reiner Z, Catapano AL, De Backer G, Graham I, Taskinen MR, Wiklund O, Agewall S, Alegria E, Chapman MJ, Durrington P, Erdine S, Halcox J, Hobbs R, Kjekshus J, Filardi PP, Riccardi G, Storey RF, Wood D. ESC/EAS Guidelines for the management of dyslipidaemias: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur Heart J 2011;32:1769-1818. 5. Nordestgaard BG, Chapman MJ, Humphries SE, Ginsberg HN, Masana L, Descamps OS, Wiklund O, Hegele RA, Raal FJ, Defesche JC, Wiegman A, Santos RD, Watts GF, Parhofer KG, Hovingh GK, Kovanen PT, Boileau C, Averna M, Boren J, Bruckert E, Catapano AL, Kuivenhoven JA, Pajukanta P, Ray K, Stalenhoef AF, Stroes E, Taskinen MR, TybjaergHansen A. Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: guidance for clinicians to prevent coronary heart disease: consensus statement of the European Atherosclerosis Society. Eur Heart J 2013;34:3478-3490a. 5 Table S1 Dutch Lipid Clinic Network criteria for diagnosis of familial hypercholesterolemia (FH) (n=4,778) % subject Variable Grading scoring (number) First degree relative with known premature atherosclerosis OR with known LDL-cholesterol > 95th percentile, OR personal history of premature (< 55 years men; < 60 years women) 36.8 1 point (1,758) cerebral or peripheral vascular disease, OR LDL-cholesterol 4.04.9 mmol/l* Personal history of premature (< 55 years men; < 60 years women) coronary heart disease OR first-degree relative with tendon xanthomata and/or arcus cornealis OR first-degree relative 30.4 2 points (1,451) child below 18 years with LDL-cholesterol > 95th percentile OR LDL-cholesterol 5.0-6.4 mmol/l* 3 points Presence of arcus cornealis below 45 years 4 points LDL-cholesterol 6.5-8.4 mmol/l* 5 points Presence of tendon xanthomata 6 points LDL-cholesterol > 8.5 mmol/l* OR functional mutation in LDL receptor gene present 8 points NA, not available * Only in those with triglyceride levels < 2.3 mmol/l Possible FH: 3-5 points; probable FH: 6-7 points; definite FH >= 8 points 6 5.5 (265) NA 1.0 (49) NA 0.08 (4) Table S2 Simon Broome Register criteria for diagnosis of familial hypercholesterolemia (FH) (n=4,778) Total cholesterol > 7.5 mmol/l OR LDL-cholesterol >4.9 mmol/l AND % subject Grading scoring (number) First degree relative with known premature atherosclerosis (< 55 years men; < 60 years women) Possible FH Personal history of premature (< 55 years men; < 60 years women) coronary heart disease Possible FH Definite Tendon xanthomas FH Definite DNA mutation FH NA, not available 7 2.7 (128) 4.2 (203) NA NA Table S3 Baseline characteristics of patients with acute coronary syndrome (ACS), by use of lipid lowering drugs before hospital admission (n=4,778) Number Demographics Age, years Female Caucasian Higher education1 Premature CHD2 Family history3 Smoking status Never Former Current Comorbidities Hypertension4 Diabetes mellitus5 Pre-existing CVD6 Objective measures Total cholesterol, mmol/L LDL-cholesterol, mmol/L7 HDL-cholesterol, mmol/L Triglycerides, mmol/L Body mass index, kg/m2 eGFR, ml/min Medication use at admission Aspirin Anti-hypertensives Not using lipid lowering drugs 3,353 Using of lipid lowering drugs 1,425 p-value 61.7 (12.6) 727 (21.7) 3,155 (94.1) 871 (29.3) 1,191 (35.5) 806 (24.4) 66.6 (11.4) 281 (19.7) 1,340 (94.0) 293 (24.2) 260 (18.2) 407 (28.9) <0.001 0.13 0.4 0.001 <0.001 0.001 <0.001 1,058 (31.9) 838 (25.2) 1,425 (42.9) 434 (30.9) 560 (39.8) 412 (29.3) 1,564 (46.7) 409 (12.2) 409 (12.2) 1,088 (76.4) 447 (31.4) 831 (58.3) <0.001 <0.001 <0.001 5.2 (1.2) 3.4 (1.0) 1.2 (0.4) 1.4 (1.0) 26.9 (4.3) 90.5 (26.5) 4.3 (1.1) 2.5 (1.0) 1.2 (0.4) 1.5 (1.3) 27.6 (4.3) 84.9 (27.5) <0.001 <0.001 <0.001 0.041 <0.001 <0.001 475 (14.2) 1,091 ( 32.5) 991 (69.6) 1,113 (78.1) <0.001 <0.001 Data are given as number (percentage) or mean (standard deviation) Abbreviations: CHD, coronary heart disease; CVD, cardiovascular disease; LDL, low-density lipoprotein; HDL, high-density lipoprotein; eGFR, estimated glomerular filtration rate 8 Defined as a high school or university graduation or higher 2 Age of onset for ACS before 55 years in males and before 60 in females 3 Based on major cardiovascular event in a brother or father younger than 55 years old, or a mother or sister younger than 60 years old 4 Defined as a systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg or use of blood pressure lowering drugs 5 Based on patients self-report, use of anti-diabetic medication/insulin or hemoglobin A1c of ≥6.5% 6 Defined as coronary heart disease, ischemic cerebrovascular disease or periphery artery disease 7 Including 65 missing values because of elevated triglycerides level of 4.5 mmol/l or above 9 Figure S1: Selection of study sample 10 Figure S2: Venn diagram for agreement between definitions of familial hypercholesterolemia (n=4,778) 11 Figure S3: Prevalence of familial hypercholesterolemia (FH), by use of lipid-lowering drugs before hospital admission a) patients not using lipid-lowering drugs before hospitalization (n=3,353) 12 b) patients using lipid-lowering drugs before hospitalization (n=1,425) 13 Figure S4: Sensitivity analyses for prevalence of familial hypercholesterolemia (FH) among patients hospitalized for acute coronary syndrome (n=4,778) 14