File
advertisement
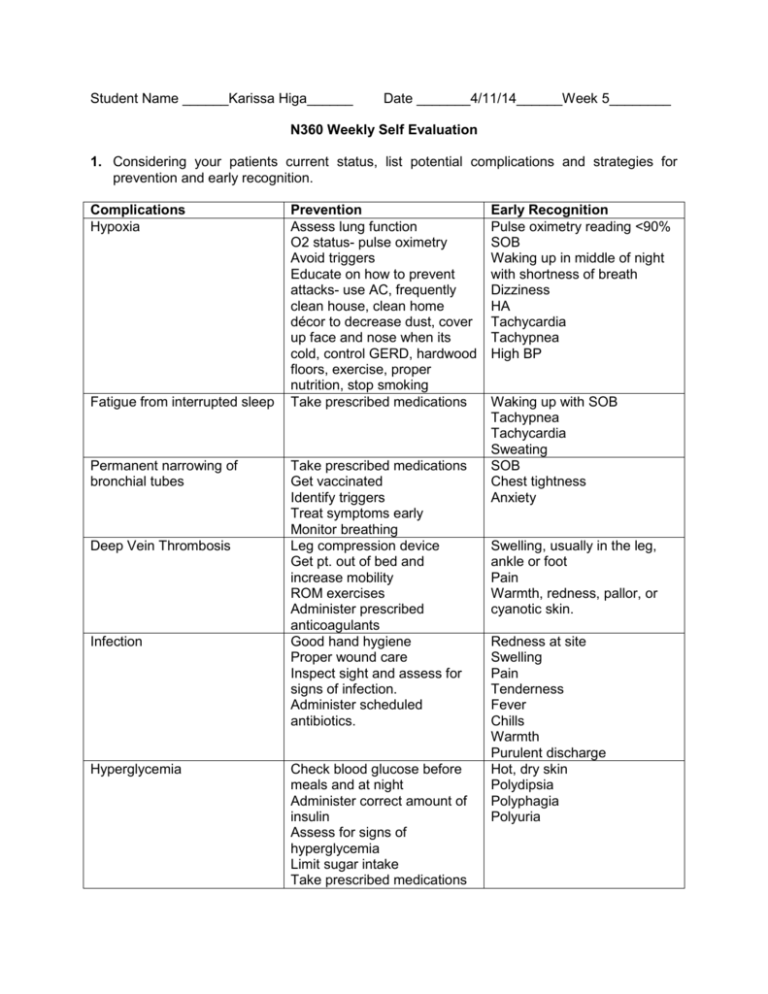
Student Name ______Karissa Higa______ Date _______4/11/14______Week 5________ N360 Weekly Self Evaluation 1. Considering your patients current status, list potential complications and strategies for prevention and early recognition. Complications Hypoxia Fatigue from interrupted sleep Permanent narrowing of bronchial tubes Deep Vein Thrombosis Infection Hyperglycemia Prevention Assess lung function O2 status- pulse oximetry Avoid triggers Educate on how to prevent attacks- use AC, frequently clean house, clean home décor to decrease dust, cover up face and nose when its cold, control GERD, hardwood floors, exercise, proper nutrition, stop smoking Take prescribed medications Take prescribed medications Get vaccinated Identify triggers Treat symptoms early Monitor breathing Leg compression device Get pt. out of bed and increase mobility ROM exercises Administer prescribed anticoagulants Good hand hygiene Proper wound care Inspect sight and assess for signs of infection. Administer scheduled antibiotics. Check blood glucose before meals and at night Administer correct amount of insulin Assess for signs of hyperglycemia Limit sugar intake Take prescribed medications Early Recognition Pulse oximetry reading <90% SOB Waking up in middle of night with shortness of breath Dizziness HA Tachycardia Tachypnea High BP Waking up with SOB Tachypnea Tachycardia Sweating SOB Chest tightness Anxiety Swelling, usually in the leg, ankle or foot Pain Warmth, redness, pallor, or cyanotic skin. Redness at site Swelling Pain Tenderness Fever Chills Warmth Purulent discharge Hot, dry skin Polydipsia Polyphagia Polyuria Hypoglycemia Hypothermia Pain at surgical site Respiratory Depression r/t PCA Compartment Syndrome Constipation as ordered Educate pt on symptoms of hyperglycemia Educate on correct insulin administration Check blood glucose before meals and at night Administer correct amount of insulin Assess for signs of hypoglycemia Ensure meals are eaten after insulin administration Educate pt on symptoms of hypoglycemia Don’t drink alcohol or smoke out in cold Protect body from cold by wearing gloves, layered clothing, two pairs of socks, scarf, and/or hat Avoid cold weather with high winds and wet clothes Educate on PCA use, report pain to the nurse Premedicate pt w/ pain meds before therapy or getting OOB Support surgical limb when turning or moving pt. Apply ice pack Provided non-pharmocological pain relieving methods Check PCA machine to make sure settings are correct Assess respiratory status of pt Educate family that only the pt should be pushing the button Educate pt on how to use PCA and its side effects Adjust dose as needed, as ordered by physician. Assess pain level CMS check Assess skin color below surgical site and around Assess perfusion below site Call MD if pain medications do not alleviate pain Encourage fluids and mobility Tachycardia Irritable Restless Polyphagia Diaphoresis Cool, clammy skin Depression Blurred vision Seizure Coma Shivering Shallow, slow breathing Confusion Drowsiness Slurred speech Pale, cool skin Slow, weak pulse Arrhythmias Heart failure Pt verbally announces pain Non verbal cues: grimacing, guarding site with hands, tachypnea, tachycardia, wincing, restless, crying, combative. Slow breathing <12 breaths/min Decreased LOC Shallow breaths Confusion Cyanosis Weakness Increased pain, medications do not help Decreased sensation Numbness/tingling Pale skin Weakness Distended abdomen Increase fiber in diet Administer stool softeners and laxatives (if needed) Assess bowel sounds, palpate, and shape of abdomen No BM in last 3 days Abdominal discomfort or pain Feeling that you can’t completely empty rectum Straining to have a BM 2. Am I getting more comfortable with the use of the nursing process to plan and evaluate nursing care? (Give examples of how it is better now or problems that still bother you). Yes. It is the 5th week and I feel comfortable with the nursing process. I am able to create a mini care plan specific to my patients and implement them in my care. I am also able to adapt to any given changes my patient may have. For example, my first pt was admitted for respiratory problems but I ended up focusing on his blood sugar level and his body temperature. I was able to change my focused assessment to monitoring for hyper or hypoglycemia and preventing further hypothermia. 3. Were my nursing diagnosis and plan of care individualized for my patients? (Give examples of how you did this.) Do I have difficulty in this area? (Explain). Yes, however like I stated before the situation changed but I was ready to adapt. I went in thinking I was going to focus on his respiratory status but ended up focusing on his diabetes and hypothermia. I made sure he wasn't showing any signs of hypoglycemia or hypothermia. I also continued to monitor his temperature and status throughout the day. 4. How are my assessment skills developing? Am I being as thorough as I need to be? What areas are still difficult for me and what am I doing to improve? (Be specific). I think I am getting used to all my assessments. As I keep doing my head to toe every week I seem to be getting better and it is becoming easier to perform. I also have been feeling comfortable doing my focused assessments like respiratory status, wound assessment, or looking for any signs of infection. 5. What new skills did I implement this week? How did I do? What could have helped me to improve? Did I ask for help when I needed it? I got to work with a hypothermia patient whose temperature was 35C. I managed my time well and did frequent checks on his temperature. I made sure to keep him warm and by the end of my shift his temperature was going back up. 6. How is my time management progressing? What areas of difficulty have I found and what can I do to improve? How do I monitor my time management while in the clinical area? This week I thought my time management was good. I was able to finish all my medications and give a bed bath to my patient. I also had to feed him his meals and clean him up when he soiled his briefs. I also finished my dressing change on time. Working with two patients kept me busy but I was still able to finish on time and do CNA tasks. 7. Was I involved in making referrals for my client in any way? How could the nursing role in this process have been strengthened? This week I worked with a patient whose primary language wasn't English. However, the primary nurse spoke the same language and we got a little response out of him. The nurse explained to him what was going on and asked about any pain, SOB, etc. I also made a referral for my second patient to the primary nurse who then called the doctor. He had an issue about the PCA function and I told my nurse about his problem, who was also informed by the night shift nurse. At the end of my shift I reminded my nurse about the problem and I’m hoping she ordered a new pump. 8. List the specific interventions, in order of priority, for two of your clients and explain how you determined which interventions took precedent. Assess breathing pattern, vital signs, signs of hyper or hypoglycemia, hypothermia, check labs, assess IV site, assess mittens to ensure proper circulation, assess heel ulcer, and assess butt excoriation. Head to toe assessment, pain (use FACES) Report any changes to primary nurse and instructor Administer prescribed medications Repositions q2h Heel dressing change Monitor glucose level and temperature Provide warming measures if needed- extra blankets, towel over head and around neck, or get order for bear hug. Focused assessments are always priority for me because that is the reason why the patient has been admitted in the first place. I want to make sure there are no complications going on caused by the primary diagnosis. Then I want to go ahead and finish up my head to toe assessment to get an idea of the patient’s overall status. Next I want to report any changes to my instructor and nurse to keep the both updated. After all my assessments I can evaluate if it is proper to administer all medications (check blood pressure and pulse before giving blood pressure medications). After medications and can do the dressing change and assess the wound site. Lastly, I want to monitor my patient for any acute changes and take the proper action if complications do arise. CMS check, surgical site assessment, pain level, respiratory status, mobility, and assess IV site. Check PCA machine to make sure it is working properly and set at the correct dose. Head to toe assessment Report changes to primary RN Administer prescribed medication Encourage IS use Administer prn medications if needed I always do assessments first to get a better picture of what my patient looks like now so I can plan my day accordingly. I can read the charts but it won’t give me an updated picture of how the patient is today. After assessments I can give the proper medications, making sure it is safe to administer. After that I can encourage my patient to use the IS to prevent pneumonia and get OOB, if tolerable, to prevent constipation and promote a quicker recovery. If his pain persisted I could have given him prn medication, but pt refused when asked.