Psychopharmacy/Neurology Rotation Goal The goal for training in
advertisement
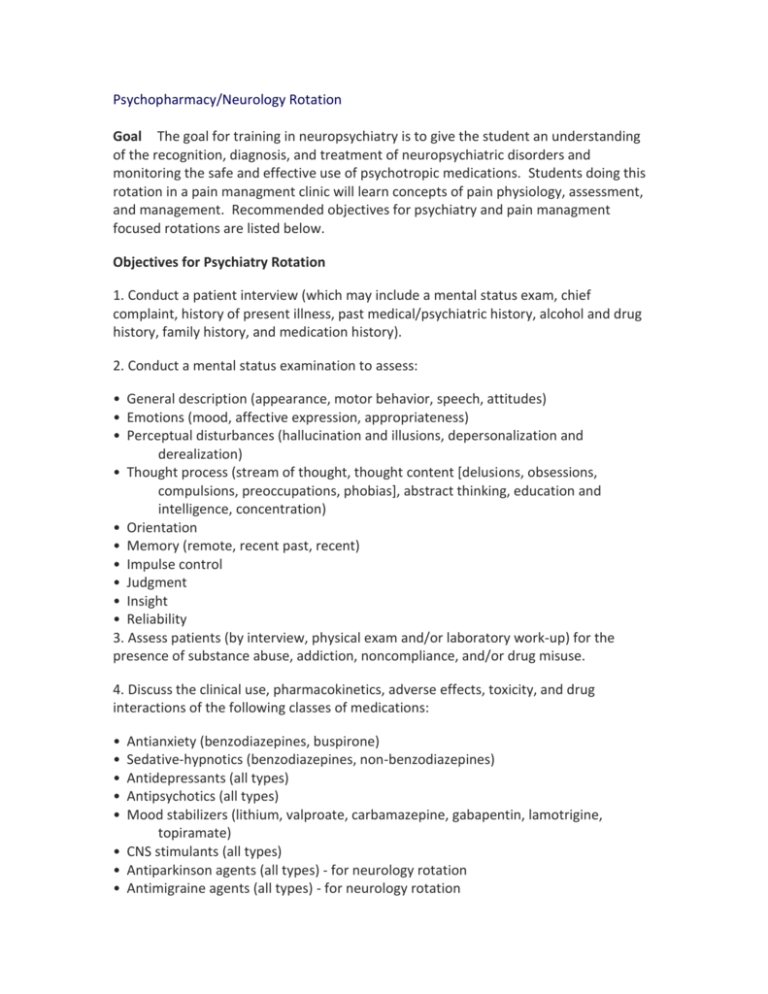
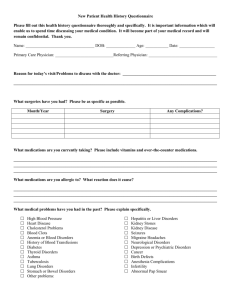
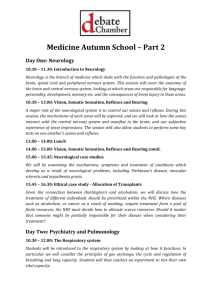
Psychopharmacy/Neurology Rotation Goal The goal for training in neuropsychiatry is to give the student an understanding of the recognition, diagnosis, and treatment of neuropsychiatric disorders and monitoring the safe and effective use of psychotropic medications. Students doing this rotation in a pain managment clinic will learn concepts of pain physiology, assessment, and management. Recommended objectives for psychiatry and pain managment focused rotations are listed below. Objectives for Psychiatry Rotation 1. Conduct a patient interview (which may include a mental status exam, chief complaint, history of present illness, past medical/psychiatric history, alcohol and drug history, family history, and medication history). 2. Conduct a mental status examination to assess: • General description (appearance, motor behavior, speech, attitudes) • Emotions (mood, affective expression, appropriateness) • Perceptual disturbances (hallucination and illusions, depersonalization and derealization) • Thought process (stream of thought, thought content [delusions, obsessions, compulsions, preoccupations, phobias], abstract thinking, education and intelligence, concentration) • Orientation • Memory (remote, recent past, recent) • Impulse control • Judgment • Insight • Reliability 3. Assess patients (by interview, physical exam and/or laboratory work-up) for the presence of substance abuse, addiction, noncompliance, and/or drug misuse. 4. Discuss the clinical use, pharmacokinetics, adverse effects, toxicity, and drug interactions of the following classes of medications: • • • • • Antianxiety (benzodiazepines, buspirone) Sedative-hypnotics (benzodiazepines, non-benzodiazepines) Antidepressants (all types) Antipsychotics (all types) Mood stabilizers (lithium, valproate, carbamazepine, gabapentin, lamotrigine, topiramate) • CNS stimulants (all types) • Antiparkinson agents (all types) - for neurology rotation • Antimigraine agents (all types) - for neurology rotation • Analgesics and opioids (all types ) - for pain rotation • Anticonvulsants (all types) - for epilepsy rotation 5. Recommend or initiate the collection of laboratory data relevant to developing a pharmacotherapeutic plan. 6. Identify possible drug-induced abnormalities and develop a differential diagnosis and plan to support or rule out a drug-induced etiology for psychiatric, neurologic or medical illness. 7. Recognize potential drug-drug interactions with medications and recommend monitoring parameters, changes in pharmacotherapy, and alternative therapies to minimize adverse effects. 8. Identify the symptoms and diagnostic criteria for the most common psychiatric disorders as described in the Diagnostic and Statistical Manual of Mental Disorders, IVTM - revised (2000). 9. Initiate, recommend and/or monitor the pharmacotherapy for the major psychiatric and/or neurologic disorders and recommend modifications in drug therapy based upon the patient's presentation, target symptoms, progress, and adverse effects. 10. Discuss the pathophysiology, clinical diagnosis, and pharmacotherapy of the following psychiatric and neurologic disorders: • Mood disorders (major depressive disorder, bipolar disorders) • Anxiety disorders (agoraphobia, generalized anxiety disorder, obsessive-compulsive disorder, panic disorder, posttraumatic stress disorder, social phobia, specific phobia) • Sleep disorders (insomnia, sleep apnea, narcolepsy) • Psychotic disorders (schizophrenia, schizoaffective disorder) • Parkinsonism (for neurology rotation) • Migraine headache (for neurology rotation) • Acute and chronic pain (for pain rotation) • Seizure disorders (for epilepsy rotation) 11. Review and evaluate the psychiatric, neurologic, medical, and/or pharmaceutical literature as it applies to the neuropsychiatric patient. 12. Provide medication education and counseling regarding drug therapy to psychiatric or neurological patients and families. 13. Serve as an educational resource regarding drug therapy for staff and trainees working in the psychiatry and/or neurology setting. 14. When possible, conduct research and scholarly activities applicable to the care of psychiatric and/or neurologic patients and the development of psychopharmacy practice. 15. Serve on a health care team and provide pharmaceutical care services to selected patients under the supervision of a physician. Objectives for Pain Management Rotation 1. Summarize the general pathology or etiology and natural history of common chronic pain problems. 2. Discuss the basic pharmacology and anatomy of the pain-sensing nervous system. 3. Describe the different types of pain: nociceptive, neuropathic, and visceral and explain the implications for pharmacotherapy for each type of pain. 4. Explain the types of pain assessment and common pitfalls in pain assessment. 5. Identify common adverse effects for different types of pain medications and appropriate monitoring parameters for assessing and treating adverse effects. 6. Discuss the myths and realities of addiction and tolerance when using opiates in the management of acute and chronic pain. 7. Explain the reason for different mechanisms of pharmacology or pharmacotherapy for common acute and chronic pain states. 8. Discuss the past barriers to effective pharmacologic treatment of cancer pain. 9. Describe the World Health organization (WHO) analgesic ladder for cancer pain. 10. Describe the shortcomings of traditional “on-demand” analgesia to acute pain management and the rationale for the use of “patient-controlled” analgesia, including the potential hazards. 11. Design a plan for initiating, monitoring, and discontinuing pain therapy for patients with acute and chronic pain syndromes. 12. Construct a plan for deciding when pain medications should be changed and plans for switching or discontinuing therapy. 13. Formulate a plan for monitoring adverse effects for different pain medications and for treatment approaches to minimize adverse effects. 14. Design a plan for assessing, treating, and monitoring a patient that is opiate dependent with an acute pain syndrome. 15. Formulate a scheme for deciding when alternative pain management therapies may be needed and recommended (e.g., physical therapy, acupuncture, epidurals, stimulators). 16. Design a plan for assessing, recommending, and monitoring nonpharmacological alternatives for treating pain syndromes, including psychological, social, and invasive therapies. 17. Observe and describe non-pharmacological treatments of back pain with or without radicular pain such as interventional procedures (injection therapy such as trigger point, joints, neural blockade, implant therapies such as spinal cord stimulator, neuraxial analgesia) 18. Recommend a plan for the dosing conversion of different types of opiates and different product formulations (e.g., oral to IV, IV to oral, morphine to 19. 20. 21. 22. 23. 24. methadone) using morphine equivalent conversion standards. Describe the benefits, hazards, and indications of epidural analgesia for acute pain, including side effects of local anesthetic narcotics. Describe the pharmacokinetics and pharmacodynamics of commonly used spinally administered medications for acute pain. Name three antidepressants that are used for the treatment of chronic pain syndromes and common adverse effects or drug interactions associated with each antidepressant. Name three anticonvulsants that are used for the treatment of chronic pain syndrome and common adverse effects or drug interactions associated with each anticonvulsant. Recommend a PCA regimen for different types of pain patients and monitoring parameters. Describe protocols for the continuous infusion of narcotics and local