lecture_2014-12-01141745605098872156547ca9b2bd64d
Diseases of the Immune System
(autoimmune diseases) Lec.2
2014-
2015
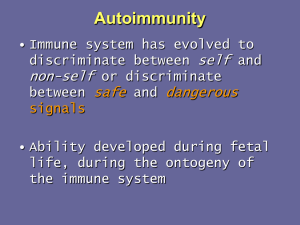
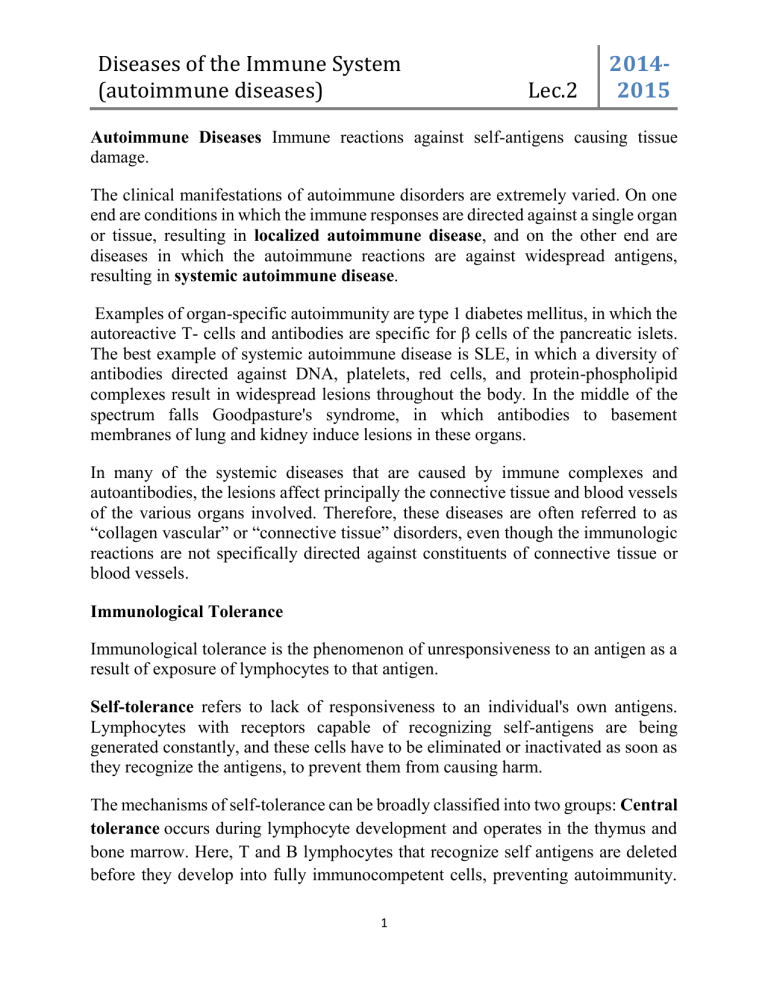
Autoimmune Diseases Immune reactions against self-antigens causing tissue damage.
The clinical manifestations of autoimmune disorders are extremely varied. On one end are conditions in which the immune responses are directed against a single organ or tissue, resulting in localized autoimmune disease , and on the other end are diseases in which the autoimmune reactions are against widespread antigens, resulting in systemic autoimmune disease .
Examples of organ-specific autoimmunity are type 1 diabetes mellitus, in which the autoreactive T- cells and antibodies are specific for β cells of the pancreatic islets.
The best example of systemic autoimmune disease is SLE, in which a diversity of antibodies directed against DNA, platelets, red cells, and protein-phospholipid complexes result in widespread lesions throughout the body. In the middle of the spectrum falls Goodpasture's syndrome, in which antibodies to basement membranes of lung and kidney induce lesions in these organs.
In many of the systemic diseases that are caused by immune complexes and autoantibodies, the lesions affect principally the connective tissue and blood vessels of the various organs involved. Therefore, these diseases are often referred to as
“collagen vascular” or “connective tissue” disorders, even though the immunologic reactions are not specifically directed against constituents of connective tissue or blood vessels.
Immunological Tolerance
Immunological tolerance is the phenomenon of unresponsiveness to an antigen as a result of exposure of lymphocytes to that antigen.
Self-tolerance refers to lack of responsiveness to an individual's own antigens.
Lymphocytes with receptors capable of recognizing self-antigens are being generated constantly, and these cells have to be eliminated or inactivated as soon as they recognize the antigens, to prevent them from causing harm.
The mechanisms of self-tolerance can be broadly classified into two groups: Central tolerance occurs during lymphocyte development and operates in the thymus and bone marrow. Here, T and B lymphocytes that recognize self antigens are deleted before they develop into fully immunocompetent cells, preventing autoimmunity.
1
Diseases of the Immune System
(autoimmune diseases) Lec.2
2014-
2015
Some self-reactive B cells may not be deleted but may undergo a second round of rearrangement of antigen receptor genes and then express new receptors that are no longer self-reactive (a process called “ receptor editing
”).
Peripheral tolerance is immunological tolerance developed after T and B cells mature and enter the periphery. Peripheral tolerance achieved by several mechanisms:
1.
Anergy: This refers to prolonged or irreversible functional inactivation of lymphocytes, induced by encounter with antigens under certain conditions.
The activation of antigen-specific T cells requires two signals: recognition of peptide antigen in association with self-MHC molecules on the surface of
APCs and a set of co-stimulatory signals (“second signals”) from APCs.
These second signals are provided by certain T cell–associated molecules, such as CD28, that bind to their ligands (the co-stimulators B7) on APCs. If the antigen is presented by cells that do not bear the co-stimulators a negative signal is delivered, and the cell becomes anergic.
2.
Suppression by regulatory T cells: A population of T cells called regulatory
T cells plays a major role in preventing immune reactions against selfantigens.
3.
Deletion by activation-induced cell death : CD4+ T cells that recognize selfantigens may receive signals that promote their death by apoptosis. This process has been called activation-induced cell death, because it is a consequence of T-cell activation.
Mechanisms of Autoimmunity : General Principles
Autoimmunity arises through some combination of susceptibility genes (causing loss of self tolerance) and environmental triggers (especially infections).
Role of Susceptibility Genes : potentially related to affects on negative selection or regulatory T-cell development
Role of Infections :
1.
This may occur secondary to co-stimulator up-regulation, which overwhelms peripheral tolerance mechanisms.
2.
Infection might also break tolerance by molecular mimicry; if a microbe shares epitopes with self antigens, immune responses directed against the pathogen could cross-react with and damage normal tissues.
2
Diseases of the Immune System
(autoimmune diseases) Lec.2
2014-
2015
3.
Tissue injury occurring in the course of response to infection can also structurally alter self antigens, or release normal self antigens; these molecules would then activate T cells that are not tolerant to the altered or previously cryptic antigens.
General Features of Autoimmune Diseases
Once induced, autoimmune diseases tend to be progressive, albeit with occasional relapses and remissions. This is, in part, due to intrinsic amplification loops that the immune system employs to allow initially small numbers of responsive cells to eventually overcome infection. In addition, immune responses are subject to the phenomenon of epitope spreading ; many possible epitopes within self antigens are not normally presented to developing T cells, and thus there is no opportunity to develop tolerance to such cryptic peptides. However, if such epitopes become recognizable in postnatal life as a result of molecular alteration of self antigens, T cells reactive to them can cause persistent autoimmunity. The phenomenon is called epitope spreading because the immune response “spreads” to determinants that were not initially recognized.
3
Diseases of the Immune System
(autoimmune diseases) Lec.2
2014-
2015
Systemic Lupus Erythematous is a Prototypical Systemic Immune Complex
Disease
SLE is a chronic, autoimmune, multisystem, inflammatory disease that may involve almost any organ but characteristically affects kidneys, joints, serous membranes, and skin.
The most important diagnostic disease-associated autoantibodies are those against nuclear antigens in particular, antibody to double-stranded DNA and to a soluble nuclear antigen complex that is part of the spliceosome, termed Sm (Smith) antigen. High titers of these two antinuclear antibodies (ANAs) are nearly pathognomonic of SLE.
Pathogenesis
The fundamental defect in SLE is a failure to maintain self-tolerance, leading to the production of a large number of autoantibodies that can damage tissues either directly or in the form of immune complex deposits. As in other autoimmune diseases, the pathogenesis of SLE involves a combination of genetic and environmental factors.
I.
Genetic Factors
1.
Familial association.
2.
HLA association.
3.
Other genes.
II.
Environmental Factors.
1.
Ultraviolet (UV) radiation (sun exposure) exacerbates the lesions of SLE. A postulated mechanism of this effect is that UV radiation causes apoptosis of host cells, leading to an increased burden of nuclear fragments and inflammatory responses to the products of dead cells.
2.
Cigarette smoking
3.
Sex hormones because SLE is 10 times more common in women during reproductive years than in men of similar ages
4.
Drugs such as procainamide and hydralazine can induce an SLE-like disease
4
Diseases of the Immune System
(autoimmune diseases) Lec.2
2014-
2015
Model for the pathogenesis of systemic lupus erythematosus: Genetic susceptibility and exposure result in failure of self-tolerance and persistence of nuclear antigens. Autoantibodies serve to internalize nuclear components, which engage TLRs and stimulate IFN production. IFN may stimulate B and T cell responses to the nuclear antigens.
IFN, interferon; IgG, immunoglobulin G; MHC, major histocompatibility complex; TLRs,
Toll-like receptors; UV, ultraviolet.
5
Diseases of the Immune System
(autoimmune diseases) Lec.2
2014-
2015
Clinical & laboratory Features: Typically, the patient is a young woman with some, but rarely all, of the following features:
1.
a butterfly rash over the face
2.
Fever
3.
pain and swelling in one or more peripheral joints (hands and wrists, knees, feet, ankles, elbows, shoulders)
4.
pleuritic chest pain,
5.
photosensitivity.
6.
In many patients, however, the presentation of SLE is subtle and puzzling, taking forms such as a febrile illness of unknown origin, abnormal urinary findings, or joint disease masked as RA or rheumatic fever.
7.
ANAs are found in virtually 100% of patients, but an important point is that
ANAs are not specific.
8.
A variety of clinical findings may point toward renal involvement, including hematuria, red cell casts, proteinuria, and in some cases the classic nephrotic syndrome
9.
in some patients anemia or thrombocytopenia may be the presenting manifestation
10.
Neuropsychiatric manifestations, including psychosis or convulsions
11.
coronary artery disease
12.
Patients with SLE are also prone to infections, presumably because of their underlying immune dysfunction and treatment with immunosuppressive drugs.
Prognosis
The clinical course of SLE is highly variable, typically with exacerbations and remissions.
The overall 10-year survival rate approaches 90%.
The worst prognosis is in patients with severe renal or CNS disease and those with systolic hypertension.
6