Common Running Injuries - Clinton Public School District
advertisement

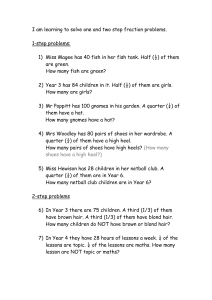
Common Running Injuries: What They Are and How to Prevent Them Kevin Sheehan, SPT Assistant Cross Country Coach Beavercreek High School 2013 Season Running is a great way to help you maintain a healthier lifestyle, however, with the amount of time and miles we put in it is common for running injuries to develop. In order to reduce the occurrence of these injuries and keep you healthy and running, I have put together some information about preventing injuries in general, preventing specific injuries, and some things you can do if you feel you are developing an injury. Although there are some stretches and exercises for many common injuries in this packet that you can do on your own, it is important to remember that there are many other kinds of injuries and these exercises will not always fix the problem. Please see your Coaches and Athletic Trainers if you feel you are injured or your symptoms are not improving. General Running Injury Prevention Problem: The strongest predictor of future injury is weekly mileage, specifically how fast you increase your mileage. Solution: Stick to the week by week plan that Coach Russ has given you. His programs are designed to increase your mileage appropriately based on your off season training, running experience, and your age. As the graph shows below, if you increase your volume and/or intensity of training by too much you will start to overtrain and will actually start to run slower in races. Problem: Running hard every day without easy days in between can increase risk of injury. Solution: Make sure to run with a group that is at your current level of running fitness. Run the hard days hard and the easy days easy. Running hard every day will not make you faster and will also increase your risk of injury. Problem: Certain running surfaces may increase risk of injury. Solution: Limit the amount of training you do on road and sidewalk. The bulk of your training should be run on grass, trails, or track. Try to avoid running on the side of a road because the camber of the road (shown below) can alter the way you run and cause injury such as shin splints. Problem: Worn out or inappropriate shoes can cause injury. Solution: Buy a good pair of shoes that are specifically made for running. If you need help picking out shoes ask your coaches, visit a running store (Runner’s Plus, Endurance Sports, Up and Running), or consult www.runnersworld.com. Keep track of how many miles are on your shoes. The cushioning in running shoes is typically good for 350-500 miles. If you are able, having two pairs of shoes you can rotate between can decrease the rate of breakdown of the cushioning in your shoes. Allowing your shoes 24-48 hours to “decompress” can help the cushioning recover after a run. Specific Running Injury Prevention Patellofemoral Pain Syndrome (PFPS) What is this? Caused by increased demand to the quadriceps muscle group and the patellar ligament, resulting in pain An achy feeling on the front of the knee, behind the kneecap (Figure 1) Usually cannot pinpoint one specific point of pain May be present throughout each run Typically aggravated by hills or stairs Swelling may be present Occasionally the knee may “give way” What can I do if I think I have this condition? Decrease total weekly distance Decrease hill work Mobilization to improve alignment of your knee cap (Figure 2) o See Coach Kevin or athletic trainer to confirm this Ice to the patellar ligament (directly below the bottom of your knee cap) o Freeze a small paper cup of water and rub 3-5 minutes to numb the area o Cross friction massage to that same area until numbing is gone (Ask Coach Kevin if you plan on doing this) How can I prevent this from happening? Strengthen your quadriceps so they can handle more demand o Lunges (Figure 3) o Wall slides: 2 legs first, 1 leg as you get stronger (Figure 4 and 5) o Body weight squats: 2 legs first, 1 leg as you get stronger (Figure 6) o Leg press Strengthen your gluteus medius muscle to improve alignment of your knee cap (Figure 7) Stretching o Calf stretch (Figure 8) o Hamstring stretch (Figure 9) o IT band stretch (Figure 10) Iliotibial Band Syndrome (ITBS) What is this? Pain on the outside of your knee due to friction of the IT band against the outside of your thigh bone (Figure 1) Pain usually comes on gradually Often described as a “burning pain” Pain typically onsets at the same time during the run Walking does not usually cause pain, but stairs may be painful Clicking and snapping may be heard and felt on the outside of the knee There may be points that are painful to touch all along the IT band that runs from the outside of your hip to the outside of your knee What can I do if I think I have this condition/want to prevent this condition? Ice the painful area o 10 minutes with a sheet or towel between the ice and your skin Mobilization to improve alignment of your knee cap (Figure 2) o See Coach Kevin or athletic trainer to confirm this Strengthen gluteus medius muscle (Figure 7) Stretching the hip muscles o IT band stretch (Figure 10) o Piriformis stretch (Figure 11) o Hip flexor stretch (Figure 12) Vary your direction when running on the track and limit time running on the track Tibial Stress Injuries (shin splints) What is this? A dull or achy pain that gradually occurs on the inside of the shin bone In the early stages of tibial stress injuries, the pain is present at the beginning of the run, disappears throughout the run, and returns several hours after the run In later stages the pain is present during the entire run and directly after the run Repetitive heel raises may cause pain as well How do I know if I have shin splints or a stress fracture in my shin? A stress fracture is characterized by pain that persists after running and during typical walking A stress fracture will have pain in one spot that you are able to pinpoint, while shin splints tend to be dull and achy over a larger area If you think you may have a stress fracture, see the Athletic Trainer What can I do if I think I have this condition/want to prevent this condition? Rest from running for a few days to try to reduce impact on the bone o You can still bike, elliptical, or water run (this form of cross training is the best simulation of actual running) to maintain your aerobic fitness Apply ice to the affected area for 10 minutes with a sheet or towel in between your skin and the ice Run on soft surfaces such as trails, grass, or track only Calf stretches (Figure 8) Strengthening of the muscles around your shin o Heel walks with toes in and toes out o Curl a towel up with your toes, then spread it back out again with your toes (Figure 13) Achilles Tendinitis What is this? Pain that occurs along your heel cord (Achilles tendon) near the back of your heel This area will generally feel stiff in the early morning and at the start of a run The area will loosen from beginning towards the middle of the run, but pain will increase gradually towards the end of the run In later stages, pain will be present throughout the run and even during normal walking There may be some swelling to the area The area may be tender to the touch What can I do if I think I have this condition/want to prevent this condition? Cross friction massage and ice to the Achilles tendon o See the above instructions under “Patellofemoral Pain Syndrome” o See Coach Kevin if you wish to do this Calf Stretches (Figure 8) Strength (for prevention or after pain has subsided) o Heel raises on a step with emphasis on slow and controlled lowering (Figure 14) Plantar Fascitis What is it? Pain may be felt on the heel and/or the inside of the arch of your foot Pain comes on gradually with training Pain typically described as “sharp” Pain is often the worst with the first few steps in the morning and at the beginning of a run (pain tends to decrease throughout the run) Pulling up on your toes, stretches the plantar fascia and may cause pain What can I do if I think I have this condition/want to prevent this condition? Cross friction massage and ice to the arch of your foot o See the above instructions under “Patellofemoral Pain Syndrome” o See Coach Kevin if you wish to do this Roll a can or ball under your arch with moderate pressure to massage the arch (Figure 15) Strengthen foot muscles o Toe curls with towel (Figure 13) Calf stretches: for prevention or after pain has subsided (Figure 8) Plantar fascia stretches: for prevention or after pain has subsided o Method 1: pull up on your toes while pushing your heel towards the outside of your foot (Figure 16) o Method 2: standing with the ball of the foot on a stair, lower your heel until you feel a stretch in the arch of your foot (Figure 17) Compartment Syndromes What is it? Increased pressure occurs in compartments in the lower leg, restricting blood flow in that compartment This causes aching or cramping leg pain, tightness, and sometimes weakness Pain typically occurs in the first 20 minutes of a run and stops after the run Compartment syndromes may be differentiated from shin splints or stress fractures because the pain is often felt on both legs, and numbness and tingling down the leg may also be present Locations of the compartments are shown in Figure 18 o Deep posterior compartment (pain on the inside of the lower leg) and anterior compartment syndrome (pain on the front and middle of the lower leg) are the most common in runners What can I do if I think I have this condition? Calf Stretches (Figure 8) Tibialis anterior stretch (Figure 19) If you suspect this problem, please see your Coaches or Athletic Trainers Stress Fractures What are they? The tibia (shin bone) is the most common stress fracture in runners, but bones in your feet (navicular, metatarsals, and sesmoids) and your fibula have also been known to develop stress fractures (Figure 20) Pain typically comes on gradually and is in one specific spot that you can pinpoint The painful spot is tender to the touch What do I do if I think I have this condition? Talk to your Coaches and Athletic Trainers as you may need to be referred to a physician to test for the fracture Exercises and Stretches Figure 1 Figure 4 Figure 2 Figure 5 Figure 3 Figure 6 Figure 7 Figure 8 Figure 9 Figure 10 Figure 11 Figure 13 Figure 15 Figure 12 Figure 14 Figure 16 Figure 17 Figure 18 Figure 19 Figure 20