Antibacterials: tetracyclins Mechanism enter bacteria via active
advertisement
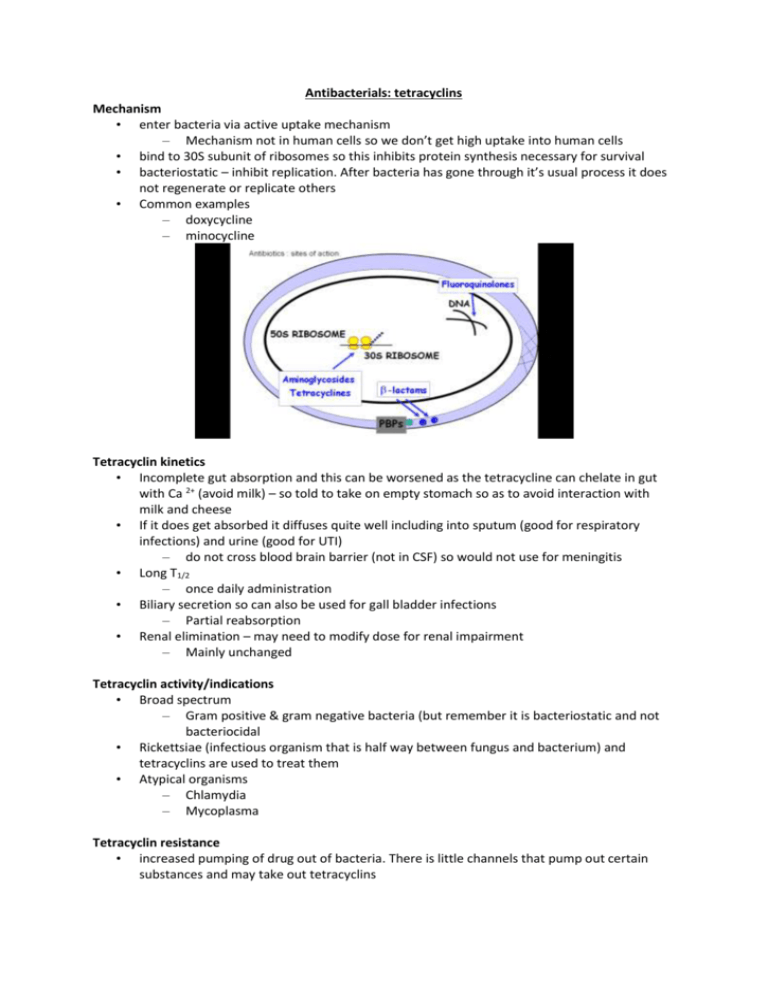
Antibacterials: tetracyclins Mechanism • enter bacteria via active uptake mechanism – Mechanism not in human cells so we don’t get high uptake into human cells • bind to 30S subunit of ribosomes so this inhibits protein synthesis necessary for survival • bacteriostatic – inhibit replication. After bacteria has gone through it’s usual process it does not regenerate or replicate others • Common examples – doxycycline – minocycline Tetracyclin kinetics • Incomplete gut absorption and this can be worsened as the tetracycline can chelate in gut with Ca 2+ (avoid milk) – so told to take on empty stomach so as to avoid interaction with milk and cheese • If it does get absorbed it diffuses quite well including into sputum (good for respiratory infections) and urine (good for UTI) – do not cross blood brain barrier (not in CSF) so would not use for meningitis • Long T1/2 – once daily administration • Biliary secretion so can also be used for gall bladder infections – Partial reabsorption • Renal elimination – may need to modify dose for renal impairment – Mainly unchanged Tetracyclin activity/indications • Broad spectrum – Gram positive & gram negative bacteria (but remember it is bacteriostatic and not bacteriocidal • Rickettsiae (infectious organism that is half way between fungus and bacterium) and tetracyclins are used to treat them • Atypical organisms – Chlamydia – Mycoplasma Tetracyclin resistance • increased pumping of drug out of bacteria. There is little channels that pump out certain substances and may take out tetracyclins – • • • • • transferred by plasmids (bits of nucleic acid that can be transferred between bacteria) decreased binding of drug to 30S ribosomes – any change of the structure of the ribosomes makes it harder for the drug to bind develops slowly (tetracyclins are about half a century old) so resistance is fairly widespread cross resistance between tetracyclines (if bacteria is resistant to one it will be resistant to the other) Porin pump is responsible for exclusion of drug from inside of the drug Resistance can be intrinsic (natural feature of the bacteria usually from changes in chromosomes) or acquired (by plasmid transmission) Tetracyclin side-effects • nausea, vomiting as with all antibiotics • that can progress to abdominal discomfort / diarrhoea • brown teeth (children – while teeth are developing) – chelation of Ca 2+ (calcium is in teeth and when the tetracylcins bind they are then taken up by teeth and stain teeth) – avoid in ages < 12 years (& pregnancy) • benign intracranial hypertension – meaning an increased pressure within the CSF but is called benign because it doesn’t cause serious symptoms more just small headaches Fluoroquinolones : mechanism • inhibit replication of bacterial DNA and therefore the bacteria cant multiply • does this by blocking activity of 2 enzymes: – DNA gyrase (involved in the folding of DNA) – DNA topoisomerase • these enzymes essential for – DNA replication & DNA repair • Bactericidal – they attack the DNA and inhibit replication • Examples – Ciprofloxacin, norfloxacin, moxifloxacin, gatifloxacin • • Gyrase involved in winding up the nucleic acid Topoisomerase works at the fork in the DNA Fluoroquinolones activity • broad spectrum • ciprofloxacin – Gram positive i.e. staphylococcus – Gram negative i.e. pseudomonas – people with cystic fibrosis get colonizations of pseudomonas • norfloxacin – Urinary tract infections as it is excreted quite high concentrations in the urine • moxifloxacin / gatifloxacin – pneumonia – moxifloxacin is also used for treatment resistant tuberculosis Resistance • relatively uncommon as it is a relatively young class of drug (been around for about 5-10 years. In about another 10 years there will be more resistant based on the usual trends for antibiotics ) • mechanisms of the resistance that has developed at the moment – – mutations of DNA gyrase – drug cant bind as well increased drug efflux – bacteria starts to pump the drug out before it gets to the gyrase Fluoroquinolone kinetics • oral formulations well absorbed • widely distributed in body tissues so achieves significant concentrations in different types of infections • mainly renal excretion. may need to modify dose in renal impairment • Range of T1/2 – moxifloxacin > norfloxacin > ciprofloxacin – moxifloxacin once daily Why kill bacteria fast? • Rapid reduction of bacterial load in the host which means there is less harmful products being released by the bacteria • Decrease in the toxicity • Decrease in immunologic “switch-on” (= allergy) i.e. if the bacteria is there for a long time it can initiate an immune response such as allergic response and next time the person gets the bacteria they can suffer a pretty significant reaction • Faster relief of signs and symptoms • Reduction of the potential for resistance development – bacteria there in a long time in the presence of the antibiotic could lead to the production of resistant bacteria • The streptococcus pneumonia are resistant to penicillin • • • • • • Vertical axis is colony forming units – means this experiment was done in vitro Control was done in saline solution and the colonies obviously replicated Levofloxacin is inhibiting the profileration of colonies Gatifloxacin works for around 10 hours Moxifloxacin continues inhibition in comparison to the control So this all shows the fluroquinolones are effective in treating penicillin resistant strept pneumonia Optimal Pharmacokinetic (PK) /pharmacodynamic (PD) parameters associated with : • high clinical and bacteriologic cure rates • low propensity for emergence of resistance Pharmacokinetic (PK) & pharmacodynamic (PD) parameters • AUC = Area under the curve • MIC90 = minimum concentration necessary to inhibit 90% of isolates • Cmax = Peak serum concentration • AUIC = Area under the inhibitory curve Optimal PK & PD parameters: to minimise emergence of resistance • AUIC = AUC/MIC90 ( Optimally >125) • Cmax/MIC90 (Optimally > 8-10) • The maximum concentration should be 8-10 times higher than the minimum inhibitory concentration for 90% of the isolates • • Vertical axis is the concentration (mg/L) Can see the Cmax is about 8 times higher • • • • • • Just read off the slide for the left side and said looks like everything meets the necessary criteria i.e. Cmax/MIC90 is between 8 and 10 AUIC is lower than what we want though Black circles is the concentration with oral doses But if we want a to get control of an infection we do IV He said we need to be aware of what MIC90 is and also the Cmax/MIC90 ratio as well as AUIC After 18 hours we would need to give another dose to stay above MIC90 but to be safe we would do q12h Side effects • nausea, vomiting, abdo pain, diarrhoea – as with all antibiotics • CNS effects – Caution with epilepsy • tendon rupture (esp in the ankle) – Mainly ciprofloxacin. Was noticed with cystic fibrosis patients • prolongation of QT interval (ECG) – moxifloxacin. If patient has history of arrhythmias we would do ECG before giving drug or if person was on another drug that increases QT we would look for another antibiotic – moxifloxacin is used in clinical trials as the ‘gold standard’ for QT prolongation. They use it as a control to see if the other drug increases QT proloongation • inhibition of P450s – drug interactions Aminoglycosides mechanism • inhibit protein synthesis – bind irreversibly to 30s ribosomal subunit – inhibits translation from messenger RNA (mRNA) to protein – the amino acids do not add on – increases the frequency of misreading of genetic code – dysfunctional proteins are created • bactericidal even though tetracyclins which work in the same area are bacteriostatic. They are more potent than tetracyclins • Examples – gentamicin, tobramicin, amikacin, netilmicin Activity • Gram negative bacteria – Including Pseudomonas species • also some gram positives • inactive against anaerobic organisms – unable to take up aminoglycosides so they don’t get into the bacteria • Used in combination with cell wall inhibitors – penicillins & aminoglycosides “synergistic”. This was noticed in vitro that together you get a better effect than just them on their own. Theory is that penicillin increases the access of the aminoglycosides to their sites of action Resistance • relatively common as they have been around for a while • mechanisms (transferred by plasmids) – enzymes acetylate, phosphorylate or adenylate aminoglycoside in periplasmic membrane. In the membrane of the bacteria these enzymes add things to the antibiotic and the drugs can no longer bind to the ribosomes – modified drug does not access ribosomes – also, changes in ribosomes may reduce drug binding • May be overcome by combining with drugs that disrupt bacterial wall (e.g. penicillins) as they can affect the enzymes in the periplasmic membrane • • So can have changes in the 30S ribosome or cell wall There may be new enzymes such acetylases which can hinder the drugs Kinetics • poor oral absorption (give IV) – they stay in the bowel so are good for bowel infection. Good for people who need bowel surgery to sterilize the bowel • widely distributed in body tissues – Not CSF so not for meningitis ; crosses placenta • rapid renal excretion (unchanged drug) so may need to decrease dose in renal impairment as drug has narrow therapeutic window • short T1/2 – but given once daily as they have a “post antibiotic effect” – this was discovered in animal models • • • • in these animal models there is a tissue infection after a bolus dose the concentration goes up and then down like usual but if you continue to sample the tissue after this the bacteria is still inhibited so antibiotic is cleared from plasma but still has an effect in the body Side effects • ototoxicity – prolonged high plasma [C] - accumulation in inner ear – increased risk with loop diuretics. Frusemide with aminoglycosides seems to double the risk of ototoxicity • renal damage – accumulation in proximal tubules and can interfere with kidney function. Need to monitor kidney function during dosing – reversible if detected early • neuromuscular blockage – inhibits acetyl choline release in neuromuscular junctions – seen if co-administered with other neuromuscular blockers (e.g. during anaesthesia) – so issue if someone is about to have general anesthetics as there is prolonged neuromsuclar blockade and the person will need to stay on a ventilator