diferencias por edad y sexo
advertisement
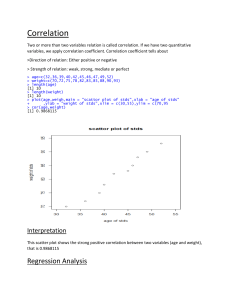
DIFERENCIAS POR EDAD Y SEXO El envejecimiento, a tenor de estos datos, no parece ser un factor clave en la falta de sueño. «Esto va en contra de la creencia popular», señala Michael Grandner, autor principal del estudio. «Los resultados nos sugieren que deberíamos volver a analizar lo que sabemos sobre el sueño de las personas mayores, tanto varones como mujeres». SABIDURÍA POPULAR EN ENTREDICHO La intención original del estudio era confirmar, en la muestra más numerosa y representativa analizada hasta ahora, que el aumento de los problemas del sueño está asociado con el envejecimiento. Sin embargo, los resultados no solo no han confirmado la opinión general, sino que parecen desafiar la sabiduría popular que sostiene que la dificultad para dormir se percibe más en los adultos mayores, además de ser una advertencia a la profesión médica que históricamente ha ignorado las quejas del sueño de los mayores y las han menospreciado al considerarlas como una parte normal del envejecimiento. El estudio examinó la incidencia de los de trastornos del sueño y fatiga durante el día de 155,877 adultos que participaron en una encuesta telefónica al azar. A los encuestados se les preguntó sobre si sufrían trastornos del sueño y cansancio durante el día. La encuesta también obtuvo datos acerca de la raza, ingresos, educación, estado de ánimo, la salud general y el tiempo desde la última revisión médica. Los datos menos sorprendentes mostraban que los problemas de salud y la depresión se asociaban con la falta de sueño, y que las mujeres tenían más trastornos del sueño y el cansancio que los varones. Sin embargo, a excepción de un repunte en los problemas del sueño durante la mediana edad - más pronunciada en las mujeres que los hombres - la calidad del sueño mejoraba consistentemente durante toda la vida. O al menos así dijeron las personas entrevistadas en la encuesta. SLEEP VOLUME 35, ISSUE 03 AGE AND SLEEP DISTURBANCE AMONG AMERICAN MEN AND WOMEN Age and Sleep Disturbances Among American Men And Women: Data From the U.S. Behavioral Risk Factor Surveillance System http://dx.doi.org/10.5665/sleep.1704 Michael A. Grandner, PhD1,2; Jennifer L. Martin, PhD, CBSM3,4; Nirav P. Patel, MD, MPH5; Nicholas J. Jackson, MPH1,2; Philip R. Gehrman, PhD, CBSM1,6; Grace Pien, MD, MSCE1,2,7; Michael L. Perlis, PhD1,6; Dawei Xie, PhD8; Daohang Sha, PhD8; Terri Weaver, PhD9; Nalaka S. Gooneratne, MD, MSc1,10 1Center for Sleep and Circadian Neurobiology, University of Pennsylvania, Philadelphia, PA; 2Division of Sleep Medicine, Department of Medicine, University of Pennsylvania, Philadelphia, PA; 3David Geffen School of Medicine, University of California, Los Angeles, CA; 4Geriatric Research, Education and Clinical Center, VA Greater Los Angeles Healthcare System, Los Angeles, CA; 5Respiratory Specialists and The Reading Hospital and Medical Center; 6Division of Pulmonary and Critical Care Medicine, Department of Medicine, University of Pennsylvania, Philadelphia, PA; 7Department of Psychiatry, University of Pennsylvania, Philadelphia, PA; 8Center for Clinical Epidemiology and Biostatistics, University of Pennsylvania, Philadelphia, PA; 9Biobehavioral and Health Science Department, University of Illinois at Chicago College of Nursing, Chicago, IL; 10Division of Geriatric Medicine, Department of Medicine, University of Pennsylvania, Philadelphia, PA Study Objective: Explore the prevalence of sleep-related complaints across age groups, examining effects of sex, general health, and depressed mood. Design: Cross-sectional analysis of data from the 2006 Behavioral Risk Factor Surveillance System (BRFSS). Setting: Epidemiologic. Participants: Complete-case analysis included 155,877 participants who responded to questions related to Self-Reported Sleep Disturbance (SLEEPDIST) and Self-Reported Tiredness/Lack of Energy (TIREDNESS). Interventions: None. Measurements and Results: Outcomes were self-reported complaints in response to survey questions assessing SLEEPDIST and TIREDNESS, dichotomized as reporting a complaint < 6 versus ≥ 6 nights or days, respectively, in a 2-wk period. Predictors were age, general health, and depressed mood. All analyses were adjusted for race/ethnicity, income, education, and time since last medical checkup. Across all age groups, women reported more SLEEPDIST and TIREDNESS. Poor general health, mild depressed mood, and moderate/severe depressed mood were associated with SLEEPDIST and TIREDNESS. Both SLEEPDIST and TIREDNESS generally declined across the life span, with fewest endorsements in respondents older than 80 yr. For SLEEPDIST, odds ratios (ORs, reference = 80+) declined from age 18-54 yr, rose slightly, and then declined again after age 59 yr in men. The pattern was similar for women, except a more marked rise was noted from age 40-59 yr. The pattern was similar for TIREDNESS. Conclusions: Advancing age was not associated with increased Self-Reported Sleep Disturbance or SelfReported Tiredness/Lack of Energy. These results suggest that the often-reported increase in sleep problems with age is a nonlinear phenomenon, mediated by factors other than physiologic aging. Citation: Grandner MA; Martin JL; Patel NP; Jackson NJ; Gehrman PR; Pien G; Perlis ML; Xie D; Sha D; Weaver T; Gooneratne NS. Age and sleep disturbances among American men and women: data from the U.S. behavioral risk factor surveillance system. SLEEP 2012;35(3):395-406.