Minerals I
advertisement
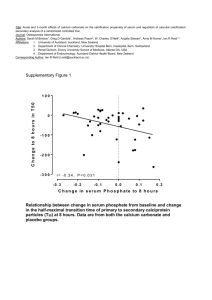
M INERALS I- Definition: Minerals are inorganic elements widely distributed in nature, & many of them have vital roles in metabolism. Minerals may be grouped according to their amount body. o Major Minerals: These are present in large amounts, in the body. Calcium, sodium, potassium, magnesium, phosphorus, sulfur and chlorine belong to this group. o Trace Minerals: These are present in small amounts & have a known function. This group includes iron, copper, iodine, manganese, cobalt, zinc & molybdenum. o Trace Minerals (function unknown): This group includes minerals whose function in the body is unknown, such as selenium, chromium, nickel & silicon. Factors that affect the requirements of minerals: 1- Species of animals: Some species of animals are more productive than others, and therefore you need large quantities of metal, for example, dairy cows and laying hens. 2- Age: Small animals need the metal more than large animals. 3- Poise food: If the proportion of food high in fat, less absorption of calcium significantly and therefore needs animals to a high proportion of this element. 4- Temperature: That high temperature leads to increased sweating and thus increases the salt with sweat and then increase requirement of metal. 5- Contrast between minerals: For example, the presence of high sodium concentrations in the diet hinders the absorption of calcium and magnesium. II- Major Minerals A- Calcium: Calcium is the most abundant mineral element in the body. It is an important constituent of the skeleton and teeth, in which about 99 per cent of the total body calcium is found; in addition, it is an essential constituent of living cell and tissue fluids o Of all the minerals in the body calcium is present in by far the largest amounts. o It comprises 1.5 - 2.0 % of the total body weight. 99 % of this mineral is in skeletal tissue (bones & teeth) as deposits of calcium salts. o The remaining 1% of body calcium performs highly important metabolic tasks & it occurs in the plasma & other body fluids. Three hormones involved in regulation o Vitamin D3 From kidney o Parathyroid hormone (PTH) From parathyroid gland o Calcitonin From thyroid gland PTH and Vitamin D3 act to increase plasma Ca, while calcitonin acts to decrease plasma Ca 1 1. Physiologic function of calcium: 1. Bone & teeth formation. The skeleton is not a stable unit in the chemical sense, since large amounts of the calcium and phosphorus in the bone can be liberated by reabsorption. This takes place particularly during lactation and egg production, although the exchange of calcium and phosphorus between bone and soft tissue is always a continuous process. reabsorption of calcium is controlled by the action of parathyroid gland. If animals are fed on a low calcium diet the ionic calcium concentration in the extracellular fluids falls, the parathyroid is stimulated and the hormone produced causes restoration of bone, liberating calcium to meet the requirement of the animal. 2. 3. 4. 5. 6. the parathyroid hormone also play important role in regulating the amount of the calcium absorbed from the intestine by influencing the production of 1,25dihydroxycholecalciferol, a derivative of vitamin D, which is concerned with the formation of calcium-binding protein, finally, the hormone stimulates the kidney to resorb urinary calcium. Blood clotting. Muscle contraction & relaxation: Ca plays an important role in the initiation of muscle contraction. This is particularly important in the contraction - relaxation cycle of the heart muscle. Nerve transmission: calcium is required for the normal transmission of nerve impulses. When an action potential reaches the nerve ends, calcium channels in the axon open, allowing calcium ions into the neuron. Those calcium ions trigger the fusion of the neurotransmitter vesicles with the membrane, and so the release of the neurotransmitter. Without calcium, you don't release the neurotransmitter, and so there is no way to get the impulse across the synapse. Cell wall permeability: ionized calcium controls the passage of fluid through cell walls by affecting cell wall permeability. Enzyme activation. 2. Clinical application: Tetany: A decrease in ionized serum calcium causes tetany, a state marked by severe, intermittent spastic contractions of the muscle & by muscular pain. It is manifested by a characteristic spasm of the muscles in the upper extremity, which causes flexion of wrist & thumb with extension of the fingers. Rickets: deficiencies in calcium, phosphorus &/or vitamin D are all related to rickets. When adequate calcium & phosphorus are not absorbed, proper bone formation cannot take place. Renal Calculi: The majority of renal stones are composed of calcium. Immobilization of the body through a cast or other orthopedic device causes an increase in the amount of calcium excreted in urine. Hyperparathyroidism &hypoparathyroidism: Because calcium & phosphorus metabolism are so directly controlled by parathyroid hormone, conditions of the parathyroid gland that increase or decrease the secretion of its hormone will immediately be reflected in abnormal metabolism of these 2 minerals. As such, dietary calcium intake should be adequate and should not exceed the usual daily allowances. 2 Deficiency symptoms: In young animals If calcium is deficient in the diet of young animals, then satisfactory bone formation cannot occur and the condition known as rickets is produced. The symptoms of rickets: 1- Misshapen bones. 2- Enlargement of joints. 3- Lameness. 4- Stiffness. In adult animals Calcium deficiency produces osteomalacia in which the calcium in the bone is withdrawn and not replaced, in osteomalacia the bone become weak and are easily broken. In hens Deficiency symptoms are soft beak and bones, retarded growth and bowed legs: the eggs have thin shells and egg production may be reduced. Milk fever: (parturient paresis) Is a condition which most commonly occurs in dairy cows shortly after calving, it is characterized by a lowering of the serum calcium levels, muscular spasms and, in extreme cases, paralysis and unconsciousness. The exact cause of hypocalcaemia associated with milk fever is obscure, but is generally considered that, with onset of lactation; the parathyroid gland is unable to respond rapidly enough to increase calcium absorption from the intestine to meet the extra demand. Source of calcium: milk, green leafy crops, especially legumes, and sugar beet pulp are good source of calcium. B. Phosphorus: o Phosphorus is closely associated with calcium & both occur in the same major food source - milk. o Both play major roles in bone building & are related to vitamin D in their absorption process. Both are regulated metabolically by parathyroid hormone, & exist in blood in definite ratio to another. o In addition it occurs in phosphoproteins, nucleic acids and phospholipids. o The element plays important role in energy metabolism in the formation of sugar-phosphates and adenosine di- and triphosphates. o The excess is excreted via the kidney or the gut (via saliva) . 3 1. Changes in serum phosphorus level: Situations of pathologic changes in serum P level include: Hypophosphatemia: Intestinal diseases as sprue & celiac disease in which P absorption is hindered or bone disease as rickets in which the Ca : P balance is upset, are characterized by low serum P levels. The serum phosphorus level is also low in primary Hyperparathyroidism, because the excess quantity of parathyroid hormone secreted results in excessive renal excretion of phosphorus. Symptoms of hypophosphatemia include muscle weakness, because the muscle cells are deprived of phosphorus essential for energy metabolism. Hyperphosphatemia: Renal insufficiency or hypoparathyroidism causes excess accumulation of serum phosphate. As a result, the calcium side of the Ca : P ratio is low, which causes Tetany. Deficiency symptoms: o Low dietary intake of phosphorus has also been associated with poor fertility, apparent dysfunction of ovaries causing inhibition, depression or irregularity of oestrus. o In cows, a deficiency of this element may also reduce milk yield. o In hens, there is a reduced egg yield, hatchability and shell thickness. 2. Food sources of phosphorus: Milk & milk products, cereal grains and fishmeal products containing bone are good sources of phosphorus. 4 C. Magnesium: o Magnesium is closely associated with ca and p o Magnesium, an essential nutrient, occurs in the body in considerable quantities. o There are ~ 25mg in an adult & 70 % of this is combined with Ca & P in the bone-salts complex. o The remaining 30% is distributed in various soft tissues & body fluids. o Mg is the commonest enzyme activator, for example in systems with thiamin pyrophosphate, and oxidative phosphorylation is reduced in mg deficiency, mg is essential activator of phosphate transferase (e.g.creatin kinase ) and its activate pyruvate carboxylase, pyruvate oxidase and reaction of the tricarboxylic acids cycle, therefore, it is essential for the efficient metabolism of carbohydrates and lipids o Ionized magnesium is essential to cellular metabolism of both carbohydrate & protein. Magnesium functions It is an essential dietary component for all farm animals. Magnesium is the commonest enzyme activator. Its metabolic function centers on reactions involving phosphorylation and energy transfer with ADP and ATP. Magnesium is also involved in the dampening of nerve impulses and muscle contraction and is antagonistic to calcium, which is stimulatory. Deficiency symptoms: o Experimental low magnesium milk diets for calves caused low serum mg levels, depleted bone mg, tetany and death. The condition is not uncommon in milk-fed calves about 50-70 days old. Colostrums is high in mg content but milk is low and this is compounded by a reduction in the efficiency of absorption of mg as the calf ages. o In adult ruminants: a condition known as hypomagnesaemic tetany associated with low blood level of mg (hypomagnesaemia). o Hypomagnesaemic tetany has been known under a variety of names, including magnesium tetany, lactation tetany and grass staggers, the condition can affect stall fed dairy cattle, hill cattle at grass as well as sheep. o hypomagnesemic tetany, also known winter tetany, is a metabolic disease involving magnesium deficiency, which can occur in such ruminant livestock as beef cattle, dairy cattle and sheep, usually after grazing on lush pastures of rapidly growing grass, especially in early spring. o Progressive symptoms may include grazing away from the herd, irritability, muscle twitching, staring, incoordination, staggering, collapse, thrashing, head thrown back, and coma. o The normal magnesium content of blood serum in cattle is within the range of 17 – 40 mg/ liter, but levels below 17 frequently occur without clinical symptoms of disease. o Urine magnesium is the better indicator of deficiency than serum mg because level of the latter do not fall until there is a sever deficiency. 5 Source of magnesium: Wheat bran, dried yeast and most vegetable protein concentration, especially cottonseed and linseed, are good sources of mg D. Sodium: o Sodium crucially important to many metabolic activities is one of the more plentiful minerals in the body. o Most of the sodium of the animal body is present in the soft tissues and body fluids. o About 1/3 of Na is present in the skeleton as inorganic bound material; the remaining 2/3 is in extra- cellular fluids. o Like potassium, sodium is concerned with the acid-base balance and osmotic regulation of the body fluids. o Sodium is the chief caution of blood plasma and other extracellular fluids of the body. o The sodium concentration within the cells is relatively low, the element being replaced largely by potassium and magnesium. o The body balance of Na is controlled through excretion by the kidneys and involves many factors, including the hormones aldosterone, angiotensin, rennin and antidiuretic hormone, as well as plasma Na concentration and renal blood flow. Sodium function Sodium is essential in the diet of animals and humans. It constitutes one of the main extracellular ions and helps to maintain water balance. However, the intracellular concentration of Na is quite low. Sodium also plays a role in the transmission of nerve impulses and in the absorption of sugars and amino acids from the digestive tract. Deficiency symptoms A deficiency of sodium in the diet leads to a lowering of the osmotic pressure, which results in dehydration of the body. Poor growth and reduced utilization of digested proteins and energy. In hens, egg production and growth are adversely affected. Rate given experimental diets low in sodium had eyes lesions and reproductive disturbance and eventually died. Sources of sodium 6 Most food of vegetable origin has comparatively low sodium contents; animal products, especially food of marine origin, are richer sources. commonest mineral supplement given to farm animals is common salt E. Potassium o Like sodium, potassium is a vital mineral element associated with physiologic fluid balance. o It is the major cation of the intracellular fluid. o However, the relatively small amount in extracellular fluid as a significant effect on muscle activity, especially heart muscle. o Small variations in the serum potassium concentration are reflected in electrocardiograph changes. 1. Clinical application: Hyperkalemia (elevated serum potassium): A rise in serum potassium results in weakening of heart action, mental confusion, poor respiration, & numbness of extremities. Hypokalemia (low serum potassium): Hypokalemia of dangerous degrees may be caused by a prolonged wasting disease with tissue destruction & malnutrition, or by prolonged GI loss of K as in diarrhea or vomiting. Additionally, the continuous use of certain diuretic drugs, as HCTZ increases K excretion. To prevent complications of cardiac failure, K should be given, especially when K depleting diuretics are used. 2. Food sources of potassium: o K is widely distributed in natural foods. Grains, leafy vegetables & meat supply considerable amounts. F. Chlorine o Chlorine occurs in the body as the chloride ion (CI). o It is the major anion in the extracellular fluid, & its highest concentration is in the CSF. o Together with ionized Na, ionized Cl in the extracellular fluid helps to maintain water balance & to regulate osmotic pressure. 1. Food sources of chlorine: o Almost the only dietary source of Cl is a partner to Na in table salt. 7 III- Trace Mineral with Known Function A. Iron Iron is distributed in the body in 4 main forms that point to its basic metabolic functions. o Transport iron: A very small amount of iron is found in the plasma. This iron is being transferred from one point of use to another by binding with a protein - transferrin. o Hemoglobin: About 75 % of the body’s iron is in hemoglobin, that is found in RBCs which is responsible for O2 transport to the cells for respiration & metabolism. o Storage Iron: Around 20 % of body iron is stored in the liver, spleen & marrow as the protein-iron compound ferritin. o Cellular Tissue Iron: About 5 % of total body iron is distributed throughout the cells as a major component of the enzyme system responsible for production of energy. 1. Iron deficiency: Anemia results from either a lack of iron or inability to use it by the body due to one of several causes: o Inadequate supply of iron in the diet - nutritional anemia. o Excessive blood iron loss - hemorrhagic anemia. o Inability to form hemoglobin in the absence of other necessary factors such as vitamin B12 o Lack of gastric HCl necessary to liberate iron for absorption. 2. Food sources of iron: o Organ meats, especially liver, are by far the best sources of iron. o Other food sources include meats, egg yolk, & seafood. B. Copper o Broadly speaking, copper seems to behave in the body as a companion to iron. o The two are metabolized in much the same way & share some functions. o Copper is additionally involved in two other areas of metabolism: Bone formation. Brain tissue formation and maintenance of the nervous system. Food sources of copper: o Cu is widely distributed in natural foods &, given a sufficient caloric intake, Cu will be amply supplied. C. Iodine o Iodine is a trace element associated mainly with the thyroid gland. o It participates in the synthesis of the thyroid hormone. o This is the only known function of iodine in human metabolism. o Deficiency of iodine will cause goiter characterized by great enlargement of thyroid gland plate. Food sources of iodine: o Commercial iodized table salt provides the main dietary source of iodine, o Seafood also provides a considerable amount of iodine. 8 D. Manganese o In nutrition, traces of manganese serve as essential activating agents that strengthen & stimulate a number of vital metabolic reactions. Food sources of manganese: o The best food sources of manganese are of plant origin: cereal bran, soybeans, legumes, nuts, tea & coffee. E. Zinc o Zinc occurs in the human body in amounts larger than those of other trace elements except iron. o It functions mainly as an essential constituent of several enzymes mainly a CO2 carrier in RBCs. o Zinc also combines readily with insulin in the pancreas. 1. Clinical application: o Hypogonadism & dwarfism from pronounced human zinc deficiency during growth periods has been recognized. o Wound healing is also related to zinc intake. According to recent studies, zinc-deficient wounds seem to be common in the average hospital, and patients benefit from zinc supplementation. 2. Food sources of zinc: Best food sources of zinc are seafood, meat and eggs. F. Molybdenum o Amounts of molybdenum in the body are very minute. o This trace mineral is present in bound form as an integral part of various enzyme molecules & facilitates the action of the specific enzyme involved. o In addition molybdenum is interrelated with copper metabolism. o It may also exert a beneficial effect upon the incidence & severity of dental caries & may enhance the well-established effect of fluoride. Food source of molybdenum: whole grains milk, leafy vegetables & organ meats. 9 IV. Trace Minerals with Unknown Functions A. Selenium o Within the last 15 years, selenium has been recognized to be an essential nutrient element in certain species, & its function as a component of several enzymes has been identified. o It was observed that selenium containing compounds protect the liver against fatty infiltration & necrosis. o This action of selenium may be related to that of Vitamin E, since the 2 substances appear to act together in curing the hepatic disease. Food Sources of Selenium: seafood, meat and whole grains. B. Chromium o The human body contains less than 6mg of chromium. o Chromium may affect lipid metabolism as well as carbohydrate metabolism; studies have shown that chromium can raise abnormally low fasting blood sugar levels & can improve faulty uptake of sugar by body tissues. o Physicians working in Jerusalem with refugee infants suffering from severe malnutrition & an inability to use sugar found that when small amounts of chromium were added to their diet, the infants made rapid recovery. o It has been speculated that chromium may have a possible link with chronic disease processes such as CV disorders & diabetes. Food sources of Chromium: Best food source is meat and whole grains. 10