Middle East Respiratory Syndrome Coronavirus (MERS-CoV)
advertisement
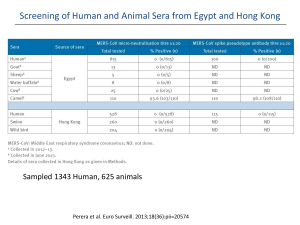
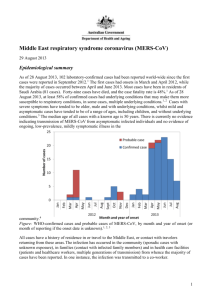
An Invited Paper Middle East Respiratory Syndrome Coronavirus MERS-CoV Image courtesy NIH/NIAID Joseph P. Dudley, Ph.D. Research Scientist, Institute of Arctic Biology – University of Alaska Fairbanks jpdudley@alaska.edu Summary The Middle East Respiratory Syndrome Coronavirus (MERS-CoV) is a novel coronavirus that is distantly related to the SARS virus. The first known human MERS-CoV cases occurred in Jordan during March-May 2012, although the virus itself was not detected and identified until September 2012. As of 1 May 2014, there have been more than 425 confirmed human MERS-CoV cases in 17 countries worldwide. Confirmed human MERS-CoV cases have been reported from the Middle East (Jordan, Kuwait, Oman, Qatar, Saudi Arabia, United Arab Emirates, Yemen), Europe (France, Germany, Greece, Italy, United Kingdom), Africa (Egypt, Tunisia), Asia (Malaysia, Philippines), and North America (United States). The typical clinical features of MERS-CoV disease are similar to those associated with the Severe Acute Respiratory Syndrome corornavirus (SARS): an acute lower respiratory disease syndrome (ARDS) with fever and dyspnea. Other common presenting symptoms include chills, rigor, headache, myalgia, malaise, and diarrhea. The documented case fatality rate for MERS-CoV (approximately 35%) is much higher than that recorded from SARS (11%). Unlike SARS, there are marked age and sex biases among MERS-CoV cases, with the highest rates of morbidity and mortality present in men over 50 years of age. The spread and proliferation of human MERS-CoV cases has been much slower than that of the SARS coronavirus, but much more rapid than that of the H5N1 avian influenza virus. Following the initial emergence of the SARS coronavirus in southern China during November 2002, more than 8,000 cases were documented in at least 26 countries worldwide by the time the 1 SARS epidemic ended in July 2003. It took more than a decade (from 1997 to 2008) the H5N1 avian influenza to achieve the same number of confirmed human cases and affected countries that were documented for MERS-CoV within two years following the first known outbreak (400+ human cases; 15+ countries). Introduction In September 2012, a novel coronavirus was isolated almost simultaneously from a patient with pneumonia in Saudi Arabia, and a patient from Qatar in the intensive care unit of a hospital in the United Kingdom. During the subsequent year, another 136 cases of MERS-CoV including 58 deaths were confirmed from patients hospitalized in 10 countries in Europe and the Middle East. The first known MERS-CoV outbreak was a retroactively identified cluster of 2 confirmed fatal cases and 11 probable nonfatal cases that occurred in Jordan during March-May 2012.1 This index outbreak in Jordan was especially notable because the cluster involved cases treated at three different hospitals, with apparent human-to-human transmission between and among the apparent index case, family members, and health care workers.2 A major resurgence of MERS-CoV cases during April 2014 brought the total number of reported confirmed MERS cases worldwide to more than 424 cases, including 131 deaths, and expanded the geographic distribution of confirmed MERS-CoV cases to include countries in Asia (Malaysia, Bangladesh) and North America (United States), and several additional countries the Middle East (Yemen, Egypt) and Europe (Greece). More MERS-CoV cases were reported during April 2014 (n=217), than were been reported during the two years following the beginning of the outbreak in March 2012 (n=207). Most of the new cases were confirmed from Saudi Arabia (n=179) and the United Arab Emirates (n=32). The underlying cause of the apparent rapid increase in new cases in the Arabian Peninsula during April 2014 was unknown at the time.3 All persons with confirmed MERS-CoV infections to date had been individuals who were either residents of Middle Eastern countries, persons with a recent history of travel to the Arabian Peninsula, or persons having close contact with individuals having a recent history of travel to the Middle East. To date, however, there is no evidence indicating any sustained transmission or community-level transmission of MERS-CoV.3 Epidemiology The typical clinical features of MERS-CoV disease are similar to those associated with the Severe Acute Respiratory Syndrome corornavirus (SARS): an acute lower respiratory disease syndrome (ARDS) with fever and dyspnea. Other common presenting symptoms include chills, rigor, headache, myalgia, malaise, and diarrhea. Unlike the related SARS coronavirus which emerged in China about a decade earlier, the MERS-CoV has been associated with a relatively high rate of deaths (case fatality rate >30%, as of April 2014) and pronounced age and sex biases among confirmed cases. The fatality rate among patients who develop severe respiratory disease symptoms typical ARDS symptomatic cases has been very high, about 60%, with the majority of fatal cases occurring in men >60 years old. Infections acquired through apparent human-to-human transmission are often associated with less severe disease symptoms. As of 30 April 2014, the median age of confirmed cases with known age is 50 years (range 1 - 94 years), with 94% of cases recorded among adults >19 years of age. The male-to-female ratio among confirmed cases is 2 : 1, with highest rates of morbidity and mortality occurring among men ≥ 50 years old. As of March 2014, the median age of primary MERS-CoV cases (i.e., those cases with no known exposure to other infected persons, presumably caused by zoonotic infection or environmental exposure) was 58 years, and 80% of these primary cases were males.6 2 Four distinct epidemiological patterns associated with human MERS-CoV cases have been identified: imported cases: isolated cases in persons with recent history of travel to the Middle East; isolated cases: isolated sporadic cases within communities (presumably from zoonotic infection); family clusters: clusters of infections within families; nosocomial outbreaks: clusters of infections within and among hospitals or health care facilities. Extensive outbreak clusters involving human-to-human transmission from patients to health care workers, family members, and other patients have been reported from hospitals in Europe and the Middle East. 4,5 The frequency of confirmed cases among healthcare workers has been increasing. Although healthcare workers comprised only 16% of all reported cases prior to April 2014 (N = 33 of 207), healthcare workers comprised nearly 30% of all reported cases during April 2014 (62 of 217).3 There is evidence that there may be multiple routes for human-to-human transmission of the MERS-CoV.6 There has been a recent trend towards a lower median age and case fatality rate caused by the increased detections of mild cases or asymptomatic infections among health care workers, children, and young adults. Among the relatively few MERSCoV cases documented from children and adolescents, the majority have been mild or asymptomatic infections. To date there has been no evidence indicating transmission of MERS-CoV from asymptomatic individuals, or ongoing community transmission of low-prevalence mildly symptomatic illness.7 Genomic Analyses and Phylogenetics The genetic diversity of available sequences in public bioinformatics databases indicates multiple introductions from a presumed zoonotic source, with subsequent human-to-human transmission. Genetic sequence analyses have estimated that the MERS-CoV probably first emerged into human populations sometime between 2007 and 2012. Two studies have identified the period during June-July 2011 as a probable date for the first emergence of MER-CoV into human populations.8,9 There is currently limited information available about the molecular evolution of MERS-CoV, with regard to how and when the virus acquired the ability for infecting humans, and the capability for human-to-human transmission.10 Complete genomic sequences of MERS-CoV identical to sequences of viruses recovered from human MERS-CoV victims have been identified from dromedary camels in Saudi Arabia, and a short sequence fragment consistent with MERS-CoV was reported in a bat collected in close proximity to the home and workplace of the 2012 index case patient in Saudi Arabia from whom the initial virus isolate was obtained.11,12 A preliminary report on sequence analyses of three MERS-CoV samples recovered from cases in Saudi Arabia during April 2014 indicated that the genome sequences of all 3 viruses were not identical, but exhibited a high degree of similarity to each other and a large number of other known MERS-CoV sequences. The receptor-binding domain in the spike protein thought to influence the transmission capability of the MERS-CoV from the new samples was 100 percent identical to the binding site in a large number of known MERS-CoV genome sequences. This study identified no evident insertions or deletions suggestive of any recent major genetic shift in the MERS-CoV genome.13 Zoonotic Reservoir Host Several lines of evidence support the hypothesis that the MERS coronavirus has emerged from a mammalian reservoir host species.10 MERS-CoV genetic sequences have been isolated from two species of mammals sampled in close proximity with human MERS-CoV cases: dromedary camels in contact with confirmed human cases in Qatar and Saudi Arabia, and an Egyptian tomb bat in Saudi Arabia. 3 The available evidence as of April 2014 indicates that the dromedary camel is the most likely animal reservoir for MERS-CoV, and the proximate source for zoonotic human infections with the virus. MERS-CoV specimens have been isolated from camels in contact with human MERS-CoV patients in Qatar and Saudi Arabia, and genetically identical MERS-CoV specimens recovered from infected camels and humans.11,12,17 A significant number of reported confirmed MERS-CoV cases are known to have had recent contact with camels, or had consumed camel milk. 14,15,16 Dromedary Camel (Camelus dromedarius) http://en.wikipedia.org/wiki/File:Camelcalf-feeding.jpg Humans may be able to be infected through drinking unpasteurized camel milk, as experimental studies have demonstrated that the MERS-CoV can survive for prolonged periods in fresh camel milk at ambient temperatures of between 4 0C and 220C.17 The detection of MERS-CoV in nasal swab specimens from camels indicates the potential for respiratory transmission of the MERS-CoV from camels to humans or other animals. Other possible potential mechanisms for MERS-CoV transmission include exposure to urine or feces from infected camels.18,19 MERS-CoV or a genetically similar precursor virus may have been circulating among camel populations in the Arabian Peninsula and northern Africa for decades. Serological investigations have identified antibodies to the MERS-CoV virus in dromedary camels from numerous countries in the Middle East and northern Africa region, including Saudi Arabia, Jordan, Oman, Egypt, Sudan, Ethiopia, and the Canary Islands. Antibodies to a MERS-CoV–like virus have been detected in serum specimens collected from camels in Saudi Arabia during 1992.10 Although camels are often herded or housed with other livestock species (including goats, sheep, cattle, horses), survey investigations have not isolated the MERS-CoV from any other domesticated animal species. 20,21 4 Camels, sheep and goats at livestock market in northern Africa. http://commons.wikimedia.org/wiki/File:MarcheTamanrasset5.jpg References 1. World Health Organization. 4 October 2013. Middle East respiratory syndrome coronavirus (MERS-CoV) – update. Accessed 30 April 2014 at http://www.who.int/csr/don/2013_10_04/en/ 2. Hijawi B, Abdallat M, Sayaydeh A, Alqasrawi S, Haddadin A, et al. 2013. Novel coronavirus infections in Jordan, April 2012: epidemiological findings from a retrospective investigation. Eastern Mediterranean Health Journal 19(Suppl 1):S120-S18. Accessed 30 April 2014 at http://applications.emro.who.int/emhj/v19/Supp1/EMHJ_2013_19_Supp1_S12_S18.pdf 3. European Centre for Disease Prevention and Control. 2014. Epidemiological update: Middle East respiratory syndrome coronavirus (MERS-CoV). Accessed 30 April 2014 at http://www.ecdc.europa.eu/en/press/news/_layouts/forms/News_DispForm.aspx?List=8db7286c-fe2d-476c-913318ff4cb1b568&ID=994 4. Memish ZA, Zumla AI, Assiri A. 2013. Middle East Respiratory Syndrome Coronavirus infections in Health Care Workers. New England Journal of Medicine 369:884-886. Accessed 30 April 2014 at http://www.nejm.org/doi/full/10.1056/NEJMc1308698 5. Public Health Agency of Canada. 30 April 2014. Summary of Assessment of Public Health Risk to Canada Associated with Middle East Respiratory Syndrome Coronavirus (MERS-CoV). Accessed 30 April 2014 at http://www.phac-aspc.gc.ca/eri-ire/coronavirus/risk_assessmentevaluation_risque-eng.php 6. World Health Organization. 2014. Middle East respiratory syndrome coronavirus (MERS-CoV) summary and literature update – as of 27 March 2014. Accessed 30 April 2014 at http://www.who.int/csr/disease/coronavirus_infections/MERS_CoV_Update_27_March_2014.pdf?ua=1 7. Cauchemez S, Fraser C, Van Kerkhove MD, Donnelly CA, Riley S, et al. Middle East respiratory syndrome coronavirus: Quantification of the extent of the epidemic, surveillance biases and transmissibility. Lancet Infectious Diseases 14(1): 50–56. Accessed 30 April 2014 at http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3895322/ 8. Cotten M, Watson SJ, Kellam P, Al-Rabeeah AA, Makhdoom HQ, et al. 2013. Transmission and evolution of the Middle East respiratory syndrome coronavirus in Saudi Arabia: a descriptive genomic study. Lancet 382(9909):1993-2002. Accessed 30 April 2014 at http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3898949/ 9. WHO MERS-CoV Research Group. 2013. State of Knowledge and Data Gaps of Middle East Respiratory Syndrome Coronavirus (MERSCoV) in Humans. PLOS Currents Outbreaks 2013 Nov 12. Edition 1. Accessed 30 April 2014 at http://currents.plos.org/outbreaks/article/state-ofknowledge-and-data-gaps-of-middle-east-respiratory-syndrome-coronavirus-mers-cov-in-humans-2/ 10. Alagaili AN, Briese T, Mishra N, Kapoor V, Sameroff SC, et al. 2014. Middle East respiratory syndrome coronavirus infection in dromedary camels in Saudi Arabia. mBio 5(2):e00884-14. Accessed 30 April 2014 at http://mbio.asm.org/content/5/2/e00884-14 11. Memish ZA, Mishra N, Olival KJ et al. 2013. Middle East Respiratory Syndrome Coronavirus in Bats, Saudi Arabia. Emerging Infectious Diseases 19: 1819-23. Accessed 30 April 2014 at http://wwwnc.cdc.gov/eid/article/19/11/13-1172_article.htm 12. Qatar Supreme Council of Health. Based on recent Scientific Research: Three camels hit by MERS Coronavirus in Qatar, 27 Nov 2013. Accessed 30 April 2014 at http://www.sch.gov.qa/sch/En/catcontent.jsp?scatId=833&scatType=1&CSRT=95265856086085056421 13. Drosten C. 2014. MERS-COV - EASTERN MEDITERRANEAN (42): SAUDI ARABIA, GENOME SEQUENCING, JEDDAH OUTBREAK. ProMEDMail 20140426.2432140. Accessed 30 April 2014 at http://www.promedmail.org/direct.php?id=20140426.2432140 14. Memish ZA, Cotten M, Watson SJ, Kellam P, Zumla A, et al. 2014. Community case clusters of Middle East Respiratory Syndrome 5 Coronavirus in Hafr Al-Batin, Kingdom of Saudi Arabia: A descriptive genomic study. International Journal of Infectious Diseases. 2014 Mar 31 [Epub ahead of print] Accessed 30 April 2014 at http://www.sciencedirect.com/science/article/pii/S1201971214014519 15. World Health Organization. 2014. Middle East respiratory syndrome coronavirus (MERS-CoV) – update. Accessed 24 April 2014 at http://www.who.int/csr/don/2014_04_17_mers/en/ 16. World Health Organization. 2014. Middle East respiratory syndrome coronavirus (MERS-CoV) – update. Accessed 24 April 2014 at http://www.who.int/csr/don/2014_04_24_mers/en/ 17. van Doremalen N, Bushmaker T, Karesh WB, Munster VJ. 2014. Stability of Middle East respiratory syndrome coronavirus in milk. Emerging Infectious Diseases [epublished ahead of print]. Accessed 24 April 2014 at http://wwwnc.cdc.gov/eid/article/20/7/14-0500_article.htm 18. Hemida MG, Chu DKW, Poon LLM, Perera RAPM, Alhammadi MA, et al. 2014. MERS coronavirus in dromedary camel herd, Saudi Arabia. Emerging Infectious Diseases [epublished ahead of print]. Accessed 24 April 2014 at http://wwwnc.cdc.gov/eid/article/20/7/14-0571_article.htm 19. Memish ZA, Cotton M, Meyer B, Watson SJ, Alsahafi AJ, et al. 2014. Human infection with MERS coronavirus after exposure to infected camels, Saudi Arabia, 2013. Emerging Infectious Diseases [epublished ahead of print]. Accessed 24 April 2014 at http://wwwnc.cdc.gov/eid/article/20/6/14-0402_article.htm 20. Hemida MG, Perera RA, Wang P, Alhammadi MA, Siu LY, et al. 2013. Middle East respiratory syndrome (MERS) coronavirus seroprevalence in domestic livestock in Saudi Arabia, 2010 to 2013. EuroSurveillance 18: 20659 http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=20659 21. Reusken CB, Ababneh M, Raj VS, Meyer B, Eljarah A, et al. 2013. Middle East Respiratory Syndrome coronavirus (MERS- CoV) serology in major livestock species in an affected region in Jordan, June to September 2013. EuroSurveillance 18(50): 20662. Accessed 30 April 2014 at http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=20662 22. Briese T, Mishra N, Jain K, Zalmout IS, Jabado OJ, et al. 2014. Middle East respiratory syndrome coronavirus quasispecies that include homologues of human isolates revealed through whole-genome analysis and virus cultured from dromedary camels in Saudi Arabia. mBio 5(3): e01146-14. Accessed 30 April 2014 at http://mbio.asm.org/content/5/3/e01146-14.full.pdf 6