Standardisation of laparoscopic total mesorectal excision for rectal
advertisement
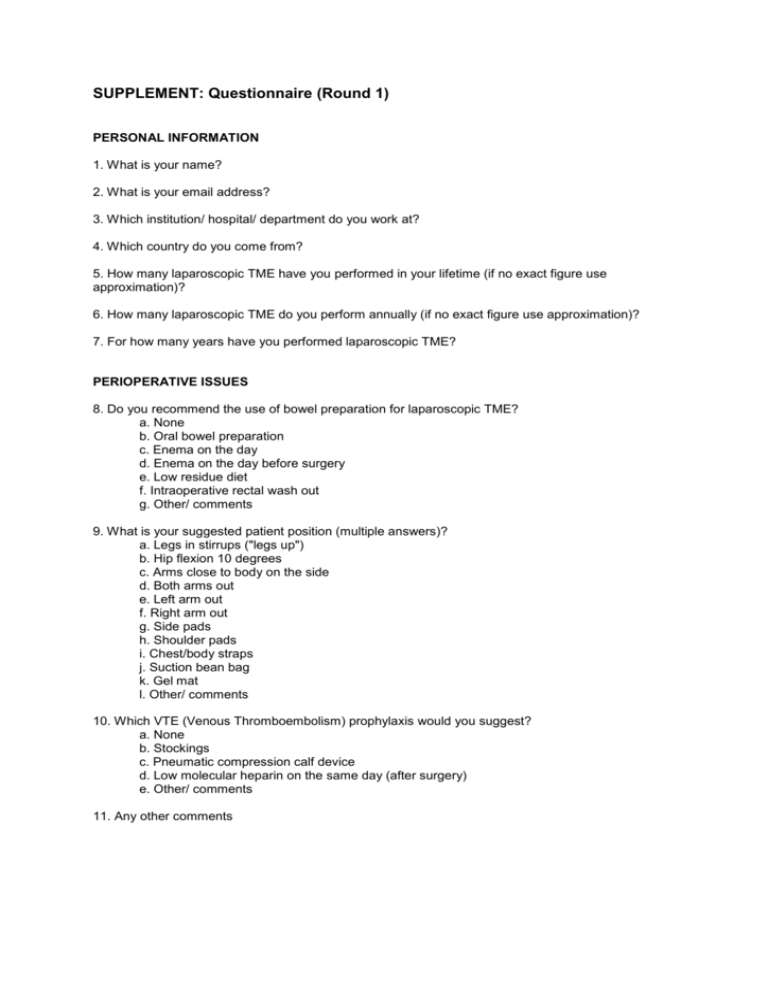
SUPPLEMENT: Questionnaire (Round 1) PERSONAL INFORMATION 1. What is your name? 2. What is your email address? 3. Which institution/ hospital/ department do you work at? 4. Which country do you come from? 5. How many laparoscopic TME have you performed in your lifetime (if no exact figure use approximation)? 6. How many laparoscopic TME do you perform annually (if no exact figure use approximation)? 7. For how many years have you performed laparoscopic TME? PERIOPERATIVE ISSUES 8. Do you recommend the use of bowel preparation for laparoscopic TME? a. None b. Oral bowel preparation c. Enema on the day d. Enema on the day before surgery e. Low residue diet f. Intraoperative rectal wash out g. Other/ comments 9. What is your suggested patient position (multiple answers)? a. Legs in stirrups ("legs up") b. Hip flexion 10 degrees c. Arms close to body on the side d. Both arms out e. Left arm out f. Right arm out g. Side pads h. Shoulder pads i. Chest/body straps j. Suction bean bag k. Gel mat l. Other/ comments 10. Which VTE (Venous Thromboembolism) prophylaxis would you suggest? a. None b. Stockings c. Pneumatic compression calf device d. Low molecular heparin on the same day (after surgery) e. Other/ comments 11. Any other comments PNEUMOPERITONEUM AND PORT POSITIONING 12. How should the pneumoperitoneum be established? a. Open cutdown (Hassan or similar) b. Veress needle c. Optical port d. Other (please specify) 13. What pneumoperitoneum pressure would you recommend? [mmHg] 14. What are your recommended port positions/size? [Port 1, Size], [Port 2, Size], etc… Please use this space to describe the location of any ports that aren't covered in the above options 15. Any other comments COLONIC MOBILIZATION 16. What is your suggested order of tasks (please rank the following from 1-6)? - TME dissection - IMA division - Splenic flexure mobilization - Left hemicolon medial mobilization - Left hemicolon lateral mobilization - IMV division 17. Are there any task groups that are missing in the previous question that you would like to add? 18. Which of the following would you recommend to obtain best possible exposure to start the procedure (multiple answers)? - Move omentum to over top of transverse colon - Move small bowel out of pelvis - Systematically/actively move small bowel loops into Right Upper Quadrant - Head down (Trendelenburg) position - Right tilt position 2030 degrees - Swab for retraction - Assistant for retraction - Other (please specify) 19. For access to the IMA (inferior mesenteric artery): what methods of retraction would you recommend (multiple answers)? a. Assistant grasps colon at rectosigmoid junction b. Assistant grasps mesocolon near rectosigmoid junction c. For long sigmoid colons: additional port for retraction d. Surgeon's left hand lifts rectosigmoid colon e. Surgeon's left hand pushes onto base of mesentery ("countertraction") while assistant is lifting colon f. Other (please specify) 20. Which of the following landmarks are important to identify the correct level of incision around the IMA pedicle? [Rate each with the following scale: Not at all important, Not important, Probably not important, Not sure, Probably important, Important, Very important, N/A] a. Sacral promontory b. Aortic bifurcation c. Right common iliac artery d. Left common iliac artery e. Right ureter f. White line of Toldt lateral to left colon (for lateral to medial approach) g. Air entering the mesocolic plane behind the IMA after initial incision 21. What instrument would you recommend for the incision of the peritoneum around IMA/IMV mobilization? a. Monopolar diathermy (hook, spatula, scissors) b. Ultrasonic scalpel c. Bipolar diathermy sealing instrument d. Sharp dissection without thermic energy (scissors) 22. What are the best instruments/methods for performing medial to lateral mobilization (or commbination of them)? a. Sharp dissection using ultrasonic scalpel b. Sharp dissection using bipolar sealing device c. Sharp dissection using diathermy (hook, spatula, scissors) d. Blunt dissection using grasper or inactive harmonic scalpel or similar device e. Blunt dissection using swab/ gauze f. Comments 23. The following structures are important to be visualized before dividing IMA: [Rate each with the following scale: Not at all important, Not important, Probably not important, Not sure, Probably important, Important, Very important, N/A] a. Surface of IMA/ superior rectal artery b. Bifurcation of left ascending colic artery c. IMV d. Left ureter e. Gerota's fascia f. Toldt's fascia g. Left gonadal vessels h. Other/ comments 24. The best method for the division of the IMA is... a. Clips b. Stapling device c. Ultrasonic sealing device d. Bipolar sealing device e. Other (please specify) 25. The level of division of the IMA should be at: a. flush to aorta b. 1cm from aorta c. Just proximal of ascending Lt colic artery d. Just distal of ascending Lt colic artery e. At the pelvic brim f. Other (please specify) 26. How important are the following structures to be visualized before dividing the IMV? [Rate each with the following scale: Not at all important, Not important, Probably not important, Not sure, Probably important, Important, Very important, N/A] a. Left ureter b. Left Gonadal vessels c. Surface of Gerota’s fascia d. Surface of Toldt fascia e. Origin of left ascending colic vein f. Duodenum g. Pancreas h. Other (please specify) 27. What level would you recommend dividing the IMV? At the lower border of the pancreas a. Near the Duodeno-Jejunal transition b. Proximal to the left ascending colic vein c. Distal (at the level of the IMA division) d. Other (please specify) 28. Should the splenic flexure be mobilized? a. Always for TME b. Selectively when length of colon unlikely to reach pelvis c. Never d. Other (please specify) 29. What is the preferred technique for the splenic flexure mobilization (multiple answers)? a. Lesser sac should be entered from below during medial to lateral mobilization b. Lateral mobilization c. Transection of gastrocolic ligament and enter lesser sac d. Divide omentum from transverse colon and enter lesser sac e. Lateral mobilization with patient in a left lateral position (repositioning of patient required) TOTAL MESORECTAL EXCISION (TME) 30. What is the preferred order of the following TME tasks? (Please rank from 1-8) - Posterior plane - Transection of rectum - Low posterior plane - Low anterior plane - Anastomosis - Anterior plane - Right lateral plane - Left lateral plane 31. Any additions/ comments to the previous question? 32. What are the best methods of ASSISTANT retraction for the dissection of the posterior plane (multiple answers)? a. Grasping the bowel near the rectosigmoid junction b. Grasping the IMA pedicle c. Grasping an appendix epiploica d. Grasping the sigmoid mesentery e. Use 2 hands (2 assistant ports) to grasp the tissues described above f. Other (please specify) 33. To obtain optimal exposure for the dissection of the posterior plane, the surgeon's left hand should (multiple answers): a. Push up on the mesorectal package using a closed instrument (blunt retraction) b. Push up on the mesorectal package using an opened instrument (blunt retraction) c. Grasp the bowel / mesorectum with an instrument to retract it d. Apply blunt traction on the parietal tissues e. Use a swab to facilitate blunt retraction f. Other (please specify) 34. What is the best instrument for dissection during this part of the procedure? a. Monopolar diathermy (hook, spatula, scissors) b. Ultrasonic scalpel c. Bipolar diathermy sealing instrument d. Sharp dissection (scissors without energy source) e. Blunt dissection f. Other (please specify) 35. Please indicate how important you consider the need to define and visualize each of the following landmarks upon entering the posterior TME plane: [Rate each with the following scale: Not at all important, Not important, Probably not important, Not sure, Probably important, Important, Very important, N/A] a. Shiny surface of mesorectal fascia b. Shiny surface of parietal presacral fascia c. “Angel hair” or loose areolar tissue d. Superior hypogastric nerves e. Other (please specify) 36. What is the best description for the dissection line in the posterior plane? a. In the middle of the loose areolar tissue b. Just at the mesorectal shiny surface (anterior aspect of the loose areolar tissue) c. In the avascular plane d. Other (please specify) 37. Which of the following statements do you agree with most? [Rate each with the following scale: Totally disagree, Disagree, Slightly disagree, Not sure, Slightly agree, Agree, Totally agree, N/A] a. “I go down posteriorly as much as I can, before opening the right lateral peritoneum to gain further access then proceed” b. “I open the right side very early to extend my dissection posteriorly and on the right lateral aspect together” c. “I go down posteriorly as much as I can before opening the left lateral peritoneum to gain further access then proceed” d. “I open the left side very early to extend my dissection posteriorly and on the right lateral aspect together” e. “I go down posteriorly as much as I can before simultaneously opening both the right and left side peritoneum to gain further access and proceed including both sides” f. “I open both the right and left side peritoneum early to facilitate my dissection and proceed widely in a circumferential manner” 38. At which point should the initial posterior plane dissection be stopped and the anterior plane opened? a. “when the rectum starts to angulate anteriorly” b. “when I am on the levator muscle” c. “when I am unable to progress further” d. “when I have to dissect the peritoneum to progress any further” e. “when I reach the level of the reflection” f. Other (please specify) 39. Where would you recommend opening the peritoneum of the anterior plane? a. At the bottom (apex) of the peritoneal reflection in all patients b. 1-2cm proximal to the reflection (towards the bladder) in all patients c. Anterior to the reflection in men, but at the reflection in women d. Other (please specify) 40. For optimal anterior retraction the ASSISTANT should: a. Retract anterior structures (bladder/prostate/uterus) with a closed/open instrument (blunt) b. Retract anterior structures using a swab held by an instrument c. Retract anterior structures by grasping the tissues with an instrument d. Other (please specify) 41. For anterior retraction the surgeon's left hand should: a. grasp the free anterior peritoneal edge to retract the mesorectum b. grasp the rectum c. use blunt soft pushing onto the rectum d. retract the anterior structures e.g. prostate/vagina/bladder 42. A transabdominal suture should be used to improve the retraction of anterior structures (bladder, uterus): a. Never b. In all patients c. In female patients d. In female patients with a large uterus e. Selectively in some females, but not in males f. Selectively in some females and some males g. Selectively if assistant retraction is insufficient h. Other (please specify) 43. Please indicate how important you would consider visualizing and defining each of the following landmarks to be in anterior dissection: [Rate each with the following scale: Not at all important, Not important, Probably not important, Not sure, Probably important, Important, Very important, N/A] a. Loose areolar tissue (“angel’s hair”) b. Bowel wall if tumour not anterior c. Seminal vesicles (male patients) d. Prostate (male patients) e. Denonvilliers fascia in all male patients f. Denonvilliers fascia – only if tumour is placed anteriorly g. Posterior vaginal wall (female patients) 44. The anterior plane of dissection should be: a. In front of Denonvilliers fascia in all patients b. Behind Denonvilliers fascia in all patients c. Only in front of Denonvilliers fascia when the tumour is anterior, otherwise behind Denonvilliers fascia d. Other (please specify) 45. Low mesorectal dissection: With regards the lateral attachments of the mesorectum, please indicate which of the following statements you agree with: [Rate each with the following scale: Totally disagree, Disagree, Slightly disagree, Not sure, Slightly agree, Agree, Totally agree, N/A] a. “Before I divide the lateral stalks I define both the anterior and posterior dissection planes” b. “I define the posterior dissection plane then progress to divide the lateral stalks before defining the anterior plane” c. “Once I see the lateral attachments I try to dissect as close to the specimen as I can to avoid injuring the nerves” d. “I divide the lateral attachments a little away from the specimen to ensure that I do not breach the mesorectum” e. Other (please specify) 46. Please indicate how important you would consider each of the following landmarks to be in defining the point of completion of a laparoscopic TME: [Rate each with the following scale: Not at all important, Not important, Probably not important, Not sure, Probably important, Important, Very important, N/A] a. Visualization of the intersphincteric plane b. Visualization of the top of the external sphincter c. The mesorectum has tapered onto the muscle wall d. Division of the posterior raphe e. Visualization of the rectal tube circumferentially f. Division of Denonvilliers g. Fusion of Denonvilliers with the prostate h. Being below the seminal vesicles at the level of the prostate 47. Completion: please indicate the degree to which you agree with the following statements: [Rate each with the following scale: Totally disagree, Disagree, Slightly disagree, Not sure, Slightly agree, Agree, Totally agree, N/A] a. “Before transecting the rectum, a digital rectal examination is required to determine the height of the tumour” b. “Before transecting the rectum a digital rectal examination is required to determine the position of the stapling device” c. “Before transection, the rectal lumen should be washed out” d. Other (please specify) 48. What type of stapler for the division of the rectum should be used (multiple answers)? a. Always 30mm b. Always 45mm c. Always 60mm d. Either 45 or 60mm, depending upon the specific patient e. Always articulating f. Always straight g. Straight/ articulating selectively h. Other (please specify) 49. Where should the stapler be inserted from? a. Right iliac fossa port b. Suprapubic port c. Left ilial fossa port d. Other (please specify) 50. How many stapler firings should be aimed for? a. Always just one b. Always two c. One or two depending upon anatomy d. Other (please specify) 51. Do you support any manoeuvres to facilitate the transection of the rectum? a. Pushing from the perineum by assistant b. Using transverse stapler through Pfannenstiel incision c. Other (please specify) 52. What is the preferred site for extraction? a. Pfannenstiel b. Left iliac fossa incision c. Right iliac fossa incision d. transverse umbilical e. vertical umbilical f. transverse left midzone g. transanal h. transvaginal i. Other (please specify) 53. How much do you agree with the following statements: [Rate each with the following scale: Totally disagree, Disagree, Slightly disagree, Not sure, Slightly agree, Agree, Totally agree, N/A] a. "A wound protector should always be used for extraction of the specimen" b. "Before performing the anastomosis the proximal colon should be actively checked for twisting" c. "Small bowel needs to be actively removed from the mesocolic gap" d. "The mesocolic gap should be closed with sutures" e. "A leak test (bubble test) should be performed after anastomosis" f. "Intraoperative endoscopy should be performed to check the integrity of the anastomosis" g. Other (please specify) 54. A diverting stoma should be performed: a. Never b. Always loop ileostomy c. Always loop colostomy d. Selectively, please specify: