Private Mental Health Alliance Centralised Data Management Service
advertisement
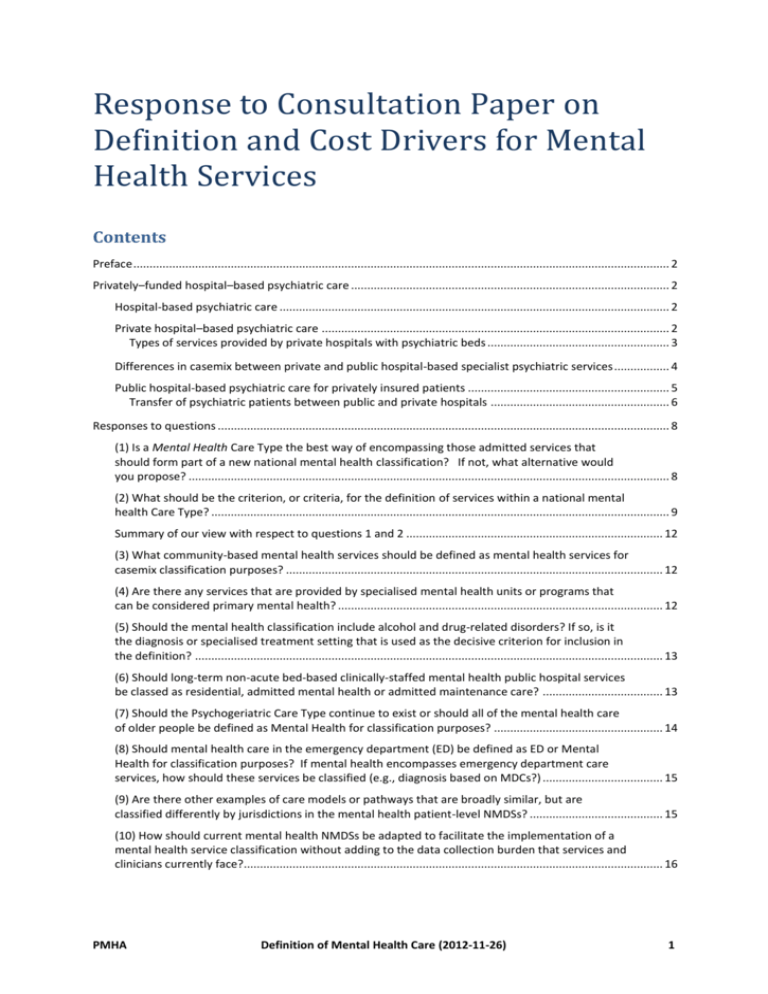
Response to Consultation Paper on Definition and Cost Drivers for Mental Health Services Contents Preface ..................................................................................................................................................................... 2 Privately–funded hospital–based psychiatric care .................................................................................................. 2 Hospital-based psychiatric care ........................................................................................................................ 2 Private hospital–based psychiatric care ........................................................................................................... 2 Types of services provided by private hospitals with psychiatric beds ........................................................ 3 Differences in casemix between private and public hospital-based specialist psychiatric services ................. 4 Public hospital-based psychiatric care for privately insured patients .............................................................. 5 Transfer of psychiatric patients between public and private hospitals ....................................................... 6 Responses to questions ........................................................................................................................................... 8 (1) Is a Mental Health Care Type the best way of encompassing those admitted services that should form part of a new national mental health classification? If not, what alternative would you propose? .................................................................................................................................................... 8 (2) What should be the criterion, or criteria, for the definition of services within a national mental health Care Type? ............................................................................................................................................. 9 Summary of our view with respect to questions 1 and 2 ............................................................................... 12 (3) What community-based mental health services should be defined as mental health services for casemix classification purposes? .................................................................................................................... 12 (4) Are there any services that are provided by specialised mental health units or programs that can be considered primary mental health? .................................................................................................... 12 (5) Should the mental health classification include alcohol and drug-related disorders? If so, is it the diagnosis or specialised treatment setting that is used as the decisive criterion for inclusion in the definition? ................................................................................................................................................ 13 (6) Should long-term non-acute bed-based clinically-staffed mental health public hospital services be classed as residential, admitted mental health or admitted maintenance care? ..................................... 13 (7) Should the Psychogeriatric Care Type continue to exist or should all of the mental health care of older people be defined as Mental Health for classification purposes? .................................................... 14 (8) Should mental health care in the emergency department (ED) be defined as ED or Mental Health for classification purposes? If mental health encompasses emergency department care services, how should these services be classified (e.g., diagnosis based on MDCs?) ..................................... 15 (9) Are there other examples of care models or pathways that are broadly similar, but are classified differently by jurisdictions in the mental health patient-level NMDSs? ......................................... 15 (10) How should current mental health NMDSs be adapted to facilitate the implementation of a mental health service classification without adding to the data collection burden that services and clinicians currently face?................................................................................................................................. 16 PMHA Definition of Mental Health Care (2012-11-26) 1 Preface The following responses to the Consultation Paper are predicated on the assumption that, whilst initially Activity-based funding will only affect some aspects of the funding of public hospital-based care, the development of a case classification for mental health services may well have direct consequences for the funding models used for private hospital-based care. Privately–funded hospital–based psychiatric care Hospital-based psychiatric care Statistics prepared by AIHW, on the basis of data submitted to the Institute by State and Territory Health Departments, enables us to obtain some insight into the volumes of care being provided. Unfortunately, variations between States and Territories in the way in which they handle Sameday admissions means that accurate statistics for what AIHW describe as Ambulatory-equivalent mental health care are not available. Nevertheless the statistics regarding episodes of Overnight inpatient care for patients with a principal diagnosis of a psychiatric disorder are informative. The following table presents the most recently available data. 1 Table 1: Mental health related separations from episodes of Overnight inpatient care where the Principal diagnosis was for a psychiatric disorder (including Alcohol or drug use disorders) during the period 1/7/2009 to 30/6/2010 inclusive. Mental health-related hospital separations With specialised psychiatric care 222,567 130,192 58.5% Public hospitals 91,503 41.1% Private hospitals 38,689 17.4% Without specialised psychiatric care 92,375 41.5% Public hospitals 82,783 37.2% Private hospitals 9,592 4.3% Private hospital–based psychiatric care Detailed information regarding the provision of psychiatric care in private hospitals with designated psychiatric beds can be gleaned from the Hospital Casemix Protocol data submitted by those hospitals to the PMHA’s CDMS. Less detailed information regarding the 1 From Australian Institute of Health and Welfare (2011) Australian hospital statistics 2009–10. Health services series no. 40. Cat. no. HSE 107. Canberra: AIHW. PMHA Definition of Mental Health Care (2012-11-26) 2 provision of care to patients with psychiatric diagnoses in all private hospitals is available in the AIHW’s Mental Health Services in Australia reports. Comparison of data held by the CDMS with data reported by AIHW indicates that there are some significant differences between what is reported by States and Territories to the AIHW and what is reported by participating hospitals to the CDMS. Particularly in the period between 2007 to 2010 not all private hospitals with psychiatric beds submitted HCP data to the CDMS. The 2009-2010 financial year is the most recent year for which parallel statistics are available. Inspection of that data suggests that in that year the CDMS data represented approximately 85% of the episodes of overnight inpatient care with specialised mental health care reported to AIHW. Consequently, an inflation factor was computed from the data for 2009-2010 and applied to the CDMS for that and the subsequent two financial years for which CDMS data is available.2 Types of services provided by private hospitals with psychiatric beds Four types of service can be distinguished in the HCP data provided to the CDMS by private hospitals with psychiatric beds. They are: Overnight inpatient care Overnight care for sameday procedures (maximum of 2 nights stay) Sameday admissions Outreach care or Hospital in the home care For the purposes of outcomes evaluation, the PMHA’s National Model treats Sameday admissions, Outreach care and hospital in the home care, and also Overnight care for sameday procedures, all as Occasions of service within episodes of Ambulatory care. For statistical reporting purposes, the AIHW treats Sameday admissions (and presumably also Outreach or hospital in the home care reported as sameday admissions) as Ambulatoryequivalent occasions of service. Comparison of the data for Ambulatory-equivalent occasions of service held by the CDMS with that reported by the AIHW indicates that there is a serious problem with that data reported to the AIHW by States and Territories. It is known that in fact there are very substantial differences between States and Territories in the way in which they classify Sameday admissions. This leads to very substantial underreporting of such admissions by South Australia and Western Australia. The following three tables provide estimates of the volume and costs of care provided to patients with principal psychiatric diagnoses in private hospitals with psychiatric beds. 2 The estimated inflation factors were 1.163 for 2009-2010, 1.109 for 2010-2011, and 1.054 for 2011-2012. PMHA Definition of Mental Health Care (2012-11-26) 3 Table 2: Estimates of the number of overnight inpatient separations for specialised psychiatric care provided in private hospitals with psychiatric beds during the periods 1/07/2009 to 30/06/2010, 1/07/2010 to 30/06/2011 and 1/07/2011 to 30/06/2012. Overnight inpatient care Overnight care for sameday procedures all Separations from overnight care 2009-2010 2010-2011 2011-2012 33,551 33,150 33,904 5,138 2,459 2,000 38,689 35,609 35,904 Table 3: Estimates of the total number of days of care for specialised psychiatric care provided in private hospitals with psychiatric beds during the periods 1/07/2009 to 30/06/2010, 1/07/2010 to 30/06/2011 and 1/07/2011 to 30/06/2012. Overnight inpatient care Overnight care for sameday procedures all overnight inpatient Service days Sameday admissions Outreach care and Hospital in the home care all ambulatory equivalent Service days 2009-2010 2010-2011 2011-2012 643,941 645,997 673,941 15,826 10,952 7,091 659,767 656,949 681,032 145,555 154,889 170,342 12,334 20,196 18,849 157,889 175,085 189,191 Table 4: Estimates of the total cost of care for specialised psychiatric care provided in private hospitals with psychiatric beds during the periods 1/07/2009 to 30/06/2010, 1/07/2010 to 30/06/2011 and 1/07/2011 to 30/06/2012. Overnight inpatient care Overnight care for sameday procedures Sameday admissions Outreach care and Hospital in the home care total cost of all care 2009-2010 2010-2011 2011-2012 342,725,694 359,513,532 379,677,656 4,038,446 2,015,435 1,815,337 38,433,260 42,609,383 47,292,994 2,203,742 4,180,151 3,835,651 387,401,142 408,318,501 432,621,638 Differences in casemix between private and public hospital-based specialist psychiatric services When considering only separations from overnight inpatient care, in the 2008-2009 financial year, separations from Private hospitals accounted for approximately 28% of all separations from specialised psychiatric overnight inpatient care for adults; separations from Public psychiatric hospitals accounted for a further 8%, whilst separations from Public acute hospitals accounted for the remaining 64%. That pattern of service provision has remained relatively constant over the past several years. PMHA Definition of Mental Health Care (2012-11-26) 4 There are important differences in the casemix of patients seen in private and public hospital-based specialist mental health services. 50000 Private hospitals 45000 Public psychiatric hospitals 40000 35000 Public acute hospitals 30000 25000 20000 15000 10000 5000 0 1 2 3 4 5 6 7 1 - Schizophrenia, Schizoaffective and Other Psychotic Disorders 2 - Major Affective and Other Mood Disorders 3 - Post Traumatic and Other Stress-related Disorders 4 - Anxiety Disorders 5 - Alcohol and Other Major Substance Use Disorders 6 - Eating Disorders 7 - Other Figure 1: Relative volume of separations from specialised psychiatric overnight inpatient care by type and sector of hospital, stratified by major diagnostic groups, for the period 1/07 2008 to 30/06/2009. Key differences are seen in both the diagnostic mix, as shown in the above figure, and also in the relative proportion of involuntary patients. In the 2008-2009 financial year, AIHW reported that 41.3% of separations from public acute hospitals and 62.7% of those from public psychiatric hospitals were for involuntary patients, whilst only 0.3% of separations from private hospitals were for involuntary patients. Whilst the very low proportion of involuntary patients seen in private hospitals does to some extent reflect regulatory issues and the complex issues surrounding the provision of informed financial consent by involuntary patients, these statistics also indicate that there are likely to be substantial differences in the needs for care between patients seen in the three hospital types. Taken together, these substantial differences in diagnosis and legal status, imply that any casemix classification developed just on the basis of patients seen in the public sector’s specialist mental health services is unlikely to be generally applicable. Public hospital-based psychiatric care for privately insured patients We have been unable to obtain detailed statistics regarding the provision within public hospitals of psychiatric care to patients with private health insurance. PMHA Definition of Mental Health Care (2012-11-26) 5 The PHIAC Annual Report does include statistics regarding the overall volume of the provision of privately-funded services within public hospitals, but does not break down those statistics by Principal diagnosis, Diagnosis related group, or Major diagnostic category. The following statistics are drawn from their Annual Report for the 2010-2011 Financial Year. The report treats Overnight Inpatient episodes and Admitted Same-day stays as Patient Episodes. However, Same-day stays are also reported separately so it is possible to calculate separate statistics for both Overnight Inpatient episodes and Same-days stays. Table 5: Episodes of admitted patient care for privately-insured patients, stratified by type of facility, during the period 1/7/2010 to 30/6/2011 inclusive. Overnight Inpatient N Same-day Stays p N p Public hospital 275,549 22.12% 219,451 10.30% Private hospital 968,262 77.71% 1,350,738 63.38% 226 0.02% 490,774 23.03% 1,897 0.15% 70,103 3.29% Day hospital facilities Hospital-substitute 1,245,934 2,131,066 As can be seen from the above, a substantial proportion of care paid for by private health insurers is provided in public hospitals. Unfortunately, as these statistics are not disaggregated by MDC or DRG, Mental health legal status, or Remoteness of hospital location, key questions about the pattern of provision of services to insured psychiatric patients in public hospitals can’t be answered. Transfer of psychiatric patients between public and private hospitals Some indication of the flow of privately insured psychiatric patients between public and private hospitals can be obtained by studying the Source of referral and Mode of Separation for episodes of Overnight inpatient care provided by private hospitals with psychiatric beds. Inspection of the following two tables reveals that in the 2010-2011 financial year about 5.2% of admissions were for patients transferred from another hospital, whilst in 2.6% of separations the patients were transferred to another acute or psychiatric hospital. The available data does not allow us to determine what proportion of those transfers into and out of private hospitals were from or to psychiatric units in public hospitals. However, even if we assume that all were, then the actual number of transfers still accounts for only 2,337 (7.82%) of the 29,896 episodes of overnight inpatient care for which data was available. PMHA Definition of Mental Health Care (2012-11-26) 6 Table 6: Source of referral for episodes of Overnight inpatient care with specialised psychiatric care provided by private hospitals with psychiatric beds during the period 1/7/2010 to 30/6/2011 inclusive. Code Description N p 1,565 5.23% 1 Admitted patient transferred from another hospital 2 Statistical admission – type change 83 0.28% 4 From Accident-Emergency 51 0.17% 5 From community health service 11 0.04% 6 From outpatients department 23 0.08% 7 From Nursing home 6 0.02% 8 By outside Medical Practitioner 26,403 88.32% 9 Other 1,753 5.86% 29,896 Table 7: Mode of separation for episodes of Overnight inpatient care with specialised psychiatric care provided by private hospitals with psychiatric beds during the period 1/7/2010 to 30/6/2011 inclusive. Code Description N 1 Discharge/transfer to an(other) acute hospital 2 Discharge/transfer to a nursing home 3 Discharge/transfer to an(other) psychiatric hospital 4 Discharge/transfer to other health care accommodation 5 p 653 2.18% 36 0.12% 119 0.40% 66 0.22% Statistical discharge - type change 151 0.51% 6 Left against medical advice/discharge at own risk 637 2.13% 7 Statistical discharge from leave 60 0.20% 8 Died 15 0.05% 9 Other (includes discharge to usual residence, own accommodation, etc) 28,158 94.19% 29,895 PMHA Definition of Mental Health Care (2012-11-26) 7 Responses to questions (1) Is a Mental Health Care Type the best way of encompassing those admitted services that should form part of a new national mental health classification? If not, what alternative would you propose? As it is presently defined, the data element Care Type, encompasses several discrete concepts: principal clinical intent (assessment, acute, rehabilitation, maintenance, palliative, etc); the status of the service that provides the care (designated unit, designated program, other); and the type of patient (newborn, adult, geriatric) which may or may not imply a specific type of service unit within the hospital. The following is the current code set for the data element Hospital service – Care type: 1.0 Acute care (Admitted care) 2.0 Rehabilitation care (Admitted care) 2.1 Rehabilitation care delivered in a designated unit (optional) 2.2 Rehabilitation care according to a designated program (optional) 2.3 Rehabilitation care is the principal clinical intent (optional) 3.0 Palliative care 3.1 Palliative care delivered in a designated unit (optional) 3.2 Palliative care according to a designated program (optional) 3.3 Palliative care is the principal clinical intent (optional) 4.0 Geriatric evaluation and management 5.0 Psychogeriatric care 6.0 Maintenance care 7.0 Newborn care 8.0 Other admitted patient care 9.0 Organ procurement - posthumous (Other care) 10.0 Hospital boarder (Other care) The notes following the definition indicate that “Persons with mental illness may receive any one of the care types (except newborn and organ procurement). Classification depends on the principal clinical intent of the care received”. The definitions of clinical intent embedded within the existing definition of Care Type can quite clearly can be applied to psychiatric care as usefully as they are applied to other specialties within the domain of physical health care. Indeed, that fact highlights the reasons why those types of care are necessary. Diagnosis alone does not necessarily identify the type of care that a patient may require. Changes of Care Type within an extended hospital stay allows such stays to be broken into discrete episodes of care to which differing casemix classifications may be applied. PMHA Definition of Mental Health Care (2012-11-26) 8 There clearly would be advantages to enabling a discrete mental health casemix classification to be applied to episodes of mental health care. The consultation paper identifies the key issue, that is, that this approach requires that the boundary between mental health and other services be clearly identifiable. Episodes of care provided in or by designated psychiatric units for patients with a principal psychiatric or substance use disorder quite clearly fall within the scope of that care type. The solution offered by the various subtypes of Rehabilitation care (i.e., Rehabilitation care delivered in a designated unit, Rehabilitation care according to a designated program , and Rehabilitation care is the principal clinical intent) and similarly for Palliative care provide an indication of how the boundary problem could be approached in the case of Mental Health. In the case of Rehabilitation, the definition makes clear that if the clinical intent is “rehabilitation”, regardless of the status of the unit providing the care or of the program within which context the care is funded, that part of the patient’s stay can be defined as a discrete episode of Rehabilitation type care. Adding Mental Health as a discrete Care Type within that framework may require that issues of clinical intent be addressed within the Mental Health specific classification. However, experience with the use of the analogous item, Focus of care, within the NOCC indicates that, at least within the ambulatory care service setting, that discrimination can be difficult to apply in practice. (2) What should be the criterion, or criteria, for the definition of services within a national mental health Care Type? As noted in the consultation paper, the present definition of Principal diagnosis as “The diagnosis established after study to be chiefly responsible for occasioning an episode of admitted patient care, an episode of residential care or an attendance at the health care establishment, as represented by a code”, regardless of the caveats mentioned in the paper, clearly should provide the first basis for the inclusion of services with a Mental Health care type in any setting where the assignment of a Principal Diagnosis is required. A definition that restricted Mental Health Care to only that care directly provided by specialised mental health service providers would omit an important sub-set of separations. For example, in general hospitals without designated psychiatric units in both the public and private sectors, patients with a principal diagnosis of a psychiatric disorder may be admitted and managed by clinicians other than those employed by community-based publicly-funded specialist mental health services. This is particularly true in regional or rural areas. That is, such patients may not receive in-reach care from community-based publicly-funded mental health service staff. Instead, their care may be provided by the hospital’s general nursing PMHA Definition of Mental Health Care (2012-11-26) 9 staff under the direction of their local GP or private Psychiatrist. Regardless, the principal reason for admission would be for the provision of psychiatric care. Use of the same logic as that applied to Rehabilitation type care would probably resolve this issue. For example, the case addressed in the preceding paragraph would fall under the 3 rd subtype identified in the following subtypes of mental health care: .1 Mental health care delivered in a designated unit .2 Mental health care according to a designated program .3 Mental health care is the principal clinical intent The consultation paper goes on to point out that diagnoses included with chapter 5 of ICD10-AM, Mental and Behavioural Disorders, do not entirely account for patients treated in designated psychiatric units. However, in all but a very few cases, it is likely that the type of care provided is almost always psychiatric care, and more importantly, that the principal diagnosis or problem is a direct consequence of a secondarily identified mental or behavioural disorder. The consultation paper also notes that a patient may not initially be admitted for mental health care, but that subsequently it may be discovered that the principal reason for their admission is a principal diagnosis of a mental or behavioural disorder. For example, a patient with severe chest pain may be admitted overnight, but on close examination the following day may be found to be suffering from severe panic disorder, rather than cardiovascular disease. Given that diagnosis, the patient might be discharged immediately, hopefully with an immediate referral to an appropriate mental health service provider. In this example, the diagnosis of panic disorder may well have been made by the cardiovascular specialist. In that case, the principal diagnosis might well be “F41.0 Panic disorder without agoraphobia”, but no explicit Mental Health Care may have been provided. This does raise some significant issues and does particularly highlight the fact that principal diagnosis alone is an insufficient basis for determining whether or not a patient received Mental Health Care. However, the capacity of any given hospital stay to be broken down into discrete episodes of care with differing care types would seem to be capable of handling such cases. The proposed sub-classification of Mental Health Care given includes within its scope, by simple definition, both care provided by a designated psychiatric or mental health care unit and the care provided within the context of a designated psychiatric or mental health care program. That is, once a service or program is explicitly designated as a specialised mental health service or program, the care provided within that context is by definition, Mental Health Care. Whilst useful and probably almost always correct, this is also clearly circular and does not resolve the definitional problem at all. This is made explicit by the inclusion of the last subclass in which “Mental health care” is identified as a kind of “Principal clinical intent”. It does however serve to make clear that the question, what is “Mental Health PMHA Definition of Mental Health Care (2012-11-26) 10 Care”, needs to be answered in a service and provider neutral manner. (The issue of who is qualified to provide such “Mental Health Care” is an important, but in this case, secondary, matter.) That is, we can’t answer the question “What is mental health care”, by stating that it is care provided in a particular type of unit or that it is care provided by a particular type of healthcare professional. Rather, the definition must explicitly identify a range of interventions explicitly targeted at a specified range of conditions, the purpose of such interventions including assessment, acute care, rehabilitation, maintenance , and possibly for some conditions, also palliative care. That definition should also explicitly include interventions aimed at addressing the longer-term social and psychological impacts of mental illness. The concept of principal clinical intent is critically important. In some cases the psychiatric input is part of the total package of medical care. One example is the anxious patient with chest discomfort that turns out to be non-cardiac chest pain. Another more frequent case is of people admitted to hospital following an overdose. Initially they may require intensive medical treatment and only later will they be transferred to a psychiatric unit. In such cases the focus isn’t necessarily mental health care at the beginning although it may be at the end. Usually in that sense, there is a discrete transfer, so there is a decision point at which the focus is medical care and then it becomes mental health care. This is however going to become more difficult as time goes on as it is increasingly found that certain medical conditions require mental health care. Consultation-liaison psychiatry services provide the strongest example of this issue. In hospital-based settings, not only will mental health service providers be called upon to explicitly assist with medical and surgical patients’ mental health problems, they may increasingly also become involved in the diagnosis and treatment of health problems that formally were considered amenable only to medical intervention. For example, increasingly certain gastrointestinal symptoms are found to be best treated with antidepressants and counselling rather than repeated endoscopies and colonoscopies. Within this context, the overall classification scheme, not just that used for Mental health type care, must continuously evolve. As psychological and behavioural interventions become part of the care for someone with a particular medical diagnosis then the casemix classification should start to capture that in the same way that the current DRGs deal with different surgical procedures. In the same way as when episode of care for a certain procedure is identified one has to count within that a certain degree of recovery time, intensive care use, the services of an anaesthetist, etc. So for some of these conditions one or two consultations from psychiatrists or other mental health professionals will also have to be counted as a part of the package of care for that condition. PMHA Definition of Mental Health Care (2012-11-26) 11 Summary of our view with respect to questions 1 and 2 Our preferred view, at this stage, is as follows. First, a separate Care Type for Mental Health care be identified and that that new Care Type be sub-classified in the same manner as which both the Rehabilitation and Palliative Care Types are now sub-classified. Second, a definition of Mental Health Care must be developed that identifies the boundaries of that Care Type within the explicit context that a patient may only be in receipt of one Care Type at any given time during their hospital stay. (We understand that that will mean that certain kinds of consultation-liaison services will remain out of scope.) Third, the definition of Mental Health Care must not be limited to that provided by a designated mental health unit or to that provided within the context of a designated program, but rather, must explicitly identify what is to be understood when it is stated that the principal clinical intent of the care provided is Mental Health Care. As noted above in our response to question 2, the definition must explicitly identify a range of interventions or classes of intervention explicitly targeted at a specified range of conditions, the purpose of such interventions including assessment, acute care, rehabilitation, maintenance, and intensive extended care. That definition should also explicitly include interventions aimed at addressing the longer-term social and psychological impacts of mental illness. (3) What community-based mental health services should be defined as mental health services for casemix classification purposes? The fact that the site of operation of the mental health service is a community-based health facility is probably not actually relevant. The question should rather be, what types of services, beyond hospital-based psychiatric overnight inpatient care, should be defined as mental health care? From that broad perspective, the answer to this question should simply be a subset of the answer to question 2 above. From the perspective of private hospital-based psychiatric services, clearly all mental health care services provided to in respect of an identified patient, whether that be facility-based individual or group-based care and also home-based care for mental and behavioural disorders and related problems, should all be in scope. (4) Are there any services that are provided by specialised mental health units or programs that can be considered primary mental health? Our understanding is that at this stage, private hospitals are not generally providing these types of services. PMHA Definition of Mental Health Care (2012-11-26) 12 We are aware that in the public sector there are quite a few pilot projects now looking at prevention, where there is a component of clinical care bound up in it. That care is arguably not at tertiary or secondary level, but rather at primary or primary prevention level. Such pilot projects are definitely being undertaken within child and adolescent mental health services. (5) Should the mental health classification include alcohol and drug-related disorders? If so, is it the diagnosis or specialised treatment setting that is used as the decisive criterion for inclusion in the definition? In general, apart from acute detox in a medical setting and presentations to EDs of persons in an acutely intoxicated state, clinical services provided to patients with a principal (not secondary) diagnosis of an alcohol and/or drug-related disorder might be expected to almost always be for some form of psychotherapeutic or behavioural care. For medical care other than for acute–detox, it is assumed that the principal diagnosis would be the medical condition itself, with the diagnosis of an alcohol and/or drug-related disorder being one of the secondary diagnoses. Even for patients undergoing acute detox in a medical setting and presentations to EDs of persons in an acutely intoxicated state, it might be expected that there would be a substantial psychiatric/behavioural component to the clinical services provided. If the above is largely true, then it could be argued that the mental health classification must include alcohol and drug-related disorders, and that it is the intersection of the diagnosis and the type of care that should be used as the decisive criterion for inclusion in the definition. Generally the model being used in the private sector is that Rehabilitation services for patients with Alcohol and other drug use disorders are almost always provided by psychiatric units. On the other hand, we understand that, particularly in public ambulatory care service settings, there may be good organisational and practical reasons why a separate classification, perhaps even a separate Care Type, for such services, may be useful. (6) Should long-term non-acute bed-based clinically-staffed mental health public hospital services be classed as residential, admitted mental health or admitted maintenance care? The key point would seem to be the costs implied by the specification that: a) the care is provided in a hospital setting; and b) that that care is provided by clinical staff. In the absence of a discrete Mental Health care type it would be appropriate to describe it as PMHA Definition of Mental Health Care (2012-11-26) 13 “Admitted maintenance care”. If there were to be a discrete Mental Health care type, within that classification, then one would need to consider what actual differences in costs and the nature of the services provided, if any, were apparent between hospital-based admitted residential care and community-based, presumably non-admitted, residential care. For private hospital-based services this specific issue is not currently relevant. However, the more general issue of how equivalent services provided in different settings are dealt with is. In general our view would be that the nature of the facility providing the service is largely irrelevant, so long as the nature of the services provided are essentially the same. From that perspective, it could be argued that the additional support in depth that a hospital setting may provide could well be important. This issue will become increasingly important as alternatives to inpatient care increase, particularly for older people and also for children and adolescents. (7) Should the Psychogeriatric Care Type continue to exist or should all of the mental health care of older people be defined as Mental Health for classification purposes? In the hospital setting, the issues that have led to the definition of a separate Psychogeriatric care type are similar to the issues that would also lead to the specification of a separate Child and adolescent mental health care type. In respect of hospital-based mental health services, the practitioners involved in the provision of care, medical and psychiatric, nursing and non-nursing, is different both in psychogeriatric services and in child and adolescent services. Consequently there is not as clean a cut either between geriatrics and psychiatry or between paediatrics and psychiatry as there is in the case of psychiatric services for adults. Depending on the age bands of patients, the setting will be different and the way you do it will be different. Outside of the hospital-based service setting the issues are likely to be different. Whether you count it as just one classification, or whether you have discrete ones is not something we are in a position to comment on. However, as the classification system will be used for payment purposes, that decision has very clear ramifications beyond those usually involved in adult mental health services. Consequently, given that there are clear reasons why Psychogeriatric care has been identified as a specific Care Type, our view is that services provided to Children and Adolescents with mental health problems will also need to be given close attention because PMHA Definition of Mental Health Care (2012-11-26) 14 the type of care and the setting in which it is given and the kind of packages will be quite different from adult mental health care. (8) Should mental health care in the emergency department (ED) be defined as ED or Mental Health for classification purposes? If mental health encompasses emergency department care services, how should these services be classified (e.g., diagnosis based on MDCs?) The paper succinctly draws out the fact that the issues of principal clinical intent (emergency care), the setting within which the care is provided (a designated emergency department), the type of patient (a person with a psychiatric or behavioural problem), and the type of service provider (specialist mental health staff) are entangled. Also, persons presenting to an ED may have strongly interacting physical and mental health issues, particularly at the time of their presentation, but also as the psycho-social and behavioural background within which their presentation takes place. Within that context any attempt to separate Mental Health from ED within the ED setting may have unintended side effects. More generally, how they are or are not disentangled may have significant cost, operational and clinical implications. In particular, separating mental health care provided in an ED from other care provided in the ED for classification purposes may have substantial unintended negative effects on efforts to integrate effective emergency mental health care into the ED setting. (9) Are there other examples of care models or pathways that are broadly similar, but are classified differently by jurisdictions in the mental health patient-level NMDSs? Under what is known as the Hospitals Casemix Protocol (HCP), all admitted patient services provided to privately insured patients by hospital establishments that have contracts with health insurance funds must provide data to those funds regarding each fund’s members’ admissions to those establishments. The HCP data is the primary source of information used by the PMHA’s CDMS in its analysis of service provision by private hospitals with psychiatric beds. Collections based on the HCP are likely to be highly accurate as the data is derived directly by hospitals from their patient administration systems. As those systems are also used for billing purposes, with that data being closely scrutinised by health insurance funds, their records are rarely incorrect. For private hospitals with psychiatric beds, all care, regardless of service setting, is provided on an admitted basis. That includes all occasions of service provided in what would under the National Outcomes and Casemix Collection be defined as the Ambulatory care service PMHA Definition of Mental Health Care (2012-11-26) 15 setting. As can be seen in Table 3 on page 4, over the past three years approximately 90% of those services are provided as Sameday admissions. The majority of those are for patients attending hospital-based, group psychological treatment programs. Those programs are usually based on either a CBT or DBT model of therapy and are not openended in duration. On average, patients receive approximately 8 to 15 occasions of service within any such episode of Ambulatory care. The remaining 10% of ambulatory-equivalent services are either Hospital-in-the-home or Outreach type care provided by hospital staff in the patients home. As well as being required to submit data to health funds under the HCP, private hospitals are also obliged to submit data to their State or Territory in accordance with that jurisdiction’s hospital data collection requirements. Those submissions form the basis of each jurisdiction’s submission of data regarding private hospital-based services to the AIHW under the various NMDSs. As already noted under the sub-section titled Types of services provided by private hospitals with psychiatric beds on page 3 of this document, Ambulatory equivalent mental health care, particularly sameday admissions of patients to group-based psychological interventions, are classified differently by some jurisdictions. This leads to very substantial underestimates in the volume of such services provided by private hospitals with psychiatric beds. More generally, it is our view that a definitive answer to this question will only be obtained by conducting a desktop review of the current State and Territory statistics collections relevant to health services that provide mental health care (whether that be specialised or not), together with the current NMDSs and the HCP data sets, all of which apply at a national level. A formal comparison of the definitions of relevant care types and related coding rules should reveal any important differences. (10) How should current mental health NMDSs be adapted to facilitate the implementation of a mental health service classification without adding to the data collection burden that services and clinicians currently face? First, regardless of what adaptations are proposed, it is our very strong view that very close attention must be paid to the actual feasibility, validity and reliability of coding and collecting any new data elements that are required by any proposed new classification. With respect to the substantive question, we suggest that, in the same way as the Rehabilitation Care Type specific data elements are currently linked to the primary HCP data set, the relevant NOCC and other required data elements could be specified within a Mental Health Care Type specific data set. Records in that new data set should be linked to the primary data set(s) at the episode level by an Episode identifier. PMHA Definition of Mental Health Care (2012-11-26) 16 To ensure that as much as possible of the full clinical path is available for analysis and reporting beyond its initial use in classification, we would expect that appropriate identifiers will also be included to enable, at least at the Establishment or Mental health service organisation level, the data to also be linked at the patient or consumer level. PMHA Definition of Mental Health Care (2012-11-26) 17