MSG-Final-Assignment-MG
advertisement
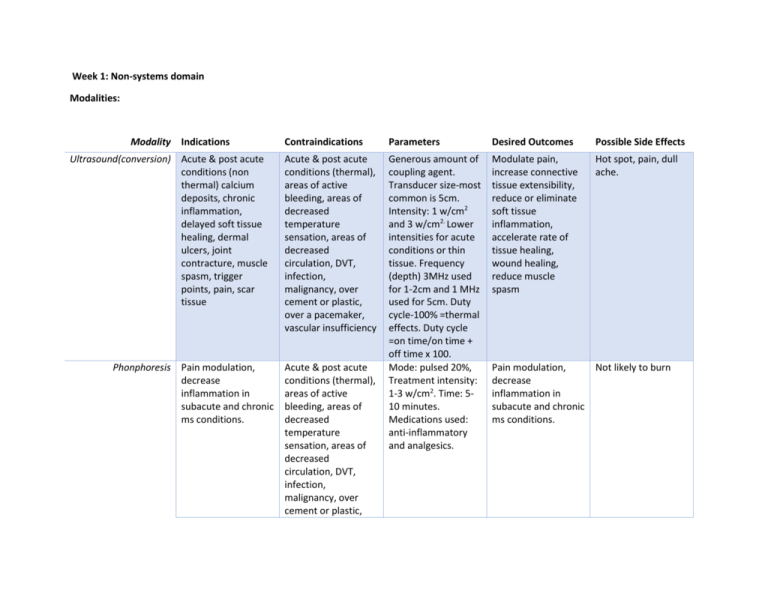
Week 1: Non-systems domain Modalities: Modality Indications Ultrasound(conversion) Acute & post acute conditions (non thermal) calcium deposits, chronic inflammation, delayed soft tissue healing, dermal ulcers, joint contracture, muscle spasm, trigger points, pain, scar tissue Phonphoresis Pain modulation, decrease inflammation in subacute and chronic ms conditions. Contraindications Parameters Desired Outcomes Possible Side Effects Acute & post acute conditions (thermal), areas of active bleeding, areas of decreased temperature sensation, areas of decreased circulation, DVT, infection, malignancy, over cement or plastic, over a pacemaker, vascular insufficiency Generous amount of coupling agent. Transducer size-most common is 5cm. Intensity: 1 w/cm2 and 3 w/cm2. Lower intensities for acute conditions or thin tissue. Frequency (depth) 3MHz used for 1-2cm and 1 MHz used for 5cm. Duty cycle-100% =thermal effects. Duty cycle =on time/on time + off time x 100. Mode: pulsed 20%, Treatment intensity: 1-3 w/cm2. Time: 510 minutes. Medications used: anti-inflammatory and analgesics. Modulate pain, increase connective tissue extensibility, reduce or eliminate soft tissue inflammation, accelerate rate of tissue healing, wound healing, reduce muscle spasm Hot spot, pain, dull ache. Pain modulation, decrease inflammation in subacute and chronic ms conditions. Not likely to burn Acute & post acute conditions (thermal), areas of active bleeding, areas of decreased temperature sensation, areas of decreased circulation, DVT, infection, malignancy, over cement or plastic, Moist Heat Modulate pain, increase connective tissue extensibility, reduce inflammation, increase tissue and wound healing, reduce muscle spasm. over a pacemaker, vascular insufficiency Impaired circulation, Impaired cognitive function, Impaired sensation, Malignant tumors, over blood clot, over pacemaker, over plastic components. Paraffin Modulate pain, increase connective tissue extensibility, reduce inflammation, increase tissue and wound healing, reduce muscle spasm. Impaired circulation, Impaired cognitive function, Impaired sensation, Malignant tumors, over blood clot, over pacemaker, over plastic components. Fluidotherapy Modulate pain, increase connective tissue extensibility, reduce inflammation, increase tissue and wound healing, reduce muscle spasm. Impaired circulation, Impaired cognitive function, Impaired sensation, Malignant tumors, over blood clot, over pacemaker, over plastic components. Decrease muscle spasm, decrease tone, increase blood flow to treatment area, increase capillary permeability, increased collagen extensibility, increased nerve conduction velocity Decrease muscle spasm, decrease tone, increase blood flow to treatment area, increase capillary permeablity, increased collagen extensibility, increased nerve conduction velocity Decrease muscle spasm, decrease tone, increase blood flow to treatment area, increase capillary permeability, increased collagen extensibility, increased nerve Burns, rashes, skin irritation Reaction to paraffin, spread of bacteria, burns, Spread of bacteria, burns, conduction velocity Diathermy Modulate pain, increase connective tissue extensibility, reduce inflammation, increase tissue and wound healing, reduce muscle spasm. Impaired circulation, Impaired cognitive function, Impaired sensation, Malignant tumors, over blood clot, over pacemaker, over plastic components. Ice Massage Inflammation, pain control, abnormal tone, acute or chronic pain, bursitis, muscle spasm, MS trauma, trigger points, tendonitis Cold intolerance, cold urticaria (hypersensitivity), infection, over an area of compromised circulation, over regenerating peripheral nerves, PVD, Raynaud’s, skin anesthesia Cold intolerance, cold urticaria (hypersensitivity), infection, over an area of compromised circulation, over regenerating peripheral nerves, PVD, Raynaud’s, skin anesthesia Cold intolerance, cold urticaria Ice Pack(conduction) Inflammation, pain control, abnormal tone, acute or chronic pain, bursitis, muscle spasm, MS trauma, trigger points, tendonitis Ice bath Commonly use for the immersion of the Decrease muscle spasm, decrease tone, increase blood flow to treatment area, increase capillary permeability, increased collagen extensibility, increased nerve conduction velocity Decrease blood flow to area, decrease spasticity, decreased edema, decreased metabolic rate, decreased nerve conduction velocity, increase pain threshold Hot spots, dull ache, periosteal pain Applied every 1-2 hrs for 10-20 minutes. Maintained at 010°F. Decrease blood flow to area, decrease spasticity, decreased edema, decreased metabolic rate, decreased nerve conduction velocity, increase pain threshold Red or dark pink. Abnormal: Erythema of the skin with wheal formation, associated c severe itching, decreased BP, increased HR Temperature ranging from 55-64° F. Body Decrease blood flow to area, decrease Inappropriate due to dependent position Apply the ice massage to an area no larger than 4x6 inches in slow overlapping circles. Treat 5-10 minutes or until analgesia occurs. Cold, burning, aching, and numbness distal extremities Cryocuff To combine cold and compression, most often used on the knee and post operatively to decrease pain Vapocoolant Reduce muscle Spray(evaporation) spasms, trigger points, myofascial referred pain TENS Acute or chronic pain modulation. (hypersensitivity), infection, over an area of compromised circulation, over regenerating peripheral nerves, PVD, Raynaud’s, skin anesthesia Cold intolerance, cold urticaria (hypersensitivity), infection, over an area of compromised circulation, over regenerating peripheral nerves, PVD, Raynaud’s, skin anesthesia Cold intolerance, cold urticaria (hypersensitivity), infection, over an area of compromised circulation, over regenerating peripheral nerves, PVD, Raynaud’s, skin anesthesia Patient with demand type pacemaker, TENS is not applied over neck, eyes, head, or following a CVA or seizures part should be immersed for 15-20 minutes. spasticity, decreased edema, decreased metabolic rate, decreased nerve conduction velocity, increase pain threshold Can provide hours of mild cooling Decrease blood flow to area, decrease spasticity, decreased edema, decreased metabolic rate, decreased nerve conduction velocity, increase pain threshold Red or dark pink. Abnormal: Erythema of the skin with wheal formation, associated c severe itching, decreased BP, increased HR Hold 18-24 inches away from treatment area, spray at 30° angle and sweep spray. Muscle should be passively stretched before and during. 10-15 minutes treatment time. See therapy ED book for all the different parameters and conditions. Increase ROM, reduce spasm/pain Frosting of the skin Acute or chronic pain modulation. Burns from exposed wires, Pain with treatment, to strong of current, improper electrode placement NMES Disuse atrophy, impaired ROM, muscle spasm, muscle reeducation, spasticity management Premod Modulate pain, increase muscle strength, increase ROM, decrease edema Iontophoresis Analgesia, calcium deposits, Dermal ulcers, edema reduction, fungal infections, hyperhydrosis, muscle spasm FES Disuse atrophy, impaired ROM, muscle spasm, muscle reeducation, spasticity management IFC Modulate pain, increase muscle strength, increase ROM, decrease edema If the patient has a pacemaker, unstable arrhythmias, seizure disorders, over carotid sinus, active bleeding, metal implants, If the patient has a pacemaker, unstable arrhythmias, seizure disorders, over carotid sinus, active bleeding, metal implants, Impaired skin sensation, allergy to agent, cuts, bruises or broken skin, over metal Amplitude- titanic muscle contraction, Pulse rate- 50-70 PPS, pulse duration 150-200 usec Disuse atrophy, impaired ROM, muscle spasm, muscle reeducation, spasticity management Burns from exposed wires, Pain with treatment, to strong of current, improper electrode placement Amplitude- strong but comfortable, pulse rate- 1-5 PPS, pulse duration- 150300 usec, mode continuous, Modulate pain, increase muscle strength, increase ROM, decrease edema Burns from exposed wires, Pain with treatment, to strong of current, improper electrode placement Direct current, max intensity 4-5 mA. Negative electrode should be twice as large as positive electrode. Skin irritation, pain, rash, allergic reaction to agent, burns, If the patient has a pacemaker, unstable arrhythmias, seizure disorders, over carotid sinus, active bleeding, metal implants, If the patient has a pacemaker, unstable arrhythmias, seizure disorders, over carotid sinus, active Tetanic muscle contraction, pulse rate 30-85 pps, duration 15-30 min, Decrease In Analgesia, calcium deposits, Dermal ulcers, edema reduction, fungal infections, hyperhydrosis, muscle spasm Disuse atrophy, impaired ROM, muscle spasm, muscle reeducation, spasticity management Modulate pain, increase muscle strength, increase ROM, decrease edema Burns from exposed wires, Pain with treatment, to strong of current, improper electrode placement. Amplitude- strong but comfortable, pulse rate- 1-5 PPS, pulse duration- 150300 usec, mode Burns from exposed wires, Pain with treatment, to strong of current, improper electrode placement bleeding, metal implants, continuous, Lumbar Traction Disk Herniation, Joint hypomobility, muscle guarding, nerve root impingement, muscle spasm, subacute pain, osteophyte formation. Bone disease, fractures, dislocation, pregnancy, osteoprosis, acute sprains/strains, aortic aneurysm, hiatal hernia Cervical Traction Disk Herniation, Joint hypomobility, muscle guarding, nerve root impingement, muscle spasm, subacute pain, osteophyte formation Biofeedback Bowel incontinence, CP, hemiplegia, impaired motor control,muscle spasms, spinal cord injuries, urinary incontinence Bone disease, fractures, dislocation, pregnancy, osteoprosis, acute sprains/strains, Conditions where muscle contraction is detrimental, skin irritation at the electrod site. Force of 25% of total body weight will allow stretching soft tissue and treat muscle spasms and disk protusions, force of 50% is used to actually separate the vertebrae. Time: 10-30min. Force on initial treatment should be 7-10% of patients body weight, 11-15 pounds. 20-30 pounds will be necessary for joint distraction. Two active electrodes should be place parallel to the muscle fibers, The reference electrode can be placed anywhere on the body, isometric contraction hold for 6-10 sec. duration 5-10 min for muscle re-education Descriptor Temperature Cool 67.0-80.0F (19.0-27.0C) Cold 55.0-67.0F(13.0-19.0C) Very Cold 32.0-55.0F(0.0-13.0C) a. Intermittent Compression Pump Definition Pneumatic unit designed to apply external pressure to an edematous body part by a two layered nylon or plastic appliances shape to fit either the upper or lower extremity used to help reduce edema. Treatment should be a minimum of 2 hours for every 24 hours and should provide pressure less than 50mmHg for upper extremities. and 60 mmHg for lower extremities to be safe and effective. The pressure is applied for 45-90 seconds and then released for 15-30 minutes. The frequency is between 304 weeks Indication Contraindications Postmastectomy lymphedema. Open the lymphatic channels using manual lymphatic massage prior to using the pup Patients with arterial insufficiency have increased peripheral resistance, and compression increases it further Traumatic edema Infections at the site of treatment may be spread by introducing bacteria into the lymphatic or venous drainage Dependent edema of pregnancy Any thrombi present may become mobile Venous insufficiency Edema in patients with congestive heart failure should not be treated, because the increased peripheral resistance increases the work of the heart. Definition Condition Indication Ion (Polarity) Contraindications Amputations Edema in patients with kidney dysfunction should not be treated, because the kidney may not be able to excrete teh additional fluid Prevention of thrombophlebitis postsurgically Obstructed lymphatic channels do not allow drainage. Treatment is ineffective, and the patient may experience increased pain Stasis ulcers Displaced fractures. Treatment may displace them further Mode of Action Concentration of Solution Dosage Athletes Foot Copper (+) Fungicidal 1% copper sulfate sodium 10mA for 15 minutes, 2x/week Slow Healing Wound Zinc (+) Bactericidal 1.0 M zinc oxide gel (8.138 g zinc oxide powder, 10g glycerol, 10g bentonite, 71.862 g water) 3-6mA for 20 minutes, increased to25-30 minutes at end of each of first 2 weeks; 5 days a week for 3 weeks. Definition Indication Contraindications Posttraumatic Edema Hyaluronidase (+) Breaks down hyaluronic acid 150 units of hyaluronidase in 250 mL of a buffer solution that consists of (1) sodium acetate 3H2O: 11.42 g (2) Glacial acetic acid: 0.923 mL (3) distilled H2O, quantum satis (qs): 1000 mL 20mA for 20 0minutes 3x/week Plantar Warts Salicylate (-) Removal and relief of pain 2% sodium salicylate in aqueous solution 10mA times min; once per week for 2-3 treatments Trigger Points Procaine or Lidocaine (+) Local anesthesia (use with caution) 1% solution in 60-80% alcohol with 1:20,000 adrenalin 20-30 mA for 20-30 minutes 1-3 times per week Acute RA Citrate (-) Prevents local autoimmune response 1% potassium citrate in distilled water 7.5-10 mA for 20 minutes; daily 3x/week Peripheral Circulatory Deficit Histamine (+) Vasodilator 1:10,000 histamine diphosphate 3-12 mA for 5-20 minute (approximately 60 mA times minute); 2-3 x/week Gout Lithium (+) Competes with sodium in formation of urate lithium urate is soluble 2% lithium chloride 5mA for 20 minutes; one time per week for 4 weeks Definition Myositis Ossificans Indication Acetate (-) Absorption of calcium Contraindications 3mL of 2% acetic acid in 4 mA for 20 minutes; distilled water followed by ultrasound for 8 minutes at 1.5 W/cm2 at 50% duty cycle Choosing an Assistive Device 2. Amount of Weight Bearing Unilateral LE WB Restriction Bilateral LE WB Restriction PWB almost full WB 1 Standard Cane 2 Standard Canes Dec PWB 1 Crutch Lofstrand Crutches Dec, Dec PWB 2 Canes 2 Crutches or Walker Dec, Dec, Dec PWB 2 Crutches 2 Crutches or Walker TT 2 Crutches or walker Unable to walk NWB 2 Crutches or walker Unable to walk Amount of Strength Unilateral LE Weakness Bilateral LE Weakness Minimal Weakness 1 Standard Cane 2 Standard Canes Decreased Strength 1 Quad Cane 2 Quad Canes Dec, Dec Strength 1 Crutch Lofsrtand Crutches Significant Weakness 2 Crutches or Walker 2 Crutches or Walker Balance Impairment Ambulatory Assistive Device Minimally Impaired 1 Cane Min-Mod Impaired 1 Lofstrand crutch Moderately Impaired 2 Crutches or Walker Significantly Impaired 2 Crutches or walker and guarding. Precautions Definition Standard Precautions Universal precautions and are designed for the care of all patients in hospitals regardless of infection or diagnosis. Droplet Precautions Reduce the risk of droplet transmission of infectious agents through the mouth, nose, coughing, sneezing, talking, or suctioning. Travel 3 ft or less. Contact Precautions Reduce the risk of transmission of infectious agents through direct or indirect contact. Airborne Precautions Reduce the risk of airborne transmission of infectious agents through evaporated droplets in Indications Procedure: Hand washing, wear gloves and change between tasks, wear mask or gown if risk of spalashing body fluids. Private room, may share room if pt has same microorganism, maintain at least 3 ft between pt and staff. Room door may remain open, wear a mask when working within 3 feet. Limit pts transport outside of room, pt should wear mask during transport. Private room, may share. Use of gloves when entering room, change of gloves, wear a gown if necessary, limit pts transport, do not share equipment Private room with monitored air pressure, 6-12 air changes within the room per hour, room door Common Situations Every hospital patient. Bacterial: meningitis, pneumonia, sepsis, pertussis, strep Viral: adenovirus, influenza, mumps, paroviarus, rubells GI, respiratory, skin or wound infections, multi-drug resistant bacteria, e-coli, diphtheria, herpes, impetigo, scabies, zoster Measles, varicella, tuberculosis air or dust particles should remain closed with pt remaining in room, respiratory protection worn when entering the room, limit pts transport outside the room, pt should wear mask during transport. Research Terminology Definition Sensitivity When referring to a medical test, sensitivity refers to the percentage of people who test positive for a specific disease among a group of people who have the disease. A true positive. SnNout: a negative test rules it out. Specificity When referring to a medical test, specificity refers to the percentage of people who test negative for a specific disease among a group of people who do not have the disease. A true negative. SpPin: a positive test rules it in. Independent Variable The variable that is presumed to have caused or influenced the dependent variable. In research, the IV is what is controlled or manipulated by the researcher. Dependent Variable The response or outcome assumed to be caused by the effect of the IV. Control Group A group against which the treatment group is compared. Should be statistically identical to the treatment group, except for the variable of interest that is being evaluated in the experiment. Used to help isolate the effect of the IV and eliminate the unintended influence of extraneous factors that can confound the results. Research Design The overall strategy that you use to integrate the different components of the study in a coherent and logical way Positive Likelihood Ratio Probability of an individual with the condition having a positive test. Negative Likelihood Ratio Probability of an individual with the condition having a negative test. Randomization A means of assigning subjects to groups in a experiment so that each subject has an equal chance of being assigned to each group. The most robust method of random assignment is accomplished by computer-generated random numbers or random number tables. P Value The probability that a particular statistical result could have happened by chance. When the p-value is smaller than the stated value of alpha, or level of significance, the null hypothesis is rejected. When the p-value is larger than the stated value of alpha, or level of significance, the null hypothesis is not rejected. Blinding Conditions that are imposed to keep groups of individuals from knowing which subjects have or have not received an intervention. Used to reduce bias and the placebo effect. Intrarater reliability The consistency or equivalent of repeated measurements made by the same person over time. Interrater reliability The consistency or equivilance of measurements made by more than one person. Interrater reliability indicates the agreement of measurements taken by different examiners. Nominal Classification scale. Qualitative rather than quantitative. Ex. Blood type, type of breath sound, and type of arthritis. Ordinal Ranking scale. Intervals between ranks may not be equal. Ex. MMT grades, levels of assist, pain, and joint laxity grades. Interval Intervals between adjacent values are equal, but no true zero point. Ex. Temperature. Ratio Intervals between adjacent values are equal and there is a true zero point. Ex. ROM, distance walked, time to complete activity (seconds), nerve conduction velocity. Mean The average; sum of all the values divided by the number of values Median Middle value, 50% Mode The value that occurs most. t-test An inferential statistical procedure for estimating a population mean or comparing two means when the population is normally Chi-square test Reliability Validity Levels of Evidence distributed and the population variance is not known. A nonparametric statistical procedure for nominal data. The test evaluates the difference between observed and expected frequencies to examine the association or independence between categorical variables. Is the reproducibility or repeatability of measurements. Is the degree to which a useful or meaningful interpretation can be inferred from a measurement. Systematic Review, Meta-analysis, Randomized Controlled Trial, Cohort study, Case control, Cross-sectional study, case or report or case series. Equipment & Devices: Assistive and Adaptive Devices: *Pressure relief push-ups are required, typically ever 15-20 minutes. *Folding frames make wheelchair transport and storage easier. Rigid frames are typically lighter and sturdier. Standard adult w/c dimensions for environmental access: 360° turning space = 60 inches X 60 inches (5ft x 5ft) 90° turning space= minimum of 36 inches Minimum for doorways and halls=32 in; ideal is 36 inches Countertops= no higher than 31 inches Ramps=recommended ratio of slope to rise is 1:12 (for every inch of vertical rise, 12 inches of ramp is required) 8.3% grade; minimum of 36 inches wide, with nonslip surface; handrail waist high for ambulators (34-38 inches) and should extend 12 inches beyond the top and bottom of runs; ramp should have level landing at top and bottom. Wheelchair measurements: Measurement Seat height Instructions Measure from the user’s heel to the popliteal fold and ADD 2 inches to allow clearance of Average adult size 19.5-20.5 inches Seat depth Seat width Back height Armrest height footrest Measure from users posterior buttock, along the lateral thigh to the popliteal fold and SUBTRACT 2 inches. Measure the widest aspect of the user’s buttocks, hips or thighs and ADD ~2 inches. Measure from the seat of the chair to the floor of axilla with the user’s shoulder flexed to 90° and then SUBTRACT ~4 inches. This will allow the final back height to be below the inferior angles of the scapulae. *Consider seat cushion Measure from the seat of the chair to the olecranon process with the user’s elbow flexed to 90° and then add ~ 1 inch. *Consider seat cushion 16 inches 18 inches 16-16.5 inches 9 inches above the chair seat Device Walker: Can be used with all levels of weight bearing. Should allow 20-25° of elbow flexion. Ascending stairs The pt should place the walker on the opposite side of the handrail and turn the walker sideways. The pt should then grasp the handrail with one hand and the top of the walker’s handpiece with the other hand. Using the handrail and walker for stability, the pt takes a step up with in uninvolved extremity. The involved extremity is then advanced to the same step and the walker follows. Descending stairs The walker is positioned in a similar manner as described previously. The pt uses the handrail and top of the walker for stability while lowering the involved lower extremity. The uninvolved LE is then lowered and the walker follows. Axillary crutches: Can be used with all levels of weight bearing, however require higher level of coordination for use. Crutch height should be adjusted no greater than 3 finger widths from the axilla. Handgrip should be The pt should use the handrail and turn the crutch sideways. This will result in pt grasping the handrail and crutch with the same hand. Pt will advance with uninvolved extremity followed by involved. Pt lowers involved LE and the crutch to the next step followed by the uninvolved extremity. adjusted to the ulnar styloid process and allow for 20-25° elbow flexion. Cane: Provides minimal stability and support for pts during ambulation. A straight cane should not be utilized for pts that are partial weight bearing. Small base & large base quad canes proved a larger BOS & can better assist w limiting weight bearing. Cane is typically used on opposite side of an involved LE. The pt should use the handrail and turn the cane sideways. This will result in the pt grasping the handrail and the cane with the same hand. The pt should use the handrail and advance the uninvolved LE to the next step. The pt will then advance the involved LE. Pt lowers involved LE to next step followed by uninvolved LE. Orthotics: 1. Foot orthosis (FO)-may be attached to the interior of the shoe (inserted pad) or the exterior (Thomas heel). Soft inserts reduce areas of high loading, restrict forces, and protect painful or sensitive areas. Ex: Metatarsal pad-located posterior to MT heads; moves pressure from the heads to the shafts; allows more push-off in weak or inflexible feet. Ex. Cushion heel-cushions and absorbs forces at heel contact; used to relieve strain on plantar fascia in plantar fasciitis. Ex. Heel-spur pad. Longitudinal arch supports: prevent depression of the subtalar joint and correct for pes planus; flat foot can be flexible or rigid. Ex. Scaphoid pad-used to support the longitudinal arch. Ex. Thomas heel-a heel wedge with an extended anterior medial border used to support the longitudinal arch and correct for flexible pes valgus (pronated foot) Posting: Rearfoot posting-alters the position of the subtalar joint, or rearfoot, from heel strike to footflat. Must be dynamic, control but not eliminate joint motion. Ex. Varus post (medial wedge)-limits or controls eversion of the calcaneus and internal rotation of the tibia after heel strike. Reduces calcaneal eversion during running. Ex. Valgus post (lateral wedge)- controls the calcaneus and subtalar joint that are excessively inverted and supinated at heel strike. Forefoot posting: supports the forefoot Ex. Medial wedge prescribed for forefoot varus. Ex. Lateral wedge prescribed for forefoot valgus. Rocker bar-located proximal to MT heads; improves weight shift onto metatarsals. Rocker bottom-builds up the sole over the metatarsal heads and improves push-off in weak or inflexible feet, May also be used with insensitive feet. 2. Ankle-foot orthosis (AFO): consists of a shoe attachment, ankle control, uprights, and a proximal leg band. Ankle controls: 1. Free motion-provides mediiolateral stability that allows free motion in DF and PF. 2. Solid ankle-allows no movement; indicated with severe pain or instability. 3. Limited motion: allows motion to be restricted in one or both directions -Bichannel adjustable ankle lock (BiCALL)-an ankle joint with the anterior and posterior channels that can be fit with pins to reduce motion or springs to assist motion -Anterior stop (dorsiflexion stop)-determines the limits of ankle DF. If set to allow too much DF knee buckling could result. -Posterior stop (plantar flexion stop) determines the limits of ankle PF. If set for too much PF, knee recurvatum could result. -Solid AFO-limits all foot and ankle motion. *Molded AFO’s are contraindicated for individuals with changing leg volume. 3. Knee-ankle foot orthosis (KAFO)-consists of a shoe attachment, ankle control, uprights, knee control, and bands or shells for the calf and thigh. Craig-Scott knee-ankle-foot Orthosis-designed specifically for persons with paraplegia, This design allows a person to stand with a posterior lean of the trunk. 4.Hip-knee-ankle-foot orthosis( HKAFO)-indicated for pts with hip, foot, knee, and ankle weakness. It consist of bilateral knee-ankle-foot orthoses with an extension to the hip joints and a pelvic band, The orthosis can control rotation at the hip and abd/add. The orthosis is heavy and restricts pts to a swing-to or swing-through gait pattern. 5.Reciprocating gait orthosis (RGO)-is a derivative of the HKAFO and incorporates a cable system to assist with advancement of the Les during gait. When the pt shifts weight onto a selected LE, the cable system advances the opposite LE. The orthoses are used primarily for pts with paraplegia. Lower Limb Prosthetics Transtibial (below knee) prosthesis: Foot ankle assembly: Functions to- absorb shock at heel strike, plantarflex in early stance, permits metatarsophalangeal hyperextension in late stance, cosmetic replacement of foot. 1.Solid ankle cushion heel (SACH) foot-the most commonly prescribed foot; non-articulated; contains an energy-absorbing cushion heel and internal wooden keel that limits sagittal plane motion, primarily plantarflexion. Permits a very small amount of mediolateral and transverse plane motion. Assists in hyperextension of knee during stance. 2.Solid ankle flexible endoskeleton (SAFE) foot-nonarticulted foot, similar to SACH foot, prescribed for more active individuals. 3.Flex-foot-a leaf-spring shank (not a foot) used with an endoskeletal prosthesis, the long band of carbon fiber originates directly from the shank; Stores energy in early stance for later use during push-off; prescribed for more active individuals. 4.Single axis foot-an articulated foot with the lower shank; motion is controlled by anterior and posterior rubber bumpers that limited DF and PF; more stable (permits only sagittal plane motion); may be prescribed for individuals with bilateral transfemoral amputations. Sockets: 1.PTB (patellar tendon-bearing) socket- a total contact socket that allow for moderate loading area of the patellar tendon. Pressure-sensitive areas of the transtibial residual limb include: anterior tibia, anterior tibial crest, fibular head and neck, fibular nerve. Pressure-tolerant areas of the transtibial residual limb include: patellar tendon, medial tibial plateau, tibial and fibular shafts, distal end (rarely, may be sensitive) Transfemoral (above knee) prosthesis: 1.Single axis-permits knee motions to occur around a fixed axis, knee flexion is needed during late stance and swing, sitting, and kneeling. Pressure-sensitive areas of the typical transfemoral residual limb: distolateral end of the femur, pubic symphysis, perineal area. Pressure –tolerant areas of the typical transfemoral residual limb: ischial tuberosity, gluteals, lateral sides of residual limb, distal end (rarely, may be sensitive) Transfemoral gait deviations: 1.Circumduction-prostheis swings out to side in arc. Possible causes: a long prosthesis, locked knee, small or loose socket, inadequate suspension, foot plantar flexed, abduction contracture, poor knee control 2.Abducted gait-prosthesis is laterally displaced to the side. Possible causes: crotch or medial wall discomfort, long prosthesis, low lateral wall or malignment, tight hip abductors 3.Vaulting-pt rises up on the sound limb to swing the prosthesis through. Possible causes: prosthesis too long, inadequate suspension, socket too small, prosthetic foot set in too much plantarflexion, too little knee flexion 4.Lateral trunk bending during stance-trunk bends toward the prosthetic side. Possible causes: low lateral wall, short prosthesis, high medial wall, weak abductors, abductor contracture, hip pain, short amputation limb 5.Forward flexion during stance-trunk bends forward. Possible causes: unstable knee unit, short ambulatory aids, hip flexion contracture 6.Lumbar lordosis during stance-exaggeration of the lumbar curve. Possible causes: insufficient support from anterior or posterior walls, painful ischial weight bearing, hip flexion contracture, weak hip extensors or abdominals. 7.High heel rise-during early swing, the heel rises excessively. Possible causes: inadequate knee friction, too little tension in the extension aid 8.Terminal swing impact-the prosthesis comes to a sudden stop as the knee extends during lat swing. Possible causes: insufficient knee friction or too much tension in the extension aid; pt fears that the knee will buckle, forceful hip flexion. 9.Swing phase whips: at toe-off, the heel moves either medially or laterally. Possible causes; socket it rotated, knee bolt is rotated, foot is malaligned. *Whip termed by direction of heel. 10.Foot rotation at heel strike-as the heel contacts the ground, the foot rotates laterally, sometimes with vibratory motion. Possible causes: foot is malaligned, stiff heel cushion, or plantar flexion bumper. 11.Foot slap-excessive PF at heel strike. Possible causes: heel cushion or PF bumper is too soft. 12.Uneven step length-pt favors sound limb and limits weight-bearing time on the prosthetic limb. Possible causes: socket discomfort or poor alignment; hip flexion contracture or hip instability. Transtibial amputation: 1. Excessive knee flexion during stance. Possible causes: socket may be aligned too far forward or tilted anteriorly; plantar flexion bumper is too hard and limits plantar flexion; high heel shoes; knee flexion contracture or weak quads. 2. Inadequate knee flexion during stance. Possible causes: socket may be aligned too far back or tilited posteriorly; plantar flexion bumper or heel cushion too soft, how heel shoes; anterodistal discomfort, weak quads. 3. Lateral thrust at midstance. Possible causes: foot is inset too much 4. Medial thrust at midstance. Possible causes: foot is outset too much. 5. Drop off or premature knee flexion in late stance. Possible causes: socket is set too far forward or excessively flexed; dorsiflexion bumper is too soft, resulting in excess dorsiflexion of the foot; prosthetic foot keel too short; knee flexion contracture. 6. Delayed knee flexion during late stance: pt feels as though walking “uphill.” Possible causes: socket is set too far back or lacks sufficnet flexion; dorsiflexion bumper is too stiff causing excess plantar flexion; prosthetic foot keel too long. Safety and protection •Ergonomics - A therapist must consistently use proper body mechanics when treating patients and avoid unnecessary stress and starin by maintaining proper alignment within the musculo system. - Principles of proper body mechanics o Use the shortest lever arm possible o Stay close to the patient when possible o Use large muscles to perform heavy work o Maintain a wide base of support o Avoid any rotary movement when lifting o Attempt to maintain your center of gravity •Posture Awareness - Use plumb line as a tool to determine verticality. Although desirable, rarely will a given patient demonstrate ideal posture with all the anatomical landmarks. •Medical Equipment - Feeding devices o Nasogastric tube (NG tube)- short term liquid feeding and medication administration. o Gastric tube (G tube)- Inserted into a small incision in the abdomen, long term feeding. o Jejunostomy tube (J tube)- inserted into the jejunum, used for long term feeding. - Monitoring devices o Arterial line- used to measure blood pressure or to obtain blood samples. o Central Venous pressure Catheter- Measuring pressures in RA or superior vena cava o Indwelling right atrial catheter (hickman)- used for long-term administration of substance into the venous system. o Intracranial pressure monitor- measures the pressure exerted against the skull. Normal pressure: 90-180 mm H20 o Oximeter- used to determine the oxygen saturation of the blood o Pulmonary artery catheter (swan-ganz catheter)- used to provide continues pulmonary artery pressure. - Sterile Techniques o All items on the sterile field must be and remain sterile o Sterile gowns are only considered sterile in the front from the waist level upwards, including sleves. o Only the top surface of the table or sterile drape is considered sterile, outtter 1 inch is not. o Do not talk sneeze or cough. o Any item that positions or falls below waist level is considered contaminated. o Sterile filds should never be left alone •Emergency Preparedness - CPR o Compression comes first, then focus on airway and breathing. o No more look, listen, and feeling. Call 911 immediately o Push chest at least 2 inches down on adults o 100 compressions/min o Don’t stop pushing, no interruptions - First Aid o Use gloves when touching all body fluids o Change gloves between tasks o Wear mask/eye protection •Abuse Recognition - PT’s are mandated reporters of neglect and/or abuse of children, elders, and the disabled in all 50 states o Signs and symptoms of abuse/neglect Unexplained physical injuries Withdrawal Increased agitation Increased depression Malnutrition Substandard care of personal hygiene Professional Responsibilities Documentation: Legal requirements: Must comply with applicable jurisdictional requirements, all handwritten entries should be in ink, charting errors should be corrected by drawing a single line through the error and initialing and dating the chart, should include the referral method (direct access, seflreferral), should include indication of no shows and cancellations. Defensible documentation: Limit use of abbreviations, date and sign all entries, document legibly, report progress towards goals regularly, document at the time of the visit when possible, clearly identify note types (daily, progress), include all related communications, include missed or cancelled visits, demonstrate skilled care, demonstrate discharge planning through the episode of care. Patient Rights: HIPPA-Pt confidentiality is maintained in all oral, written, and electronic forms, physical identifabilitiy of pts must be reduced, charts and other documentation must be stored out of public view and secured, faxes must be sent with cover sheets, cover sheets should be used on clip boards t hat contain pts paperwork. An individual can access all of their medical records. Providers have 30-60 days to respond. a. Ethical Issues: i. Autonomy- requires the wishes of competent individuals must be honored. Autonomy is often referred to as self-determination ii. Beneficence- A moral obligation of heath care professionals to act for the benefit of others iii. Confidentiality- the holding of professional secrets or discussions keeping client information within appropriate limits iv. Duty- the obligation that individuals have to society v. Fidelity - Related to confidentiality and is defined as the moral duty to keep commitments that have been promised vi. Justice- The quality of being just of fair; righteousness vii. Nonmaleficience- the obligation of health care providers to above all else, do no harm. viii. Paternalism- A term used when someone fails to recognize another individuals rights to autonomy ix. Rights- The ability to take advantage of a moral entitlement to do something or not to do something x. Veracity- Obligation of heath care providers to tell the truth. b. Legal Term Definition Abandonment unacceptable one-sided termination of services by a health care professional without patient consent or agreement Administrative law administrative agencies at the federal and state level develop rules and regulations to supplement statutes and executive orders Common Law Refers to court decisions in the absence of statutory law often creates legal precedent in areas where statues have not been enacted. Constitutional law Involves law that is derived form the federal constitution. The US Supreme Court is responsible for ultimately interpreting and enforcing the Constitution Informed Consent- The patient is required to sign a document and given permission to the health care professional to render treatment. This should be obtained from the patient in accordance with the standards of practice prior to initiation of treatment. The patient has the right to full disclosure of treatment procedures, risks, expected outcomes, and goals. Malpractice The failure to exercise the skills that would normally be exercised by other members of the profession with similar skills and training. this can include areas of professional negligence, breach of contract issues, and intentional conduct by a health care professional Term Definition Negligence The failure to do what a reasonable and prudent person would ordinarily have done under the same or similar circumstances for a given situation. In order to prove negligence the plaintiff must prove all of the following: 1. THere was a duty owed to the plaintiff by the defendant 2. There was a breach of that duty under conditions that constituted negligence and the negligence was the proximate cause of the breach 3. there was damage to the plaintiff’s person or property Risk management The identification analysis and evaluation of risks and the selection of the most advantageous method for treating them Statutory law Congress and state legislatures are responsible for enacting status. Examples of federal statutes affecting health care include the Americans with Disabilities Act and the Family and Medical Leave Act Tort- A private or civil wrong or injury, involving omission and/or commission. Role of PTA: PTA is a technically educated health care provider who assists the PT in the provision of PT. The PT is directly responsible for the PTA s actions related to pt/client management. In general, the PT is not required to be on-site for direction and supervision but must be available at least by telecommunications. The PTA makes modifications to selected interventions either to progress the pt as directed by the PT or to ensure pt safety and comfort. Reimbursement Practices: Private health insurance companies: fee for service basis. Stock, mutual, and non-profit insurance companies. Government Health Insurance-uses private contractors to manage the payment process of each health plan. Medicare Part A: provides benefits for care provided in hospitals, outpatient diagnostic services, extended care facilities, hospice, and short term care at home required by an illness for which the pt is hospitalized. Enrollment is automatic and funding is through payroll taxes. Medicare Part B: provides benefits for outpatient care, physician services, and services ordered by physicians such as diagnostic tests, medical equipment, and supplies. Enrollment is voluntary and funding is through premiums paid by beneficiaries and general federal tax revenues. Medicaid provides basic medical services to the economically indigent population who qualify by reason of low income or who qualify for welfare or public assistance benefits in the state of their residence. IFC model-International Classification of Functioning, Disability and Health Model=Is a classification of health and health-related domains. PT Examination—Cardiopulmonary Great vessels of the heart: 1. Aorta-the body’s largest artery and the central conduit of blood from the heart to the body. The aorta begins at the upper part of the left ventricle, and after ascending for a short distance arches backward and to the left (arch of the aorta). It then descends within the thorax and passes into the abdominal cavity (abdominal aorta). 2. Superior vena cava-the vein that returns venous blood from the head, neck, and arms to the right atrium. 3. Inferior vena cava-the vein that returns venous blood from the lower body and viscera to the right atrium. 4. Pulmonary arteries-the arteries that carry deoxygenated blood from the right ventricle to the left and right lungs. 5. Pulmonary veins-the veins that carry oxygenated blood from the right and left lungs to the left atrium. Heart chambers and valves: •Superior chambers of the heart (right atrium and left atrium). The wall between the atria is the atrial septum. •The two inferior chambers of the heart are the right ventricle and left ventricle. The wall between the ventricles is the ventricular septum. •The right chambers collect blood from the body and pump it to the lungs. The left chambers collect blood from the lungs and pump it to the rest of the body. •The heart has 4 valves that function to maintain unidirectional blood flow. The atrioventricular valves (AV) are between the atria and ventricles and are named by the number of leaflets or cusps. The right AV valve or triscupid valve, has 3. It controls blood flow between the RA and RV. The left AV valve, or mitral valve has 2. It controls blood flow between the LV and aorta; the pulmonary valve is between the RV and pulmonary artery. •Venous blood from the superior and inferior vena cava enters the RA and is pumped through the triscuspid valve into the RV. The tricuspid valve closes while the RV contacts to pump blood through the pulmonary valve into the pulmonary trunk, which divides the right and left pulmonary arteries serving the right and left lungs, respectively. After picking up oxygen and releasing carbon dioxide in the pulmonary capillaries, oxygenated blood returns via the pulmonary veins to the LA. Contraction of the LA forces blood through the mitral valve into the LV. The mitral valve closes when the LV contracts to pump blood through the aortic valve into the aorta where it is distributed into the coronary circulation and systemic circulation. Cardiac Cycle: Atrial systole-the contraction of the right & left atria pushing blood into the ventricles. Atrial diastole-the period between atrial contactions when the atria are repolarizing. Ventricular systole-contraction of the right and left ventricles pushing blood into the pulmonary arteries and aorta. Ventricular diastole-the period between contractions when the ventricles are repolarizing. Stroke volume-the amount of blood ejected with each myocardial contraction; normal range is 55-100 ml/beat. Its influenced by: Left Ventricular end diastolic volume: the amount of blood left in the ventricle at the end of diastole, also known as preload. The greater the preload, the greater the quantity of blood pumped. Afterload-the force the LV must generate during systole to overcome aortic pressure to open the aortic valve. Cardiac Output-the amount of blood discharged from the left or right ventricle per minute. Normal range is 4-5L. Determined by measuring HR x SV. Ejection fraction-percentage of blood empties from the ventricle during systole; a clinically useful measure of LV function. Normal averages >55%. *Diastolic filling time decreases with increased HR and with heart disease. Heart Sounds: S1 sound (“lub”)-normal closure of mitral and triscupid valves; marks beginning of systole. High frequency sound with lower pitch and longer duration than S2. Decreased in 1st degree heart block. S2 sound (“dub”)-normal closure of aortic and pulmonary valves, marks end of systole. High frequency sound with higher pitch and shorter duration than S1. Decreased in aortic stenosis. Extra sounds: Murmurs 1. Systolic-falls between S1 and S2. May indicated valvular disease or may be normal. 2. Diastolic-falls between S2 and S1. Usually indicates valvular disease. 3. Thrill-an abnormal tremor accompanying a vascular or cardiac murmur, felt on palpation. Bruit-adventitous sound or murmur (blowing sound) of arterial or venous origin, common in carotid or femoral arteries; indicative of atherosclerosis. Gallop rhythm-an abnormal heart rhythm with three sounds in each cycle; resembles the gallop of a horse. 1. S3; vibrations of the distended ventricle walls due to passive flow of blood from the atria during the rapid filling phase of diastole. Normal in healthy young children, abnormal in adults, may be associated with heart failure. “ventricular gallop” 2. S4; pathological sound of vibration of the ventricular wall with ventricular filling and atrial contraction. May be associated with HTN, stenosis, MI. “atrial gallop” Auscultation of heart sounds Procedure: The bell or diaphragm of the stethoscope is held directly on the pts bare skin with enough pressure to provide a skin seal while the pt breathes quietly through the nose. Listen over four designated auscultatory areas: Aortic area-2nd intercostal space at the right sternal border Pulmonic area-2nd intercostal spaceat the left sternal border Mitral valve-5th intercostal space, medial to the left midclaviciular line Triscupid area-4th intercostal space at the left sternal border Picture on page 264 of scorebuilders. Examine heart rhythm: A 12 lead EKG provides 12 views of the heart. It is used to assess cardiac rhythm, to diagnose the location, extent, and acuteness of myocardial ischemia and infarction, and to evaluate changes with activity. Waveforms and Intervals: 1. 2. 3. 4. P wave-atrial depolarization PR interval-time for atrial depolarization and conduction from the SA node to the AV node. Normal duration is 0.12 to .20 seconds. QRS complex-Ventricular depolarization and atrial repolarization. Normal duration is 0.06 to 0.10 seconds. QT interval-Time for both ventricular depolarization and repolarization. Normally ranges from .20 to 0.40 seconds, depending on heart rate. 5. ST segment-isoelectric period following QRS when the ventricles are depolarized. 6. T wave-ventricular repolarization Sinus Node Rhythms: 1. Normal sinus rhythm-atrial depolarization begins in the SA node and spreads normally throughout the electrical conduction system with a HR between 60-100 bpm. 2. Sinus bradycardia-sinus rhythm with a HR less than 60 bpm (in adults) 3. Sinus tachycardia-sinus rhythm with a HR more than 100 bpm. 4. Sinus arrhythmia-a sinus rhythm, but with quickening and slowing of impulse formation in the SA node resulting in a slight beat-to-beat variation of the rate. 5. Sinus arrest-a sinus rhythm, except with intermittent failure of the either the SA node impulse formation or AV node conduction that results in the occasional complete absence of P or QRS waves. Atrial dysrhythmias: Condition: Premature atrial contractions (PAC)- occur when an ectopic focus in the atrium initiates an impulse before the SA node. Clinical significance: PACs are very common and generally benign, but may progress to atrial flutter, tachycardia or fibrillation. May occur with a normal HR (from caffeine, stress, smoking, alcohol) and any type of heart disease EKG reading The p wave is premature with abnormal configuration. Atrial flutter-An ectopic, very rapid atrial tachycardia. Atrial rate of 250-350 bpm; ventricular rate dependent upon AV node conduction. Occurs with valvular disease (especially mitral), ischemic heart disease, cardiomyopathy, hypertension, acute myocardial infarction, chronic obstructive lung disease, and pulmonary emboli. Signs and symptoms include palpitations, lightheadedness, and angina due to a rapid rate. Stagnation of blood may predispose to thrombi in the atria Occurs in healthy hearts and in pts with coronary artery disease, hypertension, and valvular disease. Symptoms may include palpitations, fatigue, dyspnea, lightheadedness, syncope, and chest pain. Stagnation of blood may predispose to thrombi in the atria. Saw-tooth shaped P waves (also known as flutter waves) are characteristic. Atrial fibrillation-a common arrhythmia where the atria are depolarized between 350 and 600 times a min. EKG shows characteristically irregular undulations of EKG baseline without discrete P waves. Ventricular arrhythmias: Condition: Premature ventricular complex (PVC)premature depolarization arising the in ventricles due to an ectopic focus. Unifocal Clinical significance: A common arrhythmia that occurs in healthy and diseased hearts. Pt may be asymptomatic or have palpitations. Common causes include EKG reading: On EKG, the P wave is usually absent and the QRS complex has a wide and aberrant shape. PVCs arise from the same ectopic focus and have the same configuration. Multifocal PVCs arise from different ectopic foci and have different configurations. Bigeminy-normal sinus impulse is followed by a PVC. Trigeminey-PVC occurs after every two normal sinus impulses. anxiety, caffeine, stress, smoking, and all forms of heart disease. Ventricular tachycardia (v-tach)-3 or more consecutive PVCs at a ventricular rate of >150 bpm. V-tach longer than 30 seconds is a life threatening arrhythmia and requires immediate medical intervention. Pts are not able to maintain an adequate blood pressure and eventually become hypotensive. V-tach may degenerate into ventricular fibrillation causing cardiac arrest. Common causes include MI, cardiomyopathy, and valvular disease. P waves are absent and QRS complexes are wide and aberrant in appearance. Ventricular fibrillation (v-fib)-Ventricles do not beat in a coordinated fashion, but fibrillate or quiver asynchronously and ineffectively. No cardiac output; pt becomes unconscious. A lethal tachyarrhythmia requires immediate defibrillation. Additional measures include medications to support the circulation and intravenous antiarrythmic agents. Common causes include heart disease of any type, MI, and cocaine use. EKG shows characteristic fibrillatory waves with an irregular pattern that is either coarse or fine. Ventricular asystole-Ventricular standstill with no rhythm. Requires immediate defibrillation and/or medications to stimulate cardiac activity. Common causes include acute MI, ventricular rupture, cocaine use, lightning strikes, and electrical shock. EKG records a straight-line pattern. AV Conduction Blocks: 1st degree AV block: PR interval is longer than 0.2 seconds, but relatively constant from beat to beat. •Clinical significance: No symptoms or significant change in cardiac function. PR interval may become prolonged for many reasons include medications that suppress AV conduction. 2nd degree AV block: AV conduction disturbance in which impulses between the atria and ventricles fail intermittently. Two major types: Mobitz type 1 block (also called Wenckebach block) and Mobitz type 2 block •Clinical significance: Mobitz I-progressive prolongation of PR interval until one impulse is not conducted (generally benign) Mobitz II-consecutive PR intervals are the same and normal followed by nonconduction of one or more impulses (a more serious condition). If heart rate is slow, cardiac output will decrease with the blocked impulse. Also, 2nd degree AV block may progress to 3rd degree AV block 3rd Degree AV block (complete heart block)-All impulses are blocked at the AV node and none are transmitted to the ventricles. The atria and ventricles are paced independently; atrial rate > ventricular rate. •Clinical significance: Considered a medical emergency requiring a pacemaker. If the ventricular rate is too slow, the cardiac output drops and the pt may faint. Common causes include degenerative changes of the conduction systems, digitalis, heart surgery, and acute MI. Signs and Symptoms Right Sided Heart Failure Nausea anorexia weight gain ascites right upper quadrant pain. Increase in RAP, CVP, Jugular venous distention Positive heptojugular reflex right ventricular eave Murmur of tricuspid insufficiency Hepatomegaly Peripheral edema Signs and Symptoms Left Sided Heart Failure Fatigue cough shortness of breath DOE Orthopnea PND Diaphoresis Tachycardia S3 Gallop Crackles Increased PAP, PAWP, SVR Laterally displaced PIM Left ventricular heave Pulsus alternans confussion decreased urine output Cheyne Stokes respiration (advanced failure) Murmur of mitral insufficiency Tests of peripheral arterial circulation: Ankle brachial index (ABI)-the ratio of lower extremity pressure divided by upper extremity pressure. -Performed in UE at brachial artery, LE at posterior tibial and dorsalis pedis arteries. ABI assists in risk stratification for cardiovascular disease: <0.90 is associated with 2-4 fold increased risk for cardiovascular events and death. ABI < 0.50: increased risk of progression to severe or critical limb ischemia in 1 year. >1.40 Indicates non-compliant arteries 1.00-1.40 Normal 0.91-0.99 Borderline < or equal to 0.90 <or equal to 0.50 Abnormal Severe arterial diease, risk for critical limb ischemia, may have pain at rest Exercise Stress/Tolerance Testing: -Serves as a basis for exercise prescription, used as a screening measure for CAD in asymptomatic individuals. -A pharmacological stress test is used when a patient is unable to perform a regular ETT. Testing modes: Treadmill and cycle ergometry (leg or arm tests), step test. Maximal ETT: defined by target endpoint HR. Should only be completed in settings with advanced cardiac life support. -Age predicted maximum heart rate: 220-age -Heart rate range (Karvonenen’s): 60%-80% (HR max-resting HR) + resting HR=target HR Submaximal ETT: Symptom limited or terminated at 85% of age predicted HR max; safe in all settings Continuous ETT: workload is steadily progressed; step test allowing pt reach steady state, ramp test-pt is not permitted to reach steady state. Absolute indications for terminating an exercise test: 1. 2. 3. 4. 5. 6. Drop in SBP>10 mm Hg from baseline despite increase in workload with other evidence of ischemia Moderately sever angina (three on a scale of four) Increasing nervous system symptoms (ataxia, dizziness) Signs of poor perfusion (cynaosis, pallor) Sustained ventricular tachycardia 1.0 mm ST elevation in leads without diagnostic Q waves Pulmonary Anatomy: Muscles of inspiration: diaphragm (primary), external intercostals, and internal intercostals and considered principal muscles of inspiration. Accessory muscles of inspiration: sternocleidomastoid, scalenes, pec major & minor, and serratus anterior. Muscles of exhalation: results from passive recoil of the lungs and rib cage. During forceful breathing the rectus abdominus, external oblique, internal oblique, and transverse abdominus depress the lower ribs and compress the abdominal contents, thus pushing up the diaphragm and assisting with active exhalation. Alveolar-capillary units-The bronchi branch many times before terminating in the acinus or respiratory unit of the lung. Oxygen diffuses across the alveolar-capillary septum into the red blood cells in the lung capillaries where it combines with hemoglobin to be transported back to the heart. Carbon dioxide diffuses in the opposite direction. Pleurae-a membranous serous sac called visceral pleura covers each lung. The pleura covering the surface of the lungs is called the visceral pleura. The pleural tissue covering the inner surfaces of the chest wall, ribs, vertebrae, diaphragm, and mediastinum is called parietal pleura. Normally, the two pleurae remain in contact throughout the respiratory cycle, separated only by serous fluid. Under abnormal circumstances, the pleural space may contain air (pneumothorax) blood (hemothorax), pus or increased amounts of serous fluid, which compress the lung and cause respiratory distress. Pulmonary circulation- the portion of the circulatory system that carries deoxygenated blood from the heart to the lungs via the pulmonary arterial trunk, right and left pulmonary arteries, lobar arteries, arterioles, and capillaries. The pulmonary circulation returns oxygenated blood from the lungs to the left atrium via the pulmonary veins. Bronchial circulation-the portion of the circulatory system that supplies oxygenated blood to the bronchi and connective tissue of the lungs via the bronchial arteries, which drain directly into the bronchial veins. Lung Volumes & Capacities: Anatomic dead space volume (VD) Expiratory reserve volume (ERV) Forced expiratory volume (FEV) Forced vital capacity (FVC) Functional residual capacity (FRC) Inspiratory capacity (IC) Inspiratory reserve volume (IRV) The volume of air that occupies the non-respiratory conducing airways The maximal volume of air that be exhaled after a normal tidal exhalation. ERV is approximately 15% of total lung volume. The maximal volume of air exhaled in a specified period of time: usually the 1st, 2nd and 3rd second of a forced vital capacity maneuver. The volume of air expired during a forced maximal expiration after a forced maximal inspiration. The volume of air in the lungs after normal exhalation. FRC=ERV + RV. FRC is approximately 40% of total lung volume. The maximal volume of air that can be inspired after a normal tidal exhalation. IC=TV + IRV. IC is approximately 60% of total lung volume. The maximal volume of air that can be inspired after normal tidal Minute volume ventilation (VE) Peak expiratory flow (PEF) Residual volume (RV) Tidal volume (TV) Total lung capacity (TLC) Vital capacity (VC) volume inspiration. IRV is approximately 50% of total lung volume. The volume of air expired in one minute. VE=TV x respiratory rate. The maximum flow of air during the beginning of a forced expiratory maneuver. The volume of gas remaining in the lungs at the end of a maximal expiration. RV is approximately 25% of total lung volume. Total volume inspired and expired with each breath during quiet breathing. TV is approximately 10% of total lung volume. (500ml) The volume of air in the lungs after a maximal inspiration; the sum of all lung volumes. TLC=RV + VC or TLC= FRC + IC The volume change that occurs between maximal inspiration and maximal expiration. VC= TV + IRV + ERV. VC is ~75% of total lung volume. Normal breath sounds: Tracheal & bronchial sounds-Loud, tubular sounds normally heard over the trachea. Inspiratory phase is shorter than the expiratory phase and there is a slight pause between them. Vesicular breath sounds-High pitched, breezy sounds normally heard over the distal airways in healthy lung tissue. Inspiratory phase is longer than expiratory phase and there is no pause between them. Adventitous breath sounds: Crackles (also termed rales, crepitations): a crackling sound heard usually during inspiration that indicates pathology) atelectasis, fibrosis, pulmonary edema) Wheezes: a musically pitched sound, usually heard during expiration, caused by airway obstruction (asthma, COPD, foreign body aspiration) Lung Lobe Location & Postural Drainage Position Lobe Position Right or Left Anterior Upper Lobe/Segment Supine in a reclined seated position with knees supported Right or Left Posterior Apical Segment Seated and slumped over a pillow with lower extremities supported in a comfortable position Right and Left Anterior Segments Supine with knees supported with a pillow Right Posterior Segment Prone slightly on the left side Left Posterior segment Prone with left side of torso propped up on pillows. Torso is at a 45 degree angle. Right Middle Lobe Supine with right side propped up on pillows and lower extremities elevated 12 inches Left Ingular Supine with left side propped up on pillows and lower extremities elevated 12 inches Anterior Segments (Lower Lobes) Supine with knees supported with pillows and lower extremities elevated 18 inches Right Lateral Segment Left sidelying with lower extremities elevated 18 inches Left Lateral Segments Right sidelying with lower extremities elevated 18 inches Posterior segments Prone in comfortable position/neutral spine with pillows under abdomen and comfortable feet position with pillows under lower legs with lower extremities elevated 18 inches Superior Segments Prone in comfortable position/neutral spine with pillows under abdomen and comfortable feet position with pillows under lower legs. Arterial blood gases: pH 7.4 (7.35-7.45) PaCO2 (amount of carbon dioxide within arterial blood) 40 mm Hg at sea level breathing ambient air (35-45mm Hg) PaO2 97 mm Hg at sea level breathing ambient air (80-100 mm Hg) HCO3- (amount of bicarbonate ions within arterial blood) 24 mEq/L (22-26) SaO2 95-98% *By convention, ABG results are written or spoken in the following order: pHPaCO2PaO2HCO3- (e.g. 7.4/40/97/24) Acidemia Elevated acidity of blood (pH < 7.35) Alkalemia Decreased acidity of blood (pH > 7.45) Eucapnia Normal level of CO2 in arterial blood (35-45 mm Hg) Hypercapnia Elevated level of CO2 in arterial blood( > 45 mm Hg) Hyopcapnia Low level of CO2 in arterial blood (<35 mm Hg) Hypoxemia Low level of O2 in arterial blood (PaO2 < 80 mm Hg) Mild hypoxemia PaO2 60-79 mmHg Moderate hypoxemia PaO2 40-59 mmHg Severe hypoxemia PaO2 < 40 mmHg Hypoxia Low level of O2 in the tissue despite adequate perfusion of the tissue *An increase in the PaCO2 decreases the body’s pH. A decrease in the PaCO2 raises the body’s pH. *Supplemental oxygen is usually prescribed when the PaO2 falls below 55 mmHg. Other values: White Blood Cells (WBCs) Red Blood Cells (RBCs) Erethrosedimentation Rate (ESR) Hematocrit Platelet 4300-10,800 Male: 4.6-6.2 Female: 4.2-5.9 Male: <15 mm/hr Female: <20 Male: 45%-52% Female: 37%-48% 150,000-450,000 Sodium Calcium Potassium Magnesium Total cholesterol LDL HDL Triglyceride 135-146 8.4-10.4 3.5-5.5 1.8-2.4 <200 <100 <40 <150 Acid-Base balance Type Respiratory alkalosis pH PaCO2 HCO3- Causes Alveolar hyperventilation ↑ ↓ WML Respiratory acidosis ↓ ↑ WNL Alveolar hypoventilation Metabolic alkalosis ↑ WNL ↑ Metabolic acidosis ↓ WNL ↓ Bicarbonate ingestion, vomiting, diuretics, steroids, adrenal disease Diabetic, lactic, or uremic acidosis, prolonged diarrhea Signs & Symptoms Dizziness, syncope, tingling, numbness, early tetany Early: anxiety, restlessness, dyspnea, headache Late: confusion, somnolence, coma Vague symptoms: weakness, mental dullness, possibly early tetany Secondary hyperventilation (Kussmaul breathing), nausea, lethargy, coma Common Disorders/Pathology of the Cardiopulmonary System: Pathology Aneurysm What is it A localized abnormal dilation of a blood vessel, usually an artery. Common sites include the thoracic & abdominal aorta and vessels within the brain. Etiology Congenital defect; weakness in the wall of vessel often due to chronic HTN, connective tissue disease (Marfan Syndrome), trauma, infection Angina pectoris A transient precordial sensation of pressure or discomfit resulting from myocardial ischemia. Common types of angina pectoris are : Stable (occurs at predictable level of exertion, responds to rest or nitroglycerin) Unstable (usually is more intense, lasts longer, is precipitated by less exertion, occurs spontaneously at rest, is progressive) Prinzmetal or Inadequate blood flow & oxygenation of the heart muscle mostly due to coronary artery disease. Signs & Symptoms Variable based on the site. Aortic aneurysms are usually asymptomatic, but may include generalized abdominal or LBP. Abdominal aortic aneurysms may cause pulsations near the navel. A cerebral aneurysm can cause a sudden and severe headache, nausea & vomiting, stiff neck, seizure, loss of consciousness, & double vision. Usually described as pressure, heaviness, fullness, squeezing, burning or aching behind the sternum, but may also be felt in the neck and back, jaw, shoulders, and arms. The sensation may be associated with difficulty breathing, nausea or vomiting, sweating, anxiety, or fear. It is typically triggered by exertion or strong emotion and subsides with rest. Treatment Antihypertensive medications may be recommended for HTN. Surgery is recommended to repair large aortic aneurysms and consists of replacing the aneurysm with a synthetic fabric graft. Two surgical options for ruptured brain aneurysms are surgical clipping & endovascular coiling. Tx for acute angina include supplemental oxygen, nitroglycerin, and rest. Chronic or recurring angina pectoris is treated with long-acting nitrates, beta blockers, and calcium channel blockers. Angioplasty with stenting of the coronary arteries or coronary artery bypass surgery (CABG) may be performed when medications are not effective. Atherosclerosis variant angina (occurs due to coronary artery spasm most often associated with coronary artery disease) A slow progressive accumulation of fatty plaques on the inner walls of arteries. Over time the plaque can restrict blood flow, causing a blood clot. Although the exact cause is unknown, the process may begin with damage or injury to the inner wall of the artery from HTN, high cholesterorl, smoking or diabetes. Over time, fatty plaques made of cholesterorl and other cellular waste products build up at the site of the injury & harden, narrowing the artery and impacting blood flow. Chronic venous insufficiency (CVI) A condition in which the veins and valves in the LE are damaged and cannot keep blood flowing toward the heart. This causes veins to remain filled with blood. Weak or damaged valves inside the veins. Risk factors include age, female gender, obesity, pregnancy, and prolonged sitting or standing. Atrial septal defect (ASD) A hole in the wall of heart separating the right & left atria. In fetal circulation, there is normally an opening between the two Congenital heart defects arise from errors early in the heart’s development. Genetics & environmental factors may play a role. Varies based on the severity of disease & the artery affected. When the coronary arteries are affected, angina pectoris may result. When cerebral arteries are affected, numbness or weakness of the arms or legs, difficulty speaking or slurred speech, or drooping face muscles may result. When peripheral arteries are affected, intermittent claudication may result. Leg swelling, varicose veins, aching, heaviness or cramping, itching, redness or skin ulcers of the legs and ankles. Small to moderate sized defects may produce no symptoms or symptoms that appear after 30 years of age. Large or long Lifestyle changes, medications, & surgery. Changes include cessation of smoking, regular exercise, healthy diet, stress management. Medications may include antihypertensive, antiplatelet, and antilipidemic agents. Surgical procedures may include angioplasty, endarterectomy, and bypass surgery. Compression stockings and elevation of the legs help decrease chronic swelling. Varicose vein stripping may be performed for cases with persistent leg pain or skin ulcers due to poor circulation. Surgical closure is recommended if the defect is large, the heart is swollen or symptoms occur. A non-surgical Cor Pulmonale Coronary Artery Disease (CAD) atria to allow blood to bypass the lungs. This opening is termed foramen ovale and usually closes at birth. If the ASD persists, blood continues to flow from left to the right atria and is called a shunt. In severe cases, blood may flow from the right to the left atria. Also known as pulmonary heart disease, refers to hypertrophy of the right ventricle cased by altered structure or function of the lungs. Is the narrowing or blockage of the coronary arteries due to atheromatous plaques resulting in diminished blood flow. Pulmonary hypertension from chronically increased resistance in the pulmonary circulation CAD is thought to begin with damage or injury to the inner layer of a coronary artery. Cholesterol then tends to accumulate at the site. If a plaque ruptures, platelets will clump at the site to try to repair the artery. This clump can block the artery, leading to a heart attack. standing atrial septal defects may cause: heart murmur, SOB, fatigue, swelling of the legs, heart palpitations, frequent lung infections, stroke, cyanosis of the skin. procedure involves placing a device into the heart and across the ASD using a catheter. The cardinal symptom is progressive shortness of breath, especially with exertion. Other signs & symptoms are fatigue, palpitations, atypical chest pain, swelling of the Legs, dizziness, & syncope. The degree of stenosis required to produce signs & symptoms varies with the oxygen demand. The diminished blood flow may cause angina, shortness of breath or other symptoms, which may not be felt until >70% of the lumen is occluded. A complete blockage can cause a heart attack. Supplemental oxygen sufficient to maintain SaO2 >90% and or PaO2 >60 mm Hg. General measures include diuretics & anticoagulation. Aggressive modification of atherosclerosis risk factors to slow progression and induce regression of existing plaques and restore or improve coronary blood flow. This includes smoking cessation; weight loss; a heart healthy diet low in saturated fat, cholesterol and sodium; regular exercise. Drug therapy includes antiplatelet agents (aspirin, Deep Vein thrombosis (DVT) A condition in which a blood clot forms in one or more of the deep veins, usually in the lower extremities. DVT is a serious condition because the clot can break loose and travel to the lungs, resulting in a pulmonary embolism. Any condition that impairs normal circulation or normal blood clotting. Many factors increase the risk of a DVT including prolonged sitting or bed rest, inherited blood clotting disorders, injury or surgery of the veins, pregnancy, cancer, birth control or hormone replacement therapy, being overweight, obesity, and smoking. About 50% of DVT cases are asymptomatic. When signs & symptoms occur they can include swelling, pain, redness, and warmth in the affected leg. Endocarditis Is inflammation of the endothelium that lines the heart and cardiac valves. If left untreated, endocarditis can damage and destroy heart valves and become life threatening. May develop slowly, depending on the cause of the infection and if the heart is affected, but can include fever, chills, heart murmur, fatigue, shortness of breath, weight loss, blood in urine, and skin petechiae. Heart Failure “congestive heart failure” Is a progressive condition in which the heart cannot maintain a normal cardiac Caused by bacteria that may enter the blood from catheters or needles, dental procedures, gum disease, sexually transmitted disease or inflammatory bowel disease. Individuals with a damaged heart valve, and artificial heart valve or other heart defects are at the greatest risk. CAD, HTN, DM, MI, abnormal heart valves, and cardiomyopathy. SOB, fatigue and weakness, swelling in the legs, feet and abdomen, Clopidogel), ACE inhibitors, angiotensin II receptor blockers and statins. The goal of tx is to prevent the blood clot from getting bigger and to prevent it form breaking loose and causing a pulmonary embolism. Medications include anticoagulant and thrombolytic agents. “Filters” may be surgically inserted into the vena cave to prevent clots from reaching the lungs. Compression stockings may be recommended to reduce blood pooling. Antibiotics are the first line of treatment. Surgery may be needed to treat persistent infections or replace a damaged heart valve. Sometimes treating the underlying cause can correct heart failure Heart murmur output to meet the body’s demands for blood and oxygen. Heart failure often develops after other conditions have damanged or weakened the heart. The ventricles weaken and dilate to the point that the heart can’t pump efficiently. It can affect the right side, left side, or both sides of the heart, but typically begins with the left ventricle. The term “congestive heart failure” comes from blood backing up into the liver, abdomen, legs, and lungs. The condition can be acute or chronic. An abnormal swishing or whooshing sound heard by auscultation sometime during the cardiac cycle. Innocent heart murmurs occur when blood flows rapidly through the heart due to activity, pregnancy, fever, and anemia. Abnormal heart murmurs may be caused by turbulent blood flow through a damaged or narrowed heart valve or a hole in one of the heart’s walls. Other causes include rheumatic fever, endocarditis, calcified rapid or irregular heartbeat with S3 or S4 heart sound, persistent cough or wheezing and weight gain from fluid retention. (repairing a damaged heart valve or controlling an abnormal heart rhythm). In most cases, tx is a balance of medications, devices, and lifestyle changes to help the heart contract normally. Medications include anticoagulants, antihypertensives, and digitalis to increase the strength of contraction. In severe cases, surgery and medical devices may be needed to correct the underlying cause of the heart failure. Innocent murmurs are not usually associated with other signs or symptoms. Abnormal murmurs may be associated with cyanosis, limb edema, shortness of breath, enlarged neck veins, weight gain, chest pain, dizziness, and fainting. Innocent murmurs usually do not require treatment. Treatment for abnormal heart murmurs depends on the underlying cause and can include medications or surgery. Common medications are: digoxin, anticoagulants, diuretics, and other antihyperstensive agents. Surgical procedures include valve replacement or patching atrial or valves, and mitral valve prolapsed. Primary or essential hypertension has no known cause. HTN with an identified cause (usually renal disease) is called secondary HTN. ventricular septal defects. Hypertension Arterial hypertension in adults is a sustained elevation of systolic pressure >140 mm Hg or diastolic pressure >90 mm Hg. HTN is often asymptomatic until complications develop in the organs. An S4 heart sound is an early sign. Severe HTN (diastolic >120) can cause significant CNS symptoms (confusion, cortical blindness, hemiapresis, seizures) cardiovascular symptoms (chest pain, dyspena) and renal involvement. Lymphedema Edema, or swelling, due to an accumulation of lymph in the extremities Primary lymphedema is a rare, inherited condition caused by problems with the development of lymph vessels. Causes of secondary lymphedema include any condition or procedure that damages or obstructs lymph nodes or vessels Swelling with the restricted motion of the upper or lower extremity, arching and heaviness or a felling of fullness, brawny, fibrous, non pitting edema in one or more limbs. Myocardial Infarction AKA heart attack, a MI occurs when the blood Most occur when a ruptured atherosclerotic Chest discomfort with pressure, squeezing or Recommendations include lifestyle modifications (30 min/day exercise, weight loss to a BMI of 18.5-24, smoking cessation, reduced intake of sodium and alcohol, increased consumption of fruits, vegetables, low fat dairy and medications. Classes of medications for HTN include diuretics, beta blockers, calcium channel blockers, ACE inhibitors. There is no cure, but treatments focused on reducing swelling and controlling pain may lessen symptoms and slow or halt progression. Treatments include: gentle active exercise, pressure gradient bandages, massage, pneumatic compression, and compression garments. Surgery to remove excess tissue in the affected extremity may be considered. Treatment of MI varies from medication to Peripheral arterial disease flow through one or more of the coronary arteries is severely reduced or cut off completely. This causes irreversible necrosis to the portion of myocardium supplied by the blocked artery. plaque or blood clot blocks the flow of blood through a coronary artery. An uncommon cause is a spasm of a coronary artery pain, shortness of breath, discomfort in the upper body including the arms, shoulder, neck or back, nausea, vomiting, dizziness, sweating, and palpitations. Stenotic, occlusive, and aneurismal diseases of the aorta and peripheral arteries. Caused primarily by atherosclerosis and thromboemboic processes that alter the structure and function of the aorta and its branches Fatigue, aching, numbness, or pain primarily in the buttock, thigh, calf, or foot at rest or when walking, poorly healing wounds of the legs or feet, distal hair loss, trophic skin changes, and hypertrophic nails. surgery or both, depending on the severity and the amount of heart damage. Medications used to treat the acute MI include anticoagulants and thrombolytic agents, pain relievers, antihypertensives and cholesterol lowering medications. Surgical procedures may include coronary angioplasty with stenting or bypass surgery. Recommended lifestyle changes. For pts with asymptomatic disease, tx consist of smoking cessation, lipid lowering medications, and control of diabetes and HTN (with beta blockers). For pts with disabling intermittent claudication, treatment consists of revascularization procedures (stent, lasers) and surgery (bypass) may be recommended. Supervised exercise training should be performed for a minimum of 30-45 minutes, at least 3x a week, for a minimum of 12 weeks. Rheumatic Fever Acute respiratory distress syndrome (ARDS) Atelectasis An inflammatory disease that can develop as a complication of untreated or poorly treated strep throat from group A streptococcus bacteria. Rheumatic fever can damage the heart valves and cause heart failure. Is a sudden respiratory failure due to fluid accumulation in the alveoli. ARDS usually occurs in people who are already critically ill or who have significant injuries. Severe shortness of breath develops within a few hours to a few days after the original disease or trauma. ARDS is fatal in 25-40% of the people who develop it. Streptococus pyogenes or group A strep that cause strep throat or scarlet fever. A condition in which one or more areas of the lungs collapse or do not inflate properly Conditions and factors that prevent deep breathing and coughing can cause it. These include Mechanical cause is from fluid leaking from the smallest blood vessels in the lungs into the alveoli. Injuries include: severe viral or bacterial pneumonia, heart failure, serious head or chest injury, fxs, smoke inhalation, near drowning, prolonged use of large volumes of supplemental oxygen, drug overdose, shock. Result from the inflammation of the heart, joints, skin or central nervous system that may include red, swollen, fever, and painful joints, heart palpitations, chest pain, shortness of breath, and skin rash. Varies based on the cause. Usually include SOB, labored and unusually rapid breathing, hypotension, confusion, extreme fatigue, cough, and fever. If a small area of the lung is affected, there may be no signs or symptoms. If a large area is affected, The goals of treatment are to destroy group A strep bacteria, relieve symptoms, and control inflammation. Medications include antibiotics and anti-inflammatory agents. It is important to identify the cause of ARDS bc it can determine treatment and predict the chances for survival. The first goal of treatment is to get oxygen to the lungs and organs. Most people will be treated with supplemental oxygen and mechanical ventilation. Treating the underlying condition then becomes equally important. Medications are given to prevent and treat infection, relieve pain, provide sedation, and prevent blood clot formation. Deep breathing, changing positions, and airway clearance techniques assist to fully expand the Lung cancer (bronchial carcinoma) Bronchiectasis Refers to any epithelias carcinoma occurring in the bronchopulmonary tree. Cancers are broadly divided into two main groups: small cell lung carcinomas and non-small cell lung carcinomas, including squamous cell carcinoma, adenocarcinoma, and large cell carcinoma A progressive obstructive lung disease that produces abnormal dilation of a bronchus. This is an irreversible condition usually associated with chronic infections, aspiration, cystic fibrosis or immune system impairment. The bronchial walls weaken over time due to infection and allow for permanent dilation of bronchi and bronchioles. post operataive pain, pleural effusion, tumor, ARDS, asthma, COPD, and cystic fibrosis. there may be cyanosis, shortness of breath, increased breathing rate, and increased HR. Smoking is the primary cause of the majority of lung cancers, but it can occur in people who have never smoked or had prolonged exposure to secondhand smoke. In these cases, the exact etiology may be unknown. A new cough or changes in a chronic cough, coughing up blood, shortness of breath, wheezing, weight loss, and bone pain. Typically, signs & symptoms are not present until the disease is advanced. Injury to the airways or lung infection (pneumonia, whooping cough, measles, tuberculosis, fungal infections). Consistent productive cough, hemoptysis, weight loss, anemia, crackles, wheezes, and loud breath sounds. lungs. Supplemental oxygen, nebulized bronchodilators, and mucolytic agents. Bronchoscopy may be used to remove foreign objects or mucous plugs blocking the airways. Surgery (wedge resection, segmental resection, lobectomy, pneumonectomy, chemotherapy, and radiation therapy. Medications include antibiotics, bronchodilators, expectorants, and mucolytics. Chronic Obstructive Pulmonary Disease Cystic fibrosis Emphysema Refers to a group of lung diseases that block airflow due to narrowing of the bronchial tree. Emphysema and chronic bronchitis are the two main conditions that make up COPD. Pts have an increased total lung capacity with a significant increase in residual volume. Is an autosomal recessive genetic disease of the exocrine glands that primarily affects the lungs, pancrease, liver, intestines, sinusues, and sex organs. People who have CF inherit two faulty CF genes, one from each parent. The alveolar walls are gradually destroyed and the alveoli are turned into large, irregular pockets with gaping holes in the walls. In addition, the elastic fibers that hold open the bronchioles are Caused by long term smoking Excessive mucus production, chronic productive cough, wheezing, shortness of breath, fatigue, and reduced exercise capacity. Medications, surgery, maintaining good nutrition, and airway clearnance, breathing exercises. The causative factor is a mutation of the cystic fibrosis transmembrane conductance regulator or chromosome 7. A defective gene and its protein product cause the body to produce unusually thick, sticky mucus that leads to life threatening lung infections, obstructs the pancreas, and inhibits normal digestion and absorption of food. Smoking is the leading cause. Vary with progression and may include salty tasting skin, persistent and productive coughing, frequent lung infections, wheezing, shortness of breath, poor growth/weight gain in spite of a good appetite, and frequent greasy, bulky stools. Antibiotics, nutritional supplements, pancreatic enzyme replacements, mucolytics, and bronchodilators. PT includes airway clearance, breathing techniques, assisted cough, and ventilatory muscle training. General exercise is indicated to improve overall strength and endurance, except with severe lung disease. Medications, supplemental oxygen, antibiotics (if bacterial infection is present). Surgery, maintaining good nutrition. Etc. Shortness of breath, wheezing, chronic coughing, orthopnea, barrel chest, increase use of accessory muscles, increased respiration rate, fatigue, and reduced exercise capacity. Pleural effusion destroyed, so that they collapse during exhalation, not letting air escape from the lungs. The alveoli are permanently overinflated and dead space increase within the lungs. Is a buildup of fluid in the pleural space between the lungs and chest cavity. The excess fluid can push the pleura against the lung making it hard to breath, and in some cases, causing atelectasis. If the fluid gets infected and turns into an abscess, the condition is called empyema. Pleuritis, or inflammation of the visceral and parietal pleura. Pleuritis can be caused by a viral infection, pneumonia, and RA. Shortness of breath. If the fluid becomes infected, dry cough, fever, and chills may appear. Fever, cough, SOB, sweating, shaking chills, chest pain that fluctuates with breathing, headache, muscle pain, and fatigue. Extreme shortness of breath, a feeling of suffocating or drowning, gasping for breath, anxiety, restlessness, a sense of apprehension, coughing, frothy blood tinged sputum, chest pain, irregular pulse. Pneumonia Refers to inflammation of the lungs Usually caused by bacterial, viral, fungal, or parasitic infection Pulmonary edema Occurs when fluid collects in the alveoli within the lungs, making it difficult to breathe. *Acute pulmonary edema is a medical emergency. Occurs when the left ventricle is unable to pump blood adequately (left sided heart failure). Pressure increases inside the left atrium and then in the pulmonary veins and capillaries, causing fluid to be pushed through the capillary walls into the If the pleuritis is caused by a bacterial pneumonia, an antibiotic will be used. Most viral infections run their course without requiring treatment. NSAIDS may help relieve some of the signs and symptoms. If the fluid buildup is large, a chest tube may be inserted to drain the fluid. Antibiotics, antiviral agents, antifungal agents. Lifestyle remedies include rest and drinking plenty of fluids. Supplemental oxygen and medications. Call 911 for acute pulmonary edema. Pulmonary embolism Pulmonary Fibrosis alveoli. Non cardiac pulmonary edema, fluid leaks from the capillaries within the alveoli since the capillaries themselves become more permeable. PE is a condition where Caused by blood clots one or more arteries in the from LEs. lungs become blocked. PE can be life threatening but prompt treatment with anti-clotting medications can greatly reduce the risk of death. A condition in which microscopic damage to the alveoli causes irreversible scarring of the interstitial tissue. Normally, the tissue is highly elastic, expanding and contracting with each breath. Scarring makes the interstitial tissue stiff and thick and the alveoli less flexible, making breath more difficult. Cause is unknown. Chronic exposure to silica dust, asbestosis, grain dust, sugar cane, and bird and animal droppings can cause pulmonary fibrosis. Radiation for lung or breast cancer, chemo drugs, certain antiarrhythmic medications, and some antibiotics and can also cause fibrosis. Sudden onset of SOB, chest pain that becomes worse with deep breathing, coughing sputum. Extremity swelling, fainting. SOB, especially during or after physical activit, and a dry cough which usually does not appear until the disease is advanced and irreversible lung damage has already occurred. Fatigue, unexplained weight loss, and aching muscles and joints. Prompt treatment of anticoagulants and thrombolytic agents greatly reduces the risk of death. Surgery may be done to remove the clot. Prevention includes compression stockings, pneumatic compression, physical activity, and drinking fluids. Lung scarring is irreversible and no current treatment has proven effective in stopping the progression of the disease, some tx may improve symptoms temporarily & improve quality of life. Corticosteriods and immunosuppressive agents are often prescribed initially. Lung transplantation may be used in cases of advanced disease. Supplemental oxygen and pulmonary rehab. Restrictive Lung Dysfunction (RLD) RLD is an abnormal reduction in lung expansion and pulmonary ventilation Caused by abnormal lung parenchyma (atelectasis, pneumonia, pulmonary fibrosis, pulmonary edema, ARDS, abnormal pleura (pleural effusion, fibrosis, pneumothorax, hemothroax, and disorders affecting ventilatory pump function. Dyspnea on exertion, a persistent non productive cough, increased respiratory rate, hypoxemia, decreased vital capacity, abnormal breath sounds. Antibiotics for pneumonia, treatment of edema, reversal of CNS depression. Mechanical ventilation, supplemental oxygen, nutrition support, muscle training. Common Diagnostic Procedures: 1. Holter monitoring-EKG electrodes record 24-48 hours or longer to evaluate cardiac rhythm. 2. Angiography-inject a contrast medium into the blood vessels. Can show the location of plaques in the arteries and the extent of occlusion. 3. Bronchoscopy-Direct visualization of the bronchial tree via fiberoptic instrument that transmits image to screen. 4. Cardiac catheterization-thin, inserted into an artery in the leg or arm where a contract dye is injected. 5. Carotid ultrasound-uses sound waves to examine and visualize the structure and function of the carotid arteries. 6. Chest radiograph-used to visualize the location, size, and shape of the heart, lungs, blood vessels, ribs, and bones of the spine. Can also reveal fluid in the lungs or pleural space, pneumonia, emphysema, cancer or other conditions. 7. Computed tomography (CT)-uses an x-ray machine that rotates around a pt lying on a table. The pictures are slices of the body called tomograms and each picture is called a computed tomograph. 8. Echocardiography-uses high frequency sound waves non invasively to evaluate the functioning of the heart via real time images. Can provide information on the size and function of the ventricles, thickness of the septums, and function of the walls, valves, and chambers. 9. Fluroscopy-A continuous x-ray procedure that shows the heart and lungs. Involves a high dose of radiation, it has largely been replaced by echocardiography. 10. Magnetic Resonance Imaging (MRI)-uses a magnetic field and radio waves to create 3D images of the heart and blocked vessels to assess the size and function, thickness, and damage or heart disease. Limited for imaging the lungs. 11. Positron Emission Tomography (PET)-imaging test in which a small amount of radioactive material is injected, inhaled, or swallowed,. Radioactive material tends to accumulate in areas with high levels of chemical activity corresponding to areas of disease. PET is useful in evaluating heart disease and cancer. Cardiovascular/pulmonary Systems: Innervation of the Heart: 12. The sympathetic influence is achieved by release of epinephrine & norepinephrine. Sympathetic nerves stimulate the chambers to beat faster (chronotrophic effect) and with greater force of contraction (inotroophic effect). Sympathetic activation leads to ↑ cardiac contractility, ↑HR, venoconstriction, and arterial vasoconstriction, ultimately leading to ↑BP. 13. The parasympathetic influence is achieved via acetylcholine release from the vagus nerve. Parasympathetic nerves slow the heart rate (chronotrophic effect) primarily through their influence on the SA node. Parasympathetic leads to a ↓HR and a small decrease in contractility, resulting in a ↓ in BP. 14. Valsalva Maneuver: Forced expiration against a closed glottis produces ↑ intrathoracic pressure, ↑central venous pressure and ↓ venous return. The resultant decrease in cardiac output and BP is sensed by baroreceptors, which reflexively increase HR and myocardial contractility. 15. Pathology Cerebrovascular Accident (CVA) Diagnosis Occurs when there is an interruption of cerebral circulation that results in cerebral insufficiency, destruction of surrounding brain tissue, and subsequent neurological deficit. Laboratory/Imaging CT can confirm an area of infarct in the brain and its vascular origin, however it can present as negative for up to a few days after the event. MRI allows for the diagnosis of ischemia within the brain almost immediately after onset. PET can provide info regarding cerebral perfusion and cell function. Ultrasonography identifies areas of diminished blood flow in vessels and angiography may Management/Prognosis Medical management will initially include medically stabilizing the pt through medication and surgical intervention. PT in acute phase focuses on positioning, pressure relief, sensory awareness re-education, balance, ROM, weightbearing, facilitation, postural control. Rehab can include Bobath’s NDT, Brunnstrom’s Movement therapy, Rood, Kabat, Knott, PNF. The outcome depends on pts overall health, level of cognition, motor identify a clot and determine if surgical intervention is necessary. Congestive Heart Failure (CHF) Left sided heart failure: generally associated with signs of pulmonary venous congestion. Right sided heart failure: associated with signs of systemic venous congestion. Occurs when the heart can no longer meet the metabolic demands of the body. The heart’s inability to pump a sufficient amount of blood occurs when there in insufficient or defective cardiac filling and/or impaired contraction & emptying of the heart. The impairment in cardiac output causes the body to compensate for this deficit and this results in an increase in blood volume, cardiac filling pressure, HR, and cardiac muscle mass. A pt with CHF will initially Urinalysis and a CBC count that includes electrolyte, thyroid stimulating hormone, blood urea nitrogen (BUN), and serum creatinine levels should be performed. A chest x-ray, electrocardiogram, and echocardiogram are also recommended. A Doppler echocardiogram can determine systolic & diastolic performance, the cardiac output (ejection fraction), and pulmonary artery and ventricular filling pressures. recovery, and family support. The first 3 months of recovery typically reveals the most measureable neurologic recovery and is usually a good indicator of the longterm outcome. Research shows a pt can continue to improve for an average of 2-3 years post CVA. CHF is a common disorder. A pt can live with CHF and should benefit from PT in order to improve endurance and strength after a decline in function from hospitalization or bed rest. After diagnosis there is mean of 3.2 years of survival for men and 5.4 years for females. Cystic Fibrosis (CF) show signs of tachycardia. Other signs include venous congestion, high catecholamine levels, & impaired cardiac output, sudden weight gain, SOB, S3 gallop. Is an inherited disease that affects the ion transport of the exocrine glands resulting in impairment of the hepatic, digestive, respiratory, and reproductive systems. The disease causes the exocrine glands to overproduce thick mucus, overproduce normal secretions or overproduce sodium & chloride. Mostly affects children, African American followed by Caucasians. Neonates meconium can be tested as a screening tool for increased albumin. The quantitative pilocarpine iontophoresis sweat test is the sole diagnostic tool in determining the presence of CF. Sodium & chloride amounts greater than 60 mEq/l (standard value is 40 mEq/l) is a positive diagnosis for CF. The sweat test should be performed twice to ensure accuracy. Chest PT should be performed several times a day and includes bronchial drainage, percussion, vibration, breathing and assistive cough techniques & ventilatory muscle training. A pt with CF will require intermittent PT thought their life. The goals are to maximize secretion clearance from the lungs, optimize pulmonary function, and maximize the pts quality of life. CF is a terminal disease, however, the median age of death as increased to 35 years of age due to early detection and comprehensive management. The most Emphysema Refers to a pathologic accumulation of air in the lungs found with COPD. COPD is the second leading cause of disability in individuals under 65 years of age worldwide. Emphysema results from a nonreversible injury and destruction of elastic protein within the alveolar walls. X-ray is utilized to visually evaluate the shape and spacing of the lungs. Other imaging studies include a planogram to detect bullae and a bronchogram to evaluate mucus ducts and detect possible enlargement of the bronchi. Arterial blood gases may indicated a ↓ PaO2. Impaired FEV1,vital capacity and forced vital capacity. Total lung capacity, residual volume, and functional residual volume will be ↑. Lymphedema PostMastectomy Lymphedema following a mastectomy is termed secondary lymphedema and is the result of Lymphedema classified into 3 stages. Stage I: pitting edema that reduces with elevation common cause of death is respiratory failure. Males generally have a better prognosis than females. Pharmacological intervention, oxygen therapy, PT. PT intervention consist of generalized exercise, endurance training, pursed-lip breathing, ventilatory muscle strengthening, chest wall exercises, and pt education on posture, airway secretion clearance. Emphysema is a chronic progressive disease process. Pts require ongoing medical care and intermittent physical therapy intervention. Life expectancy decreases to less than 5 years with severe expiratory slowing measured at a rate of <1 L of air during FEV1. Pharmacological intervention or natural substances that increase proteolysis and damage to the lymphatic nodes and vessels during surgery. Excessive accumulation of lymph fluid within the soft tissues is caused by an excess load of lymph fluid or inadequate transport capacity within the lymphatic system secondary to the loss of homeostasis. Myocardial Infarction (MI) Occurs when there is poor coronary artery perfusion, ischemia, and subsequent necrosis of the cardiac overnight and does not exhibit any fibrotic changes. Stage II: identified by some fibrotic changes that being to occur & increase in non-pitting edema that does not reduce with elevation. Stage III: is characterized by skin changes, frequent infections, and severe edema that is nonpitting and fibrotic. Diagnosis is confirmed through history, observation, and several diagnostic tools to rule out other disorders. A Doppler is used to rule out DVT. CT or MRI to rule out malignancy. A lymphoscintigram is a nuclear medicine procudre that tests the function of the lymphatic system. Primary tool to detect MI is a 12 lead EKG. An inverted T wave indicates myocardial ischemia, elevated ST macrophage activity. No cure. Surgery is used in the treatment of severe cases.PT follows a treatment approach termed combined decongestive physiotherapy (CDP). Lymphedema is progressive if left untreated, but can be managed through intervention and education. Pts must comply with a home program and must remain aware of all activities that place the pt at an increased risk for lymphedema. Stabilize the pt and initiate pharmacological intervention to hinder the evolution of the MI. Cardiac rehab is Restrictive Lung Disease (RLD) tissue usually due to thrombus, arterial blockage or atherosclerosis. The location and severity of the infarct will determine symptoms and overall clinical picture. segment indicates acute infarction, and a depressed ST segment indicates a pending subendocardial or transmural infarction. A blood serum analysis can be utilized to determine the level of selected cardiac enzymes. CPK, AST, and lactic dehydrogenase can be dramatically altered during and after a MI. Is a classification of disorders caused by a pulmonary or extrapulmonary restriction that produces impairment in lung expansion and an abnormal reduction in pulmonary ventilation. There are multiple conditions that can cause restrictive lung disease. Pulmonary restriction can be caused by tumor, A chest radiography is utilized to evaluate lung structure and evidence of fibrosis, infiltrates, tumor, and deformity. Arterial blood gas analysis may indicated a decrease in PaO2. VC, FVC, and TLC will be impaired. Normal residual volume, and expiration flow rates. ERV and FRC are often decreased. recommended status post MI. The pt should start in the coronary care unit (CCU) and progress through each of the phases of cardiac rehab. P that that has experienced an MI may be able to return to all previous activities after successful completion of a cardiac rehab program. A pt must continue to reduce the modifiable risk factors and maintain an appropriate level of exercise in order limit another MI. PT includes body mechanics, posture training, diaphragm and ventilatory muscle strengthening, relaxation and energy conservation. Outcome is based on the etiology of the restrictive lung disease and pt response to PT intervention. Some disorders require surgical intervention that alleviates the condition while other interstitial pulmonary fibrosis, scarring within the lungs, and pneumonia. Extrapulmonary restrictions include pleural effusion, chest wall stiffness, structural abnormality, postural deformity, muscle weakness, and central nervous system injury. RLD includes a ↓ in lung & chest wall compliance, ↓in lung volumes and an ↑ in the work of breathing. A pt with restrictive lung disease is characterized by a reduction of lung volumes, ↓ chest mobility, ↓breath sounds, SOB, hypoxemia, rapid and shallow respiratory pattern, ineffective cough. are progressive and irreversible. Some pts with end-stage disease may be candidates for lung transplantation, however most eventually progress to ventilatory failure. 16. 17. Description of Blood Gases: Arterial Blood Gas (ABG) Are collected to evaluate acid-base status (pH), ventilation (PaCO2), and oxygenation of arterial blood (PaO2). The partial pressure of oxygen in arterial blood PaO2 and the percent oxygen saturation of hemoglobin Cardiac Biomarkers Cholesterol Test Complete Blood Count (CBC) (SaO2) provide information about how well the lungs are functioning to oxygenate the blood. The partial pressure of carbon dioxide in arterial blood (PaCO2) provides info on how well the lungs are able to remove carbon dioxide. Changes in PaCO2 directly affect the balance of pH in the body. Blood pH is tightly regulated, as an imbalance in either direction can affect the nervous system and can cause convulsions or coma. Bicarbonate (HCO3-) is an important component of the chemical buffering system that keeps the blood from becoming too acidic or basic and is often part of an ABG test. Certain enzymes leak out of the heart cells and into the blood after a myocardial infarction. Cardiac enzyme studies measure the levels of creatine phosphokinase (CK) and the protein troponin in the blood. CK-MB is a relatively specific test for myocardial infarction. It appears in blood approximately 4 hours after infarction, peaks at 12-24 hours, and declines over 48-72 hours. Cardiac troponin-I is also a specific marker for infarction, and unlike CK-MB levels, it remains elevated for 5-7 days. Also called a lipid panel or lipid profile, a cholesterol test measures the amount of cholesterol and triglycerides in the blood in order to determine the risk of atherosclerosis. Cholesterol is carried in the circulation in association with lipoproteins. A complete lipid profile includes the measurement of 4 types of lipids in the blood: total cholesterol, highdensity lipoprotein (HDL) cholesterol, low-density lipoprotein (LDL) cholesterol, and triglycerdies. HDL cholesterol is referred to as the “good” cholesterol because it helps carry away LDL cholesterol and is protective against atherogenesis. LDL is referred to as the “bad” cholesterol since it is associated with the buildup of fatty plaques within the arteries which reduce blood flow. The body converts any calories it does not need to use right away into triglycerides, which are stored in adipose tissue. High levels of triglycerides are seen in overweight people, in those consuming too many sweets or too much alcohol, and in people with diabetes who have elevated blood sugar levels. Measures red blood cell count, white blood cell count, white blood cell differential, platelets, hemoglobin, and hematocrit. A CBC is performed to assess health, to diagnose and monitor a medical condition, and to Hematocrit (Hct) Partial Thromboplastin Time (PTT) and Prothrombin Time (PT) monitor the effects of medical treatment. Is the percentage of red blood cells in total blood volume. A low hematocirt may indicate anemia, blood loss, and vitamin or mineral deficiencies. A high hematocrit may indicate dehydration or polycythemia vera, a condition that causes an overproduction of red blood cells. PTT and PT tests measure how quickly the blood clots. The tests are commonly used to monitor oral anticoagulant therapy or to screen for selected bleeding disorders. The tests examine all of the clotting factors of the intrinsic pathway with the exception of platelets. Partial thromboplastin time is more sensitive than prothrombin time in detecting minor deficiencies. 18. 19. Arterial blood gases: pH PaCO2 (amount of carbon dioxide within arterial blood) PaO2 HCO3- (amount of bicarbonate ions within arterial blood) SaO2 *By convention, ABG results are written or spoken in the following order: pHPaCO2PaO2HCO3- (e.g. 7.4/40/97/24) Partial Thromboplastin Time (PTT) Acidemia Alkalemia Eucapnia Hypercapnia Hyopcapnia Hypoxemia Mild hypoxemia 7.4 (7.35-7.45) 40 mm Hg at sea level breathing ambient air (35-45mm Hg) 97 mm Hg at sea level breathing ambient air (80-100 mm Hg) 24 mEq/L (22-26) 95-98% 26-39 seconds Elevated acidity of blood (pH < 7.35) Decreased acidity of blood (pH > 7.45) Normal level of CO2 in arterial blood (35-45 mm Hg) Elevated level of CO2 in arterial blood( > 45 mm Hg) Low level of CO2 in arterial blood (<35 mm Hg) Low level of O2 in arterial blood (PaO2 < 80 mm Hg) PaO2 60-79 mmHg Moderate hypoxemia Severe hypoxemia Hypoxia PaO2 40-59 mmHg PaO2 < 40 mmHg Low level of O2 in the tissue despite adequate perfusion of the tissue 20. *An increase in the PaCO2 decreases the body’s pH. A decrease in the PaCO2 raises the body’s pH. 21. *Supplemental oxygen is usually prescribed when the PaO2 falls below 55 mmHg. 22. 23. Other values: White Blood Cells (WBCs) (Leukocytes) 4300-10,800 Red Blood Cells (RBCs) (Erythrocytes) Male: 4.6-6.2 Female: 4.2-5.9 Erethrosedimentation Rate (ESR) Male: <15 mm/hr Female: <20 Hematocrit Male: 45%-52% Female: 37%-48% Platelet 150,000-450,000 Sodium 135-146 Calcium 8.4-10.4 Potassium 3.5-5.5 Magnesium 1.8-2.4 Total cholesterol <200 LDL <100 HDL <40 Triglyceride <150 24. 25. Pharmacological Management of Heart and Vascular Diseases: Drug Alpha Adrenergic Antagonist Agents Action Indications Reduce peripheral vascular tone by blocking alpha-1 adrenergic receptors. This Hypertension, benign prostatic hyperplasia Side Effects Dizziness, palpitations, orthostatic hypotension, drowsiness Implications for PT Use caution when rising from a sitting or lying position due to the risk of Examples Cardura (doxazosin, Minipress (prazosin), Hytrin (terazosin) action causes dilation of arterioles & veins and ↓ BP. AngiotensinConverting Enzyme (ACE) inhibitor Agents Decrease blood pressure and afterload by suppressing the enzyme that converts angiotensin I to angiotensin II. HTN, congestive heart failgure Hypotension, dizziness, dry cough, hyperkalemia, hyponatremia Angiotensin II receptor antagonist angents Block angiotensin II receptors which limit vasoconstrictio n & stimulation of vascular tissue Divided into 4 classes. Class I HTN, congestive heart failure Dizziness, back and leg pain, angina pectoris Cardiac arrhythmias Unique to the specific Antiarrhythmic Agents dizziness and/or orthostatic hypotension . Closely monitor pt during exercise. Avoid sudden changes in posture due to the risk of dizziness & fainting from hypotension . Pts w heart failure should avoid rapid increases in physical activity. Minimal implications for PT Encourage pts to Capoten (captorpril), Vasotec (enalapril), Prinivil (lisinopril), Altace (ramipril) Cozaar (losartan), Atacand (candesartan), Diovan (valsartan) Sodium channel (sodium channel blockers)contorl cardiac excitation & conduction. Class II (beta blockers)inhibit sympathetic activity by blocking Badrenergic receptors. Class III-prolong repolarization by inhibiting both potassium & sodium channels & are often considered the most effective antiarrhytmic agent. Class IV(calcium channel blockers)depress depolarization & slow conduction through the AV node. antiarrhythmic agent; exacerbation of cardiac arrhythmias, dizziness, hypotension adhere to the prescribed dosing schedule and immediately report any adverse reactions to a healthcare professional . blockers: quinidine (generic), Xylocaine (lidocaine) Beta blockers: Tenormin (atenolol) Prolonged repolarization : Cordarone (amiodarone Calcium channel blockers: Cardizem (diltiazem) Anticoagulant Agents Inhibit platelet aggregation & thrombus formation Antihyperlipide mia Agents There are 5 categories of lipid-modifying agents. The most commonly used drugs, the statins, inhibit enzyme action in cholesterol synthesis, break down LDL, ↓ triglyceride levels, and ↑ HDL levels. The Post percutaneous transluminal coronary angioplasty & coronary artery bypass graft surgery, prevention of venous thromboemboli m& cardioembolic events in pts with atrial fibrillation & prosthetic heart valves Hyperlipidemia, atherosclerosis, prevent coronary events in pts with existing coronary disease, diabetes or PVD Hemorrhage, ↑ risk of bleeding, gastrointestina l distress with oral medication A therapist must be careful to avoid injury secondary to the risk of excessive bleeding or bruising. Pt education regarding common side effects is also indicated to protect the pts. Heparin, Coumadin (warfarin), Lovenox (enoxaparin) Headache, GI distress, myalgia, rash Aerobic exercise can increase high density lipoproteins and maximize the effects of drug therapy Lipitor (atorvastatin), Zocor (simvastatin), Tricor (fenobibrate) Antithrombotic (antiplatelet) agents Beta Blocker Agents (BetaAdrenergic Blocking Agents) other categories are bile acid sequestrants, nicotinic acid, cholesterol absorption inhibitors, & fibric acid derivatieves Antithrombotic agents inhibit platelet aggregation and clot formation Decrease the myocardial oxygen demand by decreasing heart rate and contractility by blocking Badrenergic receptors Post-myocardial infarction, a-fib, prevent arterial thrombus formation HTN, agina, arrhythmias, heart failure, migraines, essential tremor Hemorrhage, thrombocytop enia, potential liver toxicity with the use of aspirin, GI distress Bradycardia, cardiac arrhythmias, fatigue, depression, dizziness, weakness, blurred vision Must be careful to avoid injury secondary to the risk of bleeding. HR & BP response to exercise will be diminished. Rate of perceived exertion may be used to monitor exercise intensity. Closely monitor pts during positional changes due Bayer (aspirin), Plavix (clopidogrel), Persantine (dipyridamole ) Tenormin (atenolol), Lopressor (metoprolol), Inderal (propanolol) Calcium Channel Blocker Agents Decrease the entry of calcium into vascular smooth muscle cells resulting in diminished myocardial contraction, vasodilation, and ↓ oxygen demand of the heart HTN, angina pectoris, arrhythmias, congestive heart failure Dizziness, headache, hypotension, peripheral edema to an ↑ risk for orthostatic hypotension . HR & BP response to exercise will be diminished. Monitor pt closely when moving to an upright position secondary to dizziness and/or orthostatic hypotension . Observe the Pt for signs & symptoms of congestive heart failure such as worsening peripheral edema, dyspnea or weight gain. Norvasc (amlodidine), Procardia (nifedipine), Calan (verapamil) Cardizem (dilitazem) Diuretic Agents ↑ the excretion of sodium & urine. This causes a reduction in plasma volume which ↓ blood pressure. Classifications include thiazide, loop, and potassium sparing agents. HTN, edema associated with heart failure, pulmonary edema, glaucoma Dehydration, hypotension, electrolyte imbalance, polyuria, ↑LDL, arrhythmias Nitrate Agents ↓ ischemia through smooth muscle relaxation and dilation of peripheral vessels Angina pectoris Headache, dizziness, orthostatic hypotension, reflex tachycardia, nausea, vomiting. Positioning changes can increase the risk of dizziness and falls due to ↓ BP. Monitor pts closely for signs & symptoms of electrolyte imbalance and muscle weakness or cramping. Pts must be educated to come to a standing position slowly. Sublingual administrati on of nitroglycerin is the preferred method to treat an acute angina attack. Thiazide: Diuril (chlorothiazid e) Loop: Lasix (furosemide) Potassium sparing: Dyrenium (triamterene) Nitrostat (nitroglycerin) , Isordil (isosorbide dinitrate), Amyl nitrite solution for inhalation. Positive Inotrophic Agents ↑the force and velocity of myocardial contraction, slow the HR, ↓conduction velocity through the AV node, & ↓ the degree of activation of the sympathetic nervous system. Heart failure, atrial fibrillation Cardiac arrthytmias, GI distress, dizziness, blurred vision Thrombolytic Agents Facilitate clot dissolution through conversion of plasminogen to plasmin. Plasmin breaks down clots & allows occluded vessels to reopen to maintain blood flow. Acute myocardial infarction, pulmonary embolism, ischemic stroke, arterial or venous thrombosis Hemorrhage (specifically intracranial in certain populations), allergic reaction, cardiac arrhythmia Therapists should monitor HR during activity, teach the pt and fam to take the pts pulse, and seek health care providers advice for rates less than 60 bpm or more than 100 bpm. Therapist must be careful to avoid situations that may cause trauma due to altered clotting activity. Lanoxin (digoxin) Linlytic (urokinase), Activase (alteplase) Pharmacological Management of Airway and Lung Diseases: Drug Action Indications Side Effects Arrhythmia s, postural hypotensio n, GI distress, dizziness, drowsiness, headache, blurred vision, fatigue, nausea, thickening of bronchial secretions Corticoster oid: systemic side affects are decreased with the inhaled form, but may include damage of supporting tissues, skin breakdown, Antihistamine Agents Block the effects of histamine resulting in a ↓ in nasal congestion, mucosal irritation, & symptoms of the common cold, sinusitis, conjunctivitis, & allergies Respiratory seasonal allergies, rhinitis & sneezing from the common cold, allergic conjunctivitis, motion sickness, and Parkinson’s disease AntiInflammatory Agents Inhaled corticosteroids, leukotriene modifiers, & mastcell stabilizers help prevent inflammatory mediated bronchoconstrcit on by inhibiting production of inflammatory cells, suppressing release of Bronchospasm, asthma Implications for PT Increase guarding when rising from a sitting or lying position due to the risk of orthostatic hypotension. Closely monitor pt during exercise. Instuct the pt in the use of correct use the inhaler and to rinse their mouth with water after use to avoid irritation of local mucosa. Advise the pts that these agents Examples Benadryl (diphenhydramin e), Allegra, Zyrtec, Claritin Corticosteroid: Qvar, Pulmicort, AeroBid Leukotriene modifier: Zyflo Mast cell stabilizer: Nasalcrom inflammatory mediators (cytokines, prostaglandins, leukotrienes), and reversing capillary permeability, in turn reducing airway edema. Bronchodilator Agents Relieve bronchospasm by stimulating the receptors that cause bronchial Bronchospasm, wheezing, and SOB in asthma & COPD osteoporosi s, ↓bone density, glaucoma, and delayed growth. Local effects include nasal irritation and dryness, sneezing and bloody mucus; Leukotrien e modifier: liver dysfunction ; Mast cell stabilizer: bronchospa sm, throat and nasal irritation, cough, GI distress Paradoxical bronchospa sm, dry mouth, GI distress, are not bronchodilat ors and should not be used to treat acute episodes of asthma. Should advice pts to take their bronchodilat or Anticholinergic: Atrovent, sprivia. Sympathomimeti cs: Ventolin, Primatene mist, smooth muscle relexation or by blocking the receptors that trigger bronchoconstricti on. Primary classifications include anticholinergic, sympathomimeti cs, & xanthine derivatives. Expectorant Agents Increase respiratory secretions which help to loosen mucus. Reducing the viscosity of secretions and increasing sputum volume improves the efficiency of the cough reflex and of ciliary action in removing accumulated secretions. chest pain, palpitations , tremor, nervousnes s. Long acting sympathom imetics, including salmeterol, increase the risk of asthma related death. Cough associated with respiratory tract infections and related conditions such as sinusitis, pharyngitis, bronchitis, and asthma, when complicated by tenacious mucus or mucus plugs and congestion GI distress, drowsiness medication as prescribed before therapy and to bring their short acting meds with them. Cardiac or vision abnormalitie s may indicate toxicity, and physician should be notified immediatley. Therapists can exploit the effects of expectoratnt agents by performing airway clearance interventions within one hour after drug administratio n. Encourage pts to take meds with a Serevent. Xanthine derivative: TheoDur, Aminophylline Mucinex (guaifenesin), terpin hydrate Mucolytic Agents ↓ the viscosity of mucus secretions by altering their composition and consistency, making them easier to expectorate. They are administered by a nebulizer. Vicous mucus secretions due to pneumonia, emphysema, chronic bronchitis, and cystic fibrosis Pharyngitis, oral mucosa inflammati on, rhinitis, chest pain glass of water. Exploit the effects by performing airway clearance interventions Pulmozyme, Mucosil or Mycomyst Cardiovascular/pulmonary/lymphatic Interventions: Aerobic Exercise Prescription: Aerobic exercise, or cardiorespiratory endurance exercise, refers to submaximal, rhythmic repetitive exercise of large muscle groups during which adenosine triphosphate is synthesized primarily by the long-term energy system and the utilization of inspired oxygen. Type (modality): walking, cycling, jogging are recommended to improve exercise tolerance, can be maintained at a constant velocity, very low interindividual variability. Dynamic arm exercise (arm ergometry): uses a smaller muscle mass, results in lower VO2 max (60%-70%lower) than leg ergometry; at a given workload, HR will be higher, stroke volume lower; systolic and diastolic BP’s will be higher. Early rehab: activity is discontinuous (interval training), with frequent rest periods; progressing to continuous training. Interval training can also be incorporated in vigorous training to allow patient to work at higher percentage of V02 max. Warm and up and cool down: gradually decrease the intensity of exercise, 5-10 minutes. Resistive exercises: to improve strength and endurance in clinically stable pts. Usually prescribed in later rehab, after a period of aerobic training. Moderate intensities are typically used (60%-80% of 1 repetition or 10 repetition maximal voluntary contraction. Precautions: monitor BP, avoid breath holding (Valsalva’s response: may dramatically ↑ BP and work of heart). Contraindicated for patients with: uncontrolled hypertension or arrhythmias Intensity: prescribed as % of functional capacity revealed on ETT, within a range of 40%-85% depending upon initial level of fitness; typical training intensity is 60%-80% of functional capacity; lower training intensities may necessitate an increase in training duration; most clinicians use a combination of HR, RPE, and METs to prescribe exercise intensity (eliminates problems that may be associated with individual measures) Heart rate: 1. Percentage of maximum HR achieved on ETT; without ETT 208-0.7 x age. 70%-85% HR max closely corresponds to 60%-80% of functional capacity or VO2 max. 2. Estimated HR max is used in cases where submax ETT has been given. 3. Heart rate range or reserve (Karvonen’s formula) Can more closely approximate the relationship between HR and VO2 max, but increased variability in pts on medications. Problems associated with use of HR alone to prescribe exercise intensity. 60%-80% (HR maxresting HR) + resting HR = target HR. 4. Beta blocking: affects ability of HR to rise in response to an exercise stress. 5. Pacemaker: can affect the ability of HR to rise in response to an exercise stress if it is fixed. 6. Environmental extremes, heavy arm work, isometric exercise and valsalva may affect HR and BP responses. Rating of perceived exertion, the original Borg RPE scale (6-20). 1. Useful along with other measures of pts effort if beta blockers or other HR suppressors are used. 2. Problems with use of RPE alone to prescribe exercise intensity: Individuals with psychological problems (depression) Unfamiliarity with RPE scale; may affect selection of ratings RPE scale 6-20 is linearly associated with HR. Ex. Multiple by 10. 6x10=60 bpm. If pt is 42 years old and reports 16 on the scale: 220-42=178 (predicted Max HR) 16x10=160bpm (borg scale) 160/178=89% so answer would be the one that correlates most with 89%. METs, or estimated energy expenditure (V02) 1. 40%-85% of functional capacity (maximal METs) achieved on ETT. Without a maximal ETT, this is an estimation of workload. 2. Problems associated with use of METs alone to prescribe exercise intensity: -With high intensity activities (jogging) need to adopt a discontinuous work pattern: walk 5 minutes, jog 3 minutes to achieve the desired intensity. -Varying skill level or stress of competition may affect the known metabolic cost of an activity. -Environmental stresses (heat, cold, high humidity, altitude, wind, changes in terrain such as hills) may affect the known metabolic cost of an activity. Duration: Conditioning phase may vary from 10-60 minutes, depending upon intensity; the higher the intensity, the shorter the duration. -Average conditioning time is 20-30 minutes for moderate intensity exercise. -Severely compromised individuals may benefit from multiple, short exercise sessions spaced throughout the day (3-10 min sessions) -Warm-up and cool-down periods are kept constant 5-10 min each. Frequency: -Frequency of activity is dependent upon intensity and duration; the lower the intensity, the shorter the duration, the greater the frequency. -Average: 3-5 sessions/week for exercise at moderate intensities and duration (>5 METs) -Daily or multiple daily sessions for low intensity exercise (<5 METs) Progression: -Modify exercise prescription if: -HR is lower than target HR for a given exercise intensity -RPE is lower (exercise is perceived as easier) for a given exercise -Symptoms of ischemia (angina) do not appear at a given exercise intensity -Rate of progression depends on age, health status, functional capacity, personal goals, and preferences. -As training progresses, duration is increased first, then intensity. Normal Cardiorespiratory Response to Acute Aerobic exercise: -↑ oxygen consumption due to ↑ cardiac output, ↑ blood flow, and oxygen utilization in the exercising skeletal muscles -Linear increase in SBP with increasing workload (8 to 12 mm Hg per MET) -No change or moderate decrease in DBP -↑respiratory rate and tidal volume Consider reduction in exercise/activity with: -Acute illness: fever, flu -Acute injury, orthopedic complications -Progression of cardiac disease: edema, weight gain, unstable angina -Overindulgence: food, caffeine, alcohol -Environmental stressors: extremes of heat, cold, humidity, air pollution Consider terminating exercise: Absolute Indications: -Drop in systolic BP >10 mm Hg with increased workload -Moderate to severe angina -↑ nervous system symptoms (ataxia, dizziness, near syncope) -Signs of poor perfusion -Technical difficulties in monitoring EKG or BP -Subject’s desire to stop -Sustained VT -ST elevation > or equal to 1.0 mm Relative Indications to terminate exercise: -ST or QRS changes (excessive ST depression) or marked axial shift -Arrhythmias other than sustained VT (multifocal PVCs, triplets, SVT, heart block, bradyarrhythmaias) -Fatigue, SOB, wheezing, leg cramps or claudication -Development of bundle branch block that can’t be distinguished from VT -Increasing chest pain -Hypertensive response (SBP >250 mmHg or DBP >115 mmHg) •Exercise prescription for post-PTCA (percutaneous transluminal coronary angioplasty): 1. Wait to exercise vigorously approximately 2 weeks post-PTCA to allow inflammatory process to subside. Walking program can be initiated immediately. 2. Use post-PTCA ETT to prescribe exercise. •Exercise prescription post-CABG (coronary artery bypass graft): 1. Limit upper extremity exercise while sternal incision is healing 2. Avoid lifting, pushing, pulling for 4-6 weeks postsurgery _____________________________________________________________________________________ Phase 1: Inpatient Cardiac Rehabilitation (Acute) Length of hospital stay is commonly 3-5 days for uncomplicated MI (no persistent angina, malignant arrhythmias, or heart failure) 1. Exercise/activity goals out outcomes -Initiate early return to independence in ADLs, typically after 24 hours or until the patient is stable for 24 hours; monitor activity tolerance -Counteract deleterious effects of bed rest: reduce risk of thrombi, maintain muscle tone, reduce orthostatic hypotension, and maintain joint mobility -Help allay anxiety and depression -Provide medical surveillance -Provide pt & fam education -Promote risk factor modification 2. Exercise/activity guidelines: -Program components: ADLs, selected arm and leg exercises, early supervised ambulation -Initial activities: low intensity (2-3 METs) progressing to > or equal to 5 METs by discharge. -Post-MI: limited to 70% max HR and/or 5 METs until 6 weeks post-MI. -Short exercise sessions, 2-3 times a day; gradually duration is lengthened and frequency is decreased. Post surgical pts: -Typically are progressed more rapidly than post MI, unless there was a peri-operative MI. -Lifting activities are restricted, generally for 6 weeks. Patient and family education goals: -Improve understanding of cardiac disease, support risk factor modification -Teach self-monitoring procedures, warning signs of exertional intolerance; (persistent dyspnea, angina pain, dizziness) -Teach concepts of energy costs, fatigue monitoring, general activity guidelines, activity pacing, energy conservation techniques; home exercise program -Provide emotional support and assist with referral to social work as needed Home Exercise Program (HEP): -Low risk pts may be safe candidates for unsupervised exercise at home -Gradual increase in ambulation time: goal of 20-30 minutes, 1-2 times per day at 4-6 weeks post MI. -Upper and lower extremity mobility exercises. -Elderly homebound pts with multiple medical problems may benefit from a home cardiac rehab program. -Pts should be skilled in self-monitoring procedures. -Recommended family training in CPR, and AED as indicated; emergency lifeline for some pts. Phase 2: Outpatient Cardiac Rehabilitation (Subacute): 1. Eligible patients -MI/acute coronary syndrome -CABG -PCI -Stable angina -Heart valve surgical repair or replacements -Heart or heart/lung transplantation -Heart failure and PAD: not covered by insurance but these populations benefit from supervised exercise program 2. Exercise/activity goals and outcomes: -Improve functional capacity -Progress towards full resumption of activities of daily living, habitual and occupational activities. -Promote risk-factor modification, counseling as to lifestyle changes. -Encourage activity pacing, energy conservation; stress importance of taking proper rest periods 3. Exercise/activity guidelines: Outpatient Program : -Pts at risk for arrhythmias with exercise, angina, other medical problems benefit from outpatient programs with availability of EKG monitoring, trained personnel and emergency support. -Group camaraderie and support of program participants may assist in risk-factor modification and lifestyle changes -Frequency: 2-3 sessions/week -Duration: 30-60 minutes with 5-10 minutes of warm-up and cool down -Programs may offer a single mode of training (walking) or multiple modes using a circuit training approach (treadmill, cycle ergometer, arm ergometer); strength training. -Pts are gradually weaned from continuous monitoring to spot checks and self-monitoring. -Suggested exit point: 9 MET functional capacity (5 MET capacity is needed for safe resumption of most daily activities) Strength training in Phase 2 programs: -Guidelines: after 3 weeks cardiac rehab; 5 weeks post MI or 8 weeks post CABG. -Begin with use of elastic bands and light hand weights (1-3 lbs) -Progress to moderate loads, 12-15 comfortable repetitions. Phase 3: Community Exercise Programs (Post-acute, Postdischarge from Phase 2) 1. Exercise/activity goals and outcomes: -Improve and/or maintain functional capacity -Promote self-regulation of exercise programs -Promote life-long commitment to risk-factor modification 2. Exercise/Activity guideliens: -Location: community centers, YMCA, or clinical facilities -Entry level criteria: functional capacity of 5 METs, clinically stable angina, medically controlled arrhythmias during exercise -Progression is from supervised to self-regulation of exercise -Progression to 50%-85% of functional capacity, 3-4 times/week, 45 minutes or more/session. -Regular medical check-ups and periodic ETT generally required -Utilize motivational techniques to maintain compliance with exercise programs, life-style modifications -Discharge typically in 6-12 months. Clinical indications for inpatient & outpatient cardiac rehab: -Medically stable post MI -Stable angina pectoris -PTCA -CABG -Compensated heart failure -Cardiomyopathy -Heart transplant -Other cardiac surgery (valve repair, pacemaker) -Peripheral arterial disease -High risk for coronary artery disease with diagnosis of DM, dyslipidemia, HTN, or obesity -End-stage renal disease Clinical Contraindications for inpatient & outpatient cardiac rehab: -Unstable angina -Resting SBP >200 mm Hg or resting DBP >110 mm Hg -Orthostatic blood pressure drop of >20 mm Hg with symptoms -Critical aortic stenosis -Acute systemic illness or fever -Uncontrolled atrial/ventricular arrhythmias -Third-degree atrial ventricular block without pacemaker -Active pericarditis or myocarditis -Recent embolism -Thrombophlebitis -Resting ST segment depression or elevation >2 mm -Uncompensated congestive heart failure -Orthopedic or metabolic conditions that would prohibit exercise Resistance Exercise Training: Goals: Improve muscle strength and endurance; enhance functional independence; decrease cardiac demands during daily activities Patient criteria for resistance training: -Post MI: resistance training permitted if remain under 70% max HR or 5 METs for 6 weeks post MI, be cautious of Valsalva with resistance training -Cardiac surgery: LE resistance training can be initiated immediately, in the absence of peri-operative MI. UE resistance training should be avoided until soft tissue and bony healing has occurred: 6-8 weeks. -Post-transcatheter procedure (PTCA, other): minimum of 3 weeks following procedure and 2 weeks of consistent participation in a supervised CR endurance training program. -No evidence of the following conditions: congestive heart failure, uncontrolled dysrhythmias, severe valvular disease, uncontrolled hypertension and unstable symptoms. Exercise Prescription: -Start with low resistance (one set of 10-15 reps) and progress slowly -Resistance can include: -Weights, 50% or more of maximum weight used to complete one repetitition (1RM) -Elastic bands -Light (1-5 lb) cuff and hand weights -Wall pulleys -Perceived exertion (RPE-Borg scale) should range from 11 to 13 (“light to somewhat hard”), but this needs to be correlated to hemodynamic response to activity. -Rate pressure product should not exceed that prescribed during endurance exercise Rehab Guidelines for Arterial Disease: 1. Risk factor modification 2. Limb protection a. Avoid excessive strain, protection of extremities from injury and extremes of temperature b. Bed rest may be required if gangrene, ulceration, acute arterial disease are present 3. Exercise Training for pts with PAD: a. May result in improved functional capacity, improved peripheral blood flow via collateral circulation and muscle oxidative capacity. b. Consider interval training with frequent rests c. Walking program: intensity such that pt reports 1 on claudication scale within 3-5 minutes, stopping if they reach a 2 (until pain subsides), total of 30-60 minutes (intervals as necessary), 3-5 days per week. d. Record time of pain onset and duration e. Non-weight bearing exercise (cycle ergometry, arm ergometry) may be necessary in some pts; less effective in producing a peripheral conditioning effect. f. Well-fitting shoes essential; with insensitive feet, teach techniques of proper foot inspection and care. g. Beta blockers for treatment of HTN or cardiac disorders may decrease time to claudication or worsen symptoms. h. Pentoxifylline, dipyridamole, aspirin and warfarin may improve time to claudication. i. High risk for CAD. 4. Lower extremity exercise: a. Modified Buerger-Allen exercises: postural exercises plus active plantar and dorsiflexion of the ankle; active exercises improve blood flow during and after exercise; effects less pronounced in pts with PAD. b. Resistive calf exercises: most effective method of increasing blood flow. 5. Medical treatment: a. Medications to decrease blood viscosity, prevent thrombus formation (heparin) b. Vasodilators: controversial c. Calcium channel blockers in vasospastic disease 6. Surgical management: a. Atherectomy, thromboembolectomy, laser therapy b. Revascularization: angioplasty or bypass grafting c. Sympathectomy: results in permanent vasodilation, improvement in blood flow to skin d. Amputation when gangrene is present _____________________________________________________________________________________ Rehab Guidelines for Venous Disease: 1. Deep vein thrombophlebitis (DVT): a. Early stages may be asymptomatic; symptomatic pts demonstrate dull ache, pain, tenderness in calf; may also see slight edema or fever. b. Acute: activity limited until a dose of low molecular weight heparin, then ambulation permitted. Compression stockings (>30-40 mm Hg) can assist with pain control c. Anticoagulation medications 2. Chronic venous insufficiency (CVI) a. Management of edema: i. Positioning: extremity elevation, minimum of 18 cm above heart. Encourage pts to elevate leg as much as possible and avoid the dependent position b. Compression therapy i. Bandages (elastic, tubular); applied within 20 minutes of rising ii. Paste bandages (Unna boot). Gauze impregnated with zinc oxide, gelatin and glycerine; applied for 4-7 days (less with some wounds) iii. Graduated compression stockings (Jobst), at least 30 mm Hg iv. Compression pump therapy, used for a 1-2 hour session twice daily v. Red flag: consider consequences of compression therapy to a limb with an ankle-brachial index (ABI) <0.8 or with evidence of active cellulitis or infection 3. Exercise a. Active ankle exercises: emphasis on muscle pump exercises (dorsiflexion/planatarflexion, foot circles) b. Cycle ergometry in sitting or attached to foot of bed c. Early ambulation as soon as pt is able to get out of bed, 3-4 times a day. Patient education: meticulous skin care Severe conditions with dermal ulceration may require surgery (ligation and vein stripping, vein grafts, valvuloplasty. _____________________________________________________________________________________ Rehab Guidelines for lymphatic Disease: 1. Phase 1 Management: edema secondary to lymphatic dysfunction a. Short stretch compression bandages, worn 24 hours/day b. Manual lymph drainage (MLD) with complete decongestive therapy i. Massage and passive ROM to assist lymphatic flow (Vodder techniques, modifications by Askonk. Leduc, Fodi) ii. Emphasis is on decongesting proximal segments first (trunk quadrant), then extremities, directing flow distal to proximal iii. Compression using multilayered padding and short-stretch bandages 1. Bandages have low resting pressure and high working pressure 2. Bandages maintain limb after techniques applied to reduce limb 3. Decongestive exercises with padding in place. Activate muscles in extremity. Work trunk and limb girdle first, then limb muscles from proximal to distal. Performed with compression bandages on. 4. Certified specialists (certified lymphedema therapist) c. Functional activities: i. Walking program, cycling ii. Water-based programs: swimming iii. Tai chi and balance activities iv. ADL training v. RED FLAG: strenuous activities, jogging and ballistic movements are contraindicated, as they are likely to exacerbate lymphedema. vi. Signs of lymph overload: discomfort, aching or pain in proximal lymph areas (axilla or inguinal areas), change in skin color. If any of these are present, discontinue activity. d. Meticulous skin care: hygiene, nail care. e. Contraindicated modalities: i. Ice, heat, hydrotherapy, saunas, contract baths, paraffin; all cause vasodilation and increase lymphatic load of water ii. No electrotherapeutic modalities greater than 30 Hz. f. Compression garments at end of Phase 1. g. Red flag: excessively high pressures will occlude superficial lymph capillaries and restrict fluid absorption 2. Phase II Management (self-management) a. Skin care b. Compression garments c. Exercise d. Lymphedema bandaging at night e. MLD as needed f. Compression pumps: use with caution; limited benefits g. RED FLAG: pressures higher than 45 mm Hg are contraindicated, as they can cause lymphatic collapse; contraindicated with soft tissue injury 3. Education a. Skin and nail care b. Self-bandaging, garment care c. Infection management d. Maintain exercise while preventing lymph overload _____________________________________________________________________________________ Basic Life Support and CardioPulmonary Resuscitation (CPR) 1. 2. 3. 4. 5. 6. Compressions come first, and then focus on airway and breathing. Only exception is newborn babies. No more looking, listening, and feeling. Call 911 immediately. Push a little harder for adult CPR: at least 2 inches deep on chest. Push a little faster: about 100 compressions/min. Hands only CPR for untrained lay rescuers. Don’t stop pushing, no interruptions. First Aid: 1. External bleeding a. Minor bleeding: i. Usually clots within 10 minutes ii. If pt/client is taking aspirin or nonsteroidal anti-inflammatory drugs, clotting may take longer b. Severe bleeding characteristics: i. Blood spurting from a wound ii. Blood fails to clot even after measures to control bleeding have been taken iii. Arterial bleed: high pressure, spurting, red iv. Venous bleed: low pressure, stead flow, dark red or maroon blood v. Capillary bleed: low pressure, oozing, dark red blood c. Controlling external bleeding: i. Use standard precautions such as wearing gloves ii. Apply gauze pads using firm pressure. If no gauze available, use a clean cloth, towel, a gloved hand or pts own hand. If blood soaks through, do not remove any gauze, add additional layers. iii. Elevate the part if possible unless it is deformed or it causes significant pain when elevated. iv. Apply a pressure bandage, such as roller gauze, over the gauze pads. v. If necessary, apply pressure with the heel of your hand over pressure points. The femoral artery in the groin and the brachial artery in the medial aspect of the upper arm are two such points. vi. Monitor A, B, Cs and overall status of the pt. Administer supplemental oxygen if nearby. Seek more advanced care as necessary 2. Internal bleeding: a. The possible result of a fall, blunt force trauma or a fx rupturing a blood vessel or organ. b. Severe internal bleeding may be life-threatening c. Severe internal bleeding characteristics: i. Ecchymosis (black and blue) in the injured area ii. Body part, especially the abdomen, may be swollen, tender, and firm iii. Skin may appear blue, gray or pale and may be cool or moist iv. Respiratory rate in increased v. Pulse rate is increased and weak vi. Blood pressure is decreased vii. Pt may be nauseated or vomit viii. Pt may exhibit restlessness or anxiety ix. Level of consciousness may decline d. Management of internal bleeding i. If minor, follow RICE procedure ii. Major internal bleeding 1. Summon advanced medical personnel 2. Monitor A, B, Cs and vital signs 3. Keep the pt comfortable and quiet. Keep them from getting chilled or overheated. 4. Reassure pt or victim 5. Administer supplemental oxygen if available and nearby 3. Shock (hypo-perfusion) a. Failure of the circulatory system to perfuse vital organs b. At first, blood is shunted from the periphery to compensate i. The victim may lose consciousness as the brain is affected ii. The heart rate increases, resulting in increased oxygen demand iii. Organs ultimately fail when deprived of oxygen iv. Heart rhythm is affected, ultimately leading to cardiac arrest and death c. Types and causes of shock: i. Hemorrhagic: severe internal or external bleeding. ii. Psychogenic: emotional stress causes blood to pool in body away from the brain iii. Metabolic: loss of body fluids from heat or severe vomiting or diarrhea iv. Anaphylactic: allergic reaction from drugs, food or insect stings v. Cardiogenic: MI or cardiac arrest results in pump failure vi. Respiratory: respiratory illness or arrest results in insufficient oxygenation of the blood vii. Septic: severe infections cause blood vessels to dilate viii. Neurogenic: traumatic brain injury, spinal cord injury or other neural trauma causes disruption of blood vessel dilation/constriction d. Signs and symptoms: i. Pale, gray or blue, cool skin ii. Increased, weak pulse iii. Increased respiratory rate iv. Decreased blood pressure v. Irritability or restlessness vi. Diminishing level of consciousness vii. Nausea or vomiting e. Care for shock: i. Obtain a history if possible ii. Examine the victim for airway, breathing, and circulation and bleeding iii. Assess level of consciousness iv. Determine skin characteristics and perform capillary refill test of finger tips 1. Capillary refill test: squeeze fingernail for 2 seconds 2. In healthy individuals, the nail will blanch and turn pink when pressure is released 3. If nail bed does not refill and turn pink within 2 seconds, the cause could be that blood is being shunted away from the periphery to vital organs or to maintain core temperature. 4. Treat any specific condition if possible: control bleeding, splint a fx, Epipen for anaphylaxis and so on. 5. Keep the victim form getting chilled or over heated 6. Elevate the legs 12 inches unless there is suspected spinal injury or painful deformities of the lower extremities 7. Reassure the victim and continue to monitor A, B, Cs 8. Administer supplemental oxygen if nearby 9. Do not give any food or drink o Bronchial Drainage Upper lobes Apical segments Bed or drainage table flat Pt leans back on pillow at 30-degree angle against therapist. Therapist claps with markedly cupped hand over area between the clavicle and top of the scapula on each side. Upper lobes posterior segments Bed or drainage table flat Pt leans over folded pillow at 30 degrees angle Therapist stands behind and claps over upper back on both sides Upper lobes anterior segments Bed or drainage table flat Pt lies on back with pillows under knees Therapist claps between clavicle and nipple on each side Left Upper lobe Lingular Segments Foot of table or bed elevated 16 inches Pt lies head down on right side and rotates ¼ turn backward. Pillow may be placed from behind shoulder to hip. Knees should be flexed Therapist claps with cupped hands over left nipple area Right Middle Lobe Foot of table or bed elevated 16 inches o Pt lies head down on left side and rotates ¼ turn backward. Pillow may be placed behind from shoulder to hip. Knees should be flexed Therapist claps over right nipple area Lower Lobe anterior basal segment Foot of table or bed elevated 20 inches Pt lies on side head down, pillow under knees Therapist claps with cupped hands over lower ribs. Draining left lie on right, Draining right Lie on left Lower lobes Posterior Basal segments Foot of table or bed elevated 20 inches Pt lies on abdomen, head down with pillow under hips. Therapist claps over lower ribs close to spine on each side Lower Lobes Superior Segments Babe or table flat Pt lies on abdomen with two pillows under hips Therapist claps over middle of back at tip of scapula on either side of spine Lower Lobes Lateral basal segments Foot of table or bed elevated 20 inches Pt lies on abdomen, head down and rotates ¼ turn upward. Upper leg is flexed over pillow for support. Therapist claps over uppermost portion of lower ribs Drainage of left lie on right, Drainage of right lie on left. Airway clearance techniques Cough: Pt should be asked to cough in the upright position, if possible, after each area of lung has been treated. Huffing: more effective in Pt with collapsible airways. Prevents the high intrathoracic pressure that causes premature airway closure. Ask pt to inhale deeply Immediately, the pt forcibly expels the air, saying ha, ha Assisted cough: the therapist hands or fist become the force behind the pt exhaled air. Used when the pts abdominal muscles cannot generate an effective cough. Position the Pt against a solid surface; supine with head of bed or table flat or in a Trendelenburg position, or sitting with wheelchair against the wall. The therapist’s hand is placed below the pts subcostal angle Pt inhales deeply As the pt attempts to cough, the therapist hand pushes inward and upward, assisting the rapid exhalation of air. Any secretions raised should be removed by a suction catheter if expectoration is problematic Tracheal stimulation: used with pts who are unable to cough on command. The therapist finger or thumb is placed just above the substernal notch, and a quick inward and downward pressure on the trachea elicits the cough reflex. Endotrachel suctioning: used only when the above airway clearance techniques fail to adequately remove secretions. (10-15 seconds) Airway Clearance Techniques: Airway clearance techniques are intended to manage or prevent the consequences of impaired mucociliary transport or the inability to protect the airway (impaired cough). The techniques may include breathing strategies, manual and mechanical techniques, and postural drainage. Indications for Airway Clearance: -Restrained secretions in the central airways -Prophylaxis against postoperative pulmonary complications -Obtain sputum for diagnostic analysis -Difficulty clearing secretions -Atelectasics caused by or suspected of being caused of mucus plugging Technique: Active Cycle of Breathing (ACB) What is it: Procedure: ACB was developed under the name “forced expiratory technique” to assist secretion clearance in pts with asthma. The name of the technique was changed to “active cycle of breathing” to emphasize that ACB always couples breathing exercise with the •Breathing control: Gentle, relaxed breathing (may be diaphragmatic breathing at pts tidal volume and resting respiratory rate for 5-10 seconds, or as long as the pt needs in order to prepare for the next phase. •Thoracic expansion exercise: 3-4 deep, slow, Precautions/Contraindica tions: -Splinting post-operative incisions to achieve adequate expiratory force -Bronchospasm or hyperreactive airways huff cough. It includes 3 phases: breathing control, thoracic expansion exercises, and forced expiratory technique. Autogenic Drainage (AD) relaxed inhalations to inspiratory reserve with passive exhalation –Chest percussion, vibration or shaking may be combined with exhalation •Forced expiratory technique: 1 or 2 huffs at mid to low lung volumes with the glottis open into the expiratory reserve volume; a brisk adduction of the upper arms may be added to self-compress the thorax AD uses controlled The pt is sitting upright in a breathing to mobilize chair with back support. secretions by varying Controlled breathing at expiratory airflow without three lung volumes: using postural drainage -“Unsticking phase”: slowly positions or coughing. The breathe in through nose at theory is to improve airflow low-lung volumes followed in small airways to facilitate by a 2-3 second breaththe movement of mucus. AD hold to allow collateral requires patience to learn, ventilation to get air so this may not be suitable behind the secretions, then for young children and pts exhale down into the who are not motivated or expiratory reserve volume. easily distracted. Because -“Collecting phase”:breath AD does not require the at tidal volume, assistance of another person interspersed by 2-3 second or equipment, it can be breath holds performed anywhere and -“Evacuating phase”: during activities of daily deeper inspirations from Requires motivation and concentration to learn living. Directed cough and huffing A directed cough tries to compensate for the pts physical limitations to elicit a maximum forced exhalation. Huffing is a forced expiratory maneuver performed with the glottis open. The maneuver is similar to fogging a pair of glasses with your breath. Although a huff does not produce the same airflow velocity as a cough, the potential for airway collapse is less. Huffing may be reinforced by a quick adduction of the arms to self-compress the chest wall. High-frequency airway oscillation The Acapella & Flutter are handheld devices that combine positive expiratory low-to-mid inspiratory reserve volume, with breath holding followed by a huff Exhalation through pursedlips may be used to control expiratory flow rate -An average treatment is 30-45 min Cough: Inhale maximally , close the glottis and hold breath for 2-3 seconds; contract the expiratory muscles to produce increased intrathoracic pressure against the closed glottis; cough sharply 2-3 times through a slightly open mouth; post-surgical pts may need to splint the chest or abdomen by applying pressure over the incision with a pillow or blanket roll. Huff: Inhale deeply through an open mouth; contract the abdominal muscles during a rapid exhalation with the glottis open, saying, “Ha, ha, ha.” -Place the device in the mouth the lips firmly sealed around the -Inability to control possible transmission of infection from pts suspected or known to have pathogens transmittable by droplets -Elevated intracranial pressure or known intracranial aneurysm -Reduced coronary artery perfusion (acute MI) -Acute unstable head, neck or spine injury -Potential for regurgitation/aspiration -Acute abdominal pathology, abdominal aortic aneurysm, hiatal hernia or pregnancy -Untreated pneumothroax -Osteoporosis -Flail chest -Pt tolerance of increased work of breathing (acute asthma, COPD) pressure and high frequency airway vibrations to mobilize mucus secretions in the airways Postural drainage, percussion, and vibration Postural drainage consists of positioning the pt so that gravity will help drain bronchial secretions from specific lung segments toward the central airways where they can be removed by cough or mechanical aspiration. Percussion, also known as cupping & clapping, is the rhythmic clapping or striking of the thorax with a cupped hand or mechanical percussor directly over the lung segment being drained. This rhythmic sequence should last for several minutes and should not be painful. Vibration is the application of a fine, tremulous action on the chest wall over the mouthpiece -Inhale slowly to 75% of a full breath -Hold the breath for 2-3 seconds -Exhale through the device for 3-4 seconds -Repeat 10-20 breaths -Remove the device and perform 2-3 coughs or huffs to raise secretions Postural drainage: The pt assumes the appropriate position for the affected lung segment. Standard positions may be modified as the pts conditions and tolerance warrant. Maintain each position for 2-3 minutes. Percussion & vibration: Place the pt in the appropriate postural drainage position; cover the skin overlying the affected segment with a thin material (towel, t-shirt, hospital gown); therapist rhythmically strikes the chest with a cupped hand for 2-3 minutes per lung segment; therapist places one hand on top of the other over affected area or -Intracranial pressure >20 mm Hg -Recent facial, oral, or skull surgery or trauma -hemodynamic instability -Acute sinusitis -Nosebleed -Esophageal surgery -Active hemoptysis -Nausea All positions are contraindicated for: -ICP >20 mm Hg -Head and neck injury until stabilized -Active hemorrhage with hemodynamic instability -Recent spinal surgery or acute spinal injury -Active hemoptysis -Empyema -Bronchopleural fistula -Pulmonary edema associated with CHF -Large pleural effusion -Confused or anxious pts who do not tolerate position changes -Rib fx, with or without fail chest -Surgical wound or healing tissue Trendelenburg position is lung segment being drained in the direction the ribs move during exhalation. It may be performed manually or with a mechanical vibrator. Vibration should be performed during exhalation. one hand on each side of the rib cage; vibrate the chest wall as the pt exhales by tensing the muscles of the hands and arms while applying moderate pressure downward; the maneuver is performed in the direction in which the ribs move on expiration; encourage the pt to cough or huff after 2-3 vibrations contraindicated for: -Uncontrolled HTN -Distended abdomen -esophageal surgery -Recent gross hemoptysis related to lung carcinoma -Uncontrolled airway at risk for aspiration )tube feeding or recent meal) -Subcutaneous emphysema -Recent epidural spinal infusion or spinal anesthesia -Recent skingrafts, or flaps on the thorax -Burns, open wounds, and skin infections -Recently placed transvenous or subcutaneous pacemaker -Suspected pulmonary tuberculosis -Lung contusion -Bronchospasm -Osteomyelitis of the ribs -Osteoporosis -Complaint of chest wall pain Breathing Exercises: Exercise Diaphragmatic Breathing (DB): involves breathing predominately with the diaphragm while minimizing the action of accessory muscles and motion of the upper rib cage during inspiration Indications Precautions/Contra Procedure -Post surgical pt with pain in the chest wall or abdomen, or restricted mobility -Pt learning active cycle of breathing or autogenic drainage airway clearance techniques -Dysnpea at rest or with minimal activity -Inability to perform ADLs due to dyspnea or inefficient breathing pattern -Moderate to severe COPD & marked hyperinflation of the lungs with diaphragmatic movement -Pts with paradoxical breathing patterns or who demonstrate increased inspiratory muscle effort, and increased dyspnea during DB -Semi-fowler’s positions is a good starting position -Sniffing can be used to facilitate contraction of the diaphragm -Have the pt place one hand on the upper chest and the other just below the rib cage -Instruct the pt to: “Breathe in slowly through your nose so that your stomach moves out against your hand. The hand on your chest should remain as still as possible. Feel your abdomen gently rise into your hand. Exhale through pursed lips, let the hand on your abdomen descend, while the hand on your upper chest Expected Outcomes -Decreased respiratory rate -Decrease use of accessory muscles of inspiration -increase tidal volume -Decrease respiratory flow rate -Subjective improvement of dyspnea -Improve tolerance for activity Inspiratory Muscle training (IMT): attempts to strengthen the diaphragm and intercostals muscles. Two different IMT devices provide different modes of training: flow resistive breathing and threshold breathing. During flow resistive breathing, the pt inspires through a mouthpiece and adapter with an adjustable diameter. Decreasing the diameter increases the resistance to breathing, provided that breathing rate, tidal volume, and inspiratory time are kept constant. Threshold loading requires a buildup Impaired inspiratory muscle strength and/or a ventilatory limitation to exercise performance -Clincal signs of inspiratory muscle fatigue -Tachypnea -Reduced tidal volume -Increased PaCO2 -Bradypnea and decreased minute ventilation remains still.” Measure the pts maximum inspiratory pressure (MIP) with a manometer. Use the measured MIP to calculate the training load. Using the threshold inspiratory muscle trainer: Place mouthpiece in mouth and inhale with enough force to open the valve, the higher the setting the greater the effort needed, begin training with the setting that elicits 30% to 40% of the pts MIP. Pt breathes at tidal volume for 5-15 min. Using the PFLEX Inspiratory muscle trainer: Place PFLEX in mouth and breath at tidal volume, setting 1 -Increased inspiratory muscle strength and endurance; decrease dysnpea at rest and during exercise; increase functional exercise capacity of negative pressure before flow occurs through a valve that opens at a critical pressure. Threshold breathing provides consistent and specific pressure for IMT, regardless of how quickly or slowly pts breathe. Paced breathing and exhale with effort: Paced breathing is a strategy to decrease the work of breathing and prevent dyspnea during activity. It allows anyone who experiences shortness of breath to become less fearful of activity and exercise. Exhale with effort is a breathing strategy employed provides the least resistance, begin training that elicits 30-40% level MIP for 10-15 min daily. -Pts with dysnpea at rest or with minimal activity -Inability to perform activity due to pulmonary limitation -Inefficient breathing pattern during activity Avoid valsalva maneuver during activity Perform activity at a tempo that does not exceed the pts breathing limitations; find a comfortable inspiration to expiration time to synchronize with the exertion phase of activity; synchronize breathing with components of the activity: inhale before or during the easier component of the activity, exhale Complete activity without dyspnea; decrease pts fear of becoming short of breath during activity during activity to prevent a pt from holding their breath. The technique breaks any activity into one or more breaths with inhalation during the resting or less active phase of the activity and exhalation during the movement or more active phase of the activity. during the more vigorous component of the activity, do not hold breath or rush through the activity. Walking: Inhale through the nose while walking 2 steps and then pause; exhale through pursed lips while walking 4 steps. Climbing stairs: inhale through the nose while standing, exhale through pursed lips while stepping up (or down) 1 or 2 stairs, remain on the step until breathing control is restored Lifting: inhale through the nose while standing or sitting; exhale through pursed lips while bending to reach the object; pause; Pursed-lip breathing (PLB) is a simple technique to reduce respiratory rate, reduce dyspnea, and maintain a small positive pressure in the bronchioles, which may help prevent airway collapse in pts with emphysema. Any pt who is SOB may use this technique. Tachypnea, dysnpea Forcing exhalation Segmental breathing: also known as localized breathing or thoracic expansion -Decreased intrathoracic lung volume, decreased chest wall lung compliance, None inhale through the nose while grabbing the object; exhale through pursed lips while standing up Semi-fowlers is a good position to initiate the breathing technique. Instruct the pt to: “breathe in slowly through your nose with the mouth closed for two counts. Pucker, or purse your lips as if you were going to whistle, then gently breathe out through pursed lips, as if trying to make a candle flame flicker, for a 4 count. Do not blow with force.” Position the pt: -sitting position for basal atelectasis -sidelying with affected lung -Decrease respiratory rate, relieve dyspnea, reduce arterial partial pressure of carbon dioxide, improve tidal volume, improve oxygen saturation, prevent airway collapse in pts with emphysema, increase activity tolerance -Increase chest wall mobility -Expand collapsed alveoli via airflow through collateral ventilation exercises, is intended to improve regional ventilation and prevent and treat pulmonary complications after surgery. It is based on the presumption that asymmetrical chest wall motion may coincide with underlying pathology (pneumonia, pleuritic chest wall pain, retained secretions) and that inspired air can be directed to a particular area by facilitation or inhibition of chest wall movement through proper hand placements, verbal cues or coordination of breathing. Sustained maximal inhalation with incentive increased flow resistance from decreased lung volume, ventilation: perfusion mismatch -Decreased intrathoracic lung volume -Decreased chest -Pt is not cooperative or is unable to understand or uppermost -Postural drainage positions with affected lung uppermost to assist with secretion removal -Therapist applies firm pressure at the end of exhalation to the pts chest wall overlying the area to be expanded -pt inhales deeply and slowly expanding the rib cage under the therapist hands -Therapist reduces hand pressure during the pts inhalation channels -assist with secretion removal -Hold the incentive spirometer in a vertical position -Absence of or improve improvement in signs of atelectaiss spirometer: (SMI), wall lung demonstrate -Have the pt -Decreased a maximal compliance proper use of the exhale respiratory rate inspiratory effort -Increased flow incentive completely, then -Resolution of is held for 3 or resistance from spirometer seal his lips fever more seconds at decreased lung -Pt is unable to around the -Normal pulse the point of volume deep breathe mouthpiece rate maximum -ventilation: effectively (with -breath in slowly -Normal chest xinspiration before perfusion (V:Q) vital capacity less and deeply ray exhalation. Many mismatch than 10 mL/Kg or through the -Improved paO2 airway clearance -Atelectasis or risk inspiratory capacity mouth, raising the -Increased forced techniques of atelectasis due less than 1/3 of ball or piston of vital capacity and include SMI to to thoracic and predicted) the spirometer peak expiratory compensate for upper abdominal -Pts with moderate -Encourage the pt flows asynchronous surgery to severe COPD move the ventilation, to -Restrictive lung with increased diaphragm and promote air defect associated respiratory rate and expand the lower passage past with quadriplegia hyperinflation chest, not the mucus and/or upper chest obstructions in dysfunctional -Hold the breath airways, and to diaphragm for at least 3 maximize alveolar seconds and note expansion. SMI is the highest level also called the piston reaches incentive -Perform SMI spirometry when independently 5using a device that 10 breaths per provides visual or hour when awake other feedback to encourage the pt to take long, slow, deep inhalations. o Abdominal Breathing Used when abdominal muscles are too weak to provide an effective cough. Abdominal splinting: used when the abdominal muscles cannot provide the necessary support needed for passive exhalation. Glossopharyngeal breathing (air gulping) can also be taught to assist coughing. Positions to relieve Dyspnea: A number of positions may be used to provide relief from dyspnea. The choice of position will depend on the circumstances at the time. The forward leaning position often provides relief of dyspnea to pts with lung disease. Forward leaning with arm support optimizes the length-tension relationship of the diaphragm and allows the pectorals minor and pectoralis major muscles to assist in elevating the rib cage during inspiration. The positions may be combined with other breathing techniques. Reverse Trendelenburg position: The opposite of the Trendelenburg position, the reverse Trendelenburg position places a person in supine with their head above their trunk and lower extremities, decreasing the weight of the abdominal contents on the diaphragm and reducing the resistance to movement during breathing. Semi-Fowler’s position: The semi-fowler’s position places a pt in supine with the head of the bed elevated to 45° and pillows under the knees for support and maintenance of a proper lumbar curve. This position is used often for pts with congestive heart failure or other cardiac conditions. Musculoskeletal System—Physical Therapy Examination 1. Anatomy and Physiology of the MS System Muscle Deltoid--Clavicular part Acromial part Spinal part Origin Lateral clavicle Acromion Scapular spine Insertion Humerus (deltoid tuberosity) Action Flexion, IR, ADD Abduction Extension, ER, ABD Innervation Axillary n. C5, C6 Supraspinatus Greater tuberosity Abduction Infraspinatus Supraspinous fossa Infraspinous fossa Greater tuberosity ER Teres Minor Lateral border Greater tuberosity Subscapularis Subscapular fossa Lesser tuberosity ER, weak adduction IR Pectoralis Major-Clavicular part Sternocostal part Abdominal part Clavicle Sternum and costal cartilages 16 Rectus sheath Humerus (crest of greater tuberosity) Coracobrachialis Coracoid process Humerus Pectoralis Minor 3rd to 5th ribs Coracoid process Serratus Anterior Superior part Intermediate part Inferior part 1st to 9th ribs Scapula (medial border) Trapezius 1.Spinous process 1.Clavicle Entire muscle: adduction, IR Clavicular & sternocostal parts:flexion; assist in respiration when shoulder is fixed Flexion, ADD, IR Draws scapula downward, causing inferior angle to move posteromedially; rotates glenoid inferiorly Lowers the raised arm, draws scapula laterally forward; elevates ribs when shoulder is fixed, rotates scapula laterally 1.Upward Suprascapular n. C4-C6 Suprascapular n. C4-C6 Axillary n. C5,C6 Subscapular n. C5, C6 Medial & lateral pectoral nn. C5-T1 Musculocutaneous C6, C7 Medial & lateral pectoral nn. C6-T1 Long thoracic n C5-C7 Accessory n (CN 1.Descending part 2.Transverse part 3.Ascending part C1-C7 2.Spinous process T1-T4 3.spinous process T5-T12 2.Acromion 3.Scapular spine rotation, rotates gleniod superiorly, tilts head to SAME side and rotates to OPPOSITE 2.Draws scapula medially 3.Draws scapula medially downward Entire muscle:steadies scapula on thorax XI), cervical plexus C3, C4 Muscle Levator Scapulae Origin Transverse process C1-C4 Insertion Scapula, superior angle Innervation Dorsal scapular n. C4-C5 Rhomboid minor Spinous process C6,C7 Rhomboid major Spinous process T1-T4 vertebrae Steadies scapula, upward rotation Dorsal scapular n. C4-C5 Latissimus Dorsi Veretbral part Scapular part Costal part Iliac part Spinous process T7-T12 vertebrae Scapula:inferior angle 9th to 12th ribs Iliac crest Scapula (inferior angle) Medial border above scapular spine Medial border below scapular spine Crest of lesser tuberosity of the humerus Action Upward rotation, inclines neck to SAME side Steadies scapula, upward rotation IR, ADD, extension, “cough muscle” Thoracodorsal n. C6-C8 IR, ADD, extension Lower subscapular n. C5-C7 Elbow: flexion, Musculocutaneous Teres major Biceps brachii Supraglenoid Crest of lesser tuberosity of the humerus Radial tuberosity Dorsal scapular n. C4-C5 Long head Short head tubercle of scapula Coracoid process of scapula Brachialis Humerus (distal half of anterior surface) Scapula (infraglenoid tubercle) Posterior humerus (medial septum) Posterior humerus (lateral septum) Lateral epicondyle of humerus Ulnar tuberosity Triceps brachii Long head Medial head Lateral head Anconeus Muscle Superfical Group Pronator teres Flexor carpi radialis Palmaris Longus supination (when elbow flexed powerful supinator) Shoulder:flex, abd, and IR of humerus Flexion of elbow n. C5, C6 Olecranon of ulna Elbow: extension Shoulder-long head:extension and ADD Radial n. C6-C8 Olecranon of ulna Extends the elbow and tightens joint Radial n. C6-C8 Origin Humeral head:medial epicondyle of humerus Ulnar head: coronoid process Medial epicondyle Insertion Lateral radius (distal to supinator insertion) Action Elbow: weak flexor Forearm: pronation Innervation Median n. C6, C7 Base of 2nd metacarpal Median n. C6, C7 Medial epicondyle Palmar aponeurois Wrist: flexion & ABD (radial deviation of hand) Elbow: weak flexion Wrist: flexion tightens palmar aponeurosis Musculo. C5,C6 & radial C7 Median n. C7, C8 Flexor carpi ulnaris Intermediate Group-Flexor digitorum superficialis Deep Group-Flexor digitorum profundus Flexor pollicis longs Humeral head: medial epicondyle Ulnar head: olecranon Humeral head: medial epicondyle Ulnar head: coronoid process Ulna Pisiform; hook of hamate; base of 5th metacarpal Wrist: flexion and ADD (ulnar deviation) Ulnar n. C7-T1 Sides of middle phalanges of 2nd to 5th digits Elbow: weak flexor Wrist: MCP, and PIP joints of 2nd to 5th digits: flexion Wrist, MCP, PIP, and DIP of 2nd to 5th digits: flexion Wrist: flex, abd CMC of thumb:flexion MCP & IP of thumb:flexion Hand: pronation Distal radioulnar joint: stabilization Elbow: flexion Forearm: semipronation Elbow: weak flexion Wrist: extension & ABD Elbow: weak flexion Wrist: extension & ABD Median n. C8, T1 Action Wrist: extension Innervation Radial n. C7, C8 Radius (midanterior surface) Distal phalanges of 2nd to 5th digits (palmar surface) Distal phalanx of thumb (palmar surface) Pronator quadrates Distal ulna (anterior surface) Distal radius (anterior surface) Brachioradialis Distal humerus Styloid process of the radius Extensor carpi radialis longus 2nd metacarpal base Extensor carpi radialis brevis Lateral supracondylar ridge of distal humerus Lateral epicondyle of humerus Muscle Extensor Origin Lateral epicondyle Insertion Dorsal digital 3rd metacarpal base Median n. C8, T1 Ulanr n. C8, T1 Median n. C7,C8 Median n. C7, C8 Radial n. C5, C6 Radial n. C6, C7 Radial n. C7, C8 expansion of 2nd to 5th digits digitorum Extensor digiti minimi Lateral epicondyle 5th digit Extensor carpi ulnaris Supinator Lateral epicondyle, ulnar head Olecranon, lateral epicondyle, annular ligament Radius and ulna Base of 5th metacarpal Radius Extensor pollicis brevis Radius (posterior surface) Base of proximal phalanx of thumb Extensor pollicis longus Ulna (posterior surface) Base of distal phalanx of thumb Extensor indicis Ulna (posterior surface) Lumbricals Tendons of flexor digitorum Posterior digital extension of 2nd digit 2nd-5th digits on dorsal digital Abductor pollicis longus Base of 1st metacarpal MCP, PIP, and DIP of 2nd to 5th digits: Extension/ABD of fingers Wrist: ext, ulnar abd of hand MCP, PIP, & DIP of 5th digit: ext and abd Wrist: ext, add Radial n. C7, C8 Radial n. C7, C8 Supination Radial n. C6, C7 Radiocarpal joint: abd of hand Carpometacarpal joint of thumb: abd Radiocarpal joint: abd Carpometacarpal & MCP of thumb: ext Wrist: ext, abd CMC of thumb: add MCP & IP of thumb: ext Wrist: ext MCP, PIP, & DIP of 2nd digit: ext 2nd-5th digits— MCP: flexion Radial n C7, C8 Radial n. C7, C8 Radial n. C7, C8 Radial n. C7, C8 Median n C8, T1 profundus Muscle Iliopsoas 1.Psoas minor 2.Psoas major 3.Iliacus Origin 1.T12-L1 vertebrae 2.T12-L4 & associated vertebral disks; L1L5 vertebrae 3.Iliac fossa Gluteus maximus Sacrum, ilium Gluteus medius Ilium Gluteus minimus Ilium Tensor fasciae latae ASIS Piriformis Pelvic surface of expansion Insertion 1.Iliopectineal arch 2&3. Lesser trochanter PIP and DIP: extension Action 1.Assists in upward rotation of the pelvis 2&3: Hip joint:flex, ER Lumbar spine:bends trunk laterally to same side; contraction raises the trunk from the supine position Upper Entire muscle: ext, ER of hip fibers:iliotibial in sagittal and coronal tract Lower fibers: planes gluteal tuberosity Upper: abd Lower: add Greater trochanter ABD, stabilizes pelvis Ant part: flex, IR Pos part: ext, ER Greater trochanter ABD, stabilizes pelvis Ant part: flex, IR Pos part: ext, ER Iliotibial tract Tenses the fascia lata Hip joint: abd, flex, IR Greater trochanter ER, ABD, ext; stabilizes hip Innervation 1&2: direct branches from the lumbar plexus (psoas) L2-L4 3. Femoral n. L2-L4 Inferior gluteal n. L5-S2 Superior gluteal n. L4-S1 Superior gluteal n. L4-S1 Superior gluteal n. L4-S1 Direct branches sacrum Obturator internus Medial surface of greater trochanter ER, ADD, and ext Medial surface greater trochanter ER, ADD, and ext Quadratus femoris Inner surface of obturator membrane Superior: ischial spine Inferior: ischial tuberosity Ischial tuberosity Intertrochanteric crest of femur ER, ADD of hip Pectineus Pecten pubis Femur Muscle Adductor longus Origin Superior pubic ramus Inferior pubic ramus Inferior pubic ramus Insertion Femur ADD, ER, & slight flexion; stabilizes pelvis Action ADD, flex (up to 70 degrees) ext (past 80 degress of flex) ADD, flex (up to 70 degrees) ext (past 80 degress of flex) Hip: ADD flex Knee: flex & IR Gemelli Adductor brevis Gracilis Obturator externus Adductor minimus Adductor magnus Outer surface of obturator membrane Inferior pubic ramus Inferior pubic ramus; ischial tuberosity Sartorius ASIS Rectus femoris AIIS Femur Tibia (medial border of tuberosity (SGT) Trochanteric fossa of femur Medial lip of linea aspera Medial lip of linea spine; adductor tubercle of the femur Medial to tibial tuberosity Tibial tuberosity from sacral plexus S1-S2 Direct branches from sacral plexus L5, S1 Direct branches from sacral plexus L5, S1 Direct branches from sacral plexus L5, S1 Femoral n, obturator n, L2, L3 Innervation Obturator n. L2-L4 Obturator n. L2, L3 Obturator n. L2, L3 Hip:ADD & ER; stabilizes pelvis Obturator n L3, L4 ADD , EXT, slight flexion of hip ADD, EXT, slight flexion; stabilizes pelvis Obturator n. L2-L4 Hip: flex, abd, ER Knee: flex, IR Hip: flex Femoral n. L2, L3 Obturator L2-L4; tibial n. L4 Femoral n. L2-L4 Vastus medialis Both sides of tuberosity Both sides of tuberosity Tibial tuberosity Head of fibula Semimembranosus Linea aspera (medial lip) Linea aspera (lateral) Femoral shaft Iscial tuberosity; lateral lip of linea aspera Ischial tuberosity Semitendinosus Ischial tuberosity Medial to tibial tuberosity Fibularis longus Fibula head Medial cuneiform (plantar side); 1st metatarsal base Fibularis brevis Fibula Tibialis anterior Upper 2/3 of tibia Extensor hallucis longus Fibula-middle third 5th metatarsal base Medial cuneiform & 1st metatarsal base (plantar surface) 1st toe at base of DIP Extensor digitorum longus Fibula head; tibia lateral condyle 2nd to 5th toes at the base of DIP Fibularis tertius Distal fibula Gastrocnemuis Femur (medial & 5th metatarsal base Calcaneal Vastus lateralis Vastus intermedius Biceps femoris Medial tibial condyle Knee: ext Knee: ext Femoral L2-L4 Knee: ext Femoral L2-L4 Knee: ext Hip: extends, stabilizes pelvis Knee: flex, ER Hip: extends, stabilizes pelvis Knee: flex, IR Hip: extends, stabilizes pelvis Knee: flex, IR Talocrural joint:PF Subtalar:eversion(pronation) Supports transverse arch of foot PF; eversion Femoral L2-L4 Tibial n L5S2/Common fibular L5-S2 Tibial n. L5-S2 Talocrural: DF Subtalar: inversion (supination) Tibial L5-S2 Superficial fibular n. L5, S1 Superficial fibular L5, S1 Deep fibular L4, L5 DF, active in eversion/inversion, ext of MTP and IP of big toe DF, eversion (pronation); extends MTP and IP of 2nd5th toes DF, eversion Deep fibular L5 Talocrural: PF Tibial S1, S2 Deep fibular L5, S1 Deep fibular L5, S1 Soleus lateral epicondyles) Fibula head, tibia tuberosity via Achilles Calcaneal tuberosity via Achilles Calcaneal tuberosity via Achilles Plantaris Femur (lateral epicondyle) Tibialis posterior Adjacent borders of tibia & fibula Flexor digitorum longus Flexor hallucis longus Tibia (posterior surface) Fibula (posterior surface) Popliteus Masseter Lateral femoral condyle Zygomatic arch Posterior tibial surface Mandibular angle Temporalis Temporal fossa Coronoid process Navicular tuberosity, cuneiforms, 2nd-4th metatarsal bases 2nd-5th distal bases 1st distal base Lateral pterygoid Medial pterygoid Sternocleidomastoid Sternum Clavicle Mastoid process Occipital bone Knee: flexion PF Tibial S1, S2 Negligible; may prevent compression of posterior leg musculature during knee flex PF, inversion (supination), supports the longitudinal and transverse arches Tibial S1, S2 PF, inversion, MTP and IP 2nd-5th: PF PF, inversion, MTP and IP 2nd-5th toes: PF; supports medial longitudinal arch Knee: flexion, IR (stabilizes knee) Elevates (adducts) and protrudes mandible Elevate (adduct) mandible Retract (retrude) mandible Unilateral: lateral movement (chewing) Bilateral: protrudes mandible (pulls disk forward) Unilateral: lateral movements (chewing) Elevates (adducts) mandible Unilateral: Tilts head to same side, rotates head to opposite side. Bilateral: Tibial n. L5-S2 Tibial n. L4, L5 Tibial n. L5-S2 Tibial n L4-S1 Mandibular (CN V) Mandubualr n. (CN V) Mandibular N. Mandibular n. Accessory (CN XI) Longus Capitis, Longus Colli, Rectus Capitis anterior, Rectus capitis lateralis Scalenes Rectus capitis posterior minor and major, Obliquus capitis inferior and superior extends head, aids in respiration Flexion C3-C6, C1-C2, C5C7 1st rib, 2nd rib Elevates upper ribs, bends cervical spine to same side, flexes neck Extends head, rotates head to same side Direct brances C3C8 Force Couple- is defined as two forces that act in opposite directions to rotate a segment around its axis of motion. Ex. Deltoid pulls the humerus up, rotator cuff pulls the humeral head down to allow smooth movement of the humeral head in the glenoid cavity. Ex. Trapezius and serratus anterior cause upward rotation of the scapula during arm elevation. Rhomboids, levator scapulae, and pec minor cause downward rotation with purposeful shoulder extension (chopping wood) Ex. Serratus anterior and pec minor result in scapular protraction. Ex. Rhomboids, middle and lower trap cause scapular retraction. Ex. Upper trap and levator scap create elevation while pec minor and latissimus dorsi cause depression of the scapula. If the muscle is in a shortened position, the overlap of actin and myosin reduces the number of sites available for cross-bridge formation. Active insufficiency-occurs when the muscle is incapable of shortening to the extent required to produce full range of motion at all joints crossed simultaneously. Ex: The finger flexors cannot produce a tight fist when the wrist is fully flexed, as they can when it is in neutral position. If the muscle is in a lengthened position compared with the optimum length, the actin filaments are pulled away from the myosin heads such that they cannot create as many cross-bridges. Passive insufficiency –occurs when the two-joint muscle cannot stretch to the extent required for full range of motion in the opposite direction at all joints crossed. Ex: a larger range of hyperextension is possible at the wrist when the fingers are not fully extended. 2. MS Tests and Measures MMT Grades 0 Zero; No evidence of contraction 1 Trace; Slight contraction, no motion 2- Poor minus; Movement through partial test range in gravity eliminated position 2 Poor; Movement through complete test range in gravity eliminated position 2+ Poor plus; Movement through complete test range in gravity eliminated position and through up to one half of test range against gravity 3- Fair minus; Movement through complete test range in gravity eliminated position and through more than half of test range against gravity 3 Fair; Movement through complete test range against gravity 3+ Fair plus; Movement through complete test range against gravity and able to hold against minimum resistance 4 Good; Movement through complete test range against gravity and able to hold against moderate resistance 5 Normal; Movement through complete test range against gravity and able to hold against maximum resistance Normal ROM Cervical: Flex/Ext/lateral flex/45 degrees; Rotation-60-70 Lumbar: Flex-90; Ext-25; lateral flexion-35; Rotation-45 Shoulder: Flex-180; Ext-60; Abd-180; IR-70; ER-90 Elbow: Flex-150; Ext-0; Pronation/supination-80 Wrist: Flex-80; Ext-70, RD-20; UD-30 1st CMC: Flex-15; Ext-20 MCP Fingers: Flex-90; Ext-45 MCP thumb: Flex-50; Ext-0 PIP: Flex-100; Ext-0 DIP: Flex-90; Ext-0 Hip: Flex-120; Ext-30; Abd-45; Add-30; IR-45; ER-45 Knee: Flex-135; Ext-0-10 Ankle: DF-20; PF-50; Inv-35; Ev-15 1st MTP: Flex-30; Ext-70 Subtalar: Inverstion-5; Eversion-5 End-Feels: Firm (stretch)-ankle dorsiflexion, finger extension, hip IR, forearm supination, Knee ext Hard (bone to bone)-elbow extension Soft (soft tissue approx.)-elbow flexion, knee flexion Posture: Ideal plumb line alignment: -Slightly posterior to coronal suture -Through external auditory meatus -Through axis of the odontoid process -Midway through the tip of the shoulder -Through the bodies of the lumbar vertebrae -Slightly posterior to the hip joint -Slightly anterior to the axis of knee -Slightly anterior to the lateral malleolus -Through the calcaneocuboid joint Mobilizations: Grade 1-Small amplitude oscillations performed at beginning of range. Grade 2-Larger amplitude oscillations performed into mid-range of a joint. Grade 3-Large oscillations performed through the available range of a joint and into the tissue resistance. Grade 4-Small amplitude oscillations performed into the tissue resistance. *Grades 1 and 2 maintain joint mobility, relieve pain, and are indicated in the subacute state of joint inflammation or sprain. *Grade 3 maintains joint mobility. * Grade 4 increases joint mobility. *Grades 3 and 4 are both indicated in more advanced stages of hypomobility or for joint impingement or motion restrictions. These grades should NOT be used when the joint has inflammation and pain (e.g. with acute exacerbation with RA) Types of Fractures: Avulstion fx-a portion of bone becomes fragmented at the site of tendon attachment due to a traumatic and sudden stretch of the tendon. Closed fx-a break in a bone where the skin over the site remains intact Comminuted fx-a bone that breaks into fragments at the site of injury Compound fx-a break in a bone that protrudes through the skin Greenstick fx-a break on one side of a bone that does not damage the periosteum on the opposite side. This type of fx is often seen in children. Nonunion fx-a break in a bone that has failed to unite and heal after 9-12 months. Stress fx- a break in a bone due to repeated forces to a particular portion of the bone. Spiral fx- a break in a bone shaped like an “S” due to torsion and twisting. Types of Muscular Contraction: Concentric-occurs when the muscle shortens while developing tension Eccentric-occurs when the muscle lengthens while developing tension Isometric-occurs when tension develops, but there is no change in the length of the muscle Isotonic-occurs when the muscle shortens or lengthens while resisting a constant load. (hand held weights) Isokinetic-occurs when the tension developed by the muscle, while shortening or lengthening at a constant speed (variable load), is maximal over the full range of motion (Cybex, Biodex, and Lido) Common DTRs: -Biceps (C5-C6) -Brachioradialis (C6) -Triceps (C7) -Patellar tendon (L3, L4) -Achilles tendon (S1, S2 Responses: Areflexia (absent) =0 Hyporeflexia (sluggish) = 1+ (LMN) Normal =2+ Hyperreflexia (brisk) = 3+ (UMN) Common Neural tension tests: -Passive SLR =sciatic nerve •Tibial nerve=passive SLR with DF & eversion •Fibular nerve=passive SLR with PF & inversion •Sural nerve=passive SLR with DF and inversion •Prone knee bend=femoral nerve •Passive neck flexion=spinal dura Common Disorders/Pathology of the MS system: Pathology What is it Etiology 1.Arthrogryposis A non progressive, nongenetic, congenital disorder -not inherited 2.Complex Regional Pain Syndrome (CPRS) Formerly known as “Reflex Sympathetic Dystrophy” Abnormal sympathetic reflex resulting from a persistent painful lesion - 3.Colles fracture Most common wrist fx resulting -Results from falling onto Signs & Symptoms -Characterized by rigid joints of the extremities (usually symmetrical) -sausage like shapeless limbs, and weak/non functioning limbs -Pain, edema, decreased circulation, osteoporosis, skin dryness, decreased proprioception, and atrophy of muscles in close proximity to involved area -The distal fragment of the Treatment -Surgery, ROM exercises, splinting, positioning, ADL training, use of adaptive devices Modalities to decrease pain, joint mobs, weight bearing or closed chain exercise, massage, manual lymphatic drainage, splinting -Casting, early active ROM and PROM are essential for from a fall on an outstretched hand extended wrist 3A.Smith’s fracture Distal fx of the radius, which dislocates in the ventral direction. (reverse colles fx) -Results from a fall onto a flexed wrist 4.DJD (Osteoarthritis) Chronic disease that causes deneneration of articular cargilage, thickening of subchondral bone often affecting weight bearing joints 5.Fibromyalgia An immune system disorder -Unknown, typically appears during middle age & affects nearly all individuals to some extent by age 70. Occurs more common in men than women up to age 55. Risk factors: overweight, fxs or other joint injuries, athletic overuse -Unknown origin; often radius has a dorsal displacement with a radial shift of the wrist and hand -Fragment dislocates in the ventral direction -Gradual onset of pain present at the affect joint, increased pain after exercises, increased pain with weather changes, enlarged joints, crepitus, stiffness, limited joint ROM, Heberden’s nodes, & Bouchard’s nodes. -Characterized by aching or functional recovery, progressive resistive exercises, mobs, closed-chain stabilization exercises -Casting, early active ROM and PROM are essential for functional recovery, progressive resistive exercises, mobs, closed-chain stabilization exercises -Reduce pain, promote joint function, and protect the joint. NSAIDS/acetaminophen, and corticosteroids. Viscosupplementation which is administered into the knee to improve lubrication. PT: PROM/AROM, heating and cooling agents, pt education, strengthening, e-stim, energy conservation, bracing. Surgical intervention can include arthroscopic surgery to total joint replacement. -Holistic and multidisciplinary approaches are necessary. that causes tenderness, pain, and stiffness in the muscles. 11/18 points throughout the body related to stress, anxiety, fatigue, and sleeplessness in women more than men. 6.Osteogenesis Imperfecta A connective tissue disorder that affects the formation of collagen during bone development. There are 4 classifications of imperfects that vary in level of severity. 7.Osteochondriti s dissecans Seperation of the articular cartilage from the underlying bone -The cause is genetic inheritance with types I and IV considered autosomal dominant traits and types II and III considered autosomal recessive traits. Osteochondra l fracture burning of the muscles “a migraine headache of the muscles” diffuse pain, or tender points on both sides of the body. -Pathological fractures, osteoporosis (brittle bones), hypermobile joints, bowing of the long bones, weakness, scoliosis, impaired respirator function ADL education and training, Stress management training, analgesics and antidepressants, local modalities and techniques for muscle pain relief, aerobic/conditioning exercises, improve sleeping patterns -Management begins at birth with caregiver education on proper handling and facilitation of movement. PT will focus on AROM emphasizing symmetrical movements, positioning, functional mobility, fracture management, and the use of orthotics. In severe cases, wheelchair prescription. -Usually involving the medial femoral condyle near the intercondylar notch and observed less frequently at the femoral head and talar -If fracture is displaced then surgery is indicated. PT after surgery: gait training, functional strengthening, conditioning. 8.Osteomalacia Decalcification of bones -Results from vitamin D 9.Osteomyelitis Acute or chronic bone infection -Commonly the result of combined traumatic injury and an acute infection. 10.Osteoporosis Most common metabolic bone disease -Affects white females most commonly, depletes bone mineral density, which may predispose the indivudal to fracture dome -May cause deformities, fractures, and severe pain -In children: most common site includes the distal femur and proximal tibia, humerus, and radius. In adults, the disease commonly localizes in the pelvis and vertebrae and is usually a result of contamination related to surgery or trauma -Common sites of fx: thoracic and lumbar spine, femoral neck, proximal humerus, proximal tibia, pelvis, distal radius -Pain control, functional mobility training -High doses of IV antibiotics, the infected extremity is immobilized by a cast, traction or bed rest. -Pain management, postural reeducation, , breathing exercises, general conditioning, pectoral stretching, abdominal strengthening(with caution— do not want excessive and repeated flexion of spine as this can lead to wedge fractures in these pts) 11.Paget’s disease(osteitis deformans) A slowly progressive metabolic bone disease characterized by an initial phase of excessive bone reabsorption followed by a reactive phase of excessive abnormal bone formation. The new bone structure is fragile and weak and causes painful deformities of the external contour and the internal structures. -Unknown 12.Patellofemor al syndrome The patella fails to properly track in the trochlear groove of the -Repetitive overuse disorder, decreased -Usually affects several skeletal areas including spine, pelvis, femur, and skull. The disease can be fatal when associated with congestive heart failure (widespread disease creates a continuous need for high cardiac output), bone sarcoma, or giant cell tumors. Involved sites can fx easily and heal slowly and usually incompletely. Vertebral collapse or vascular changes can lead to paralysis. -Anterior knee pain, q-angle greater than 18°, instability -If pt is asymptomatic, treatment is not needed. If symptoms are present, pt will require drug therapy. -Modalities to decrease pain & inflammation, McConnell’s taping technique, stretching of the iliotibial band and femur 13.Scleroderma A chronic disorder characterized by fibrosis and changes in the internal organs and skin quad strength, decreased lower extremity flexibility, patellar instability, increased tibial torsion or femoral anteverison. Increased risk for developing: females, growth spurts, runners who have increased mileage, overweight, Positive chondromalac ia test (Clark’s sign) -Frequently accompanied by Raynaud’s phenomenon or pain usually occurs in the first 30° of knee flexion, stair climbing, prolonged sitting, squatting, or jumping tensor fascia latae, strengthening of the VMO, shoe inserts to decrease genu valgum and pes planus, On-Track Brace to reposition patella, transverse friction massage over the lateral retinaculum, patellar mobilization: medial patellar glide and stretching deep fibers of lateral retinaculum to decrease patellar tilt. -Polyarthalgia is a prominent early symptom, heartburn and dyspnea occasionally are the first -Maintain joint ROM, medications, strengthening exercises 14.Pronator teres syndrome Median nerve entrapment in the pronator teres muscle 15.Rheumatoid Arthritis (RA) Chronic, systemic inflammatory disorder, the disease presents with a chronic inflammatory reaction in the synovial tissues -Unknown. Women more affected than men (40-60 years age) May initially occur at any joint, but it is manifestations of the disease. Positive rheumatoid factor test, other blood tests -DD via pronator teres test: The clinician strongly resists pronation of the elbow as the pts elbow is extended from 90° of flexion toward full extension, test is + if tingling or paraesthesia is provoked in the forearm and hand in a median nerve distribution Onset may be gradual or immediate, symmetrical involvement, pain and tenderness of affected joints, -Manual nerve glides, stretching exercises, AROM exercises, Ultrasound, NMES for nerve healing Reduce inflammation and pain, promote joint function, and prevent joint destruction and deformity. NSAIDS, DMARDS are slow acting and take weeks or months to become effective but can slow the progression. PT: of a joint that results in erosion of cartilage and supporting structures within the capsule. 16.Juvenile RA Most common chronic rheumatic disease in children and presents with inflammation of the joints and connective tissues. Classification of JRA includes systemic, polyarticular, and oligoarticular. Onset is prior to age 16 with common in the small joints of the hand, foot, wrist, and ankle. It has periods of exacerbation and remission. It is diagnosed based on clinical presentation of involved joints & blood RA factors. -Unknown, is theorized that an external source such as a virus, infection or trauma may trigger an autoimmune response producing JRA in a child with a genetic predisposition . morning stiffness, warm joints, decrease in appetite, malaise, increased fatigue, swan neck deformity (DIP flexion, PIP hyperextension ) boutonniere deformity (DIP ext, PIP flexion, low grade fever PROM/AROM, heating and cooling agents, splinting, pt education, energy conservation, body mechanics, and joint protection techniques. Fever and Rash. -Systemic JRA occurs in 1020% of cases and presents with acute onset, high fevers, rash, enlargement of the spleen & liver, and inflammation of the lungs and heart. Polyarticular JRA accounts for 30-40% of -Pharmacological management to relieve pain and inflammation through NSAIDS, corticosteroids, antirheumatics, and immunosuppressive agents. PT: PROM/AROM, positioning, splinting, strengthening, endurance training, weight bearing activities, postural training, functional mobility. Pain management includes the use of modalities such as paraffin, ultrasound, warm water, and cryotherapy. Surgical intervention may be complete remission in 75% of children. 17.Gout (gouty arthritis) Metabolic disease marked by elevated level of serum uric acid and deposition of urate crystals in the joints, soft tissue, and kidneys. cases and presents with high female incidence, significant rheumatoid factor, and arthritis in more than four joints with symmetrical involvement. Oligoarticular accounts for 40-60% of cases and affects less than five joints with asymmetrical involvement. Most often affects the feet, especially the great toe, ankle, and midfoot. There is severe joint pain commonly at night with warmth, erythema, and extreme tenderness/ indicated secondary to pain, contractures or irreversible joint destruction. Anti-inflammatory medications, daily use of colchicines, lowering the urate concentration in body fluids with diet, weight loss, and moderation of alcohol intake, allopurional to reducehyperuricemia, rest, elevation, and joint protection during acute phase. 18.Hemophilia 19.Iliotibial band friction syndrome 20.Myositis Ossfifcans hypersensitivity . Hemorrhagic -Results from -Can cause disorder that is a deficiency of pain, swelling, hereditary specific extreme clotting tenderness, factors and possibly permanent deformity. Bleeding near peripheral nerves can cause peripheral neuropathies, pain parathesia, and muscle atrophy. An irritation -Often occurs -Positive Ober’s caused by the in runners test, excessive rubbing of the from an hip IR in stance, ITB over the overuse palpation over lateral epicondyle syndrome ITB insertion, of the femur positive Noble compression test Often caused by -Can be -Frequent trauma to a induced by locations: muscle resulting early quads, in hematoma mobilization brachialis, and that may calcify and stretching biceps brachii. or ossify with Radiological aggressive PT studies will -Splinting, Ice, rest, and elevation are needed in acute stage. In chronic situations, joint protection, maintaining joint function, daily exercises for ROM, endurance and strength, ADL training, and the use of appropriate splints and Ads should be addressed. -Stretching exercise program, modalities for pain and inflammation, soft tissue mobilization techniques, shoe orthosis may be necessary. -Conservative with gentle active and active assisted ROM, passive stretching is not indicated, NO manual stretching with overpressure at end-range. 21.Scoliosis Lateral curvature of the spine. Most often quantified using the Cobb method with a standing radiograph. Classified as functional (nonstructural)(r esults from leg length discrepancy, muscle imbalance, poor posture) can be corrected w/lateral bending. Neuromuscular scoliosis results w/developmental pathology resulting in alterations within the structure of the spine. Observed in pts w/CP or Marfan syndrome. Degenerative following trauma to the muscle -Typically idiopathic. It is most commonly diagnosed between 10 and 13 years of age. Girls and boys have a similar risk of developing a mild curve (10°or less), however, girls have a significantly greater risk of acquiring a curve greater than 30° show calcium deposits -Shoulder level asymmetry w/ or w/out the presence of a rib humb. Pain is not typically associated w the spinal curvature, rather it is a result of the abnormal forces placed on other tissues of the body. -Based on magnitude of curve and degree of progression. If curve not progressing no formal action is taken. PT: muscle strengthening, and flexibility exercises, shoe lifts, and bracing. A spinal orthosis is often warranted with a curve that ranges between 25-40°. Surgical intervention may be required with curves greater than 40°. Ankylosing spondylitis scoliosis occurs due to the normal aging process and is facilitated by changes such as osteophyte formation, bone demineralization, and disk herniation. Neuromuscular and degenerative scoliiosis are considered to be forms of structural scoliosis since the curves are inflexible and do not reduce w/lateral bending. Progressive inflammatory disorder of unknown etiology that initially affects axial skeleton Initial onset (usually mid and low back pain for 3 months or greater) before fourth decade of life First symptoms include mid and low back pain, morning stiffness, and scaroiliitis. Results in kyphotic deformity of the cervical & thoracic spine NSAIDS, corticosteroid therapy. PT: implementation of flexibility exercises for trunk to maintain/improve normal joint motion & length of muscles in all directions, especially extension. 22.Sjogren’s syndrome A rheumatoidlike disorder characterized by dryness of the mucous membranes, joint inflammation, and anemia. -More common than systemic lupus erythematosu s (SLE) and less common than RA. 23.Achilles Tendonitis Is a repetitive disorder resulting in microscopic tears of collagen fibers on the surface or in the substance of the Achilles tendon. The tendon is most often impacted in an avascular zonelocated two to six centimeters above the insertion of the tendon. -Repetitive overload of the tendon caused by changes in training intensity or faulty techniques. Pts w/limited flexibility and strength in the gastroc/soleu s and pts w a pronated or cavus foot are at increased & a decrease in lumbar lordosis. -Dryness of the eyes and mouth along with joint inflammation. Arthritis occurs in about 33% of the pts & is similar in distribution to RA, but milder & without joint destruction. -aching or burning in the posterior heel, tenderness of the Achilles tendon, pain w increased activity, swelling, and thickening in the tendon area, muscle weakness due to pain, morning stiffness -Sipping fluids throughout the day, chewing surgarless gum, using a mouthwash for mouth dryness, medications for pain and inflammation occasionally needed, maintain mobility and function through a regular exercise program. -Initially RICE, NSAIDS, as needed. A heel lift and cross training may be used to limit the amount of tensile loading through the tendon. Prevention includes heel cord stretching exercises, use of appropriate soft-soled footwear, eccentric strengthening of the gastroc/soleus, and avoiding sudden changes in intensity of training programs. 24.Adhesive Capsulitis Results in a loss of ROM in active and passive shoulder motion due to soft tissue contracture. The condition is caused by adhesive fibrosis and scarring between the capsule, rotator cuff, subacromial bursa, and deltoid. 25.Anterior cruciate ligament sprain ACL runs from the anterior intercondylar area of the tibia to the medial aspect of the lateral femoral condyle in the intercondylar risk. -May be related to a direct injury to the shoulder or may being insidiously. Peak incidence occurs in individuals 40 and 60 years of age w females being affected more. Pts w diabetes have increased incidence. The condition is self-limiting and typically resolves in 1-2 years. -Noncontact twisting injury associated with hyperextensio n, varus or valgus stress to the knee. An ACL sprain -Insidious onset of localized pain often extending down the arm, subjective reports of stiffness, night pain, restricted motion in a capsular pattern. (ER most limited) -Increase ROM with glenohumeral mobilization, ROM exercises, and palliative modalities. The therapist and pt should AVOID overstretching and elevating pain since this can result in further loss of motion. Surgical options include suprascapular nerve block and closed manipulation under anesthesia. -The pt may report a loud pop or feeling of the knee “giving way” or “buckling” followed by dizziness, sweating, and -Initially RICE, NSAIDS, and analgesics as needed. Conservative treatment includes lower extremity strengthening exercises emphasizing the quads and hamstrings. Surgery if often warranted for a complete tear. A de-rotation brace may 26.Posterior cruciate ligament sprain notch. The ligament prevents anterior displacement of the tibia in relation to the femur. The extent of the sprain is classified according to the extent of ligament damage. A grade I sprain involves microscopic tears of the lig, while a grade III indicates a completely torn ligament. PCL runs from the posterior intercondylar area of the tibia to the lateral aspect of the medial femoral condyle in the intercondylar notch. The PCL prevents posterior displacement of the tibia in relation to the often involves injury to other knee structures such as the medial capsule, MCL, and menisci. swelling. Special tests: Lachman’s & lateral pivot shift test be beneficial for a pt with ACL deficient knee, but has limited benefit for a pt following surgical reconstruction. (90°-40°flex) -Most common cause of injury are landing on the tibia with a flexed knee or hitting a dashboard in a MVA w a flexed knee. Isolated PCL tears are not common and often involve -The pt may report feeling as if the femur is sliding off the tibia. Swelling and mild pain may be present, but often the pt is asymptomatic. Special tests: posterior drawer, posterior sag sign -Initially RICE, NSAIDS, PT: lower extremity strengthening and functional progression. If surgery is performed, isolated hamstrings exercises are often AVOIDED for a minimum of six weeks. femur 27.Medial collateral ligament sprain MCL runs from slightly above the medial femoral epicondyle to the medial aspect of the shaft of the tibia. A MCL sprain often ivolves injury to other knee structures (ACL/medial meniscus) 28.Meniscus Tear The medial & lateral menisci are attached to the proximal surface of the tibia. The menisci are thick at the periphery and thinner at their internal other knee structures such as the ACL, MCL, LCL, and menisci -A contact or noncontact, fixed foot, tibial rotational injury associated with valgus force and external tibia rotation can damage MCL. Often associated w activities such as football, skiing, and soccer. -Associated with fixed foot rotation while weight bearing on a flexed knee. This action produces compression and rotational -Clinical presentation includes knee pain, swelling, anatlgic gait, decreased ROM, and a feeling of instability. A valgus stress test can be used to assess the integrity of the MCL. -Initially RICE, NSAIDS. Conservative treatment includes decreasing inflammation, protecting the knee joint and ligament, ROM, and strengthening exercise as tolerated. Strengthening exercises gradually become more aggressive and functional activities are introduced. Surgery is rarely required since the MCL is well vascularized. -Joint linepain, swelling, catching or a locking sensation. Special tests: Apley’s compression test, bounce home test, and -Initially RICE, NSAIDS. Conservative treatment consists of palliative modalities and strengthening exercise. Surgery ranging from a partial meniscectomy to a meniscal repair is often warranted for active individuals. Meniscal repairs are typically performed on 29.Lateral epicondylitis “tennis elbow” unattached edges. The medial meniscus is more commonly injured than the lateral bc it is less mobile due to its attachment to the joint capsule. The incidence of medial tears increases significantly over time with ACL deficiency. Mensical injuries are definitively diagnosed w arthroscopy or MRI. Refers to an irritation or inflammation of the common extensor muscles at their origin on the lateral epicondyle of the humerus. Individuals who take part in racquet sports are at greatest forces on the meniscus McMurray test. tears located on the outer edges of the meniscus due to the increased vascularity. -Caused by eccentric loading of the wrist extensor muscles, usually the extensor carpi radialis brevis, resulting in microtrauma. Lateral epicondylitis can be -Pain is present immediately anterior or distal to the lateral epicondyle of the humerus. Pain typically worsens with repetition and resisted wrist extension. -Initially RICE, NSAIDS, and activity modification. PT: attempt to increase strength(initial emphasis on eccentric phase of ex), flexibility, and endurance of the wrist extensors. A strap placed 2-3 inches distal to the elbow joint can reduce muscular tension placed on the epicondyle and may diminish or eliminate pt symptoms. *Resist wrist risks 30.Medial epicondylosis “golfers elbow” Usually a degenerative condition of the pronator teres & flexor carpi radialis tendons at their attachment to the medial epicondyle of the humerus. 31.Congenital Hip dysplasia Also known as developmental dysplasia, is a condition characterized by malalignment of the femoral head within the precipitated by poor mechanics or faulty equipment such as too small of a handle on a tennis raquet. Most common in individuals between 3050. -Occurs w overuse in sports, such as baseball, swimming, or jobs that require a strong hand grip and excessive pronation of the formearm -Cultural predisposition , malposition in utero, environmenta l and genetic influences extension, wrist radial deviation, and forearm pronation with fingers fully flexed (fist) simultaneously =Cozen’s test. Clinician: passively supinate forearm, extend elbow, and extend wrist. Reproduces pain at medial epicondyle. Same as lateral -Clinical presentation includes asymmetrical hip abduction with tightness and apparent femoral -Dependent on age, severity, and initial attempts to reposition the femoral head w/in the acetabulum through the constant use of a harness, bracing, splinting, or traction. Open reduction w/ subsequent application of a acetabulum. The condition develops during the last trimester in utero. 32.Congenital Limb Deficiencies A congenital limb deficiency is a malformation that occurs in utero, secondary to an altered developmental course. Congenital limb deficiencies are classified as longitudinal or transverse. A longitudinal limb deficiency refers to a reduction or absence of an element or elements within the long axis of the bone. A transverse limb deficiency refers to a limb that has developed to a -The majority of congenital limb deficiencies are idiopathic or genetic in origin. Other possible etiologies include poor blood supply, constricting amniotic bands, infection, and maternal drug exposure. shortening of the involved side. Testing for this condition may include Ortolani’s test, Barlow’s test, and diagnostic ultrasound. -structural or acquired abnormality of a limb, phantom limb pain. hip spica cast may be required if conservatice treatment fails. PT: stretching, strengthening, and caregiver education. -Symmetrical movements, strengthening, ROM, weight bearing activities, and prosthetic training when appropriate. 33.Congenital torticollis “wry neck” particular level beyond which no skeletal elements exist. Characterized by a unilateral contracture of the sternocleidomast oid muscle. The condition is most often identified in the first 2 months of life. 34.Glenohumera Refers to l instability excessive translation of the humeral head on the glenoid during active rotation. Subluxation refers to joint laxity, allowing for more than 50% of the humeral head to passively translate over the glenoid rim w/out dislocation. Dislocation is the -Cause is unknown, may be associated with malpositionin g (breech) in utero and birth trauma. A combination of forces stress the anterior capsule, gelenhumeral ligament, and rotator cuff, causing the humerus to move anteriorly out of the glenoid fossa. An anterior dislocation is the most common and -Clinical presentation includes lateral cervical flexion to the SAME side as the contracture, rotation toward the opposite side, and facial asymmetries. Subluxation:fee ling the shoulder “popping” out and back into place, pain, paresthesias, sensation of the arm feeling “dead” positive apprehension test, capsular tenderness, swelling; Dislocation: severe pain, paresthesias, limited ROM, -Initially-treatment is conservative with emphasis on stretching (ex. Right torticollis: to stretch, perform left side bending & right rotation), AROM, positioning, and caregiver education. Surgical management is indicated when conservative options have failed and the child is over one year of age. -Initial immobilization with a sling for 3 to 6 weeks. RICE and NSAIDS. Following immobilization, ROM, and isometric strengthening should be initiated followed by progressive resistive exercises emphasizing the internal and external rotators, as well as the large scapular muscles. 35.Impingement Syndrome 36.Legg-CalvePerthes Disease complete separation of the articular surfaces of the glenoid and the humeral head. Approx 85% of dislocations detach the glenoid labrum (Bankart lesion) Is one of the most common injuries of the shoulder. It is often caused by repetitive microtrauma from upper extremity activity performed above the horizontal plane. is usually associated with shoulder abd and LR. weakness, visible shoulder fullness, arm supported by contralateral limb. -Caused by the humeral head and the associated rotator cuff attachments migrating proximally and becoming impinged on the undersurface of the acromion and the coracoacromi al igament Characterized by degeneration of the femoral head due to a disturbance in -Trauma, genetic predisposition , synovitis, vascular -discomfort or mild pain deep within the shoulder, pain with overhead activities, painful arc of motion (70-120 abduction), positive impingement sign, tenderness over the greater tuberosity and the bicipital groove -gradual onset of ‘aching” pain at hip, thigh, and knee. AROM limited -Initially RICE, NSAIDS, and activity modifications. Once tolerated, treatment includes rotator cuff strengthening and scapular stability exercises. Long-term prevention includes continued strengthening of the rotator cuff and scapula stabilizers, along with improved biomechanics related to sport specific or relevant work activity. -Activities are variable based on the clinical presentation, but primary focus is to relieve pain, maintain the femoral head in the proper 36A.Slipped capital femoral epiphysis (SCFE) 37.OsgoodSchlatter Disease the blood supply (avascular necrosis). The disease is selflimiting and has four distinct stages: condensation, fragmentation, re-ossification, and remodeling. Most common hip disorder observed in adolescents abnormalities, infection (Age of onset:2 & 13 years avg.6 yrs) Males have 4x greater incidence AKA traction apophysitis, is a self-limiting condition that results from -Caused by repetitive tension to the patellar tendon over -Unknown; onset in males: 10-17 years, avg 13. Onset in females: 8-15 years, avg 11. Males have 2x the incidence of females. in ABDuction & ext. Characteristic psoatic limp due to weakness of psoas major; affected LE moves in ER, flex, and adduction -pt describes pain as vague at knee, thigh, & hip. AROM is restricted in ABD, FLEX & IR. With chronic conditions, pt may demonstrate a Trendelenburg gait. Diagnostic tests: plain film shows displacement of upper femoral epiphysis. -Point tenderness over the patella tendon at the insertion on the position & improve ROM. PT: may be required intermittently for stretching, splinting, crutch training, aquatic therapy, traction, and exercise. Orthoics and surgical intervention may benecessary. NSAIDS for pain, joint bone protection strategies, maintain/improve joint mechanics, implementation of aerobic capacity/endurance (aquatic programs) Post surgical interventions include regaining functional flexibility, improving strength/endurance/cooridn ation, and gait training. -Conservative treatment focuses on education, icing, flexibility exercises, and eliminating activities that place strain on the patella repetitive traction on the tibial tuberosity apophysis. 38.Plantar fasciitis Refers to inflammation of the plantar fascia at the proximal insertion on the medial tubercle of the calcaneus. The plantar fascia is a broad structure comprised of connective tissue which spans from the calcaneus to the metatarsal heads. The structure is designed to provide support to the arch of the foot. Excessive tension over time creates chronic the tibial tuberosity in young athletes. This can result in a small avulsion of the tuberosity and subsequent swelling. -Often associated with an acute injury from excessive loading of the foot or chronic irritation from an excessive amount of pronation or prolonged duration of pronation. The condition is most common in pts between 40-60 years of age. tibial tubercle, anatalgic gait, pain with increasing activity tendon such as squatting, running, or jumping. -Clinical presentation includes tenderness at the insertion of the plantar fascia, presence of a heel spur, pain that is worse in the morning or after periods of prolonged inactivity, difficulty with prolonged standing, & pain when walking in bare feet. -Initially RICE, NSAIDS. A heel cup, massage using a tennis ball or rolling pin, medial longitudinal arch taping, and joint mobs may be helpful. Prevention includes heel cord stretching exercises, use of appropriate soft-soled footwear, & avoiding sudden changes in the intensity of training programs. Orthotics may be used to minimize hyperpronation (resting night splints) 39.Talipes Equinovarus “clubfoot” 40.Rotator cuff tear inflammation and microtears at the proximal insertion. Is a deformity characterized by the heel pointing downward and the forefoot turning inward. Can be torn due to an acute traumatic incident or as a result of a chronic degenerative pathology. Pts 50 -Unknown, theories postulate familia tendency, positioning in utero or a defect in the ovum. This condition accompanies other NM abnormalities including spina bifida and arthrogryposi s, & may result from the lack of movement in utero. -Intrinsic factors associated with rotator cuff tears include impaired blood supply -Clinical presentation includes adduction of the forefoot, varus positioning of the hindfoot, and equines at the ankle (PF) -Medical management begins shortly after birth and includes splinting and serial casting. The goal of intervention is to restore proper positioning of the foot and ankle. Failed management or severe involvement may require surgical intervention & subsequent casting. -arm positioned in internal rotation and adduction, point tenderness at the greater tubercle and -Conservative management: RICE, NSAIDS. Primary focus of therapy is to prevent adhesive capsulitis and strengthen UE musculature. Surgical management to repair the tendon can be arthroscopic, mini-open with 41.Total Hip years of age and older are particularly susceptible to tears due to chronic degenerative pathology. Rotator cuff tears are classified as partial thinkness or full thickness. A partialthickness tear extends through only a portion of the tendon. A full-thickness tear is a complete tear of the tendon. The size of the tear can range from small (1cm or less) to large (more than 5cm) Refers to removal of the proximal & distal surfaces of the hip with subsequent replacement by an acetabular component and a femoral implant. to the tendon, resulting in degeneration. Extrinsic factors include trauma, repetitive microtrauma, and postural abnormalities. acromion, marked limitation in shoulder flexion and abduction w upper trap recruitment evident, increased tone in anterior shoulder structures. arthroscopic assist or a traditional open approach. Following surgery, the pt will be immobilized in a sling. The amount of immobilization time will vary depending on surgeon preference, procedure, and size of tear. A large tear may require 4-6 weeks of immobilization. PT beings with PROM, gradually to AAROM. Active motion & isometric exercises begin once approved by the surgeon. The pt will gradually become functional w ADLS and progress to more aggressive strengthening activities. Return to functional activities requiring dynamic over head motion occurs in 9-12 months. -Elective surgical procedure. Needs include OA, RA, osteomyelitis, and avascular necrosis. -Prior to surgery, severe pain with weight bearing, loss of mobility, gross instability or limitation in ROM, failure of non-operative -Initially PT focuses on decreasing inflammation and allowing tissues to heal, emphasizing adherence to hip precautions, minimizing muscle atrophy, and regaining full PROM. Tx can include ankle pumps, quad and glut sets, active hip Surgical procedure can be anterolateral, direct lateral or posterolateral. Fixation can be cemented or cementless. Cemented fixation allows weight bearing as tolerated often immediately. Cementless and hybrid fixation rely on bone growth and may dictate partial weight bearing or NWB initially. Cementless is normally for young, active individuals (less than 65 years)Average lifespan of a total hip is 15-20 years. 42.Total knee Elective surgery management or a previous surgical procedure. flexion w/in available range, assistive device training, and progressive ambulation. As the pt progresses, treatment moves toward regaining full strength & endurance and attaining independence in the home setting. Anterolateral approach: AVOID-hip flexion greater than 90, hip ext, adduction. Direct lateral approach:AVOID-hip flexion beyond 90, hip ext, ER, and adduction. Posterolateral approach:AVOID-hip flexion beyond 90, IR, adduction Severe pain w weight bearing, loss of mobility, gross instability or limitation in Initially, PT treatment focuses on decreasing inflammation & allowing tissues to heal, emphasizing adherence to knee ROM, marked deformity of the knee, failure of nonoperative management. 43.Temporoman dibular joint syndromes Can be divided into 3 diagnostic categories: 1. Joint abnormalitiestrauma arthritis, disease or neoplasm. 2.Congenital structural defects. Can include meniscus, ligaments that control movement of the disc, the condyles, the fossa, or the articular tubercles. 3. Loss -Joint noise, joint locking, AROM of the jaw, lateral deviation of the mandible during depression or elevation, decreased strength, tinnitus, headaches, forward head posture, and paint w/movement. precautions, minimizing muscle atrophy, and regaining full PROM. Knee flexion requires a minimum of 90° for ADLS & 105° to rise comfortably from sitting. Theraputic activities include ankle pumps, quads and glut sets, AROM, CPM, assistive device training, & progressive ambulation. Advanced activities include wall slides, controlled lunges, stationary cycling, & step ups. -Postural reeducation, modalities for pain, inflammation reduction, biofeedback, joint mobilization, AROM and muscle strengthening exercises, pt education for eating soft foods and decreasing habits that stress the TMJ(biting nails or pencils), instruct the pt in maintaining the rest position of the tongue (upright postural position of the tongue on the hard palate). of functional mobility of unknown etiology. May result from increased activity in the muscles of mastication as the result of stress & anxiety. *Specific conditions of TMJ: 1. Synovitis & capsulitis-pain located anterior to ear area, unable to fully close back teeth together, opening less than 40 mm secondary to pain, pain decreases w rest. 2.TMJ hypermobility-pt reports “my jaw feels like it goes out of place,” may report joint noises, short term episodes of jaw “catching” in fully opened position. Mandibular depression is greater than 40mm and deviates toward the NONinvolved (contralateral) side, palpable irregularities during closure. 3. Disc displacement w/reduction-Pt reports joint noises with opening and closing equal to “pops” or “clicks.” Palpation over lateral poles reveals an opening click (the reduction of the disc) and a closing click (the disc displacing anterior to the condyle). These noises equal the “reciprocal click.” 4. Disc displacement w/out reduction-Pt reports intermittent locking without joint noises. Opening of mandible is limited to 20-25 mm with deflection toward INVOLVED side. Limited lateral excursion toward the opposite side of the involved joint. *primary glide is inferior, which gaps joint, stretches the capsule, and allows relocation of anteriorly displaced disc. Musculoskeletal Pathologies: Pathology Achilles Tendon Rupture Diagnosis Contributing Factor Normally occurs within 1-2 inches above its tendinous Occurs most frequently when pushing off a Clinical Presentatio n Pt will present with swelling over the Lab/Imaging Management/Outco me X-ray to rule out avulsion fx or bony injury. MRI Immobilization through casting or surgical repair. Pharmacological insertion on the calcaneus. weight bearing extremity with an extended knee, through unexpected DF while WBing or with a forceful eccentric contraction of the PFors. Poor stretching routine, improper shoe wear. A person over 30 is at higher risk, average 3050 years who participate in recreational activities. distal tendon, a palpable defect in the tendon above the calcaneal tuberosity, pain & weakness with PF. Pt will limp and often complain that there was a snap or pop associated with severe pain during the inury. A pt will not be able to stand on their toes. Thompson test will result in no movement into PF. A complete rupture will result in a palpable can be used to located the presence & severity of the tear or rupture. management is not necessary except to relieve pain. Serial casting for approx 10 weeks followed by the use of a heel lift to ensure maximal healing without stress on the tendon for 3-6 months. If pt requires surgical intervention then a cast or brace is required for 6-8 weeks. PT includes ROM, stretching, icing, gait training, strengthening, plyometrics, and skill specific training. Modalities, pool therapy, may assist in recovery. Pt should return to their previous functional level within 6-7 months. Adhesive Capsulitis “frozen shoulder” is characterized by inflammation and fibrotic thickening of the anterior joint capsule of the shoulder. The capsule becomes adherent to the humeral head and under goes contracture. This condition causes symptoms of GH limitations and pain. Primary adhesive capsulitis has no known etiology, it is associated with DM, hypothyroidi sm or cardiopulmo nary conditions. Secondary adhesive capsulitis can result from trauma, immobilizatio n, reflex sympathetic dystrophy, RA, abdominal disorders, and psychogenic disorders. Occurs more in the middle aged gap in the tendon prior to the insertion. Restricted active and passive ROM at the GH joint. Pain that radiates below the elbow and awakens the pt at night. PROM is limtied during this acute phase due to pain & guarding. Pain is present with a loss of GH motion, restricted elevation, and ER. An arthrogram can assist with the diagnosis by detecting a decreased volume of fluid within the joint capsule. Greatest restriction in ER and abduction. Self-limiting process that can take over 12 months to run its course. A physician can inject corticosteroids to assist with recovery. Surgical intervention to break up adhesions or release adhered muscles. PT during acute phase includes icing or superficial heat, gentle joint mobs, progressive strengthening, pendulum exercises, & isometrics. During the chronic phase: ultrasound, grade III and IV mobs, PNF to restore painless ROM. PT is usually prescribed on an outpatient basis 3-5 months after diagnosis. Follows a nonlinear pattern of recovery. Ankylosing Spondylitis Is a systemic condition that is characterized by inflammation of the spine and larger peripheral joints. The chronic inflammation causes destruction of the ligamentous osseous junction with subsequent fibrosis and ossification of the area. population with females having a greater incidence than males. Genetic inheritance. Typically seen between 2040 years of age, and men are at a 2-3x greater risk than women. More common in Caucasians. Spontaneous recover is said to take 12-24 months. Will present with recurrent & insidious epidoses of low back pain, morning stiffness, impaired spinal extension, and limited ROM in the affected joints for over a 3 month period of time. Other manifestatio ns include kyphosis, fatigue, weight loss, and peripheral joint X-ray of the spine may be negative in the initial stage of AS but with progression will revel areas of erosion, demineraliza tion, calcification, and syndesmopht ye formation. In later stages, X-ray will reveal fusion of the SI joint and a bamboo appearance of the spine. Lab work can be used to rule out Reduce inflammation, maintain functional mobility and relieve pain. PT should include postural exercises emphasizing extension, general ROM, pain management, and energy conservation. Low impact and aerobic exercise with emphasis on extension and rotation are appropriate for a pt with AS. High impact and flexion exercises are contraindicated. Swimming is highly recommended. AS slowly progresses over a 15-25 year period and may remain isolated to the spine and SI joint ACL sprain— Grade III Extends from the anterior intracondylar region of the tibia to the medial aspect of the lateral femoral condyle. The ligament prevents anterior translation of the tibia on the fixed femur and posterior translation of the femur on the fixed tibia.Permits up to 500 lbs of pressure prior to rupture. Ligament has poor blood supply and does not have the ability to heal a complete tear. Injuries to the ACL most commonly occur Participation in athletic activities requiring high levels of agility (soccer, basketball) and contact sports. Women have higher incidence of ACL injury than males. involvement . The peak incidence of ACL injury occurs between 14 and 29 years. A grade III is characterize d by significant pain, effusion, and edema that significantly limits ROM. Pt may be unable to WB. other diseases. MRI is the preferred imaging tool to identify the presence of an ACL tear. X-rays may be used to rule out a fracture. Subjective reports such as hearing a pop. or spread to larger joints. Control edema, increase ROM, strengthening. Patellar tendon graft is the most commonly used. Pts often initially present with a knee immobilizer and crutches to protect the graft. Treatment begins to focus on strengthening focusing on closed chain exercises. Closed chain is considered more desirable than openchain since they minimize anterior translation of the tibia. Pts electing to have surgery can expect to return to their previous functional level in 46 months. Bicipital Tendonitis during hyperflexion, rapid deceleration, hyperextenion, or landing in an unbalanced position Is an inflammatory process of the tendon of the long head of the biceps. Impingement or an inflammatory injury can result in symptoms of shoulder pain. Repeated full abduction and ER of the humeral head can lead to irritation that produces inflammation, edema, microscopic tears within the tendon, and degeneration of the tendon.Commo Often caused through repetitive overhead activity and motion. There is usually direct trauma to the tendon as the shoulder motion approaches excessive abduction and ER. High risk:baseball pitchers, tennis players, gymnastics, rowers, and swimmers. Can also be caused Pts report a deep ache directly in the front and on top of the shoulder. The ache may spread down into the biceps muscle and is usually made worse with lifting heavy objects. Resting the shoulder typically reduces the pain. Bicipital tendinopath y, pain to palpation No lab tests to assist with diagnosis. Plain x-rays do not diagnosis bicipital tendonitis, but may show calcification the groove or subacromial spurring. MRI can view the tendon, but is expensive and not usually used unless the pt is not responding to conservative treatment. Generally the pt should avoid all overhead movement, reaching, and lifting of objects. Active PT is not often initiated immediately, however, the pt may be referred for instruction in general education of the pathology, guidelines for restrictions, pendulum exercises, and the use of TENS. Pt may benefit from iontophoresis or phonophoresis. As pt progresses out of acute stage therapy should focus on an exercise program that stretches and strengthens the Carpal Tunnel Syndrome n in overhead activities. Individuals who throw, swim, or swing a racquet or club are at greatest risk. secondary to rotator cuff disease, impingement , labral tears. The carpal tunnel is created by the transverse carpal ligament, the scaphoid tuberosity and trapezium, the hook the Any condition such as edema, inflammation , tumor or fibrosis, may cause compression over the anterior sholulder in the area of the biciptial groove, pain with the biceps resistance test (shoulder flexion against resistance with the elbow extended and forearm supinated) and a positive Yerganson’s or Speed’s are positive indicators. Most pts are diagnosed between 3555 years with a greater prevalence in women. A pt will affected muscle groups. This can restore the tendon’s ability to function properly, improve healing, and prevent future injury. Once pt doesn’t experience pain they can slowly return to activity. Most pts can return to their activities after an average of 6-8 weeks of PT. Electromyogr aphy and electroneuro graphic studies can be used to diagnose a motor conduction Local corticosteroid management, splinting, and PT. Pt includes splinting, carpal mobilization, and gentle stretching. May require surgery if conservative hamate and pisiform, and the volar radiocarpal ligament and volar ligamentous extensions between the carpal bones. The median nerve, for flexor digitorum profundus tendons, and the flexor polllicis longus tendon pass through the carpal tunnel.Carpal tunnel syndrome occurs as a result of compression of the median nerve. The increase in pressure produces ischemia in the nerve and results in of the median nerve. Repetitive use, RA, pregnancy, DM, trauma, tumor, hypothyroidi sm, and wrist sprain or fracture. present with sensory changes along the median nerve distribution in the hand. Night pain, weakness of the hand, muscle atrophy, ↓ grip strength, clumsiness and ↓ wrist mobility. delay along the median nerve. MRI is sometimes used to identify inflammation of the median nerve, altered tendon or nerve positioning. Positive Tinel’s sign, Positive Phalen’s treatment fails. Post surgical should include heat with estim, iontophoresis, cryotherapy, gentle ROM. Pt should initially avoid wrist flexion and a forceful grasp. After 4 weeks, a pt can progress with active wrist flexion, gentle stretching, putty exercises, light progressive resistive exercise, and modification of body mechanics. Radial deviation against resistance should be avoided due to the tendency for irritation. Rehab usually lasts 6-8 weeks. Congenital Torticollis sensory and motor disturbances. Is a condition that causes the neck to involuntarily unilaterally contract to one side secondary to contraction of the sternocleidomas toid muscle. The head is laterally flexed toward the contracted muscle, the chin faces the opposite direction, and there may be facial asymmetries. May be caused by local trauma to the soft tissues of the neck just before or during delivery. Malpositioni ng in utero. Pts head is laterally flexed towards the shortened muscles side and chin is pointed toward the opposite shoulder. Cervical spine X-rays are used to assess potential fracture or subluxation. A CT scan or MRI of the cervical spine can identify the presence of a potential neck mass. Electromyogr aphy study may be useful in defining the degree of muscle or nerve involvement. Typically treated with non-operative intervention for 1224 months before considering surgical intervention. PT includes family/caregiver education and teaching, passive stretching, local heat, analgesics, sensory biofeedback, and TENS. AROM with subsequent strengthening is also indicated to correct the infants positioning of their head. PT is indicated after surgery and should include manual stretching of the neck to maintain the overcorrected position. Manual stretching should be continued 3x daily for 3-6 months. A cervical collar may Degenerative Spondylolisthe sis (DS) Is the forward slippage of one vertebra on the vertebra below. Classifications include congenital, isthmic, degenerative, post-traumatic, and pathologic. Degenerative is caused by the weakening of joints that allows for forward slippage one vertebral segment on the one below due to degenerative changes. Can result in stenosis of the spinal canal. Most common site is L4-L5 level. DS is caused by arthritis and degenerative changes in the spine. Usually affects individuals over 50. More common in African females. Back pain is a primary symptom that is said to increase with exercise, lifting overhead, prolonged standing, getting out of bed or car, walking up stairs on an incline, and positioning in extension. Pain maybe severe and radiate depending on the area of stenosis. Sensory and motor loss may be significant and follow a myotomal Plain radiographs of the vertebral column are adequate to confirm the diagnosis of DS. CT scan or MRI may be indicated to rule out any other contributing conditions or to further assess nerve impingement . be used for first 6-12 weeks after surgery. Management should initially include education, medication, activity modification, and PT. Activity modification and rest should be instituted to further allow inflammation to subside and improve overall symptoms. William’s flexion exercises should be performed to strengthen the abdominals and reduce lumbar lordosis. External support may relive intradiscal pressure. Majority of pts with DS are successful with conservative tx. Fibromyalgia Syndrome (FMS) Is classified as a rheumatology syndrome or a nonartiicular rheumatic condition. Pain the primary symptom caused by tender points within muscles, tendons, and ligaments. Diet, sleep disorders, viral infections, psychological distress, occupational & environment al factors, hypothyrodis m, trauma, and hereditary links. Juvenile RA JRA is a form of arthritis found in children less Develops in children with a genetic or dermatomal distribution. Greater incidence in females and can affect any age but most frequently diagnosed between 1468 years. Widespread hx of pain, 11/18 tender points. Fatigue, memory and visual impairment, sleep disturbance s, irritable bowel syndrome, headaches, and anxiety/dep ression. 3 types of JRA and classified by No specific tests to diagnose FMS. Radiographs are negative and blood work often appears normal except for a possible alteration in the levels of substance P. this substance is a chemical involved with pain transmission. There is not a single test to identify Education, medical management, and exercises. Physicians must address hormonal imbalances, sleep disturbances. Psychotherapy may be warranted for anxiety/depression. PT includes relaxation, heat, ultrasound, posture and body mechanics, biofeedback, improve a pts fitness level. These pts require short exercise sessions initially (3-5 minutes) due to a low tolerance for exertion. FMS is not curable, likely to experience these symptoms for years or even their entire lifetime. A pediatric rheumatologist is ideal to direct a Lateral Epicondylitis than 16. Causes inflammation & stiffness to multiple joints for a period of greater than 6 weeks. An autoimmune disorder occurs when the immune cells mistakenly being to attack the joints and organs. predispositio n for the disease. May be triggered by environment al factors or a viral/bacteria l infection. Girls have a higher incidence of JRA and most commonly in the toddler or adolescent. number of joints involved, symptoms, presence of RF. Symptoms include persistent joint swelling, pain, and stiffness. the presence of JRA. Blood tests may include serum evaluation to measure inflammation and detect RF. Tennis elbow, is characterized by inflammation or degenerative changes at the common extensor tendon that attatches to the lateral epicondlye of the elbow. Repetitive wrist action against resistance during extension and supination appear to produce this condition. Unilateral involvement , pain along the lateral aspect of the elbow and sometimes radiates into the dorsum of the hand. No lab or imaging studies are required to diagnose. Xray or MRI to rule out other conditions. team in the complex care of JRA. Primary goals are to maintain a high level of physical functioning and quality of life. PT should include ROM, exercise, pain control, functional mobility, strengthening, endurance, aerobic trainng. Modalities, splints and orthotics, pt/family education will optimize the quality of life. Surgical intervention is sometimes warranted. Some pts outgrow JRA while others will be on a long term basis. RICE, avoid all activities that aggravate the injury. NSAIDS. Modalities or iontophoresis with dexamethasone. Phonophoresis with hydrocortisone. Resting splints may be used during acute MCL Sprain— Grade II Primary symptom is pain. Continued microtrauma Men are more likely to develop lateral epicondylitis and in individuals in their late 30’s & 40’s. Resists medially directed force at the knee. Primary stabilizer against valgus force and ER of the tibia (especially during knee flexion). A grade II is characterized by partial tearing of the ligament’s fibers resulting in joint Individuals participating in contact activities requiring a high level of agility or susceptible. MOI is usually a blow to the outside of the knee joint. Can also be injured by twisting of Pain will increase with wrist flexion with elbow extension, resisted wrist extension, and resisted radial deviation. The pain usually ↑ with activity and is noted at night. Will present with an inability to fully extend and flex the knee, pain and significant tenderness along the medial aspect of the knee, possible decrease in strength, potential stage to relieve tension in the involved muscles. PT should use stretching & strengthening. All exercise must remain pain free. Counter-force bracing may be indicated. Overall outcome is favorable and should return to previous activities. MRI is extremely expensive and therefore may not be commonly employed with a suspected MCL injury without other extenuating circumstance s. A valgus stress test Conservative management including RICE. Pharm intervention for pain management. May utilize a full length knee immobilizer or a hinge brace and crutches to limit WBing. PT should increase ROM, light resistive exercises. Heel slides, stationary cycling without resistance. Resistive exercises Osteoarthritis laxaity when the ligament is stretched. the knee. loss of propriocepti on, and an antalgic gait. Slight to moderate swelling around the knee. will help detect medial instability. A pt with a grade II MCL sprain may exhibit 5-15° of laxity with valgus stress at 30° of flexion. OA is a degenerative chronic disorder resulting from the biochemical breakdown of articular cartilage in the synovial joints. Primary OA is idiopathic occurring within intact joints and no history that supports the initiation of this condition. Primary OA is related to the aging process and typically occurs in older adults. Joints of the hands, knees, hips, and spine. Decrease in ROM, crepitus, deep and aching pain. Pts have pain during activity that is alleviated by rest and respond to analgesics. Morning OA is typically diagnosed on the basis of clinical examination and x-ray findings. Lab tests will not diagnose OA. should be directed towards the quads and may include isometrics and closed kinetic chain ex. Gait and stair climbing. E-stim, transverse friction massage to the healing ligament so it doesn’t adhere down. Pt should be able to return to previous functional level within 4-8 weeks following injury. Pharm intervention,k glucocorticoid intraarticiular injections may improve symptoms. Nutritional education and weight reduction may be indicated to reduce stress on joints. Posture retraining, work site eval, strengthening, relaxation and hydrotherapy, modalities, pt Osteogenesis Imperfecta (OI) A rare congenital disorder of collagen synthesis that affects all connective tissue in the body. Reduces collagen from 20-50%. Secondary OA results from trauma that has adversely affected the cartilage. In pts greater than 55, the prevalence of OA I higher in women then men. Most children inherit OI from parents as either an autosomal dominant or autosomal recessive trait. 25% of the time the genetic defect occurs by spontaneous mutation of the genes. stiffness, deviated gait pattern, muscle atrophy. 4 types that have a wide range of clinical presentatio ns. Type I is the mildest form & presents with easy bruising, triangular face, and possible hearing loss. Type II is most severe form where a child dies in utero or early education, aquatic therapy, and functional activities. If conservative magnt fails, joint replacement therapy may be indicated. A skin biopsy is used to examine the collagen and determine what type of OI is present. X-rays and bone scans may be used for evidence of deformities and old fxs. Bone densitometry may also be used to measure bone mass and estimate Goals include maximizing independence with mobility, improving optimal bone mass and muscle strength, and prevention of fxs. Pharm intervention has no strong effect. Children should not be given steroids since it may deplete bone and increase fragility. Light weight orthotics may be indicated early to support the extremities and assist with ambulation. Pt childhood. Type III is severe, presents with retardation, progressive deformties, ongoing fxs, severe osteoporosi s, triangular face, significicant limitations in functional mobility. Type IV is usually milder and experience fxs easily prior to puberty, shorter stature, bowing of long bones, possible hearing loss, brittle teeth. the risk of fx. initially focuses on parent handling techniques, recognition of fxs, positioning, and activities that facilitate safe movement. Swimming is agood alternative for strengthening and exercise. All strengthening exercises should avoid rotational forces, placing weights/resistance near a joint, and using long lever arms. Surgical procedures known as “rodding’ may also be indicated if child has more than 2 fxs to the same bone within 6 months. PT may be required intermittently over the pts childhood. A strong predictor of a child’s ability to ambulate in the future also lies in the Osteoporosis Metabolic bone disorder where the rate of bone resorption accelerates while the rate of bone formation slows down; osteoclast activity exceeds osteoblast activity. This decreases the overall bone density and strength. Primarily affects trabecular bone in postmenopausal pt. Risk factors include inadequate dietary calcium, smoking, excessive caffeine, high intake of alcohol or salt, small stature, Caucasian race, inactive lifestyle, family history or chronic disease. Postmenopa usal osteoporosis targets women 5060 years. Senile osteoporosis targets men and women Low thoracic or lumbar pain, experience compressio n fxs of the vertebrae and complain of back pain. Pain is acute and ↑ with WBing and palpation. Pt may also present with deformities such as kyphosis, Dowager’s hump, a decrease in height. No accurate measure of overall bone strength, Xrays are taken to investigate the amount of degeneration and the decrease in density. A bone mineral test accounts for 70% of bone strength and is the easiest way to determine osteoporosis. child’s ability to sit by 10 months. Some have minimal involvement while others use power wheelchairs. Vitamin & supplemental management. Hormone replacement therapy is recommened. PT should include pt education regarding exercise, positioning, pain management, nutrition, and fall prevention. A PT may require a corset our lumbar support if at risk for fxs. Aquatic tx will help but should not replace WBing activity. Surgical intervention may be required for fxs. Pts should be educated to avoid heavy resistance, excessive flexion during exercise, or use of ballistic movements. Patellofemoral Syndrome Is caused by abnormal tracking of the patella between the femoral condyles. Most commonly occurs when the patella is pulled too far laterally during knee extension. Damage can range from softening of the cartilage of complete cartilage destruction resulting in exposure of subchrondral bone. >70 years. Adolescence, More prevalent in females than males, and has a direct associated with the activity level of the pt. Patella alta, insufficnet lateral femoral condyle, weak vastus medialis obliquus, excessive pronation, excessive knee valgus, and tightness in LE muscles (iliopsoas, hamstrings, gastroc, and vastus lateralis. Often describes a gradual onset of anterior knee pain following an increase in physical activity. Located behind the patella and may be exacerbated with activities that increase compressive forces (stair climbing, jumping) and also sitting with knee flexed 90° for prolonged period. Point tenderness is common over the Laboratory or imaging studies are not commonly used to diagnose PF syndrome. Xrays are used to rule out a fx. Arthrogram and arthroscopy can used to examine the articular cartilage. Clarke’s sign can be useful. Pts often have an increased Q angle (13° in males, 18° in females) Q angle is measured using the ASIS, midpoint of patella, and tibial Conservative maganment is usually successful, surgery is rare. PT includes controlling edema, stretching (hams, IT band, TFL and rectus femoris), strengthening (VMO in WBing and nonWBing positions; quad setting, SLR and mini squats) Deep squats should be avoided), improving ROM, and activity modification. Mob activity to ↑medial glide can be beneficial to increase the flexibility of the lateral fascia. Patellar taping can improve position and tracking. An active pt must ↓ their level of activity to relieve additional stress. Pt that undergoes conservative mangt can return to Plantar Fasciitis Imflammatory process at its origin on the calcaneus. PF is a chronic overuse condition that develops secondary to repetitive stretching of the PF through excessive foot pronation during the loading phase of gait. Excessive pronation during gait, tightness of the foot calf muscles, obesity, and possessing a high arch. Running or dancing, prolonged walking or standing are at an increased risk. lateral border of the patella and crepitus may be elicted when the patella is manually compressed into the trochlear groove. Severe pain in the heel when first standing up in the morning. Pain typically subsides for a few hours during the day, but increases with prolonged activity. Described as pain “that moves around” Point tubercle. previous activities within 4-6 weeks. Prognosis is a full recovery unless failure to adequately address the cause of PF syndrome. Initially treated based on symptoms and physical exam. If pain persists after 6-8 weeks of PT, MRI may be used to confirm the diagnosis. Medical and pharm mangt. Requires corticosteroid injections or antiinflammatory medications. PT consists of ice massage, deep friction massage, shoe modification, heel insert, foot orthotic prescription, modifications of activity, gentle stretching. Muscle strengthening for the intrinsic and extrinsic muscles should be implemented once tenderness, usually unilateral and tightness in the Achilles tendon. Reflex Sympathetic Dystrophy Also known as complex regional pain syndrome. Type I (occurring subsequent to trauma) type II (associated with peripheral nerve injury) is usually found in an extremity that has experience some form of trauma. Symptoms result from a disturbance in the functioning of the sympathetic nervous system. This causes a Trauma, surgery, CVA, TBI, repetitive motion disorders, and LMN and periperhal nerve injuries. Most likely found in 3560 years of age with females 3x more likely to be affected than males. Intense burning and chronic pain in the affected extremity that will eventually spread proximally. Edema, thermal changes, discoloratio n, stiffness, and dryness are seen during stage I (acute stage). Progression to stage II (dystrophic X-rays may reveal bone less, osteoporosis, erosion. Thermograp hic studies, laser Doppler flowmetry. the acute symptoms have subsided. Night tension splints may be indicated is symptoms persist. Pt should return to functional level within 8 weeks. Total resolution of symptoms can take up to 12 months. RSD requires prolonged medical management. Tx is based on identifying the underlying cause and stage of RSD at the time of diagnosis. Surgical interventions such as sympathetic blocks, or a sympathectomy are used to alleviate pain. PT includes pain control, pt education, skin care, joint mob, desensization, functional activity training. Overall prognosis is better for a pt that beings tx early in the cycle. release of norepinephrine in the periphery and subsequent vasoconstriction of blood vessels. This results in pain and ↑ in sensitivity to peripheral stimulation RA Rheumatoid Arthritis is an autoimmuine disorder of the connective tissue that is characterized by chronic inflammation within the synovial membranes, Genetic predispositio n with viral or bacterial triggers. The incidence of RA in women is 3x greater than in men. Diagnosed most frequently stage) is characterize d by worsening and constant pain, tropic skin changes. Stage III (atrophic stage) is characterize d by continued pain, hardened edema, atropic changes to fingertips or toes. RA will vary in onset and progression from pt to pt. May be sudden or develop over a period of weeks. Early signs include RSD can spontaneously resolve, continue with ongoing symptoms that can last for years or follow a pattern of remissions. Research indicates a better prognosis if treatment is initiated within the first 6 months of the disease. Blood work assists with the diagnosis of RA through evaluation of the RF, white blood cell count, erythrocyte sedimentatio n rate, Early medical mangt is critical to improve the long term outcomes of the disease. It will focus on pain relief, reduction of edema, and preservation of joint integrity. PT includes pt education regarding regular rest, pain Rotator Cuff Tendonitis tendon sheaths, & articular cartilage. Smaller peripheral joints are usually the first to be affected. between 3050 years of age. Repetitive overload can produce impingement of the supraspinatus tendon Individuals participating in activities that require excessive overhead activity such fatigue, bilateral involvement , tenderness of smaller joints, & low grade fever. Pts experience pain with motion, stiffness, progression of symptoms to larger synovial joints. In later stages the heart can become affected and deformities, subluxations and contracture s can occur. Often reports difficulty with overhead activities and a dull hemoglobin, and hematocrit values. A synovial fluid analysis evaluates the content of synovial fluid within the joint. X-rays can be used to evaluate the joint space and the extent of decalcificatio n. relief, relaxation, positioning, joint protection techniques, gentle massage, hydrotherapy, hot pack, paraffin, or cold modalities, gentle isometrics, and instruction in use of assistive devices. Low impact conditioning, endurance and strength during remission. PT cannot halt RA but can improve a pts ability to function. No known cure that creates irreversible damage and deformity and results in disability. MRI can be used to identify the presence of rotator cuff tendonitis, however, Early PT: cryotherapy, activity modification, ROM, & rest. After pain subsides pt is instructed in strengthening immediately proximal to the greater tubercle of the humerus. The impingement is caused by an inability of a weak supraspinatus muscle to adequately depress the head of the humerus in the glenoid fossa during elevation of the arm. As a result the humerus translates superiorly due to the disproprotionat e action of the deltoid. as swimming, tennis, baseball, painting, and other manual labor. Individuals from 25-40 years of age are the most likely to develop this condition. ache following periods of activity. The pt may experience a feeling of weakness and identify the presence of a painful arc of motion most commonly occurring between 60120° of active abduction. Pt usually presents with pain with palpation of the musculoten dinous junction of the involved muscle or with stretching or resisted due to the high cost is not commonly employed prior to formal treatment. Xrays with the shoulder laterally rotated can be used to identify the presence of calcific deposits or other bony abnormalitie s. Special tests including the empty can, jobe test, neer’s, Hawkinskennedy can be used to confirm. exercise. All ROM should be pain free. ROM using a pulley system or a cane can serve as an effective intervention. Elastic tubing and hand held weights are often preferred. Shoulder shrugs and push-ups with arms abducated to 90° can effectively be used to strengthen the upper trap and serraus anterior. Pt should be able to return to previous level of functioning within 4-6 weeks. Also depends on classification of stage. Stage I is population less than 25 years. Stage II is 25-40 years. Stage III end stage and likely over 40. Sciatica A herniated disk Secondary to a is an herniated Disk intervertebral disk that bulges and protrudes posterolaterally against a nerve root. Sciatica is the diagnosis of compression of The natural aging process. Each decade the composition of the annulus fibrosus and nucleus pulposus is contraction of the muscle. Pain often increases at night resulting in difficulty sleeping on the affected side. Difficulty with dressing, and repetitive motions such as lifting, reaching, throwing, swinging or pushing and pulling. Low back & gluteal pain that typically radiates down the back of the thigh along the sciatic nerve Radiologic testing of the spine and electrophysi ologic studies are initially performed to assist with diagnosis. Short-term bed rest, overall reduction of intradiskal pressure, pt education, PT, meds and in rare instances surgical intervention. PT will include pain mangt, traction, heat, lumbar endurance the sciatic nerve (L4, L5, S1, S2, S3) secondary to a herniated disk causing pts symptoms. Other causes of sciatica include tumor, infection, spondyloisthesis , narrowing of the canal, and blood clots. altered and decreases in overall stability. Once there is adequate structural breakdown within the disk, a pt becomes high risk for injury. As expected, sciatica secondary to a hearniated disk is most often seen in pts between 40 and 60 years. distribution. Sciatic pain occurs from nerve root compressio n and can be dull, aching or sharp. Pain may have a sudden onset or develop gradually over time. Early sciatica may involve discomfort or pain limited to the low back and gluteal region. Leg pain can become greater than the back pain and can radiate the entire length of the nerve to Other imaging may include myelogram, discography, CT scan or MRI. Blood work may assist with differential diagnosis. The SLR will reproduce symptoms in the case of a herniated disk. activities, mckenzie exercises, stretching, and walking are indicated with tolerance. Lifting, squatting, and climbing are contraindicated due to the significant ↑ in intradiskal pressure.Most herniations will spontaneously decrease in size with conservative treatment. Research indicates majority of pts will improve with 2-4 months of conservative tx, however 2% undergo surgery. Pts needs stabilization exercises at home. This condition can be corrected through rest and PT. Healing of the disk can also occur and scarring can reinforce the posterior aspect and annular fibers so that it is protected Scoliosis Pt presents with lateral curvature of the spine. The curve is usually found in the thoracic or lumbar area. The curve of the spine may be towards the right or left & Idiopathic scoliosis, accounts for 80% of all cases. Upwards of 1:10 children are affected by some form of scoliosis with the toes. The pt may also experience intermittent numbness and tingling localized to the dermatomal distribution, limited thoracolum bar range of motion in all planes, tenderness to palpation at the segment of herniation and muscle guarding. A pt with a structural curve will present with asymmetrie s of the shoulders, scapulae, pelvis, and skinfolds. Juvenile from further protrusion. X-ray should be taken in an anterior and lateral view with the pt standing and with the pt bending over. A device called Based on the type and severity of the curve. E-stim to alleviate pain and biofeedback for education with proper posture and positioning. A pt with scoliosis that is less than 25° should be monitored every with our without rotation. Typically, the rotation will occur towards the convext side to the major curve. 1:4 requiring treatment for the curve. Infantile (03), juvenile (4-puberty), adolescent (12 for girls, 14 for boys), or adult (skeletal maturation) scoliosis. Nonstructural scoliosis is a reversible curve that can change with repositioning . Thisi type of curve is non progressive and is usually cased by poor posture or leg length discrepancy. Structural scoliosis cannot be corrected with idiopathic scoliosis is characterize d by a thoracic curve with convexity towards the right. As the curve progresses there will be a rib hump posteriorly over the thoracic region on the convex side of the curve. Adolescent scoliosis of greater than 30° is seen more in females than males. Curves that are less than 20° rarely cause a person to experience significant a scoliometer can be used to measure the angle of trunk rotation. The Cobb method can be used to determine the angle of curvature. A bone scan or MRI can be used to determine and rule out conditions such as infections, neoplasms, spondylosis, disk herniations, or compression fractures. 3 months. Breathing exercises & a strengthening program for the trunk and pelvic muscles are indicated. A pt with scoliosis that ranges beween 25 & 40° requires a spinal orthosis and PT for posture, flexibility, strengthening, respiratory function, and proper utilization of the spinal orthosis. A pt with scoliosis greater than 40° usually requires surgical spinal stabilization. One method is spinal fusion and stabilization with a Harrington Rod. Prognosis for structural scoliosis is based on the age of onset and severity of the curve. Early intervention results in the best possible outcome. If the Spondylolisthe sis Refers to forward slippage of one vertebral body with respect to the vertebral body below it. In many cases there can be symptoms that range from localized or radiating pain to significant nerve compression, radiculopathy or neurogenic claudication. Spondylosis has a 2:1 male to female predominance compared to all forms of spondylolisthesi s, which movement and can be caused by congenital, musculoskele tal, and neuromuscul ar reasons. A defect in the pars interarticulari s that may produce the forward slippage of a vertebrae as found with spondylolisth eiss. High risk activities include gymnastics, wrestling, football, and weight lifting. problems or impairment s. Pain is the most common symptom. If the pt is young, pain is usually confined to the area of slippage and may occasionally radiate. Progression involves neurological , motor, sensory, and reflex changes. Pain is usually provoked with activity especially when it curvature is over 50° there likely will be ongoing progression of the curve each year of life. Lateral and anteroposter ior plain xrays of the lumbar spine should be obtained. The oblique view can show the pars as having the appearance of a “Scottie dog with a collar” when a spondylosis is present. Other studies may include a bone scan, CT scan and myelogram. Lab studies will not assist with Initially treated conservatively regardless of the type or causative factors. PT is indicated with emphasis on activity modification, pt education on disease process, bracing, and therapeutic stretching and strengthening. Exercise protocols should include exercise and activity that reduces stress with spinal extension. Conservative treatment is very successful especially with the younger pt, however, surgery may be indicated for indicated a female to male predominance of 2:1. Overall, females tend to me more prone to progressive spondyloisthesis and require surgery. Temporomand TMJ is a ibular Joint complex joint Dysfunction that is classified as a condylar, hinge, and synovial joint. The TMJ contains fibrocartilaginou s surfaces & articular discs. TMJ dysfunction occurs due to a change in the joint structure that can cause multiple symptoms and a limitation in function. In many instances inflammation & muscle spasm surrounding the Predisposing factors, triggering factors, and perpetuation /sustaining factors. Can occur due to injury or trauma to the joint, congenital abnormalitie s, internal derangement of joint structure, arthritis, dislocation, disk degeneration , metabolic conditions or stress. Habits involves extension of the spine. diagnosis. unsuccessful pts. A pt will present with symptoms that include pain, muscle spasm, abnormal or limited jaw motion, headache, and tinnitus. Pt will often complain of feeling and hearing a “clicking or popping” sound with motion at the TMJ. May include x-ray, MRI, mandibular kinesiograph y, CT scan, and a dental examination. Pharm management, splint to assist with realignment of the joint and a guard or bite plate to maintain proper position. PT is based on the exact etiology of the dysfunction. It includes pt education, postural retraining, moist heat, ice, biofeedback, ultrasound, e-stim, TENS, stretching, joint mobs, ROM and relaxation. PT intervention should improve a pts condition and decrease the symptoms. If conservative joint produces symptoms for the pt. Total Hip Warranted secondary to progressive and severe osteoarthritis or RA, developmental dysplasia, tumors, nonuntion fx, avascular necrosis. Destruction of cartilage resuls in bone to bone contact. of gum chewing and nail biting may increase the incidence of injury. Pts are typically between 2040 years with a greater incidence in women. Intraarticular disease or the destruction of articular cartilage may come for arthritis, repetive microtrauma, obesity, nuturitional imbalances, falls or abnormal joint mechanics. treatment fails, surgery may be required. Pt will present with decreased ROM, impaired mobility skills, and persistent pain that increases with motion and weight bearing. The pt is usually over 55 years of age and has experienced consistent pain that is not relieved through X-ray, CT and MRI procedures may be used to view the integrity of the joint. These procedures are also used to rule out a fx or tumor. Contraindicat ions for surgery include active infection, severe obesity, arterial insufficiency, A THA that utilizes a posteriorlateral approach allows the abductor muscles to remain intact, however there may be a higher incidence of joint instability due to the interruption of the posterior capsule. Management will include pharm (anticoagulant), hip precautions, ankle pumps, quad sets, gluteal sets, heel slides, and isometric abduction, scar management. At the time of hospital discharge the pt Total Knee May be warranted secondary to progressive and disabling pain within the knee joint. Destruction of articular cartilage secondary to OA. conservativ e measures. NM disease, and certain mental illness. Severe knee pain that worsens with motion and weight bearing, limited ROM, possible deformity and impaired mobility. X-ray, CT, and MRI imaging are used to determine the extent of deterioration . A pain assessment scale and the Arthritis Impact Measuremen t tool may be used. should be able to extend the hip to neutral and flex the hip to 90°. The pt should have diminished to no pain, increased strength and endurance, and improved mobility within 6-8 weeks after surgery. Post-operative care includes a knee immobilizer, elevation of the limb, crotherapy, CPM, and initiation of knee protocol exercises. A noncemented knee requires toe touch weight bearing for up to 6 weeks to allow the bone to grow and affix to the prosthesis. PT should focus on mobility training with the AD. Early ambulation is encouraged in order to avoid Deconditioning and Total Shoulder Sever pain and impaired shoulder motion due to deterioration of the GH joint. These Degenerative joint disease, pain and limited ROM secondary to OA, RA, avascular Pt will exhibit impaired ROM at the shoulder, may lack independen X-ray will reveal the level of degeneration within the shoulder complex. the risk of DVT. PT should include ankle pumps, quad sets, and hamstring sets as well as ROM and stretching. A goal of 90° of knee flexion and 0° knee extension is often established prior to discharge. Precautions follow surgery for several months: avoid squatting, avoid quick pivoting, do not use pillows under the knee while in bed, and avoid low seating. The pt should experience relief of pain that will allow a full return to previous functional activities within 8-12 weeks after surgery. A pt status post TSA will remain hospitalized for an average of 2-5 days. A CPM may be prescribed by the surgeon for the use candidates have undergone conservative treatment measures that have failed to improve their condition. necrosis, fracture or rotator cuff arthropathy. Others are bone tumor, Paget’s disease or with recurrent dislocations. ce with functional mobility and ADLs, and severe pain. It is this unremitting pain (with failed conservatice treatment) that is the primary indication for TSA. Usually performed on pts between 5570 years. MRI or CT will allow the physician to assess the integrity of the rotator cuff and deltoid muscles surrounding the joint. during the pts hospitalization. PT is initiated the day after surgery and should follow the shoulder rehab protocol designed by the surgeon. The shoulder usually remains immobilized using a sling during initial rehab. The Neer shoulder protocol advocates initiating isometric shoulder exercise approx. 3 weeks after surgery and active shoulder exercises 6 weeks after surgery. PROM and AAROM are indicated but AROM at the shoulder is contraindicated during the first phase of rehab. PT includes pain mgnt, AROM, therapeutic ex, edema management, pt education in selfROM and wand/pendulum ex Transfemoral Amputation due to Osteosarcoma Osteosarcoma is the 2nd most common primary bone tumor and is a highly malignant cancter that begins in the medullary cavity of a bone and leads to the formation of a mass. It usually affects bones with an active growth phase such as the femur or tibia and is often located in the metaphysic. Osteosacrom as can occur as a primary or secondary cancer and the etiology is unknown. This form of tumor primarily affects young children (especially males), adolescents, and young adults under 30 years of age. A peak time for incidence is and use of modalities. A pt must not perform any form of medial rotation or lateral rotation beyond 3540° during the first 2-3 weeks post surgery. PT should assist the pt to meet goals of relieving pain and regaining functional motion. Found most X-ray, MRI Physical & often in long and occupational bones at the scintigraphy therapies should site of the allow the begin immediately most active physician to after the epiphyseal determine transfemoral growth the amputation. plate, the presence, Preprosthetic distal femur, location, and intervention should proximal size of a focus on ROM, tibia, tumor. The positioning, proximal “Codman’s strengthening, humerus, triagle” can desensitization, and and pelvis. be seen on x- pt education for care The knee ray indicating of the residual limb. region reactive Pts with a accounts for bone at the transfemoral approx 50% site where amputation should of the lie prone for period osteosarco periosteum of time each day to mas. Pts has been prevent a hip flexion Transtibial Amputation due to Arteriosclerosi s Obliterans Amputation may be necessary to remove the tumor and surrounding tissues to avoid metastic disease. during a growth spurt. Arteriosclerosis obliterans (AKA peripheral arterial disease; PAD) is a form of peripheral vascular disease that produces thickening, hardening, and eventual narrowing and Risk factors associated with arteriosclero sis obliterans include age, diabetes, sex, HTN, high serum cholesterol and lowdensity lipid that require amputation secondary to an osteosarco ma will present with a mass often found in the tibia or femur. Most common symptoms are pain and swelling, pain worse at night or with exercise a lump may develop. The pt that requires a transtibial amputation secondary to this condition is typically an individual over 45 years that smokes and elevated by the neoplasm. Definitive diagnosis for an osteosarcom a is made through tissue biopsy of the tumor. contracture. Modalties may be used to improve ROM and decrease pain. Serial casting may be indicated if a contracture develops. Without complication the pt should be able to return home with support and receive short term physical therapy for prosthetic training. Arteriosclero sis obliterans can be diagnosed using Doppler ultrasonogra phy, MRI or arteriograph y. These diagnostic tests A pt should be a candidate for inpatient PT services immediately after the transtibial amputation. Preprosthetic intervention should focus on strength, ROM, functional mobility, use of Ads, desensitization, and occlusion of the arteries. This results in ischemia and subsequent ulceration of the affected tissues. The affected area may become necrotic, gangrenous, and require amputation. levels, smoking, impaired glucose tolerance, obesity, and sedentary lifestyle. Unsuccessful mangt of PVD may ultimately lead to uncontrolled infection, gangrene, necrosis, and amputation. Males have an overall higher incidence of arteriosclero sis than females. will present with intermittent claudication that produces cramps and pain in the affected areas. Resting pain, decreased pulses, ischemia, pallor skin, and decreased skin temp. examine the degree of blood flow throughout the extremities. pt education. A pt should be able to achieve estabilished goals and function with a prosthesis and an AD if warranted. Pharmacological Management of the MS System: Drug Nonopiod Agents Opioid Agents Action Indications Side Effects Provide analgesia and pain relief, produce antiinflammatory effects, and initiate antipyretic properties. These drugs promote a reduction of prostaglandin formation that decreases the inflammatory process, decreases uterine contractions, lowers fever, and minimizes impulse formation of pain fibers. Opioid agents Mild to moderate pain of various origins, fever, headache, muscle ache, inflammation (except acetaminophen ), primary dysmenorrheal , reduction of risk of myocardial infaction (aspirin only) Nausea, vomiting, vertigo, abdominal pain, gastrointestin al distress or bleeding, ulcer formation, potential for Reye syndrome in children (aspirin only) Moderate to Mood swings, Implications for PT Pts are at increased risk for masked pain that would allow for movement beyond limitation or false understanding of their level of mobility. Complaints of stomach pain should be taken seriously with a subsequent referral to a physician. A therapist Examples Tylenol (acetaminoph en); Nonsteroidal antiinflammatorie s (NSAIDS): Aspirin (acetylsalicylic acid), Aleve (naproxen), Advil (ibuprofen, Celebrex (celecoxib) Roxanol (narcotics) provide analgesia for acute severe pain management. The medication stimulates opioid receptors within the CNS to prevent pain impulses from reaching their destination. Certain drugs are also used to assist with dependency and withdrawal symptoms. severe pain of various origins, induction of conscious sedation prior to a diagnostic procedure, management of opiod dependence, relief of severe and persistent cough (codeine) sedation, confusion, vertigo, dulled cognitive function, orthostatic hypotension, constipation, incoordination , physical dependence, tolerance Glucocorticoid Agents (Corticosteriods) Glucocorticoids provide hormal, antiinflammatory, and metabolic effects including suppression of articular and Replacement therapy for endocrine dysfunction, anti inflammatory and immunosuppre ssive effects; Muscle atrophy, GI distress, glaucoma, adrenocortical suppression, drug induced Cushing syndrome, must monitor the pt for potential side effects, especially signs of respiratory depression. Treatment that is otherwise painful should be scheduled approximately 2 hours after administration to maximize the analgesic benefit. A pt may not accurately report if a particular technique is painful. A therapist must wear a mask when working with pts on glucocorticoid therapy since their immune system is (morphine), Demerol (meperidine), Oxycontin (oxycodone), Sublimaze (fentanyl), Paveral (codeine) Deermacort (hydrocortison e or cortisol), Cordrol (prednisone), Prediapred (prednisolone) , Medrol (methylpredis Diseasemodifying Antirheumatic Agents systemic diseases. These agents reduce inflammation in chronic conditions that can damage healthy tissue through a series of reactions. Vasoconstrictio n results from stabilizing lysosomal membranes and enhancing the effects of catecholamines . treatment of rheumatic, respiratory, and various other diseases weakening with breakdown of supporting tissue (bone, ligament, tendon, skin) mood changes, HTN DMARDS slow or halt the progression of rheumatic disease. They are used early during the disease process to slow the progression Rheumatic disease, preferably during early treatment Nausea, headache, joint pain and swelling, toxicity, GI distress, sore throat, fever, liver dysfunction, hair loss, weakened. A therapist must be aware of signs of toxicity including moon face, buffalo hump, and personality changes. Pts are at risk for osteoporosis and muscle wasting. Treatment of an injected joint will require special care due to ligament and tendon laxity or weakening. Therapists should recognize that many of the gents have a high incidence of toxicity. olone), Decadrol (dexamethaso ne), Nasonex (mometasone) Rheumatrex (methotrexate ), Arava lefunomide), Antimalaria: Aralen (chloroquine), Plaquenil (hydroxychlor oquine); Gold prior to widespread damage of the affected joints. They act to induce remission by modifying the pathology and inhibiting the immune response responsible for rheumatic disease. potential for sepsis, retinal damage Individual Joints MS: Shoulder: Upward rotators: Upper trap, lower trap, serratus anterior Downward rotators: Levator scapulae, rhomboids External rotators: Infraspinatus, teres minor, deltoid Internal rotators: Subscapularis, Latissimus, teres major, pec major & minor Abductors: deltoid, supraspinatus Adductors: subscapularis, pec major, lat, teres major & minor ROM: FLEX/ABD: 180 ER: 90 IR: 90 EXT: 60 compounds: Ridaura (auranofin), Solganal (aurothiogluco se); Tumor necrosis factor inhibitors: Humira (adalimumab), Enbrel (etanercept) Arthrokinematics: Motion to Increase Abduction Early flexion (0-45) Internal rotation Horizontal adduction Extension/lateral rotation Horizontal abduction Late flexion (120-180) Mobilization Glide Inferior or caudal glide Posterior glide Posterior glide Posterior glide Anterior glide Anterior glide Anterior glide Degree of Abduction: First 20 degrees: Supraspinatus 90-150 degrees: serratus anterior and trapezius Degree of Elevation: 0-60 degrees: anterior delt, coracobrachialis, pec major 60-120 degrees: serratus anterior, and trap Force couple of the shoulder: -Downward rotation: levator and rhomboids vs. lat, pec major and minor -Upward rotation: serratus (most effective rotator) and upper trap vs. lower trap that contributes during later phase of shoulder abduction Peripheral Nerve Tests: •Spinal Accessory nerve-Inability to abduct the arm beyond 90 degree, Pain in shoulder with abduction •Musculocutaneous nerve- Weak elbow flexion with forearm supinated •Long thoracic nerve- Pain on flexing fully extended arm, inability to flex fully on extended arm, winging of scapula at 90 degree of forward flexion •Suprascapular nerve- Increased pain on forward shoulder flexion, pain increased with scapular abduction, pain increased with cervical rotation to opposite side *Painless weakness is usually due to neurologic problems or myopathies. * Shoulder weakness may be caused by a rotator cuff tear or nerve injury. * Symptoms that are not associated with movement should alert the clinician to a more serious condition. * Pain that is worse at night, but increased when rolling onto the shoulder, points to periarticualr mechanical problems. * Pain that occurs between 70-110 degrees of abduction is deemed a “painful arc” and may indicate rotator cuff impingement, or tearing, or subacromial bursitis. Pain which occurs in the 120-160/160-180 degrees range, may indicate involvement of the A-C joint. * Loss of ACTIVE motion with preservation of PASSIVE motion is likely caused by rotator cuff tear. * A severely restricted active abduction pattern with NO pain is suggestive of a rupture of the supraspinatus or deltoid. * Loss of BOTH active AND passive motion is usually caused by adhesive capsulitis. * A loss of passive OR active ROM may be associated with a loss of flexibility in the passive restraints to motion. Muscles prone to tightness-Upper trap, levator, pec major and minor, upper cervical extensors, sternocleidomastoid, scalene, teres major and minor, subscapularis Muscles prone to lengthening-Middle and lower trap, rhomboids, serratus anterior, deep neck flexors, supraspinatus, infraspinatus Closed packed position-90 degress of GH ABD & full ER Capsular pattern: Most limited: ER, ABD, & IR (least) Common MMT for the shoulder: 1. Scapular Elevation (Upper trap, Levator Scap): Sitting, apply resistance over superior aspect of shoulders in inferior direction. Gravity Eliminated: Pt prone 2. Scapular Adduction (Middle trap): Pt prone and performs active scapular adduction. Examiner applies resistance over lateral aspect of scapula in direction of scapular abduction. Gravity eliminated: Seated c shoulder abducted to 90 degrees and full lateral rotation. 3. Scapular adduction and depression (Lower trap): Prone c upper extremity in ~130 abd and 0 degrees elbow extension. Apply resistance over lateral aspect of scapula. Gravity eliminated: No separate test. 4. Scapular adduction and downward rotation (Rhomboid major and minor): Pt prone with upper extremity behind back. Shoulder in medial rotation and adduction (dorsum of hand on gluteal region). Apply resistance on vertebral border of scapula in direction of scapular abduction and upward rotation. Gravity eliminated: Pt seated with arm behind back. 5. Scapular abduction and upward rotation (Serratus Anterior): Pt supine with UE in 90 degrees shoulder flexion and elbow extension. Apply resistance by grasping wrist and pushing down. Gravity eliminated: Seated with UE in 90 degrees shoulder flexion with arm supported on flat surface. 6. Shoulder flexion (anterior delt, coracobrachialis): Pt seated with UE in 0 degrees flexion and adduction, palm facing trunk. Apply resistance proximal to elbow. Gravity eliminated: Side-lying with arm to be tested uppermost and supported. 7. Shoulder extension (Lat, Teres major, pos delt): Pt prone, with palm facing ceiling. Pt raises arm through range, apply resistance just proximal to elbow. Gravity eliminated: Side-lying with arm to be tested uppermost and supported. 8. Shoulder abduction (Middle delt, supraspinatus): Seated. Apply resistance proximal to elbow. Gravity eliminated: Supine on firm surface. 9. Shoulder horizontal abduction (posterior delt): Pt prone with upper extremity in 90 degree shoulder abduction, 90 degree elbow flexion, arm hanging off table. Apply resistance over distal humerus. Gravity eliminated: Seated 10. Shoulder horizontal adduction (Pec major): Supine with UE in 90 degrees shoulder abd, 90 degree elbow flexion. Have pt horizontally adduct shoulder; apply resistance just proximal to elbow in direction of abduction. Gravity eliminated: Seated 11. Shoulder Internal rotation (Subscapularis, Pec major, Lat, Teres major): Prone with UE in 90 degrees shoulder abduction, 90 degrees elbow flexion, arm hanging down. Pt moves through full range of IR, apply resistance just proximal to wrist in direction of ER. Gravity eliminated: Prone, with arm hanging off side of table, rotate humerus along long axis. 12. Shoulder external rotation (Infraspinatus, teres minor): Prone with UE in 90 degrees shoulder abduction, 90 degrees elbow flexion, arm hanging down. Pt moves through full range of ER, apply resistance just proximal to wrist in direction of IR. Gravity eliminated: Prone, with arm hanging off side of table, rotate humerus laterally along long axis. Special tests for the Shoulder: Dislocation: 1. Apprehension test for anterior shoulder dislocation: The pt is positioned in supine with arm in 90 degrees abduction. Therapist laterally rotates pts shoulder. A positive test is indicated by a look of apprehension or a facial grimace prior to reaching end point. 2. Apprehension test for posterior dislocation: The pt is positioned in supine with the arm in 90 degrees of flexion and medial rotation. The therapist applies a posterior force through the long axis of humerus. A positive test is indicated by a look of apprehension. Biceps tendon Pathology: 1. Ludington’s test: The pt is positioned in sitting and is asked to clasp both hands behind the head with the fingers interlocked. The pt is then asked to alternately contract and relax the biceps muscles. A positive test is indicated by absence of movement in the biceps tendon and may be indicative of a rupture of the long head of the biceps. 2. Speed’s test: The pt is positioned in sitting or standing with the elbow extended and the forearm supinated. The therapist places one hand over the bicipital groove and the other hand on the volar surface of the forearm. The therapist resists active shoulder flexion. A positive test is indicated by pain or tenderness in the bicipital groove region. 3. Yeargason’s test: The pt is positioned in sitting or standing with the arm in 90 degrees of elbow flexion and forearm pronated. The humerus is stabilized against the pts thorax. The therapist places on hand on the patient’s forearm and the other hand over the bicipital groove. The patient is directed to actively supinate and laterally rotate against resistance. A positive test is indicated by pain or tenderness in the bicipital groove and may be indicative of bicipital tendonitis. Rotator Cuff Pathology/Impingement: 1. Drop arm test: The pt is positioned in sitting or standing with the arm in 90 degrees of abduction. The pt is asked to slowly lower the arm to their side. A positive test in indicated by the patient failing to slowly lower the arm to their side or by the presence of severe pain and may be indicative of a tear in the rotator cuff. 2. Hawkins-Kennedy Impingement test: The pt is positioned in sitting or standing. The therapist flexes the pts shoulder to 90 degrees and then medially rotates the arm. A positive test is indicated by pain and may be indicative of shoulder impingement involving the supraspinatus tendon. 3. Neer impingement test: The pt is positioned in sitting or standing. The therapist positions one hand on the posterior aspect of the patient’s scapula and the other hand stabilizing the elbow. The therapist elevates the patients arm through flexion. A positive test is indicated by a facial grimace or pain and may be indicative of shoulder impingement involving the supraspinatus tendon. 4. Supraspinatus test(empty can): The pt is positioned with the arm in 90 degrees of abduction followed by 30 degrees of horizontal adduction with the thumb pointing downward. The therapist resists the patient’s attempt to abduct the arm. A positive test is indicated by weakness or pain and may be indicative of a tear of the supraspinatus tendon, impingement, or suprascapular nerve involvement. Thoracic Outlet Syndrome: 1. Adson maneuver: The pt is positioned in sitting or standing. The therapist monitors the radial pulse and asks the pt to rotate their head to face the test shoulder. The pt is then asked to extend their head while the therapist laterally rotates and extends the pts shoulder. A positive test is indicated by an absent or diminished radial pulse and may be indicative of thoracic outlet syndrome. 2. Allen test: The pt is positioned in sitting or standing with the test arm in 90 degrees of abduction, lateral rotation, and elbow flexion. The pt is asked to rotate the head away from the test shoulder while the therapist monitors the radial pulse. A positive test is indicated by an absent or diminished pulse when the head is rotated away from the test shoulder. A positive test may be indicative of thoracic outlet syndrome. 3. Costoclavicular syndrome test (military brace): Pt positioned in sitting. The therapist monitors the pts radial pulse and assists the pt to assume a military posture. A positive test is indicated by an absent or diminished radial pulse and may be indicative of thoracic outlet syndrome caused by compression of the subclavian artery between the first rib and the clavicle. 4. Roos test: The pt is positioned in sitting or standing with the arms positioned in 90 degrees of abduction, lateral rotation, and elbow flexion. The pt is asked to open and close their hands for three minutes. A positive test is indicated by the inability to maintain the test position, weakness of the arms, sensory loss or ischemic pain. A positive test may be indicative of thoracic outlet syndrome. 5. Wright (hyperabduction test): The pt is positioned in sitting or supine. The therapist moves the pts arm overhead in the frontal plane while monitoring the pts radial pulse. A positive test is indicated by an absent or diminished radial pulse and may be indicative of compression in the costoclavicular space. Miscellaneous: 1. Glenoid Labrum tear test “clunk test”: The pt is positioned in supine. The therapist places one hand on the posterior aspect of the pts humeral head while the other hand stabilizes the humerus proximal to the elbow. The therapist passively abducts and laterally rotates the arm over the patient’s head and then proceeds to apply an anterior directed force the humerus. A positive test is indicated by a clunk or grinding sound and may be indicative of a glenoid labrum tear. 2. Upper limb tension tests: Neural provocation maneuvers. Symptoms and relevant changes in symptoms should be identified after each step. Non-involved side tested first. Joint position ULTT 1 Shoulder depression with 110° abd, elbow ext, forearm supination, wrist ext, finger and thumb ext “yay position” ULTT 2 Shoulder depression with 10° abd, elbow ext, forearm supination, wrist ext, finger and thumb ext, shoulder lateral rotation ULTT 3 Shoulder depression with 10° abd, elbow ext, forearm pronation, wrist flexion, ulnar deviation, finger and thumb flexion, shoulder medial ULTT 4 Shoulder depression with 10-90° abd, elbow flexion, forearm supination, wrist ext, radial dev, finger and thumb ext, shoulder lateral rotation “waiter’s Sensitization Test Contralateral cervical Contralateral cervical lateral flexion lateral flexion Nerve Bias Median nerve, anterior interosseous nerve Median nerve, musculocutaneous nerve, axillary nerve rotation “waiter’s tip” Contralateral cervical lateral flexion Radial nerve tray position” Contralateral cervical lateral flexion Ulnar nerve Shoulder conditions: 1. Glenohumeral subluxation and dislocation: •Most dislocations (95%) occur in anterior-inferior direction. •Anterior-inferior dislocation occurs when abducted upper extremity is forcefully, externally rotated, causing tearing of the inferior glenohumeral ligament, anterior capsule, and occasionally glenoid labrum. •Posterior dislocations are rare, and occur with multidirectional laxity of glenohumeral joint. •Posterior dislocation occurs with horizontal adduction and internal rotation of glenohumeral joint. •Complications include compression fracture of posterior humeral head (Hill-Sachs lesion), tearing of superior glenoid labrum from anterior (front) to posterior (back) (aka SLAP superior labrum, anterior to posterior) lesion, an avulsion of anteroinferior capsule and ligaments associated with glenoid rim (Bankart’s lesion), and bruising of axillary nerve. •Following surgical repair for dislocation/chronic subluxation, pts should avoid apprehension position (flexion to 90 or greater, horizontal abduction to 90 or greater, and ER to 80) •Diagnostic tests utilized: plain film, CT, or MRI •Diagnosis made by clinical examination. Apprehension tests will be positive. Goals, outcomes, interventions: PT intervention is varied, depending on if surgery is indiciated. Biomechanical faults caused by joint restriction should be corrected with joint mobs. 2. Instability: •Divided into two categories: traumatic (common in young throwing athletes), and atraumatic (individuals with congenitally loose connective tissue around the shoulder). •Characterized by popping/clicking and repeated dislocation/subluxation of the GH joint. •Unstable injuries require surgery to reattach the labrum to the glenoid. •Bankart’s lesions require surgery. •Diagnosis made by clinical exam by comparing results of pt history with the AROM, PROM, resistive tests, and palpation. •MRI arthrograms are VERY effective in identifying labral tears. •Meds: acetaminophen for pain, NSAIDS for pain/inflammation Goals, outcomes, interventions: Intervention emphasizes return of function without pain. Functional training and restoration of muscle imbalances using exercise to normalize strength. • For patients requiring surgery, the shoulder is usually kept in a sling for 3-4 weeks. After 6 weeks, more sports-specific training can be done, although full fitness may take 3-4 months. 3. Labral tears: • Glenoid labrum injuries are classified as either superior (toward the top of the glenoid socket) or inferior (toward the bottom of the glenoid socket). A SLAP lesion is a tear of the rim above the middle of the socket that may also involve the biceps tendon. A tear of the rim below the middle of the glenoid socket is called a Bankart’s lesion, and also involves the inferior glenohumeral l igament. Tears of the glenoid labrum may often occur with other shoulder injuries, such as a dislocated shoulder. • Characterized by the following signs and symptoms: -Shoulder pain that cannot be localized to a specific point -Pain is made worse by overhead activities or when the arm is held behind the back -Weakness -Instabilitiy in the shoulder -Pain on resisted flexion of the biceps -Tenderness over the front of the shoulder • Unstable injuries require surgery to reattach the labrum to the glenoid. Bankart’s lesions require surgery. • Diagnosis made by clinical exam, through comparing results of AROM, PROM, resistive tests, and palpation. •MRI arthrograms are very effective in identifying labral tears. • The gold standard for identifying a labral tear is through arthroscopic surgery of the shoulder. •Meds: acetaminophen, NSAIDS Goals, Outcomes, Interventions: Return to function without pain, normal strength, endurance, coordination, and flexibility. •Following surgery, the shoulder is usually kept in a sling 3-4 weeks. After 6 weeks, more sports specific training can be done. 4. Thoracic Outlet Syndrome (TOS): •Compression of neurovascular bundle (brachial plexus, subclavian artery and vein, vagus and phrenic nerves, and the sympathetic trunk) in thoracic outlet between bony and soft tissue structures. •Compression occurs when size or shape of thoracic outlet is altered. •Common areas of compression: Superior thoracic outlet, Scalene triangle, between clavicle and first rib, between pectoralis minor and thoracic wall. •Surgery may be performed to remove a cervical rib or a release of anterior and/or middle scalene muscle. •Diagnostic tests utilized: plain film imaging to identify abnormal bony anatomy and MRI to identify abnormal soft tissue anatomy. Electro diagnostic test to assess nerve dysfunction. •Clinical exam of special tests will be helpful to make diagnosis: Adson’s, Roos test, Wright test, Costoclavicular test. •Medications: acetaminophen, NSAIDS Goals, Outcomes, Interventions: Postural reeducation, functional training of muscle imbalance, flexibility. Joint mobs, Manipulations (1st rib articulation) 5. Acromioclavicular and sternoclavicular joint disorders: •Mechanism of injury is a fall onto shoulder, with UE adducted, or a collision with another individual during a sporting event. •Traditionally, degree of injury is grated from first to third degree. Rockwood classification scales uses grades from I to IV, with grades IV-VI as variations of the traditional grade III. •UE is positioned in neutral with use of sling in acute phase. AVOID shoulder elevation during the acute phase of healing. •Diagnostic tests: plain film imaging •Special test useful in making diagnosis: Shear test •Surgical repair is rare, due to tendency of acromioclaviculr joint degeneration following the repair. •Meds: acetaminophen, NSAIDS Goals, Outcomes, Interventions: Return of function without pain. Functional training and restoration of muscle imbalances using exercise to normalize strength, endurance, coordination, and flexibility. •Manual therapy techniques to AC and SC joints such as soft tissue/massage, joint oscillations, and mobilizations to normalize soft tissue and joint biomechanics. *Arthrokinematics for Sternoclavicular joint: (Protraction=same direction)( Elevation=opposite) Motion to Increase Mobilization Glide SC elevation Inferior glide SC protraction Anterior glide 6. Subacromial/subdeltoid bursitis: •Subacromial and subdeltoid bursae (which may be continuous) have a close relationship to rotator cuff tendons, making them susceptible to overuse. •Palpable by extending the humerus. •The bursa is located over the bicipital groove under the deltoid muscle, separating this muscle from the rotator cuff and allowing for free motion of the deltoid over the humerus. •They can also become impinged beneath the acromial arch. •Diagnosis made by clinical exam. Differentiate from contractile condition by comparing results of AROM, PROM, and resistive tests 7. Rotator cuff tendonosis/tendonopathy: •Tendons of the rotator cuff are susceptible to tendonitis, due to relatively poor blood supply near insertion of muscles. •Results from mechanical impingement of the distal attachment of the rotator cuff on the anterior acromion and/or coracoacromial ligament with repetitive overhead activities. •Diagnostic tests utilized: MRI may be used, but sometimes not sensitive enough for accurate assessment. •Clinical exam include the following special tests: Supraspinatus test, Neer’s impingment test 8. Impingement syndrome: •Characterized by soft tissue inflammation of the shoulder from impingement against the acromion with repetitive overhead AROM. •Diagnostic tests utilized: arthrogram or MRI •Clinical exam will include the following: Neer’s, Supraspinatus test, Drop arm test •Surgical repair of shoulder impingement. The pt should avoid shoulder elevation greater than 90°. Goals, Outcomes, Interventions: Restoration of posture, correction of muscle imbalance 9. Bicipital tendonosis/tendonopathy: •Most commonly an inflammation of the long head of the biceps. •Results from mechanical impingement of the proximal tendon, between the anterior acromion and the bicipital groove of the humerus. •Diagnostic tests utilized: MRI may be used, but sometimes not sensitive enough. •Clinical exam will include Speed’s test. •Meds: acetaminophen and NSAIDS 10. Proximal humeral fractures: •Humeral neck fractures frequently occur with a fall onto an outstretched UE among older osteoporotic women. Generally does not require immobilization or surgical repair, since it is a fairly stable fx. •Greater tuberosity fractures are more common in middle-aged and elder adults. Usually related to a fall onto the shoulder, and does not require immobilization for healing. •Diagnostic tests utilized: plain film radiographs. •Early PROM is important in preventing capsular adhesions. 11. Adhesive Capsulitis (frozen shoulder): •Characterized by a restriction in shoulder motion as a result of inflammation and fibrosis of the shoulder capsule, usually due to disuse following injury or repetitive microtrauma. •Restriction follows a capsular pattern of limitation: Greatest limitation in ER, followed by abduction, and flexion, and least restricted in IR. •Commonly seen in association with diabetes mellitus. Elbow: Supination: (Supinator, biceps) C5-C6 Pronation: (Pronator quadrauts, pronator teres, flexor carpi radialis) C8-T1, C6,C7 Extension of wrist: (ECRL, ECRB, ECU) C6-C7, C7-C8 Flexion of wrist: (FCR, FCU) C6-C7, C7-C8 UD of wrist: (FCU, ECU) C7-C8, C7-C8 RD of wrist: (FCR, ECRL, abd pollicis longus, ext pollicis brevis) C6-C7, C7-C8 Ext of fingers: (Extensor digitorum communis, ext indicis, extensor digiti minimi) C7-C8 Flexion of fingers: (flex digit profundus, superficialis, lumbricals, interossei, flexor digit minimi): C8-T1 Abduction of fingers: (Doral interossei, abductor digiti minimi) C8-T1 Adduciton of fingers: (palmar interossei) C8, T1 Ulnar nerve (C8-T1) *Largest branch of the medial cord of the brachial plexus. Entrapment site: cubital tunnel and Guyon’s canal. Intervention: splint wrist in neutral position at night, elbow pad. Education-positioning in elbow ext and decreasing direct pressure on nerve; stretch flexor carpi ulnaris Median nerve (C5-T1) *AIN branches off median nerve and supplies motor innervation to the index and middle flexor digitorum profundus, the flexor pollicis longus, and the pronator quadrates. Entrapment site: carpal tunnel, proximal forearm. Intervention: splint wrist in neutral position at night, stretching exercises for pronator teres, rest periods in supination. Radial nerve (C5-T1) Entrapment site: arcade of froshe, forearm. Intervention: positioning in supination and avoid repetitive pronation and supination activities. ROM: Flexion: 5° hyperextension to 145° flexion Extension: 0° to 5-10° hyperextension Arthrokinematics: Joint Ulnohumeral (same) Proximal radioulnar (opposite) Distal radioulnar (same) Motion to Increase Elbow flexion Elbow extension Pronation Supination Pronation Supination Mobilization Glide Anterior Posterior Posterior (lateral) Anterior (medial) Anterior (medial) Posterior (lateral) Force couples: •The triceps/biceps during elbow extension and flexion •pronator teres and pronator quadratus/supinator during forearm pronation and supination •FCR, FCU, flexor digitorum communis/ERCL, ECRB, and extensor communis during wrist flexion and extension •triceps/biceps and brachioradialis; pronator teres/supinator/ and FCR, FCU/ECRB, and ECRL during activities requiring elbow stabilization Closed-pack position: Humeroulnar-full extension and maximum forearm supination; open-packed position: 70° of flexion with 10° supination Capsular pattern: flexion more limited than extension Common MMT for the elbow: 1. Elbow flexion (biceps brachii): Seated, with UE in 0° shoulder add, 0° elbow ext, forearm supination. Apply resistance just proximal to wrist in direction of elbow extension. Gravity eliminated: seated w arm supported on table. 2. Elbow flexion (brachialis): Seated, same position except forearm PRONATION. Apply resistance just proximal to wrist in direction of elbow extension. Gravity eliminated: seated with arm supported (hand thumb side down) 3. Elbow flexion (brachioradialis): Seated, same position except NEUTRAL forearm rotation. Gravity eliminated: Seated, with arm supported (palm face down on table) 4. Elbow extension (triceps, anconeus): Supine w UE in 90° shoulder flexion, full elbow flexion, full forearm supination. Flex pts elbow slightly, then apply resistance just proximal to wrist in direction of elbow flexion. Gravity eliminated: Seated w arm supported, shoulder abducted to 90°, elbow full flexed, forearm supinated (pinky on table) 5. Forearm supination (supinator, biceps): Seated w UE in 0° shoulder abd, 90° elbow flexion, full forearm pronation. Apply resistance over volar surface of ulna and dorsal surface of radius in direction of pronation. Gravity eliminated: Seated w UE in 90° shoulder flex, 90° elbow flexion, full forearm pronation 6. Forearm pronation (pronator quadraus, pronator teres): Seated, w UE in 0° shoulder abd, 90° elbow flex, full forearm supination. Apply resistance over volar surface of radius and dorsal surface of ulna in direction of supination. Gravity eliminated: Same except full forearm supination. Special tests for the elbow: Ligamentous Instability 1. Varus stress test: The pt is sitting w the elbow in 20-30° of flexion. Therapist places one hand on the elbow and the other proximal to the pts wrist. The therapist applies a varus force to test the LCL while palpating lateral joint line. A positive test is indicated by increased laxity in the LCL when compared to the contralateral limb, apprehension or pain. A positive test may be indicative of a LCL sprain. 2. Valgus stress test: Same position as varus, except therapist applies a valgus force to test the MCL while palpating the medial joint line. A positive test is indicated by increased laxity in the MCL when compared to the contralateral limb, apprehension or pain. A positive test may be indicative of a MCL sprain. Epicondylitis 1. Cozen’s test: Pt is positioned in sitting w the elbow in slight flexion. Therapist places his/her thumb on the patient’s lateral epicondyle while stabilizing the elbow joint. The pt is asked to make a fist, pronate the forearm, radially deviate, and extend the wrist against resistance. A positive test is indicated by pain in the lateral epicondyle region or muscle weakness and may be indicative of lateral epicondylitis. 2. Lateral epicondylitis test: The pt is positioned in sitting. The therapist stabilizes the elbow w one hand and places the other hand on the dorsal aspect of the pts hand distal to the proximal interphalangeal joint. The pt is asked to extend the third digit against resistance. A positive test is indicated by pain in the lateral epicondlye region or muscle weakness and may be indicative of lateral epicondylitis. 3. Medial epicondylitis test: Pt positioned in sitting. The therapist palpates the medial epicondyle and supinates the pts forearm, extends the wrist, and extends the elbow. A positive text is indicated by pain the medial epicondyle region and may be indicative of medial epicondylitis. 4. Mill’s test: Pt positioned in sitting. The therapist palaptes the lateral epicondyle, pronates the pts forearm, flexes the wrist, and extends the elbow. A positive test is indicated by pain in the lateral epicondyle region and may be indicative of lateral epicondylitis. Neurological Dysfunction 1. Tinel’s sign: Pt positioned in sitting w the elbow in slight flexion. Therapist taps with the index finger between the olecranon process and the medial epicondyle. A positive test is indicated by a tingling sensation in the ulnar nerve distribution of the forearm, hand, and fingers. A positive test may be indicative of ulnar nerve compression or compromise. 2. Pronator teres syndrome test: Pt sitting w elbow in 90° flexion and supported. Therapist resists forearm pronation and elbow extension simultaneously. A positive test reproduces a tingling or parestheisa within the median nerve distribution. A positive test may be indicative of median nerve entrapment within pronator teres. Occurs with repetitive gripping activities. Elbow conditions: (See chart for common MS diagnosis) 1. Distal humeral fractures: •Complications can include loss of motion, myositis ossificans, malalignment, neurovascular compromise, ligament injury, and CRPS. •Supracondylar fxs must be examined quickly for neurovascular status, due to high number of neurological (typically radial nerve involvement) and vascular structures that pass through this region (may lead to Volkmann’s ischemiaI. In youth, it is important to assess growth plate as well. These fxs have a high incidence of malunion. *Volkmann’s Contracture=severe pain in forearm, sensation of pressure if compartment syndrome. Onset is nerve and muscle ischemia, secondary to arterial compromise. Pt has pain w/in 2 hrs increase by passive finger ext, pallor, paresis, pulselessness, pt has wrist ext, and finger flex contractures. •Lateral epicondyle fxs are fairly common in young people, and typically require an open reduction internal fixation (ORIF) to ensure absolute alignment. •Diagnostic tests utilized: plain film Goals, outcomes, Interventions: pain reduction and limiting the inflammatory response following trauma/surgery. Improving flexibility of shortened structures, strengthening, and training to restore functional use of UE. 2. Osteochondrosis of humeral capitellum: •Osteochondritis dissecans affects central and/or lateral aspect of capitellulm or radial head. An osteochondral bone fragment becomes detached from articular surface, forming a loose body in joint. Caused by repetitive compressive forces between radial head and humeral capitellum. Occurs in adolescents between 12 and 15 years of age. 3. Panner’s disease: •Is a localized avascular necrosis of capitellum leading to loss of subchondral bone, with fissuing and softening of articular surfaces of radiocapitellar joint. Etiology is unknown, but occurs in children age 10 or younger. •Diagnostic tests: plain film Goals, outcomes, Interventions: PT includes rest with avoidance of any throwing or upper extremity loading activities (gymnastics) When pt is pain-free, initiate flexibility and strengthening/endurance/coordination ex. During late phases of rehab, a program to slowly increase load on joint it initiated. If symptoms persist, surgical intervention is necessary. After surgery initial focus of rehab is to minimize pain and swelling using modalities. 4. Radial nerve entrapment: •Occurs within radial tunnel as a result of overhead activities and throwing. Clinical signs include lateral elbow pain that can be confused with lateral epicondylitis, pain over supinator muscle, and presthesias in a radial nerve distribution. Tinel’s sign may be positive. •Diagnostic tests utilized: electrodiagnositc tests. Goals, outcomes, and interventions: Early intervention includes rest, avoiding exacerbating activities, use of NSAIDS, modalities and soft tissue massage. If abnormal neurotension is present, neurodynamic mobilization may be indicated. Protective padding and night splints to maintain slackened position of involved nerves. 5. Elbow dislocations: •Posterior dislocations account for most dislocations occurring at the elbow. Posterior dislocations are defined by position of olecranon relative to the humerus. •Posterolateral dislocations are most common, and occur as the result of elbow hyperextension from a fall on the outstretched UE. •Posterior dislocations frequently cause avulsion fxs of medial epicondyle secondary to traction pull of medial collateral ligament. •Anterior and radial head dislocations account for only 1-2% of all elbow dislocations. With a complete dislocation, ulnar collateral ligament will rupture, with possible rupture of anterior capsule, lateral collateral ligament, brachialis muscle, and/or wrist flexor and extensor muscles. •Clinical signs include rapid swelling, severe pain at the elbow, and a deformity with the olecranon pushed posteriorly Goals, outcomes, and interventions: Initial intervention includes reduction of the dislocation. If elbow is stable, there is an initial phase of immobilization, followed by rehab focusing on regaining flexibility within limits of stability and strengthening. *Nurse-maid’s (pulled) Elbow-pain localized to superior radioulnar joint, caused by longitudinal pull on forearm, a partial slippage of the annular ligament over the head of the radius pt will avoid use of arm, arm held in pronation, pt has inability to supinate w/out pain. Special tests: palpate sulcus proximal to radial head. Wrist & Hand *The wrist is positioned in slight extension to allow effective hand function. *Wrist extension of 20°-30° is needed for optimal use of the hand. *The most active muscle in grasping is the extensor carpi radialis brevis, which holds the wirst in extension. Two types of functional grasp: 1. The power grip is used to exert force on an object and maintain it against the palm. This requires finger flexion and wrist extension with ulnar deviation. 2. The precision (prehension) grip is used for accurate functions with the object held between the fingertips. Four stages of gripping: Opening the hand, closing the fingers, exerting force, and releasing the object. The thumb, wrist, hand, and fingers control the gripping actions with varying ranges of precision or power. ROM: Flex-80 Ext-70 RD-20 UD-30 MCP flex-90 DIP hyperextension-10 MCP hyperextension-45 PIP flex-100 DIP flex-90 The wrist joint comprises the distal radius & ulna, 8 carpal bones, and the bases of 5 metacarpals. The carpal bones lie in two transverse rows. The proximal row contains (lateral to medial) scaphoid (navicular), lunate, triquetrum, and pisiform. The distal row holds the trapezium, trapezoid, capitate, and hamate. Arthrokinematics: Joint Radiocarpal (opposite) Mid carpal (same) Metacarpophalangeal (same) Motion to increase Wrist extension Wrist flexion Wrist ulnar deviation Wrist radial deviation Wrist extension Wrist flexion Finger flexion Finger extension Mobilization glide Anterior Posterior Lateral Medial Anterior Posterior Anterior (Ventral) Posterior (Dorsal) Closed pack position: Extension with radial deviation Loose pack position: neutral with slight ulnar deviation Capsular pattern: (wrist)=Flexion and extension equally limted (MCP and IP)=flexion more limited than extension Common MMT for the wrist/hand: 1. Wrist flexion and radial deviation (flexor carpi radialis): Seated w forearm supinated and supported on a flat surface. Pt flexes and deviates wrist to radial side while examiner maintains stabilization of forearm. Apply resistance along volar aspect of bases of first and second metacarpals in direction of wrist ext and ulnar deviation. Gravity eliminated-seated w arm in neutral (halfway between pronation and supination) 2. Wrist flexion and ulnar deviation (flexor carpi ulnaris): Seated w forearm supinated and supported. Pt flexes and deviates wrist to ulnar side while examiner maintains stabilization of forearm. Apply resistance along volar aspect of 5th MC bone in direction of wrist ext. Gravity eliminated-Same as other. 3. Wrist extension and radial deviation (extensor carpi radialos longus and brevis): Seated with forearm pronated and supported on a flat surface. Pt extends and deviates wrist to radial side. Apply resistance along dorsal aspect of 1st and 2nd metacarpals in direction of wrist flexion and ulnar deviation. Gravity eliminated-seated w forearm in neutral rotation, wrist in neutral position, forearm supported. 4. Wrist extension and ulnar deviation (extensor carpi ulnaris): Seated with forearm pronated and supported. Pt extends and deviates wrist to ulnar side. Apply resistance along dorsal aspect of 5th metacarpal in direction of wrist flexion and radial deviation. Gravity eliminated-Seated w forearm in neutral rotation, and supported on surface. 5. Finger flexion(lumbricals, palmar and dorsal interossei): Seated with forearm fully supinated and supported, wrist in neutral, fingers extended. Pt flexes MCP joints while extending IP joints. Apply resistance with one finger along volar surface of proximal phalanx of 2nd-5th digits individually in direction of MCP extension. Gravity eliminated-Seated w forearm in neutral rotation and supported on flat surface. Special tests for the wrist/hand: Ligamentous Instability 1. Ulnar collateral ligament instability test-The pt is positioned in sitting. The therapist holds the pts thumb in extension and applies a valgus forace to the metacarpophalangeal joint of the thumb. A positive test is indicated by excessive valgus movement and may be indicative of a tear of the ulnar collateral and accessory collateral ligaments. This type of injury is referred to as gamekeeper’s or skier’s thumb. Vascular Insufficiency 1. Allen test-Pt is positioned in sitting or standing. Pt is asked to open and close the hand several times in succession and then maintain the hand in a closed position. Therapist compresses the radial and ulnar arteries. Pt is then asked to relax the hand and the therapist releases the pressure on one of the arteries while observing the color of the hand and fingers. A positive test is indicated by delayed or absent flushing of the radial or ulanr half of the hand and may be indicative of an occlusion in the radial or ulnar artery. Contracture/Tightness 1. Bunnel-Littler test-Pt is positioned in sitting with the metacarpophalangeal joint held in slight extension. Therapist attempts to move the PIP joint into flexion. If the PIP joint does not flex with the MCP joint extended, there may be a tight intrinsic muscle or capsular tightness. If the PIP joint fully flexes with the MCP joint in slight flexion, there may be intrinsic muscle tightness without capsular tightness. 2. Tight retinacular ligament test-The PIP joint is held in a neutral position while the therapist attempts to flex the DIP joint. If the therapist is unable to flex the DIP joint, the retinacular ligaments or capsule may be tight. If the therapist is able to flex the DIP joint with the PIP joint in flexion, the retinacular ligaments may be tight and the capsule may be normal. Neurological Dysfunction 1. Froment’s sign-Pt is positioned in sitting or standing and is asked to hold a piece of paper between the thumb and index finger. The therapist attempts to pull the paper away from the pt. A positive test is indicated by the pt flexing the distal phalanx of the thumb due to adductor pollicis muscle paralysis. If at the same time, the pt hyperextends the metacarpophalangeal joint of the thumb, it is termed Jeanne’s sign. Both objective findings may be indicative of ulnar nerve compromise or paralysis. 2. Phalen’s test-Pt is positioned in sitting or standing. Therapist flexes the pts wrists maximally and asks the pt to hold the position for 60 seconds. A positive test is indicated by tingling in the thumb, index finger, middle finger, and lateral half of the ring finger and may be indicative of carpal tunnel syndrome due to median nerve compression. 3. Tinel’s sign-Pt is positioned in sitting or standing. Therapist taps over the volar aspect of the pts wrist. A positive test is indicated by tingling in the thumb, index finger, middle finger, and lateral half of the ring finger distal to the contact site at the wrist. A positive test may be indicative of carpal tunnel syndrome due to median nerve compression. Miscellaneous 1. Finkelstein test-Pt is positioned in sitting or standing and is asked to make a fist with the thumb tucked inside the fingers. Therapist stabilizes pts forearm and ulnarly deviates the wrist. A positive test is indicated by pain over the abductor pollicis longs and extensor pollicis brevis tendons at the wrist and may be indicative of tenosynovitis in the thumb (De Quervain’s disease) 2. Grind test- Pt positioned in sitting or standing. The therapist stabilizes the pts hand and grasps pts thumb on the metacarpal. Therapist applies compression and rotation through the metacarpal. A positive test is indicated by pain and may be indicative of degenerative joint disease in the CMC. 3. Murphy sign-Pt is positioned in sitting or standing and is asked to make a fist. A positive test is indicated by the pts third metacarpal remaining level with the second and fourth metacarpals. A positive test may be indicative of a dislocated lunate. Wrist/hand conditions: (See chart for common MS pathologies) 1. Dupuytren’s Contracture: •Observed as banding on palm and digit flexion contractures, resulting from contracture of palmar fascia that adheres to skin. •Affects men more than women •Contracture usually affects the MCP and PIP joints of 4th and 5th digits in nondiabetic individuals and affects 3rd and 4th digits most often in individuals with diabetes. Goals, outcomes, and Interventions-flexibility ex, splint application, promote restoration of normal hand function 2. Boutonniere deformity: •Results from rupture of central tendinous slip of extensor hood. •Observed deformity is extension of MCP and DIP with flexion of PIP. •Commonly occurs following trauma, or in rheumatoid arthritis with degeneration of the central extensor tendon. 3. Swan neck deformity: •Results from contracture of intrinsic muscles with dorsal subluxation of lateral extensor tendons. •Observed deformity is flexion of MCP and DIP with extension of PIP. •Commonly occurs following trauma, or with RA following degeneration of lateral extensor tendons. 4. Ape hand deformity: •Observed as thenar muscle wasting, with first digit moving dorsally until it is in line with second digit. •Results from median nerve dysfunction. 5. Mallet finger: •Rupture or avulstion of extensor tendon at its insertion into distal phalanx of digit. •Observed deformity is flexion of DIP joint. •Usually occurs from trauma, forcing distal phalanx into a flexed position. 6. Gamekeeper’s thumb: • A sprain/rupture of ulanr collateral ligament of MCP joint of first digit. •Results in medial instability of thumb. •Frequently occurs during a fall wile skiing, when increasing forces are placed on thumb through ski pole. •Immobilized for 6 weeks. 7. Boxer’s fx: •Fx of neck of 5th metacarpal •Frequently sustained during a fight, or from punching a wall in anger •Casted for 2-4 weeks Hip: Flexors: Psoas, Iliacus, Pectineus, Rectus femrois Extensors: Glut max, semitendinosus, semimembranosus, biceps femoris (long head) Abductors: glut med. Assist movers: glut min, TFL, Sartorius, rectus, piriformis (at 90° hip flex) Adductors: Adductor magnus, adductor longus, adductor brevis, gracilis, pectineus ER: Glut max, gemellus inferior & superior, obturator externus & internus, quadratus femoris, piriformis (at less than 60° hip flexion) IR: TFL, glut min Assist movers: semitendinosus, semimembranosus, gracilis, piriformis (at 90° hip flexion) ROM: Flex-110-120° Ext-10-15° Abd-30-40° Add-25-30° ER-40-60° IR-30-40° Arthrokinematics: Joint Hip Motion to increase Abduction ER/extension IR/flexion Mobilization Glide Inferior Anterior Posterior Closed packed position: full ext, medial rotation Loose packed position: 30° flex, 30°abd, slight lateral rotation Capsular pattern: most limited flexion, abduction, and medial rotation (sometimes medial rotation is most limited) End-feels for the hip: Tissue stretch/approximation (flexion and adduction) Common MMT of the hip: 1. Hip flexion (Iliacus and Psoas Major)-Seated with legs off side of treatment table, holding on to table edge with hands. Pt flexes hip through range while keeping knee flexed. Apply resistance over anterior aspect of distal thigh in direction hip ext. Gravity eliminatedSidelying on side of lower extremity to be tested. 2. Hip flex, abd, and external rotation(Sartorius)-Seated with legs off side table, holding on to table. Pt will slide heel of limb being tested up shin of opposite leg. Pt flexes, abducts, and externally rotates hip while flexing knee. Apply resistance. Gravity eliminated-Supine with heel of lower extremity to be tested on ventral surface of contralateral ankle, contralateral lower extremity extended. 3. Hip extension (glut max, semitendinosus, semimembranosus, and biceps femoris)-Prone with lower extremities extended. Apply resistance over posterior aspect of distal thigh in direction of hip flexion. Gravity eliminated-Sidelying on side of lower extremity to be tested. 4. Hip abduction (glut med and min)-Sidelying with limb to be tested uppermost. Apply resistance over lateral aspect of distal thigh in direction of hip adduction. Gravity eliminated-Supine with hips fully adducted. 5. Hip abduction with flexion (tensor fascia lata)-Sidelying with limb to be tested uppermost, hip or upper limb in 45° flexion an neutral rotation, lower limb flexed for balance. Abduct pts hip 30°, maintaining hip in flexion, apply resistance over lateral aspect of distal thigh in direction of hip adduction. Gravity eliminated-Long sitting, hips flexed to 45°, knees extended. Pt supports trunk by learning back on extended arms. 6. Hip adduction (magnus, longus, brevis, pectineus, and gracils)-Sidelying on side of limb to be tested, pt may hold table for support. Pt adducts hip of test limb, apply resistance on medial aspect of distal thigh in direction of hip abduction. Gravity eliminated-Supine with non-test limb in full abduction. 7. Hip medial rotation(TFL, glut min and med)-Seated with legs hanging over table, with towel under knee of limb to be tested. Medially rotate pts hip by moving foot laterally; resistance is applied in medial direction on lateral aspect of distal leg. Gravity eliminated-Supine with limb to be tested in full hip lateral rotation. 8. Hip lateral rotation(piriformis, gemellus superior & inferior, obturator internus & externus, and quadratus)-Seated with legs off table, towel under knee of test limb. Laterally rotate pts hip by moving foot medially. Apply resistance in lateral direction on medial aspect of distal leg. Gravity eliminated-Supine with limb to be tested in full medial rotation. Special tests for the hip: Contracture/Tightness 1. Ely’s test-Pt is prone while the therapist passively flexes the pts knee. A positive test is indicated by spontaneous hip flexion occurring simultaneously with knee flexion and may be indicative of a rectus femoris contracture. 2. Ober’s test-Pt is positioned in side-lying with the lower leg flexed at the hip and knee. The therapist moves the test leg into hip extension and abduction and then attempts to slowly lower the test leg. A positive test is indicated by an inability of the test leg to adduct and touch the table and may be indicative of a tensor fasciae latae contracture. 3. Piriformis test-Pt is positioned in sidelying with the test leg positioned toward the ceiling and the hip flexed to 60°. Therapist places one hand on the pts pelvis and the other hand on the pts knee. While stabilizing the pelvis, the therapist applies a downward (adduction) force on the knee. A positive test is indicated by pain or tightness, and may be indicative of piriformis tightness or compression on the sciatic nerve caused by the piriformis. 4. Thomas test-Pt is positioned in supine with the legs fully extended. The pt is asked to bring one of their knees to the chest in order to flatten the lumbar spine. The therapist observes the position of the contralateral hip while the pt holds the flexed hip. A positive test is indicated by the straight leg rising from the table and may be indicative of a hip flexion contracture. 5. 90-90 straight leg raise test-The pt is positioned in supine and asked to stabilize the hips in 90° of flexion with the knees relaxed. The therapist instructs the pt to alternately extend each knee as much as possible while maintaining the hips in 90° of flexion. A positive test is indicated by the knee remaining in 20° or more of flexion and is indicative of hamstrings tightness. Pediatric Tests 1. Barlow’s test-The pt is positioned in supine the hips flexed to 90° and knees flexed. The therapist tests each hip individually by stabilizing the femur and pelvis with one hand while the other hand moves the test leg into abduction while applying forward pressure posterior to the greater trochanter. A positive test is indicated by a click or clunk and may be indicative of a hip dislocation being reduced. The test is considered to be a variation of Ortolani’s test. 2. Ortolani’s test-The pt is positioned in supine with the hips flexed to 90° and knees flexed. The therapist grasps the legs so that their thumbs are placed along the pts medial thighs and the fingers are placed on the lateral thighs toward the buttocks. The therapist abducts the pts hips and gentle pressure is applied to the greater trochanters until resistance is felt at approx 30°. A positive test is indicated by a click or a clunk and may be indicative of a dislocation being reduced. Miscellaneous 1. Craig’s test-Pt is positioned in prone with the test knee flexed to 90°. The therapist palpates the posterior aspect of the greater trochanter and medially and laterally rotates the hip until the greater trochanter is parallel with the table. The degree of femoral anteversion corresponds to the angle formed by the lower leg with the perpendicular axis of the table. Normal anteversion for an adult is 8-15°. 2. Patrick’s test (FABER test)-The pt is positioned in supine with the test leg flexed, abducted, and externally rotated at the hip onto the opposite leg. The therapist slowly lowers the test leg through abduction toward the table. A positive test is indicated by failure of the test leg to abduct below the level of the opposite leg and may be indicative of iliopsoas, sacroiliac or hip joint abnormalities. 3. Quadrant scouring test-The pt is positioned in supine. The therapist passively flexes and adducts the hip with the knee in maximal flexion. The therapist applies a compressive force through the shaft of the femur while continuting to passively more the pts hip. A posistive test is indicated by grinding, catching or crepitation in the hip and may be indicative of pathologies such as arthritis, avascular necrosis or an osteochondral defect. 4. Trendelenburg test-Pt is positioned in standing and is asked to stand on one leg for approx 10 seconds. A positive test is indicated by a drop of the pelvis on the unsupported side and may be indicative of weakness of the gluteus medius muscle on the supported side. Conditions of the hip (see MS chart): 1. Avascular necrosis (AVN) •Multiple etiologies resulting in an impaired blood supply to the femoral head. •Hip ROM is decreased in flexion, IR, and abduction •Diagnositc tests utilized: plain film imaging, bone scans, CT, and MRI •Symptoms include pain in the groin and/or thigh, and tenderness with palpation at the hip joint •Coxalgic gait •Corticosteriods contraindicated since they may be causative factor Goals, outcomes, interventions-Joint/bone protection strategies, maintain joint mechanics and connective tissue functions. Implementation of aerobic capacity/endurance conditioning, such as aquatics. Post surgical intervention includes regaining functional flexibility, improving strength, and gait training. 2. Piriformis Syndrome •Piriformis muscle is an external rotator of the hip and can become overworked with excessive pronation of the foot, causing abnormal femoral internal rotation. •Considered a tonic muscle that is active with motion of sacroiliac joint, particularly sacrum •Tightness or spasm of the piriformis muscle can result in compression of sciatic nerve and/or sacroiliac dysfunction. •Diagnostic tests utilized: possibly electrodiagnostic tests for sciatic nerve •Signs & symptoms include: restriction in internal rotation, pain with palpation of piriformis muscle, referral of pain to the posterior thigh, weakness in external rotation, positive piriformis test, uneven sacral base •Perform lower extremity biomechanical examination to determine if abnormal biomechanics are the cause. Must rule out involvement of lumbar spine and or SI joint. •NSAIDS and neurontin Goals, outcomes, interventions-Reduction of pain using modalities and manual therapy techniques, such as soft tissue massage to piriformis, joint oscillations to hip or pelvis to inhibit pain, correction of muscle imbalances and biomechanical faults using strengthening. Restore muscle balance and pt education regarding protection of the SI joint (instruction not to step off a curb onto the dysfunctional LE) Knee “Screw home mechanism”-describes the 5° of tibial external rotation, which occurs during terminal knee extension. Occurs as closed-chain internal femoral rotation during weight bearing to provide increased stability of knee joint during weight-bearing activities. Can also occur as open-chain external tibial rotation. Unlocking occurs through action of popliteus. Open-chain unlocking occurs primarily with popliteal action. Internal rotation of femur is the same as external rotation of tibia. ROM: Flex-135° Closed pack position-full extension, lateral rotation of tibia Loose-pack position-25° flex Capsular pattern: flexion more limited than extension Arthrokinematics: Joint Tibiofemoral (knee) Patellofemoral Motion to increase Knee extension Knee flexion Knee extension Knee flexion Mobilization glide Anterior/medial/lateral Posterior Superior Inferior Common MMT of the knee: 1. Knee extension (quadriceps femoris)-Seated with legs off side of table and towel under knee of test limb. Pt extends knee through full range, apply resistance over anterior aspect of distal leg in direction of knee flexion. Gravity eliminated-Side lying on side to be tested, knee fully flexed. 2. Knee flexion(biceps femoris, semitendinosus, and semimembranosus)-Prone with lower extremities extended. Flex pts knee to 90°, rotating knee laterally. Apply resistance over posterior aspect of distal leg in direction of knee extension.(Biceps femoris) Prone with lower extremities extended, flex pts knee to 90°, rotating knee medially (semitendinous and semimembranosus) Gravity eliminatedSidelying on side to be tested. Special tests for the knee: Ligamentous Instability 1. Anterior drawer test-Pt is positioned in supine with the knee flexed to 90° and the hip flexed to 45°. The therapist stabilizes the lower leg by sitting on the forefoot. The therapist grasps the pts proximal tibia with two hands, places their thumbs on the tibial plateau, and administers an anterior directed force to the tibia on the femur. A positive test is indicated by excessive anterior translation of the tibia on the femur with a diminished or absent end-point and may be indicative of an anterior cruciate ligament injury. 2. Lachman test-Pt is positioned in supine with the knee flexed to 20-30°. The therapist stabilizes the distal femur with one hand and places the other hand on the proximal tibia. The therapist applies an anterior directed force to the tibia on the femur. A positive test is indicated by excessive anterior translation of the tibia on the femur with a diminished or absent end-point and may be indicative of an ACL injury. 3. Lateral pivot shift test-Pt is positioned in supine with the hip flexed and abducted to 30° with slight medial rotation. The therapist grasps the leg with one hand and places the other hand over the lateral surface of the proximal tibia. The therapist medially rotates the tibia and applies a valgus force to the knee while the knee is slowly flexed. A positive test is indicated by a palpable shift or clunk occurring between 20 and 40° of flexion and is indicative of anterolateral rotator instability. The shift or clunk results from the reduction of the tibia on the femur. 4. Posterior drawer test-Pt is positioned in supine with the knee flexed to 90° and the hip flexed to 45°. The therapist stabilizes the lower leg by sitting on the forefoot. The therapist grasps the pts proximal tibia with two hands, places their thumbs on the tibial plateau, and administeres a posterior directed force to the tibia on the femur. A positive test is indicated by excessive posterior translation of the tibia on the femur with a diminished or absent end-point and may be indicative of a PCL injury. 5. Posterior sag sign-Pt is positioned in supine with the knee flexed to 90° and the hip flexed to 45°. A positive test is indicated by the tibia sagging back on the femur and may be indicative of a PCL injury. 6. Slocum test-Pt is positioned in supine with the knee flexed to 90° and the hip flexed to 45°. Therapist rotates the pts foot 30° medially to test anterolateral instability. The therapist stabilzes the lower leg by sitting on the forefoot. Therapist grasps the pts proximal tibia with two hands, places their thumbs on the tibial plateau, and administers an anterior directed force to the tibia on the femur. A positive test is indicated by movement of the tibia occurring primarily on the lateral side and may be indicative of anterolateral instability. The test can also be performed to assess anteromedial instability by rotating the pts foot 15° laterally. 7. Valgus stress test-Pt is positioned in supine with the knee flexed to 20-30°. The therapist positions one hand on the medial surface of the pts ankle and the other hand on the lateral surface of the knee. The therapist applies a valgus force to the knee with the distal hand. A positive test is indicated by excessive movement and may be indicative of a MCL sprain. A positive test with the knee in full extension may be indicative of damage to the MCL, PCL, posterior oblique ligament, and posteromedial capsule. 8. Varus stress test-Pt is positioned in supine the knee flexed to 20-30°. The therapist positions one hand on the lateral surface of the pts ankle and the other hand on the medial surface of the knee. The therapist applies a varus force to the knee with the distal hand. A positive test is indicated by excessive varus movement and may be indicative of a LCL sprain. A positive test with the knee in full extension may be indicative of damage to the LCL, PCL, arcuate complex, and posterolateral capsule. Meniscal Pathology 1. Apley’s compression test-The pt is positioned in prone with the knee flexed to 90°. The therapist stabilzes the pts femur using one hand and places the other hand on the pts heel. The therapist medially and laterally rotates the tibia while applying a compressive force through the tibia. A positive test is indicated by pain or clicking and may be indicative of a meniscal lesion. 2. Bounce home test-The pt is positioned in supine. The therapist grasps the pts heel and maximally flexes the knee. The pts knee is extended passively. A positive test is indicated by imcomplete extension or a rubbery end-feel and may be indicative of meniscal lesion. 3. McMurray test-The pt is positioned in supine. The therapist grasps the distal leg with one hand and palpates the knee joint with the other. With the knee fully flexed, the therapist medially rotates the tibia and extends the knee. The therapist repeates the same procedure while laterally rotating the tibia. A positive test is indicated by a click or pronounced crepitation felt over the joint line and may be indicative of a posterior meniscal lesion. Swelling 1. Brush test-Pt is positioned in supine. The therapist places one hand below the joint line on the medial surface of the patella and strokes proximally with the palm and fingers and far as the suprapatellar pouch. The other hand then strokes down the lateral surface of the patella. A positive test is indicated by a wave of fluid just below the medial distal border of the patella and is indicative of effusion in the knee. 2. Patellar tap test-Pt is positioned in supine with knee flexed or extended to a point of discomfort. The therapist applies a slight tap over the patella. A positive test is indicated if the patella appears to be floating and may be indicative of joint effusion. Miscellaneous 1. Clarke’s sign-The pt is positioned in supine with the knees extended. The therapist applies slight pressure distally with web space of their hand over the superior pole of the patella. The therapist then asks the pt to contract the quads muscle while maintaining pressure on the patella. A positive test is indicated by failure to complete the contraction without pain and may be indicative of patellofemoral dysfunction. 2. Hughston’s plica test-The pt is positioned in supine. The therapist flexes the knee and medially rotates the tibia with one hand while the other hand attempts to move the patella medially and palpate the medial femoral condyle. A positive test is indicated by a popping sound over the medial plica while the knee is passively flexed and extended. 3. Noble compression test-Pt positioned in supine with the hip slightly flexed and the knee in 90° of flexion. The therapist places the thumb of one hand over the lateral epicondyle of the femur and the other hand around the pts ankle. The therapist maintains pressure over the lateral epicondyle while the pt is asked to slowly extend the knee. A positive test is indicated by pain over the lateral femoral epicondlye at approximately 30° of knee flexion and may be indicative of iliotibial band friction syndrome. 4. Patellar apprehension test-The pt is positioned in supine with the knees extended. The therapist places both thumbs on the medial border of the patella and applies a laterally directed force. A positive test is indicated by a look of apprehension or an attempt to contract the quads, in an effort to avoid subluxation and may be indicative of patella subluxation or dislocation. Knee conditions (see MS chart) 1. Classification of ligament injuries: Tissue Healing: Acute Inflammatory Phase (2-3 days) Proliferative/Repair Phase (Day 3-Week 8) Remodeling Phase (Week 6-Month 12) Grades of sprain: Grade I-Mild stretch, no macroscopic tear, no functional instabililty; Healing time: 1-2 weeks Grade II-Moderate stretch, partial tear, some functional instabililty; Healing time: 2-3 weeks Grade III-Severe, complete tear/rupture; Healing time: 3-6 weeks (requires external bracing) Repairs: (Depending on the choice of graft, these healing times will follow these general guidelines) •0-2 weeks-Maximum protection phase -Focus on muscular control/proprioception -Inflammatory/proliferative phase •2-6 weeks-Moderate protection phase -Restore normal gait, ROM -Protect graft -Proliferatieve phase •6-12 weeks-Gradually-less-protection phase -Improve confidence -Progress strength, power, and proprioception -Maturation phase •12-24 weeks-Graded return to sport phase -Return to former levels of function in a graded fashion -Continue strength/flexibility/power -Maturation p hase •24 weeks-Return to sport 2. Tendon Healing: Inflammatory phase-3-7 days Proliferative phase-day 5-week 5 Remodeling phase-week 6-month 6 Tendonitis/overuse injuries: -Remove offending activity -Follow tissue healing guidelines ●Days 1-7 •PROM, AAROM (if tolerated), no loading •Modalities (“stop the bleeding”) ●Days 7-Week 5 •Progressive addition of load from PROM to AAROM to AROM as tolerated •Avoid adhesions between tendon and paratenon •Provide cardiovascular perfusion to area (train well-leg/arm, increase heart rate and perfusion) ●Weeks 6-Month 6 •Progressively load tendon from AROM to resisted ROM •This can include isometric, isotonic, isokinetic, and eccentric work •GRADUAL and progressive loading as tolerated 3. Genu varum & valgum •Normal tibiofemoral shaft angle is 6° of valgum •Genu varum is an excessive medial tibial torsion, commonly referred to as “bowlegs” •Genu varum results in excessive medial patellar positioning and the pigeon-toed orientation of the feet •Genu valgum is an excessive lateral tibial torsion commonly referred to as “knock knees” •Genu valgum results in excessive lateral patellar positioning 4. Anterior compartment syndrome •Increased compartmental pressure resulting in a local ischemic condition •Multiple etiologies: direct trauma, fracture overuse, and/or muscle hypertrophy •Symptoms of chronic or exertional compartment syndrome are produced by exercise or exertion and descriped as a deep, cramping, feeling •Symptomes of acute ACS are produced by sudden trauma causing swelling within the compartment •Diagnosis made by clinical exam •Acute ACS is considered a medical emergency and requires immediate surgical intervention with fasciotomy. 5. Anterior tibial periostitis (shin splints) •Musculotendinous overuse condition •Three common etiologies: 1. Abnormal biomechanical alignment 2. Poor conditioning 3. Improper training methods •Muscles involved include anterior tibialis and extensor hallucis longus •Pain elicited with palpation of lateral tibia and anterior compartment Goals, outcomes, interventions: correction of muscle imbalances and biomechanical faults using strengthening, endurance, and coordination exercises. Flexibililty exercises for anterior compartment muscles, as well as the tricpes surae, to gain restoration of normal function Ankle/foot -The talocrural joint is formed between the talus and the distal tibia. -The posterior talofibular ligament (PTFL) is the strongest of the lateral ligament complex. It is rarely injured except in severe ankle sprains. -The strength of the ankle ligaments from weakest to strongest is the ATFL, PTFL, CFL, and deltoid complex. -The fibular (peroneal) muscles serve as both plantar flexors and evertors of the foot. The peroneus longus also abducts the forefoot in the transverse plane, thereby serving as a support for the medial longitudinal arch. ROM (ankle): DF-0-20 PF-0-50 INV-0-35 EVR-0-15 ROM (subtalar): INV-0-5 EVR-0-5 Closed pack position (talocrural): maximum DF Loose pack position: 10° PF, midway between maximum inversion and eversion Capsular pattern: Plantar flexion more limited than dorsiflexion Closed packed position of (Subtalar, Midtarsal, and tarsometatarsal): Supination Loose packed position: midway between extremes of range of movement Capsular pattern of subtalar: limitation of varus range of movement Capsular pattern of midtarsal: DF, PF, ADD, MR Closed packed position of metatarsophalangel and interphalangeal: full extension Loose packed position: Neutral(MTP); slight flexion (IP) Arthrokinematics: Joint Talocrural Subtalar Motion to Increase Plantarflexion Dorsiflexion Inversion Eversion Mobilization Glide Anterior Posterior Lateral Medial Common MMT of the Ankle/foot: 1. Ankle plantarflexion: Weight-bearing test (Gastrocnemius and Soleus)-Standing on one leg (test limb), knee extended, foot flat on floor. Pt rises on toes of weight bearing leg through range of plantar flexion, keeping knee extended. Pt repeats motion until fatigued or stopped by examiner. (Soleus)-pt is standing on one limb, knee flexed, foot flat on floor. Pt demonstrates movement of rising on toes with knee flexed. Gravity eliminated-side-lying on side to be tested. 2. Ankle plantarflexion: Non-weight bearing test (Gastroc & Soleus)-Prone with knee extended, foot off end of table, ankle neutral. Pt plantarflexes ankle through ROM, apply resistance on superoposterior aspect of calcaneus in direction of ankle DF. Soleus-prone with knee flexed to 90°, ankle neutral. 3. Ankle dorsiflexion and subtalar inversion-Seated with legs off table, ankle neutral. Dorsiflex and invert pts ankle through ROM, apply resistance over dorsal surface of medial side of foot in direction of PF and eversion. Gravity eliminated-Supine with LE’s extended, ankle of test limb in neutral, foot extended beyond edge of table. Special tests of the ankle/foot: Ligamentous Instability 1. Anterior Drawer test-Pt is positioned in supine. The therapist stabilizes the distal tibia and fibula with one hand, while the other hand holds the foot in 20° of plantar flexion and draws the talus forward in the ankle mortise. A positive test is indicated by excessive anterior translation of the talus away from the ankle mortise and may be indicative of an anterior talofibular ligament (ATFL) sprain. 2. Talar tilt-Pt is positioned in sidelying with knee flexed to 90°. The therapist stabilizes the distal tibia with one hand while grasping the talus with the other hand. The foot is maintained in a neutral position. The therapist tilts the talus into abduction and adduction. A positive test is indicated by excessive adduction and may be indicative of a calcaneofibular ligament sprain. Miscellaneous 1. Thompson test-Pt is positioned in prone with the feet extended over the edge of a table. The therapist asks the pt to relax and proceeds to squeeze the muscle belly of the gastrocnemius and soleus muscles. A positive test is indicated by the absence of plantar flexion and may be indicative of a ruptured Achilles tendon. 2. Tibial torsion test-Pt is positioned in sitting with the knees over the edge of a table. The therapist places the thumb and index finger of one hand over the medial and lateral malleolus. The therapist then measures the acute angle formed by the axes of the knee and ankle. Normal lateral rotation of the tibia is considered to be 12-18° in an adult. 3. True leg length discrepancy test-Pt is positioned in supine with the hips and knees extended, the legs 15-20 cm apart, and the pelvis in balance with the legs. Using a tape measure, the therapist measures from the distal point of the ASIS to the distal point of the medial malleoli. A positive test is indicated by a bilateral variation of greater than 1 cm and may be indicative of a true leg length discrepancy. Conditions of the Foot/ankle (see MS chart): 1. Ligament sprains: •95% of all ankle sprains involve lateral ligaments •With lateral sprains, foot is plantar flexed and inverted at time of injury 2. 3. 4. 5. 6. 7. •Diagnostic test utilized: MRI Tarsal tunnel syndrome: •Entrapment of the posterior tibial nerve or one of its branches within the tarsal tunnel •Over/excessive pronation, overuse problems resulting in tendonitis of the long flexor and posterior tibialis tendon, and trauma may compromise space in the tarsal tunnel •Symptoms include pain, numbness, and paresthesias along the medial ankle to the plantar surface of the foot •Diagnostic tests utilized: electrodiagnostic tests •Positive Tinel’s sign at the tarsal tunnel Goals, Outcomes, interventions: Use of orthoses to maintain neutral alignment, neurodynamic mobilization may be indicated Charcot-Marie-Tooth Disease: •Peroneal muscular atrophy that affects motor and sensory nerves •May begin in childhood or adulthood •Initially affects muscles in lower leg and foot, but eventually progresses to muscles of hands and forearm •Slowly progressive disorder with varying degrees of involvement, depending on degree of genetic dominance. •No specific treatment to prevent, since it is an inherited disorder. Rearfoot varus (subtalar varus, calcaneal varus): •Etiology-abnormal mechanical alignment of tibia, shortened rearfoot soft tissues, or malunion of calcanus. •Deformity observed: rigid inversion of calcaneus when subtalar joint is in neutral position Rearfoot valus: •abnormal alignment of the knee (genu valgum) or tibial valgus •Deformity observed: eversion of calcaneus with a neutral subtalar joint Forefoot varus: inversion of forefoot Forefoot valgus: eversion of forefoot Cervical Spine ROM: Flex-45 Ext-45 Lateral flex-45 Rotation-60 Capsular pattern: Full flexion most limited followed by limited extension, and symmetric limitation of rotation and sidebending. *Limitation of or pain on cervical rotation usually suggests pathology at the C1-C2 (atlantoaxial) segment, because most rotation occurs here. Special tests of cervical region: 1. Foraminal compression test (Spurling’s)-Pt is positioned in sitting with the head laterally flexed. The therapist places both hands on top of the subject’s head and exerts a downward force. A positive test is indicated by pain radiating into the arm toward the flexed side and may be indicative of nerve root compression. 2. Vertebral artery test-Pt is positioned in supine. The therapist places the pts head into extension, lateral flexion, and rotation to the ipsilateral side. A positive test is indicated by dizziness, nystagmus, slurred speech or loss of consciousness and may be indicative of compression of the vertebral artery. **Performing mobilization/manipulation within cervical region w/out performing this test beforehand would be considered a breach in standard care. 3. Hautant’s test-Differentiates vascular versus vestibular causes of dizziness/vertigo. Two steps to this test: 1. Pt sitting with shoulders at 90° and palms up. Have pt close eyes and remain in this position for 30 seconds. If arms lose their position, there may be a vestibular condition. 2. Pt sitting with shoulders at 90° and palms up. Have pt close eyes, and cue pt into head and neck ext with rotation right, then left, remaining in each position for 30 seconds. If arms lose their position, the condition may be vascular in nature. 4.Transverse Ligament stress test (sharp-purser)-Tests integrity of transverse ligament. Pt supine, with head supported on table. Glide C1 anterior. Should be firm end-feel. Positive findings: soft end-feel, dizziness, nystagums, lump sensation in throat, nausea. 5. Lhermitte’s sign-Identifies dysfunction of spinal cord and/or an upper motor neuron lesion. Pt in long sitting on table. Passively flex pts head and one hip, while keeping knee in extension. Repeat with other hip. Positive finding is pain down the spine and into the upper or lower limbs. 6. Romberg test-Identifies upper motor neuron lesion. Pt standing, and closes eyes for 30 seconds. Excessive swaying during test indicates positive finding. Conditions of the cervical spine: 1. “Whiplash” acceleration/deceleration injury-occurs when excess shear and tensile forces are exerted on cervical structures. Structures injured may include facets/articular processes, facet joint capsules, ligaments, disc, anterior/posterior muscles, fracture to odontoid process and spinous processes, TMJ, sympathetic chain ganglia, spinal and cranial nerves. Signs and symptoms-early include headaches, neck pain, limited flexibility, reversal of lower cervical lordosis and decrease in upper cervical kyphosis, vertigo, change in vision and hearing, irritability to noise and light, dysesthesias of face and bilateral upper UEs, nausea, difficulty swallowing, and emotional lability. Late include chronic head and neck pain, limitation in flexibility, TMJ dysfunction, limited tolerance to ADLs, disequilibrium, anxiety, and depression. Common clinical findings include postural changes, excessive muscle guarding with soft tissue fibrosis, segmental hypermobility, and gradual development of restricted segmental motion, crainial and caudal to the injury. Medications: NSAIDS, muscle relaxants, trigger point injections, corticosteroid injection or by mouth Goals, outcomes, interventions: Spinal manipulation, correction of muscle imbalance, joint mobs, pt education on elimination of harmful positions, postural education. Manual or mechanical traction: cervical spine positioned at 15° of flexion to provide optium intervertebral foraminal opening. Contraindications: joint hypermobility, pregnancy, RA. Down syndrome, or any other systemic disease that affects ligamentous integrity. Thoracic and Lumbar Spine ROM: Flex-80 Ext-25 Lateral flex-35 Rotation-45 Capsular pattern for both: lateral flexion and rotation equally limited, extension Lumbar special tests: 1. Stork standing test-Identifies sponlylolisthesis. Pt standing on one leg, cue pt into trunk extension. Repeat with opposite leg on ground. Positive finding is pain in low back with ipsilateral leg on ground. 2. McKenzie’s slide glide test-Differentiates between scoliotic curvature versus neurological dysfunction causing abnormal curvature (lateral shift) of trunk. Test is performed if “lateral shift” of trunk is noted. Pt standing, stand on one side of pt so that upper trunk is shifted toward you. Place your shoulders into pts upper trunk and wrap your arms around pts pelvis. Stabilize upper trunk and pull pelvis, to bring pelvis and trunk into proper alignment. Positive test is reproduction of neurological symptoms as alignment of trunk is corrected. 3. Bicyle (van Gelderen’s test)-Differentiates between intermittent claudication and spinal stenosis. Pt seated on stationary bike. Pt rides bike while witting erect. Time how long they can ride at a set pace/speed. After a sufficient rest period, have pt ride bike at same speed while in a slumped position. Determination is based on length of time pt can ride bike in sitting upright vs sitting slumped. If pain is related to spinal stenosis, pt should be able to ride bike longer while slumped. 4. Standing flexion test-Tests the iliosacral motion and determines if there is a joint dysfunction and the side of involvement. The clinician palpates both the PSISs and asks the pt to bend forward. The PSIS that either moves cranially first or farthest is considered the blocked or positive side. Spinal conditions: 1. Spondyloysis/spondyloisthesis: Thought to congenitallyl defective pars interarticularis. Spondylolysis is a fracture of the pars interarticularis with positive “Scotty dog” sign on oblique radiographic view of spine. Spondylolisthesis is the actual anterior or posterior slippage of one vertebra on another, following bilateral fracture of pars interarticularis. It can be graded according to amount of slippage from 1 (25% slippage) to 4 (100% slippage). Diagnostic tests utilized: plain film (oblique to see fracture and lateral views to see slippage) Clinical exam including stork test, helps identify this condition. Goals, outcomes, and interventions: Dynamic stabilization of trunk, with particular emphasis on abdominals. AVOID EXTENSION and/or other positions that add stress to the defect (extension, ipsilateral side-bending, and contralateral rotation). Braces such as Boston brace and TLSO. Spinal manipulation may be contraindicated for this condition, particularly at the level of defect. 2. Spinal or intervertebral stenosis-Congenital narrow spinal canal or intervertebral foramen, coupled with hypertrophy of the spinal lamina and ligamentum flavum or facets, as the result of age-related degenerative processes or disease. Results in vascular and/or neural compromise. Signs and symptoms: Bilateral pain and paresthesia in back, buttocks, thighs, calves, and feet. Pain decreases in spinal flexion, increases in extension. Pain increases with walking. Pain relieved with prolonged rest. Diagnostic tests utilized: plain films, MRI, and/or CT scan Clinical exam including bicycle. Goals, outcomes, and interventions: Perform flexion-based exercise, and exercises that promotes dynamic stability throughout the trunk and pelvis. Avoid extension and/or other positions that narrow the spinal canal (ipsilateral sidebending or rotation) 3. Disc Conditions-Internal disc disruption: Internal structure of disc annulus is disrupted; however, external structures remain normal. Most common in lumbar region. Symptoms include constant deep, achy pain, and increased pain with movement. No objective neurological findings, although pt may have referred pain in LE. Regular CT or myelogram will not demonstrate any abnormal findings. Can be diagnosed by CT discogram or an MRI. Goals, outcomes, interventions: Spinal manipulation may be contraindicated for this condition. Limit repetitive bending and twisting movements, limiting UE overhead and sitting activities, and carrying heavy loads. Posterolateral bulge/herniation-Most commonly observed disc disorder of lumbar spine due to three structural deficiencies: Posterior disc is narrower in height than anterior disc, Posterior longitudinal ligament is not as strong and only centrally located in lumbar spine, posterior lamellae of annulus are thinner. Etiology-overstretching and/or tearing of annular rings, vertebral endplate and /or ligament structures, from high compressive forces or repetitive microtrauma. Results in loss of strength, radicular pian, paresthesia and inability to perform ADLS. Goals, outcomes, interventions-exercise program to promote dynamic stability throughout trunk and pelvis and to provide optimal stimulus for regeneration of disc. Positional gapping for 10 minutes to increase space within region of space occupying lesion. If left posterolateral lumbar herniation is present: -Have pt side-lying on right side, with pillow under right trunk, flex both hips and knees, rotate trunk to left (or pelvis to right), pt can be taught to perform this at home. Spinal manipulation may be contraindicated for this condition. Sacroiliac Joint: Special tests: 1. Gillet’s test (march test)-After palpating the PSISs, the pt stands on one leg and pulls the opposite knee toward the chest. The blocked or dysfunctioning joint will not move while the normal joint will move inferiorly. 2. Long-sitting test-Used to determine if there is a posteriorly or anteriorly rotated innominate based on apparent leg length differences. If the lower limb on the affected side appears longer with a pt lies supine, but shorter when sitting, the test is positive, indicating an anterior innominate rotation on the affected side. Long to short=anterior If the lower limb is shorter in supine and appears to get longer when sitting, then a posterior innominate rotation exists on the affected side. Short to long=posterior 3. Sitting flexion test-therapist localizes the PSISs as the pt, in a sitting position, bends forward with arms across the chest and passes elbows between the knees as if to touch the floor. The pts feet should be in contact with the floor or resting on a stool. A positive test occurs when a blocked joint moves first and/or farther cranially. 4. Straight leg raise-Used to evaluate low back pain and can indicate the unilateral dysfunction of the SI joint. The test is positive if pain extends from the back down the leg in the sciatic nerve distribution. The cluster of 5 tests (3/5 to be positive) have a sensitivity of .91 and specificity of .87 related to SI joint pain. The tests are: 1. Distraction (applies cross arm pressure to both ASIS, + if increased pain) 2. Thigh thrust (pt supine with hip flexed to 90°, examiner applies posteriorly directed force through the femur, + if pain or symptoms reproduced) 3. Gaenslen’s test (pt supine with one leg hanging over edge of table, other if flexed toward chest. Examiner applies firm pressure to both the hanging leg and flexed, + if symptoms increase or reproduced) 4. Sacral thrust (pt lies prone and examiner applies a force vertically downward to the center of the sacrum, + if symptoms increased or reproduced) 5. Compression test (pt positioned in sidelying with affected side up, hips are flexed approx 45° and knees flexed to 90°. Examiner applies a force vertically downward on ASIS, + if symptoms increase or reproduced) TMJ (see MS chart) Capsular pattern: limitation of mouth opening Closed packed position: Clenched teeth Loose packed position: mouth slightly open ROM: Opening: 40mm Rotation: 25mm Translatory glide:15mm GAIT: Stance Phase (60% of gait cycle) Swing Phase (40% of gait cycle) Standard Terminology Heel strike Foot flat Midstance Heel off Toe Off Acceleration Midswing Deceleration Rancho Los Amigos Terminology Initial Contact Loading response Midstance Terminal Stance Pre-Swing Initial Swing Midswing Terminal Swing • = Standard terminology ( ) =Rancho terminology Stance Phase: •Heel strike: is the instant that the heel touches the ground to begin stance phase. (Initial Contact): is the beginning of the stance phase that occurs when the foot touches the ground •Foot flat: is the point in which the entire foot makes contact with the ground and should occur directly after heel strike. (Loading response): corresponds to the amount of time between initial contact and the beginning of the swing phase for the other leg. •Midstance: is the point during the stance phase when the entire body weight is directly over the stance limb. (Midstance): corresponds to the point in stance phase when the other foot is off the floor until the body is directly over the stance limb. •Heel off: is the point in which the heel of the stance limb leaves the ground. (Terminal stance): begins when the heel of the stance limb rises and ends when the other foot touches the ground. •Toe off: is the point in which only the toe of the stance limb remains on the ground. (Pre-swing): begins when the other foot touches the ground and ends when the stance foot reaches toe off. Swing phase: •Acceleration: beings when toe off is complete and the reference limb swings until positioned directly under the body. (Initial swing): beings when the stance foot lifts from the floor and ends with maximal knee flexion during swing. •Midswing: is the point when the swing limb is directly under the body. (Midswing): begins with maximal knee flexion during swing and ends when the tibia is perpendicular with the ground. •Deceleration: begins directly after midswing, as the swing limb begins to extend, and ends just prior to heel strike. (Terminal swing): beings when the tibia is perpendicular to the floor and ends when the foot touches the ground. Phase Heel Strike Hip Knee Begins to extend from a position of 20-40° of flexion. Hip in slight add & ER. Full knee extension before heel contact, but flexing as heel makes contact. Tibia ER Ankle Moving into PF Foot Supination (rigid at heel contact) Muscle Activity Ant tib: eccentric (to control pronation) EHL & ED: eccentric (decelerate PF) Pos tib, soleus, gastroc: eccentric (decelerate pronation) G max & hams: eccentric (resist flexion) Erector spinae: eccentric Foot Flat Hip moving into ext, add & IR. 20° flexion, moving towards extension. IR Midstance Neutral position, pelvis rotates posteriorlly. 15° Neutral flexion (moving toward extension) PFDF Pronation (adapting to support surface) 3° DF Neutral (control trunk flexion). G max & hams: concentric (to move hip into extension). After foot is flat, quads activity becoming concentric to bring femur over. Pos tib, soleus, FHL, FDL: eccentric to decelerate movement Pos tib, soleus, & gatroc: concentric (to supinate subtalar and metatarsal joint) Iliopsoas: eccentric. Glut med: creating reverse action to stabilize opposite pelvis. Quad Heel Off Toe Off 10-15° extension, abd, & ER. Moving towards 10° ext, abd, & ER. 4° flexion ER 15° DF Moving from full ext to 40° flexion. ER 20° PF Supination (rigid for push-off) Supination activity decreasing Quads activity decreasing Peroneus longus & abd hallucis: concentric (to PF 1st ray) Peronus brevis: antagonist to supinators of subtalar and metatarsal joints. FHL, EHL, EHB, & intrinsics: concentric stability. Adductor magnus: eccentric (to control pelvis) Reaction forces moving posterior to knee. Quadseccentric Phase Acceleration to Midswing Hip Slight flexion (015°) moving at 30° flexion and external rotation to neutral Knee 30°-60° knee flexion and external rotation of tibia moving toward neutral. Ankle& Foot 20° DF and slight pronation Midswing to Deceleration Continued flexion at about 30° to 40° Moving to near full extension & slight lateral tibial rotation Ankle in neutral; foot in slight supination Muscle Activity Hip: flexors working concentrically to bring limb through; contralateral glut med concentrically contracting to maintain pelvis position. Hamstrings concentrically contracting. Dorsiflexors contracting concentrically. Glut max contracting eccentrically to slow hip flexion. Quads contracting concentrically & hamstrings eccentrically. Dorsiflexors contracting isometrically. Peak Muscle Activity During the Gait cycle: Tibialis anterior: Peak activity is just after heel strike. Responsible for eccentric lowering of the foot into plantar flexion. Gastroc-soleus Peak activity is during late stance phase. Responsible for concentric group: raising of the heel during toe off. Quadriceps group: Two periods of peak activity. In periods of single support during early stance phase and just before toe off to initiate swing phase. Hamstrings group: Peak activity is during late swing phase. Responsible for decelerating the unsupported limb. ROM Requirements for Normal gait: Hip flexion 0-30° Hip extension 0-10° Knee flexion 0-60° Knee 0° extension Ankle DF 0-10° Ankle PF 0-20° Gait terminology: •Base of support-the distance measured between the left and right foot during progression of gait. The distance decreases as cadence increases. The average base of support for an adult is 2-4 inches. •Cadence-the number of steps an individual will walk over a period of time. The average value for an adult is 110-120 steps per minute. •Degree of toe-out-the angle formed by each foot’s line of progression and a line intersecting the center of the heel and second toe. The average degree of toe-out for an adult is 7° •Step length-the distance measured between right heel strike and left heel strike. The average for an adult is 28 inches. •Stride length-the distance measured between right heel strike and the following right heel strike. The average for an adult is 56 inches. Abnormal gait patterns: •Antalgic-a protective gait pattern where the involved step length is decreased in order to avoid weight bearing on the involved side, usually secondary to pain. •Ataxic-a gait pattern characterized by staggering and unsteadiness. There is usually a wide base of support and movements are exaggerated. •Cerebellar-a staggering gait pattern seen in cerebellar disease. •Circumduction-a gait pattern characterized by a circular motion to advance the leg during swing phase; this may be used to compensate for insufficient hip or knee flexion or dorsiflexion. •Double step-a gait pattern in which alternate steps are of a different length or at a different rate. •Equine-a gait pattern characterized by high steps; usually involves excessive activity of the gastrocnemius. •Festinating-a gait pattern where a pt walks on toes as though pushed. It starts slowly, increases, and may continue until the pt grasps an object in order to stop. •Hemiplegic-a gait pattern in which pts abduct the paralyzed limb, swing it around, and bring it forward so the foot comes to the ground in front of them. •Parkinsonian-a gait pattern marked by increased forward flexion of the trunk and knees; gait is shuffling with quick and small steps; festinating may occur. •Scissor-a gait pattern in which the legs cross midline upon advancement •Spastic-a gait pattern with stiff movement, toes seeming to catch and drag, legs held together, and hip and knee joints slightly flexed. Commonly seen in spastic paraplegia. •Steppage-a gait pattern in which the feet and toes are lifted through hip and knee flexion to excessive heights; usually secondary to dorsiflexor weakness. The foot will slap at initial contact with the ground secondary to the decreased control. •Tabetic-a high stepping ataxic gait pattern in which the feet slap the ground. •Trendelenburg-a gait pattern that denotes gluteus medius weakness; excessive lateral trunk flexion and weight shifting over the stance leg. •Vaulting-a gait pattern where the swing leg advances by compensating through the combination of elevation of the pelvis and plantar flexion of the stance leg. MS Interventions: Orthopaedic Surgical Repairs: 1. Surgical repairs of upper extremity: a. Rotator Cuff tears i. Usually degenerative and occur over time, with impingement of supraspinatus tendon between the greater tuberosity and acromion. ii. Signs and symptoms include: -Significant reduction in AROM into abduction -No reduction of PROM -Drop arm test is positive -Poor scapulothoracic and glenohumeral rhythm b. Diagnostic tests utilized: arthrogram traditionally had been the “gold standard” test. MRI may be done, but may not be as sensitive. c. PT goals, outcomes, and interventions: -Rehab is initiated, following a period of immobilization with surgical intervention -PT intervention emphasizes return or normal strength/endurance/coordination of muscles, joint mechanics, flexibility (AROM/PROM), and scapulothoracic and glenohumeral rhythm with overhead function. 2. Tendon injuries and repairs of the hand: a. Flexor tendon repairs i. First 3-4 weeks, distal extremity is immobilized with a protective splint, with wrist and digits flexed. Rubber band traction is applied to maintain interphalangeal joints in 30-50° of passive flexion. ii. PT goals, outcomes and interventions: 1. Pt can perform resisted extension and passive flexion with constraints of splint. AROM to tolerance is initiated at 4 weeks. 2. Goal is to manage all soft tissues through wound-healing phases by providing collagen remodeling, which preserves free tendon gliding. 3. Early intervention consists of wound management, edema control, and passive exercises. 4. Active extension exercises are initiated first followed by flexion. 5. Resistive and functional exercises are introduced when full AROM is achieved. b. Extensor tendon repairs i. Distal repairs are immobilized such that the distal interphalangeal joints are in neutral for 6-8 weeks. ii. PT goals, outcomes, and interventions: 1. AROM is initiated at 6 weeks, with PIP joints in neutral 2. Goal is to manage all soft tissues through wound-healing phases by providing collagen remodeling, which preserves free tendon gliding 3. Early intervention consists of wound management, edema control, and passive exercises. 4. Active extension exercises are initiated first, followed by flexion. 5. Resistive and functional exercises are introduced when full AROM is achieved. 6. Proximal repairs are immobilized, with the wrist and digital joints in extension for 4 weeks. 7. PT goals, outcomes, and interventions: Early AROM/PROM in flexion with MCP joint in extension. At 6 weeks, full AROM is initiated into flexion and extension. 3. Surgical repairs of lower extremity: a. Total hip replacement/arthroplasty (THR): This info may vary, depending on surgical procedure and/or MD preference/protocol. Must be familiar with postoperative protocol for each patient relative to procedure and/or MD. b. Cemented vs. non-cemented. i. Cemented hips can tolerate full weight bearing immediately following surgery. ii. Cement may crack with aging, causing a loosening of prosthesis. Noncemented technique is more stressful on bones during the surgical procedure. iii. Noncemented procedures are typically used with younger and/or more active individuals. Cemented technique may be better for those who will benefit from immediate ability to weight bear e.g. those with dementia or significant debilitation. iv. Bed positioning with a wedge to prevent adduction v. Pt should avoid the position of hip flexion >90° with adduction and IR. vi. Partial weight bearing to tolerance is initiated on the second post-surgery day, using crutches or a walker with typical surgical procedures. vii. PT goals, outcomes, and interventions: PT focuses on bed mobility, transitional movements, ambulation, and return to premorbid ADLs. c. Open reduction internal fixation (ORIF) following femoral fx: i. Pt will typically be non-weight bearing for 1-2 weeks, using crutches or a walker. Thereafter, the pt will be partial weight bearing as tolerated. ii. PT goals, outcomes, and interventions: Pt focus on bed mobility, transitional movements, ambulation, and return to premorbid ADLs. Important to note that guidelines/precautions can vary significantly. d. Total knee replacement/arthroplasty (TKR): i. TKR surgery is typically performed as a result of severe DJD of the knee joint, which has lead to pain and impaired function. ii. PT goals, outcomes, interventions: Goals of early rehab (1-3 weeks) include muscle reeducation, soft tissue mobilization, lymphedema reduction, and initiation of PROM (CPM), AROM, and reduction of postsurgical swelling. iii. Goals of the second phase of rehab include regaining endurance, coordination, and strength of the muscles surrounding the knee. Functional activities include progressive ambulation stair climbing, as well as transitional training based on healing and the type of prosthesis used. iv. Goals and outcomes of the last phase of rehab include returning the pt to premorbid ADLs. Functional and endurance training and proprioceptive exercises introduced during this phase. v. The weight bearing status of pts with a cemented prosthesis is at the level of the pts tolerance. Pts with cementless prostheses are progressed according to the time frame for fx healing. Weight bearing is 25% at 1-7 weeks, 50% by week 8, 75% by week 10, and 100% without an AD by week 12. vi. Avoidance of forceful mobilization and PROM into flexion >90° is important, because of the mechanical restraints of the prosthesis. vii. Biomechanical faults caused by joint restrictions should be corrected with joint mobilizations to the specific restrictions identified during the exam. e. Ligamentous repairs of the knee i. Six phases of rehab are followed with ACL and PCL reconstructive surgery. Anterior cruciate ligament reconstruction: -Immediately following surgery, a CPM unit is utilized, with PROM from 0°-70° of flexion. -Motion is increased to 0°-120° by the 6th week. -Reconstruction is usually protected with a hinged brace set at 20°-70° of flexion initially. -Pt is non-weight bearing for approx 1 week. -Weight-bearing progresses as tolerated to full weight bearing -Pt is weaned from brace between the 2nd and 4th weeks Posterior cruciate ligament reconstruction: -Generally similar to ACL repair, except is often initially in hinged brace at 0° during ambulation. -6 phases of rehab for ACL/PCL are as follows: Preoperative, maximum protection, controlled motion, moderate protection, minimum protection, and return to activity. -Specific interventions: -Soft tissue massage to quad/hams to reduce muscle guarding; joint oscillations to inhibit joint pain and muscle guarding; correction of muscle imbalances and biomechanical faults; progress to functional training based on pts occupation and recreation. Lateral retinacular release: -Typically performed as a result of patellofemoral pain syndrome (PFPS). Purpose of procedure is to restore normal tracking of the patella during contraction of the quads muscle. PT intervention: 1. Should emphasize closed kinetic chain exercises to strengthen quadriceps muscle and regain dynamic balance of all structures (contractile and noncontractile) surrounding knee. 2. Normalize the flexibility of the hamstrings, triceps surae, and ITB will help restore mechanical alignment. 3. Mobilization of patella is important to maintain nutrition and decrease the likelihood of adhesions. Meniscal arthoscopy: 1. Partial meniscectomy: a. Partial weight bearing as tolerated when full knee extension is obtained b. PT goals, outcomes, and interventions: i. ii. iii. iv. Initial goals focus on edema/effusion control AROM is urged after surgical day 1. Isotonic and isokinetic strengthening by day 3. Jogging on the ball of the foot or toes is recommended to decrease the loading of the knee joint. 2. Repairs a. Pt will be non-weight bearing for 3-6 weeks b. Rehab of the joint begins within 7-10 days of procedure. c. PT goals, outcomes, interventions: Soft tissue/massage to quad/hams, joint oscillations, correction of muscle imbalances, biomechanical faults, progression to functional training 3. Surgical repairs of spine: a. Rehab varies according to the type of surgery performed. b. A back protection program and early mobilization exercises should be initiated prior to surgery. c. Pts should avoid prolonged sitting, heavy lifting, and long car trips for approx 3 months. d. Repetitive bending with twisting should always be avoided. e. With microdiscetomies, rehab time is decreased bc the fibers of the annulus fibrosus are not damaged. f. With laminectomy/discectomy, early movement and activation of paraspinal musculature (especially mulitfidus) is necessary. g. Multilevel vertebra fusion: i. Typically requires 6 weeks of trunk immobility with bracing ii. Once brace is removed and movement is allowed, important to regain as much normal/functional movement as possible, while restoring functional activation of muscles. iii. With combined anterior/posterior surgical approach, bracing is seldom used. h. With Harrington rod placement for idiopathic scoliosis, rehab goals focus on early mobilization in bed and effective coughing. i. The pt can begin ambulation between the 4th and 7th postoperative days j. The pt should avoid heavy lifting and excessive twisting and bending. k. PT goals, outcomes, and interventions: Soft tissue/massage to paraspinal muscles; joint oscillations to inhibit joint pain, correction of muscle imbalances, make sure that multifidus function is restored. Interventions for Patients/clients with Acute Conditions o Acute Phase Immobilization with limited (1-2 days) bed rest. Use of braces, slings, corsets, cervical collars, assistive devices, and taping Control inflammatory response (RICE) Physical agents: ice and electrical stimulation Compression and elevation to reduce and prevent effusion and swelling. NSAIDs Rest/relaxation to reduce pain Soft tissue/massage techniques Assisted movement of injured tissue Joint oscillations (grade 1-2) for pain relief Therapeutic exercise Dose of 40-60% of one rep max to stimulate regeneration of tissue and revascularization. Exercise should be nontraumatic, meaning no pain and/or increased edema as a result of the exercise. Educate Pt/client on joint protection strategies o Subacute phase Avoidance of continued irritation and repetitive trauma. Modify activities at home/work/recreation Modify use of equipment or type of equipment at home/work/recreation Correct biomechanical faults, such as leg length discrepancy, abnormal foot biomechanics, abnormal throwing motion. Joint mobilization Continued therapeutic exercises, including flexibility/endurance/coordination exercise. Postural reeducation Biomechanical education o Functional restoration phase Maintain or return to optimal level of Pt function Normalize flexibility of joints and related soft tissues Restore loading capacity of connective tissues to normal strength Functional strengthening exercise Functional stabilization of the involved joint/region. Interventions for Patients/Clients with a Chronic Condition o Determine possible causative factors Abnormal remodeling of injured tissues Chronic low-grade inflammation due to repetitive stresses of tissues. o Reduce stresses to tissues Identify/eliminate magnitude of loading Identify/eliminate direction of forces Identify and eliminate any biomechanical barriers that are preventing haling Pt education regarding protection of joints and associated soft tissues. o Regain structural integrity Improving flexibility Postural reeducation Increasing tissue capacity to tolerate loading Functional strengthening, endurance, and coordination exercises. o Resume optimal patient function and prevention of reoccurrence Pt education regarding causative factors in dysfunction Work conditioning Specific Interventions: o Soft tissue/myofascial techniques Aid in reduction of metabolites for muscle, reactivating a muscle that has not been functioning secondary to guarding and ischemia, revascularization of muscle, and also decreased guarding in a muscle Autonomic: stimulation of skin and superficial fascia to facilitate a decrease in muscle tension. Mechanical: movement of skin, fascia, and muscle causes histological and mechanical changes to occur in soft tissue to produce improved mobility and function. Goals: decrease pain, edema, and muscle spasm, increase metabolism and cutaneous temp, stretch tight muscles and other soft tissues, improve circulation, strengthen weak muscles, and mobilize joint restrictions. Indications: Pt with soft tissue and joint restrictions that result in pain and limits in ADLs Contraindications Absolute- soft tissue breakdown, infection, cellulitis, inflammation, and or neoplasm. Relative- hypermobility and sensitivity Traditional massage techniques such as effleurage and petrissage Functional Massage Three techniques used to assist in reactivation of a debilitated muscle and/or to increase vascularity to a muscle. o Soft tissue without motion Traditional technique; however hands do not slide over skin; instead, they stay in contact with the skin while hands and skin move together over the muscle. Direction of force is parallel to muscle fibers, and total stroke time should be 5-7 seconds. o Soft tissue with passive pumping Place muscle in shortened position and with one hand place tension on muscle parallel to muscle fibers. Other hand passively lengthens muscle and simultaneously gradually releases tension of hand in contact with muscle. o Soft tissue with active pumping Place muscle in lengthened position, and with one hand place tension on muscle, perpendicular to muscle fiber. Other hand glides limb as Pt actively shortens muscle. As muscle shortens, gradually release tension of hand in contact with muscle. Transverse Friction Massage o Used to initiate an acute inflammatory response for a tissue that is in metabolic stasis, such as a tendonosis. o Involved tendon is briskly massaged in a transverse fashion o Performed for 5-10 min and tends to be very uncomfortable for the pt Movement approaches require the pt to actively participate in treatment. Examples include: o Feldenkrais Facilitates development of normal movement patterns The practitioner uses skillful, supportive, gentle hands to create a sense of safety, maintain supportive contact, while introducing new movement possibilities in small, easily available increments. o Muscle energy techniques Include voluntary contraction in a precisely controlled direction, at varying levels of intensity, against an applied counterforce from the clinician. Purpose is to gain motion that is limited by restrictions of the neuromuscular system. Modification of PNF technique o PNF hold-relax-contract technique Antagonist of the shortened muscle is contracted to achieve reciprocal inhibition and increased range o Articulatory techniques Joint oscillations Inhibit pain and/or muscle guarding Lubricate joint surfaces Provide nutrition to the joint structure Grades 3-4 are beneficial to stretch tight connective tissue Five grades of joint play in neutral Grade I oscillations are small amplitude at the beginning of the range of joint play. Grade II oscillations are large amplitude at the midrange of joint play. Grade III oscillations are large amplitude at the end range of joint play. Grade IV oscillations are small amplitude at the end of joint play. Grade V is a manipulation of high velocity and low amplitude to the anatomical endpoint of a joint. Indications for use of oscillation grades, per Maitland Grade I and II are used to improve joint lubrication/nutrition, as well as decrease pain and muscle guarding. Grades III and IV are used to stretch tight muscles, capsules, and ligaments Grade V is used to regain normal joint mechanics, as well as decrease pain and muscle guarding. Contraindications Absolute: joint ankylosis, malignancy involving bone, disease that affects the integrity of ligaments, arterial insufficiency, and active inflammatory and/or infective process. Relative: arthrosis (DJD), metabolic bone disease, hypermobility, total joint replacement, pregnancy, spondylolisthesis, use of steroids, and radicular symptoms. Joint mobilization (nonthrust) To stretch/lengthen/deform collagen and normalize the arthrokinematic glide of joint structures. Grades of translatoric glide, as described by Kaltenborn: o Grade I Loosening translatoric glide Movement is very small amplitude traction force Used to relieve pain and/or decompress a joint during joint glides, performed within examination or intervention. o Grade II Tightening translatoric glide. Movement takes up slack in tissues surrounding joint. Used to alleviate pain, assess joint play, and/or reduce muscle guarding. o Grade III Stretching translatoric glide Movement stretches tissue crossing joint Used to assess end-feel, or to increase movement (stretch tissue) Traction: manual, mechanical, and self or auto traction Vertebral bodies separating Distraction and gliding of facet joints Tensing of the ligamentous structures of the spinal segments Intervertebral foramen widening Spinal muscle stretching Contraindications Absolute: joint ankylosis, malignancy involving bone, disease that affect the integrity of ligaments, arterial insufficiency, and active inflammatory and/or infective process. Relative: arthrosis (DJD), metabolic bone disease, hypermobility, total joint replacement, pregnancy, spondylolisthesis, use of steroids, and radicular symptoms. Manipulation thrust Inhibit pain and/or muscle guarding Improve translatoric glide in cases of joint dysfunction due to restriction. Health-care practitioners who commonly perform manipulative thrusts include physical therapist, osteopaths, chiropractors, and medical doctors. Types of manipulations o Generalized Fairly forceful, long lever techniques intended to include as many vertebral segments as possible. More commonly performed by chiropractors o Specific Aimed at having an effect on either a specific segment or only a few vertebral segments. Uses minimal force with short lever arms Often include locking techniques based on biomechanics to ensure that a specific vertebral segment receives the manipulative thrust. More commonly performed by a PT. o Mid-range Vary gently, short lever arm technique Barrier is created in mid-range by specific positioning of patient as well as creating tautness in surrounding soft tissues. More commonly performed by osteopathic practitioners. Contraindications Absolute: joint ankylosis, malignancy involving bone, disease that affect the integrity of ligaments, arterial insufficiency, and active inflammatory and/or infective process. Relative: arthrosis (DJD), metabolic bone disease, hypermobility, total joint replacement, pregnancy, spondylolisthesis, use of steroids, and radicular symptoms. Common mistakes in performing a thrust manipulation Not communicating clearly with the pt regarding the technique. Taking too long to position the pt Not performing the trial thrust prior to the actual thrust Not allowing the person to bottom out with their breath prior to performing the thrust. Taking up the slack as the Pt exhales and then letting off with pressure prior to the thrust Velocity too slow/amplitude to great. Suggested algorithm to perform a manipulation Consider indications and contraindications Explain the intensions and implications regarding manipulation to the Pt Describe the actual technique to the Pt Place the Pt into position and assess for Pt comfort Perform a pre-thrust force into the rage to determine Pt comfort. Ask Pt to inhale and then exhale. Take up the slack into the range as they exhale. When they reach the end of exhalation perform the thrust. o Neural tissue mobilization Movement of neural structures to regain normal mobility. Tension test for upper and lower extremities Movement of soft tissues that may be restricting neural structures Indications: used for pts who have some type of restriction in neural mobility, anywhere along the course of the nerve. Postural reeducation: to open up the intervertebral foramen and decrease tension to tissue. Contraindications: extreme pain and/or increase in abnormal neurological signs Determine whether managing irritated or nonirritated neurologic tissue: 1. Irritated tissue a. Utilize grade II mobilizations (based on Maitland scale): should be nonpainful 2. Nonirritated tissue: a. Utilize garde III mobilizations to engage the barrier but remain nonpainful. Therapeutic exercise for ms conditions: 1. Therapeutic exercise is indicated to: a. Decrease muscle guarding b. Decrease pain c. Increase vascularity of tissue d. Promote regeneration and/or speed up recovery of connective tissues, such as cartilage, tendons, ligaments, capsules, intervertebral discs e. Mobilize restricted tissue to increase flexibility f. Increase endurance of muscle g. Increase coordination of muscle h. Sensitize muscles to minimize joints going into excessive range, in cases of hypermobility i. Develop dynamic stability and functional movement patterns, allowing for optimal function within the environment 2. Home exercise program for pts with ms conditions: a. Pts home program will consist of exercsies to reinforce clinical program b. Necessary to perform enough repetitions for desired physiological effect on appropriate tissues, as well as to develop coordination and endurance in order to promote dynamic stability within functional patterns. 3. Dry Needling a. Also referred to intramusuclar manual therapy (IMT) b. Utilized to break up trigger points in myofascial pain syndrome c. A solid filiform needlel is inserted into the trigger point (within the muscle) Manual Therapy Approaches in Rehab: 1. All approaches proved a philosophical basis, subjective evaluation, objective examination, a diagnosis, and a plan of care. 2. Approaches can be divided into three categories: a. Physician generated. i. Mennell believed the joint is the dysfunctional unit. ii. Osteopaths suggest that any component of the somatic system is responsible for dysfunction. iii. Cyriax contends that dysfunction is due to interplay between contractile and noncontractile tissues. b. Physical Therapist Generated i. Mckenzie feels that postural factors preciptiate discal dysfunction. Treatment emphasizes the use of extension exercises. ii. Maitland proposes that the subjective evaluation should be integrated with objective measures to determine the dysfunctional area iii. Kaltenborn believes that abnormal joint mobility and soft tissue changes account for dysfunction c. Chiropractic generated i. Focus is to restore normal joint function through soft tissue and joint manipulation. Chiropractics believe that restoration of normal biomechanical function affects other systems of the body as well, thus improving the state of health in many ways. Psychosocial Considerations: 1. Malingering (symptom magnification syndrome) a. Defined as a behavioral response where displays of symptoms control the life of the patient, leading to functional disability. b. There may be psychological advantages to illness. i. The pt may feel protected from the threatening world. ii. Uncertainty or fear about the future. iii. Social gain iv. Reduces stressors c. Therapist needs to recognize symptoms and respond to the pt i. Tests to evaluate malingering back pain may include Hoover test, Burn’s test, and Waddell’s signs. ii. Hoover test involves the therapists evaluation of the amount of pressure the pts heels place on the therapists hands when the pt is asked to raise one lower extremity while in a supine position. iii. Burn’s test requires the pt to kneel and bend over a chair to touch the floor. iv. Waddell’s signs evaluate tenderness, simulation tests, distraction tests, regional disturbances, and overreaction. Waddell’s scores can be predictive of functional outcome. v. Functional capacity evaluations are used to evaluate psychosocial as well as physical components of disability. vi. Emphasize regaining functional outcomes, not pain reduction. d. Secondary gain. i. Usually some type of financial gain for staying ill. ii. Workers compensation iii. Larger settlement for injury claims iv. Frequently seen in clinics that manage industrial injuries v. May not want to return to work for various reasons associated with the work environment (stress, disliking coworkers) MS Imaging: Tissue Air Fat Bone Cortex Radiograph Black Poorly visualized White CT Black Black White TI MRI Black White Black T2 MRI Black Gray Black Bone Marrow White Gray White Gray Neuromuscular Examination: Blood Supply to the Brain: Blood Supply to the Brain Anterior cerebral artery (ACA): anterior frontal lobe; medial surface of frontal & parietal lobes Middle Cerebral artery (MCA): most of outer cerebrum, basal ganglia, posterior and anterior internal capsule, putamen, pallidum, lentiform nucleus Posterior cerebral artery (PCA): portion of midbrain, subthalamic nucleus, basal nucleus, thalamus, inferior temporal lobe, occipital and occipitoparietal cortices Expected Possible Impairment -Contralateral LE motor and sensory involvement -Loss of bowel and bladder control -Loss of behavioral inhibition -Significant mental changes -Neglect -Aphasia -Apraxia & agraphia -Perservation -Akinetic mutism with significant bilateral involvement -Most common site of CVA -Wernike’s aphasia in dominant hemisphere -Homonymous hemianopsia -Apraxia -Flat affect with right hemisphere damage -Contralateral weakness and sensory loss of face and upper extremity with lesser involvement in the lower extremity -Impaired spatial relations -Anosognosia in non-dominant hemisphere -Impaired body schema -Contralateral pain & temp sensory loss -Contralateral hemiplegia (central area), mild hemiparesis -Ataxia, athetosis or choreiform movement -Quality of movement is impaired -Thalamic pain syndrome -Anomia -Hemiballisums -Visual agnosia Vertebral-basilar artery: lateral aspect of pons and midbrain together with superior surface of cerebellum, cerebellum, medulla, pons, midbrain -Homonymous hemianopsia -Memory impairment -Alexia, dyslexia -Cortical blindness form bilateral involvement -Loss of consciousness -Hemiplegia -Comatose or vegative state -Inability to speak -Locked in syndrome -Vertigo -Nystagmus -Dysphagia -Dysarthria -Syncope -Ataxia Spinal Cord tracts: Ascending tracts-Sensory tracts ascending in the white matter of the spinal cord arise either from cells of spinal ganglia or from intrinsic neurons within the gray matter that receive primary sensory input. Relay sensory feedback to the cerebrum and cerebellum. Descending tracts-Involved with voluntary motor function, muscle tone, reflexes and equilibrium, visceral innervation, and modulation of ascending sensory signals. Ascending Tracts Fasciculus cuneatus (posterior or dorsal column): sensory tract for trunk, neck, UE proprioception, vibration, two-point discrimination, and graphesthesia. Descending Tracts Anterior corticospinal tract-pyramidal motor tract responsible for ipsilateral voluntary, discrete, and skilled movements Fasciculus gracilis (posterior or dorsal column): sensory tract for trunk and LE proprioception, two-point tract discrimination, vibration, and graphesthesia Spinocerebellar tract (dorsal): sensory tract that ascends to the cerebellum for ipsilateral subconscious proprioception, tension in muscles, joint sense, and posture of the trunk and LEs. Spinocerebellar tract (ventral): sensory tract that ascends to the cerebellum, some fibers crossing with subsequent recrossing at the level of the pons for ipsilateral subconscious proprioception, tension in muscles, joint sense, and posture of the trunk, UEs, and LEs. Sino-olivary tract-ascends to the cerebellum and relays info from cutaneous and proprioceptive organs Spinoreticular tract: the afferent pathway for the reticular formation that influences level of consciousness Lateral corticospinal tract-pyramidal motor tract responsible for contralateral voluntary fine movement •Damage to the corticospinal tracts results in a positive Babinksi sign, absent superficial abdominal reflexes and cremasteric reflex, and the loss of fine motor or skilled voluntary movement. Reticulospinal tract: extrapyramidal motor tract responsible for facilitation or inhibition of voluntary and reflex activity through the influence on alpha and gamma motor neurons. Rubrospinal tract: extrapyramidal motor tract responsible for motor input of gross posture tone, facilitating activity of flexor muscles, and inhibiting the activity of extensor muscles. Tectospinal tract: extrapyramidal motor tract responsible for contralateral postural muscle tone associated with auditory/visual stimuli Vestibulospinal tract: extrapyramidal motor tract responsible for ipsilateral gross postural adjustments subsequent to head movements; facilitating activity of the extensor muscles and inhibiting activity of the flexor muscles •Damage to the extrapyramidal tracts results in significant paralysis, hypertonsicity, exaggerated deep tendon reflexes, and clasp-knife reaction. Spinotectal tract-sensory tract providing afferent information for spinovisual reflexes and assists with movement of eyes and heads towards a stimulus Anterior spinothalamic tract-sensory tract for light touch and pressure Lateral spinothalamic tract-sensory tract for pain and temperature sensation Cranial Nerves: Nerve I-Olfactory Afferent (sensory) function Smell II-Optic Eye Efferent (motor) function How to test Identify familiar objects, close off other nostril Test visual fields (Snellen eye III-Oculomotor IV-Trochlear V-Trigeminal Skin of face, mucous membranes of nose, sinuses, mouth, anterior tongue VI-Abducens VII-Facial Taste: anterior tongue VIII-Vestibulocochlear Hearing & balance (ear) IX-Glossophyaryngeal Touch, pain: posterior tongue, pharynx Taste: posterior tongue Touch,pain: pharynx, larynx, bronchi Taste: tongue, epiglottis X-Vagus XI-Spinal Accessory XII-Hypoglossal Voluntary: Elevation of eyelid, superior, medial, and inferior recti, inferior oblique muscle of eyeball. Turns eye up, down & in Autonomic: smooth muscle of eyeball Turns adducted eye down Temporal & masseter muscles (mastication) Turns eye out (lateral rectus muscle) Facial expressions. Autonomic: lacrimal, submandibular, and sublingual glands Select muscle of pharynx; parotid gland Muscles of palate, pharynx, and larynx Thoracic and abdominal viscera Sternocleidomastoid & trapezius Tongue movements chart), 20 ft away, test peripheral vision Up, down, and in (medial gaze) Pupillary size/shape, reaction to light Downward & lateral gaze Corneal reflex, face sensation, clench teeth; push down on chin to separate jaws Lateral gaze Close eyes tight, smile and show teeth, whistle and puff cheeks Identify familiar tastes Eye-head coordination, vestibular ocular reflex, auditory acuity. Weber’s test: place tuning fork on top of head. Rinne’s test-place on mastoid process Gag reflex, ability to swallow, listen to voice quality Examine for difficulty in swallowing, ability to say “ahhh” Resisted shoulder shrug Tongue protrusion (if injured, tongue deviates toward injured side) Upper Motor Neuron (UMN) VS. Lower Motor Neuron (LMN) UMN Lesion Central Nervous System Cortex, brainstem, corticospinal tracts, spinal cord CP, hydrocephalus, ALS, CVA, birth injuries, MS, Huntington’s chorea, TBI, Pseudobulbar palsy, brain tumors Location of Lesion: Structures involved: Disorders: Tone: Reflexes: Involuntary movements: Strength: Muscle Bulk: Hypertonia; velocity dependent Increased: hyperreflexia, clonus, + Babinski Muscle spasms: flexor or extensor Stroke: weakness or paralysis on one side of the body Disuse atrophy Voluntary movements: Impaired or absent: dyssynergic patterns LMN Lesion Peripheral nervous system Anterior horn cell, spinal roots, peripheral nerves, cranial nerves Poliomyelitis, ALS, Guillain-Barre syndrome, tumors involving the spinal cord, trauma, progressive muscular atrophy, infection, Bell’s palsy, carpal tunnel syndrome, muscular dystrophy, spinal muscular atrophy Hypotonia, flaccidity; not velocity dependent Decreased or absent, hyporeflexia With denervation: fasciulations Segmental or focal pattern Neurogenic atrophy: rapid focal severe wasting Weak or absent if nerve interruped Reflexes: Superficial Reflex Testing: Reflex Abdominal Reflex Spinal Level T8-L1 Corneal “blink” reflex Trigeminal and facial nerves Procedure Stoke briskly & lightly with a blunt object from each quadrant of the abdomen in a diagonal manner towards the umbilicus Ask the pt to look up and away from you; stroke the cornea using a piece of cotton Normal response Contraction of the abdominals and deviation of the umbilicus in the direction of the stimulus Both eyes will blink with contact to one eye Cremasteric reflex L1-L2 Gag Reflex Glossopharyngeal & vagus nerves Plantar reflex L5-S1 Scratch the skin of the upper medial thigh The therapist lightly stimulates each side of the back of the throat and notes the reaction A brisk and brief elevation of the testicle on the ipsilateral side A gag will occur post stimulation; may be absent in some percentage of the normal population Stroke the lateral aspect of the Flexion of the toes *Babinski sole of the foot with the blunt end reflex is the abnormal response of a reflex hammer from theheel that indicates CNS lesion to the ball of the foot and medially to the base of the great toe Reflex Grading Scale: Reflex Grading 0=no response 1+=diminished response 2+=active normal response 3+=exaggerated resonse 4+=hyperactive; very brisk Interpretation Always abnormal May or may not be normal Normal May or may not be normal Always abnormal Stroke: Ceberovascular accident-is a specific event that results in a lack of oxygen supply to a specific area of the brain secondary to either ischemia or hemorrhage. Types of Cerebrovascular Accidents: Transient Ischemic Attack (TIA): Completed Stroke: Stroke in Evolution: Is usually linked to an atherosclerotic thrombosis which causes a temporary interruption of blood supply to an area of the brain. Symptoms resolve typically between 24-48 hrs. A CVA that presents with total neurological deficits at the onset. A CVA, usually caused by a thrombus that gradually progresses. Total neurological deficits are not seen for one to two days after onset. Ischemic Stroke: Once there is a loss of perfusion to a portion of the brain (within just seconds), there is a central area of irreversible infarction surrounded by an area of potential ischemia. •Embolus (20% of ischemic CVAs): associated with cardiovascular disease, can be a solid liquid or gas and originate in any part of the body. Occurs rapidly with no warning, and presents with a headache. •Thrombus: atherosclerotic plaque develops in an artery and occludes the artery causing an infarct. Symptoms can appear in minutes or over several days. Usually occurs during sleep or upon awakening after a MI or post surgical procedure. Abnormal bleeding in the brain due to a rupture in blood supply. HTN is usually a precipitating factor causing rupture of an aneurysm. Characteristics include: headache, vomiting, high BP. Approx. 50% of deaths from hemorrhagic stoke occur within the first 48 hours. Hemorrhage (10-15% of CVAs): Characteristics of a CVA: Left Hemisphere Weakness, paralysis of the right side ↑ frustration ↓ processing Possible aphasia (expressive, receptive, global) Possible dysphagia Right Hemisphere Weakness, paralysis of the left side ↓attention span Left hemianospia ↓awareness and judgment Possible motor apraxia (ideomotor and ideational) ↓discrimination between left and r ight Right hemianopsia Left inattention Memory deficits ↓abstract reasoning Emotional lability Impulsive behaviors Brainstem Unstable vital signs ↓consciousness ↓ ability to swallow Weakness on both sides of the body Paralysis on both sides of the body Cerebellum ↓balance Ataxia ↓coordination Nausea ↓ability for postural adjustment Nystagmus ↓spatial orientation Left hemisphere (right hemiplegia): Slow, cautious, and insecure. Give frequent feedback and support. Use appropriate communication: words, gestures, assess level of understanding. Don’t underestimate ability to learn. Right Hemisphere (left hemiplegia): Quick, impulsive, poor judgment. Use verbal cues (demonstrations or gestures may confuse pts). Give frequent feedback: focus on slowing down and controlling movement. Focus on safety, avoid clutter. Do not overestimate ability to learn. Synergy Patterns: Upper Limb Scapula Shoulder Elbow Forearm Wrist Fingers Thumb Flexor synergy Elevation & retraction Abduction & ER Flexion Supination Flexion Flexion with adduction Flexion and adduction Extensory synergy Depression & Protraction IR & adduction Extension Pronation Extension Flexion with adduction Adduction and flexion Flexor synergy Abduction and ER Flexion Dorsiflexion with supination Extension Extenor synergy Extension, IR, and adduction Extension Plantar flexion with inversion Flexion and adduction Lower limb Hip Knee Ankle Toes CVA tests and measures: National Institue of Health (NIH) Stroke Scale: Functional Independce Measure (FIM): Stroke Impact Scale: Assessment of an acute CVA relative to impairment Provides a level of burden through assessment of mobility and ADL management Assessment of physical and social disability or level of impairment Fugl-Meyer Assessment of Physical Performance: secondary to CVA Motor, sensory, and balance impairment; also assesses pain and ROM NM & nervous system Terminology Agnoisa: the inability to interpret information. Agraphesthesia: the inability to recognize symbols, letters, or numbers traced on the skin. Agraphia: the inability to write due to a lesion within the brain and is typically lfound in combination with aphasia. Alexia: the inability to read or compreheand written language secondary to a lesion within in the dominant lobe of the brain. Anosognosia: the denial or unawareness of one’s illness; often associated with unilateral neglect. Aphasia: the inability to communicate or comprehend due to damage to specific areas of the brain. Apraxia: the inability to perform purposeful learned movements or activities even though there is no sensory or motor impairment that would hinder completion of the task. Asterognosis: the inability to recognize objects by sense of touch. Body schema: having an understanding of the body as a whole and the relationship of its parts to the whole. Constructional apraxia: the inability to reproduce geometric figures and designs. A person is often unable to visually analyze how to perrom a task. Decerebrate rigidity: a characteristic of a cortiospinal lesion at the level of the brainstem that results in extension of the trunk and all extremities. Decorticate rigidity: a characteristic of a cortiospinal lesion at the level of the diencephalon where the trunk and lower extremities are positioned in extension and the upper extremities are positioned in flexion. Dilopia: double vision Dysarthria: slurred and impaired speech Dysphagia: inability to properly swallow Dysprosody: impairment in the rhythm and inflection of speech. Emotional lability: a characteristic of a right hemisphere infarct where there is an inability to control emotions and outbursts of laughing or crying that are inconsistent with the situation. Fluent aphasia (Wernike’s aphasia/temporal): characteric of receptive aphasis where speech produces functional output regarding articulation, but lacks content and is typically dysprosodic using neologisic jargon. Hemiparesis: condition of weakness on one side of the body Hemiplegia: condition of paralysis on one side of the body Homonymous hemianopsia: the loss of the right or left half of the visual field of vision in both eyes. Ideational apraxia: the inability to perform an initial motor plan and sequence tasks where the proprioceptive input necessary for movement is impaired. Ideomotor apraxia: a condition where a person plans a movement or task, but cannot volitionally perform it. Automatic movement may occur, however a person cannot imose additional movement on command. Neologism: substitution within a word that is so severe that it makes the word unrecognizable. Non-fluent aphasia (Broca’s aphasia/frontal lobe): characteristic of expressive aphasia where speech is nonfunctional, effortful, and contains paraphasias. Writing is also impaired. Perservation: the state of repeatedly performing the same segment of a task or repeatedly saying the same word/phrase without a purpose Synergy: mass movement patterns that are primitive in nature and coupled with spasticty due to brain damage Unilateral neglect: the inability to interpret stimuli and events on the contralateral side of a hemispheric lesion. Leftsided neglect is most common with a lesion to the right inferior parietal or superior temporal lobes. Spinal Cord Injuries: Anterior Cord Syndrome: Brown-Sequard’s Syndome: Cauda Equina Injuries: An incomplete lesion that results from compression and damage to the anterior part of the spinal cord. The MOI is cervical flexion. There is a loss of motor function and pain and temperature sense below the lesion due to damange of the corticospinal and spinothalamic tracts. Usually caused by a stab wound, which produces hemisection of the spinal cord. There is paralysis and loss of vibratory and postion sence on the ipsilateral side as the lesion due to the damage of the corticospinal tract and dorsal columns. There is a loss of pain and temp sense on the contralateral side of the lesion from damage to the lateral spinothalamic tract. Occurs below the L1 spinal level where the long nerve roots transcend. Can be complete, however they are frequently incomplete due to the large number of nerve roots in the area. A cauda equine injury is considerd a peripheral nerve injury. Characterics include flaccidity, arelexia, and impairment of bowel and bladder function. Full recovery Central Cord Syndome: Poserior Cord Syndrome: is not typical due to the distance needed for axonal regeneration. An imcomplte lesion that results from compression and damage of the central portion of the spinal cord. The MOI is usually cervical hyperextension that damages the spinothalamic t tract, corticospinal tract, and dorsal columns. The UEs present with greater involvement than the LEs, and greater motoer deficts exist as compared to sensory deficits. A relatively rare syndrome that is caued by compression of the posterior spinal artery and is characterized by a loss of pain perception, proprioception, two-point discrimination, and stereognosis. Motor function is preserved. Classification of Level of Injury: Motor level: determined by the most caudal key muscles that have muscle strength of 3 or greater with the superior segment tested as normal (5). Sensory level: determined by the most caudal dermatome with a normal score of 2/2 for pinprick and light touch. Terminology: Myelotomy: Neurectomy: Neurogenic bladder: Nonreflexive bladder: Paradoxical breathing: Paraplegia: A surgical procedure that severs certain tracts within the spinal cord in order to decrease spastic and improve function. A surgical removal of a segment of nerve in order to decrease spasticity and improve function. The bladder empties reflexively for a pt with an injury above the level of S2. The bladder is flaccid as a result of a cauda equine or conus medullaris lesion. Sacral reflex arc is damanged. A form of abnormal breathing that is common in tetraplegia where the abdomen rises and the chest is pulled inward during inspiration. On expiration the abdomen falls and the chest expands. Used to describe injuries that occur at the level of the thoracic, lumbar, or sacral spine. A physiologic response that occurs between 30 and 60 minutes after trauma to the spinal cord and can last up to several weeks. Describes injuries that occur at the level of the cervical spine. Spinal shock: Tetraplegia: Spinal Cord tests and measures: ASIA Impairment Scale A= B= C= D= E= Complete: no sensory or motor function is preserved in sacral segments S4-S5. Sensory Incomplete: Sensory but not motor function is preserved below the neurologic level and extends through sacral segments S4S5. Motor Incomplete: Motor function is preserved below the neurologic level, and most key muscles below the neurologic level have a muscle grade less than 3. Motor Incomplete: Motor function is preserved below the neurologic level, and most key muscles below have a muscle grade greater than or equal to 3. Normal: sensory and motor functions are normal. Traumatic Brain Injury: Types of brain injury: Open Injury: Closed Injury: Primary Injury: Secondary Injury: Direct penetration through the skull to the brain. Ex: gunshot wounds, knife, or shart objects, skull fx, direct trauma. Without penetration through the skull. Ex: Concussion, contusion, hematoma, hypoxia, drug overdose, near drowning, acceleration/deceleration injuries Initial injury to the brain sustained by impact. Ex: skull penetration, skull fx, and contusions. Coup lesion: a direct lesion of the brain under the point of impact. Contracoup lesion: results on the opposite side of the brain. Rebound effect of the brain after impact. Brain damage that occurs as a response to the initial injry. Ex: increase pressure, hypoxia, ischemia Levels of Consciousness: Coma: Stupor: Obtundity: Delirium: Clouding of consciousness: Consciousness: A state of unconsciousness and a level of unresponsiveness to all interal and external stimuli. A state of general unresponsiveness with arousal occurring from repeated stiumuli. A state of consciousness that is characterized by a state of sleep, reduced alertness to arousal, and delayed responses to stimuli. A state of consciousness that is characterized by disorientation, confusion, agitation, and loudness. A state of consciousness that is characterized by quiet behavior, confusion, poor attention, and delayed responses. A state of alertness, awareness, orientation, and memory. Traumatic Brain Injury Tests and Measures: Ranchos Los Amigos Levels of Cogntive Functioning: I. II. No response Generalized Response III. Localized Response IV. Confused-agitated V. Confused-inappropriate VI. Confused-appropriate Pt appears to be in a deep sleep and is completely unresponsive to any stimuli. Pt reacts inconsistently and non-purposefully to stimuli in a nonspecific manner. Responses are limited and often the same regardless of stimulus presented. Pt reacts specifically, but inconsistently to stimuli. Responses are directly related to the type of stimulus presented. May follow simple commands such as closing the eyes or squeezing the hand in an inconsistent, delayed manner. Pt is in a heightned state of activity. Behavior is bizarre and non-purposeful relative to the immediate behavior. Does not discriminate among persons or objects, is unable to cooperate directly with treatment effors. Verbalizations frequently are incoherent and/or inappropriate. Gross attention to environment is very brief. Pt lacks short and long term recall. Pt is able to respond to simple commands fairly consistently. However with increased complexity of commands or lack of any external structure, responses are non-purposeful, randome, or fragmented. Memory is severly impaired, inappropriate use of objects may perform previously learned taks with structure but is unable to learn new info. Pt shows goal-directed behavior, but is dependent on external input or direction. Follow simple directions consistently and shows carryover for relearned tasks such as self-care. Responses may be incorrect due to memory problems, but they are approparite to the situation. Past memories show VII. Automatic-appropriate VIII. Purposeful-appropriate more depth and detail than recent memory. Pt appears appropriate and oriented with the hospital and home setting. Goes through daily routine automatically, but frequently robot-like. Pt shows minimal to no confusion and has shallow recall of activities. Shows carryover for new learning, but a decreased rate. With structure is able to initiate social or recreational activityes, judgment remains impaired. Pt is able to recall and integrate past and recent events and is aware of and responsive to environment. Shows carryover for new learning and needs no supervision once tasks are learned. May continue to show a decreased ability relatively to premorbid abilities, abstract reasoning, tolerance for stress, and judgment in emergencies or unusually circumstances. Glasgow Coma Scale: Eye opening, Best motor response, Verbal response Severe brain injury/coma: 8 or less Moderate brain injury: 9-12 Mild brain injuries: 13-15 NM and Nervous System Patholody: Pathology Alzheimer’s Disease What is it A progressive neurodegenerative disorder that results in deterioration and irreversible damange within the cerebral cortex. Etiology Unknown, however hypothesized causes unclude lower levels of neurotransmitters, higher levels of aluminum within brain tissue, genetic inheritance, autoimmune disease. Risk of developing increases with age, higher incidence in women. Signs & Symptoms Difficulty with new learning and subtle changes in memory and concentration. Progression includes a loss of orientation, word finding difficulty, depression, poor judgment, rigidity, bradykinesia, shuffling gait, impaired ability to perform self-care skills. Later stages include Treatment There is no curative treatment for the disease process. Medications are administered to inhibit acetylcholinesterase, alleviate cognitive symptoms, and control behavioral changes. PT: should focus on maximizing pts remaining function and providing family and caregiver incontinence, functional dependence, and an inability to speak. Amyotrophic Lateral Sclerois (ALS) A chronic degenerative disease that produces both upper and lower motor neuron impairments. Produces weakness and muscle atrophy. The rapid degeneration causes denervation of muscle fibers, mustly atrophy, and weakness. Unknown. Theories include genetic inheritance, virus, metabolic disturbances, and toxicity of lead and aluminum. Higher incidence in men and beings ages 40-70. Bell’s Palsy A temporary unilateral facial paralysis secondary to trauma with demyelination and/or axonal degeneration of the facial nerve. This is a common clinical condition with the highest incidence in individuals between 1545 years of age. Unclear, however may be secondary to viral infection, specifically the herpes simplex/herpes zoster virus. Inflammation and subsequenet pressure injure the nerve with varying degress of damage. Diabetic Neuropathy A complication and direct Primary diagnosis is result Lower motor neuron signs include asymmetric muscle weakness, cramping, and atrophy within the hands. Weakness spreads in a distal to proximal path. Upper motor neuron symptoms can include spasticity, clonus, + Babinski. A pt with ALS will exhibit fatigue, oral motor impairment, motor paralysis, and eventual respiratory paralysis. Asymmetrical facial appearanace with “drooopoing” of the eyelid and mouth, potential for drooling, dryness of the eye, and inability to close the eyelid due to weakness. Weakness and sensory education. Many pts require a long term care secondary to personality changes, aggressive behavior, and end stage complications. Effective management of ALS is based on supportive care and symptomatic therapy. Pharmacological intervention may include riluzole. Physical, occupational, speech, respiratory, and nutritional therapies may be warranted with the focus on quality of life and caregiver training. The sooner the person is diagnosed and treated, the better the outcome. Some pts have very mild involvement and their symptoms typically resolve within 2 weeks with formal medical intervention. PT may be indicated for stimulation of the facial nerve, facial massage, and exercise. Pts require strict Epilepsy Guillain-Barre Syndrome effect of diabetes. Nerve ischemia results from microvascular disease combined with the direct effects of hyperglycemia on neurons resulting in the impairment of nerve function. of DM. Chronic condition where there is temporary dysfunction of the brain that results in hypersynchronus electrical discharge of cortical neurons and seizure activity that is typically unprovoked and unpredictable. A seizure is a transient even that is a symptom of interrupted brain functioning. A seizure is the hallmark sign of epilepsy, however, one seizure does not signal epilepsy. Acute polyneuropathy, that is a temporary inflammation and Various classifications of seizures, many cases are idiopathic. Other associated conditions: genetic influence, head trauma, dementia, CVA, cerebral palsy, down syndrome, and autism. Unknown, however, it is hypothesized to be an autoimmune response to a disturbances occur distally in a symmetrical pattern. Initial symptoms include tingling, numbness or pain, especially in the feet. Additional symptoms may include wasing of muscles in the feet or hands “stocking glove” sensory distribution imparitmens, orthostatic hypotension, weakness, urinary impairments, and significant pain. Seizure symptoms vary, depending on type and extent. Loss of awareness or consciousness and disturbances of movement, sensation, mood or mental function may occur. -Stay calm & prevent injury -Remove all objects that could cause harm -Do not restrain -Avoid placing anything in pts mouth -Call 911 if seizure lasts longer than 5 minutes Motor weakness in a distal to proximal progression, sensory impairment, and monitoring of blood glucose levels to prevent further nerve pathology. PT is typically indicated to address the various symptoms including pain management, foot care, and overall fitness. Antiepileptic medication to manage seizures. No cure. Typically requires hospitalization for treatment of symptoms. demyelination of the peripheral nerves’ myelin sheaths, potentially resulting in axonal degeneration. The autoantibodies of GBS attack segments of the myelin sheath of the peripheral nerves. Can occur at any age, however there is a peak in frequency in young adult population and again in adults between their 5th and 8th decades. previous respiratory infection, influenze, immunization or surgery. Viral infections, EpsteinBarr syndrome, cytomegalovirus, bacterial infections, surgery, and vaccinations. Huntington’s Disease (chorea) Is a neurological disorder of the CNS and is characterized by degeneration and atrophy of the basal ganglia and cerebral cortex within the brain. The neurotransmitters become deficient and are unable to modulate movement. Is genetically transmitted as an autosomal dominant trait with the defect linked to chromosome 4 and to the gene identified as IT15. The disease is usually perpetuated by a person that has children prior to diagnosis. The average age for developing symptoms is between 35-55 years, however can develop at any age. Multiple Sclerosis Produces patches of demyelination of the myelin sheaths that surround nerves within Genetics, viral infections, and environment all have a role in the development of MS. MS can oocur at possible respiratory paralysis. Will initially present with distal symmetrical motor weakness, mild distal sensory impairments, and transient paresthesias that progress towards the upper extremities and head. Level of disability peaks within 2-4 weeks after onset. Muscle and respiratory paralysis, inability to speak or swallow may also occur. Can be life threatening. HD is a movement disorder that included affective dysfunction and cognitive impairment. The pt may present with involuntary choeric movements, mild alteration in personality, grimacing, protrusion of the tongue, and ataxia with choreoathetoid movements. Late stage HD includes mental immobility, and rigidity. Vary based on the type. Initial symptoms include visual problems, paresthesias and sensory Cardiac monitoring and mechanical ventilation may be required. PT may include pulmonary rehab, strengthening, mobility training, wheelchair and orthotic prescription, AD training. Medical management requires genetic, psychological, and social counceling for the pt and family. Pharmacological mangt is initiated once choreiform movement impairs a pts functional capacity. PT should maximize endurance, strength, balance, postural control, and functional mobility. Pharmacoligcal, medical, and therapeutic interventions. The goal is to lessen the length of the brain and spinal cord. This decreases the efficiency of nerve impulse transmission and symptoms will vary based on the location and the extent of demyelination. There is subsequent plaque development and eventual failure of impulse transmission. any age with the highest incidence between 20-35 years of age. Myasthenia Gravis Autoimmune disease resulting in neuromuscular junction pathology. There is a defect specifically in the transmisstion of nerve impulses to the muscles at the NM junction. Antibodies block or destroy the receptors that are needed for acetylcholine uptake and this prevents muscle contraction. Autoiummune disease process that also has an association with an enlarged thyms. There is also an associated with DM, RA, lupus and other immune disorders. There are multiple forms of gravis that range from mild to severe involvement. Parkinsons’ Disease Primary degenerative disorder and is characterized by a decrease in production of dopamine Unknown. Contributing factors that can produce symptoms include genetic defect, toxicity from carbon monoxide, changes, clumsiness, weakness, ataxia, balance dysfunction, and fatigue. The clinical course usually consists of periods of exacerbations and remissions, with the degree of neurologic dysfunction. exacerbations and maximize the health of the pt. Pharmacological intervention is indicated along with physical, occupational, and speech therapies throughout the disease process. PT includes regulation of activity level, relaxation and energy conservation techniques, normalization of tone, balance and gait training, core stabilization, and AD training. The cardinal signs include Myasthenia gravic “crisis” extreme fatiguability and is a medical emergency skeletal muscle weakness where there is an that can fluctuate within exacerbation that includes minutes or over an the respiratory muscles extened period. The ocular and requires a ventilator. muscles are typically PT will focus on obtaining affected first and approx. a respiratory baseline and half of the pts experience pulmonary intervention as ptosis and diplopia, needed. Energy Dysphagia, dysarthria, and conservation and cranial nerve weakness are strengthening using also common. isometric contractions are appropriate for most pts. A resting tremor in the Relies heavily on hands (sometimes called pharmacolocial pill rolling tremor), or feet intervention. Dopamine that increases with stress replacement therapy is and disappears with most effective in reducing Post-polio Syndrome (neurotransmitter) within the corpus striatum of the basal ganglia. The basal ganglia stores the majority of dopamine and is responsible for modulation and control of voluntary movement. excessive copper, encephalitis, and other neurodegenerative diseases such as HD or Alzheimer’s. The majority of pts are between 50 and 79. A viral infection resulting in neuropathy that includes focal and asymmetrical motor impairments. This virus was all but eradicated in the 1960s with the development of a vaccine. Post-polio is a LMN A previous diagnosis of polio is essential to diagnose PPS. Approx 2550% of persons with polio experience PPS decades after their initial recovery (interval approx 25 years) movement or sleep. Early symptoms: balance disturbances, difficuly rolling over and rising from bed, and impairment with fine manipulataive movements seen in writing, bathing and dressing. Progression of the disease includes hypokinesia. Sluggish movement, difficulty with initiating and stopping movement, festinating and shuffling gait, bradykinesia, poor posture, cogwheel and lead pipe rigidity of skeletal muscles. Pts may also experience freezing during ambulatin, speech, blinking, and movements of the arms. Mask like appearance with no expression. Commonly there is slow and progressive weakness, fatigue, muscle atrophy, pain, and swallowing issues. movement disorders, rigidity and tremor. PT should include maximizing endurance, strength, and functional mobility. Verbal cueing and visual feedback are also effective tools to use with this population. No pharmacological intervention to alter the progression of PPS. Emphasis of treatment surrounds lifestyle modification and symptomatic intervention. PT should emphasize supervised exercise, pathology that affects the functional independence, anterior horn cells of adaptive equipment, and those previously affected education to assit pts to with polio. Surviving axons maintain as much were originally able to independence as possible. increase the size of ther innervation ratio to assist denervated muscle. PPS occurs when the compensated reinnervation fails and results in ongoing muscle denervation. Peripheral nerve lesions: A lesion of the nerve can occur through many MOIs. Ex. Compression, fx, compartment syndrome Double crush syndrome: Mononeuropathy: Neuroma: Peripheral neuropathy: Polyneuropathy: Wallerian degeneration: Existence of two separate lesions along the same nerve that create more severe symptoms that in only one lesion existed. An isolated nerve lesion, associated condtions include trauma and entrapment Abnormal growth of nerve cells; associated conditions include vasculitis, AIDS, entrapment Impairment or dysfunction of the peripheral nerves; associated conditions include diabetic peripheral neuropathy, trauma, alcoholism Diffuse nerve dysfunction that is symmetrical and typically secondary to pathology and not trauma, associated conditions include GBS, peripheral neuropathy, use of neurotoxic drugs, and HIV Degeneration that occurs distally, specifically to the myelin sheath and axon. Classification of Acute Nerve Injuries: Neurapraxia: (Class I) -Mildest form of injury -conduction block usually due to myelin dysfunction -Axonal continuity preserved -Nerve conduction is preserved -Nerve fibers are not damaged -Symptoms include pain, minimal muscle atrophy, numbness or greater loss of motor and sensory function, diminished proprioception Axonotmesis: (Class II) Neurotmesis: (Class III) -Recovery is rapid and complete and will occur within 4-6 weeks -Pressure injuries are the most common -A more severe grade of injury to a peripheral nerve -Reversible injury to damaged fibers since they maintain an anatomical relationship to each other -Damage occurs to the axons with preservation of the endoneurium, epineurium, Schwann cells, and supporting structures -Distal Wallerian degeneration can occur -The nerve can regenerate distal to the site of the lesion at rate of 1mm per day -Recovery is spontaneous and varies from spotty to no recovery; surgery may be required for repair -Traction, compression, and crush injuries are most common -The most severe grade of injury to a peripheral nerve -Axon, myelin, connective tissue components are all damaged or transected -Irreversible injury, no possibility of regeneration -Flaccid paralysis and wasting of muscles occur, total loss of sensation to area supplied by the nerve -All motor and sensory loss distal to the lesion becomes permantely impaired -No spontaneous recovery ; with surgical reattachment potential regenerating axons may grow at 1 mm per day -Complete transaction of the nerve trunk Pediatrics & Development Concepts of Development Cephalic to Caudal: Gross to fine: Mass to specific: Proximal to distal: A person develops head and UE control prior to trunk and LE control. There is a general skill acquisition from the direction of head to toe. A general trend for large muscle movement acquisition with progression to small muscle skill acquisition. A general trend for a person to acquire simple movements and progress towards complex movements. A concept that uses the midline of the body as the reference point. Trunk control (midline stability) is acquired first with subsequent gain in distal control (extremities). Infant Reflexes and Possible Effects if Reflex Persists Abnormally: Reflex: Normal: Interferes with: Asymmetrical Tonic Neck Reflex (ATNR) Stimulus: Head position Response: Arm & leg on face side are extended, arm & leg on skull side are flexed with convexity toward face side Normal age of response: Birth to 6 months Symmetrical Tonic Neck Reflex (STNR) Stimulus: Head position, flexion or extension Response: When head is in flexion, arms are flexed legs extended. When head is in extension, arms are extended, legs are flexed. Normal age of response: 6-8 months Tonic Labyrinthine Reflex (TLR) Stimulus: Position of labyrinth in inner ear— reflected in head position Response: in the supine position, body and extremities are held in extension; in the prone position, body and extremities are held in flexion Normal age of response: Birth to 6 months Stimulus: Touch to skin along spine from shoulder to hip Response: Lateral flexion of trunk to side of stiumuls Normal age of response: 30 weeks of gestation to 2 months Stimulus:Pressure in palm on ulnar side of hand Response: Flexion of fingers causing a strong grip Normal age of response: Birth to 4 months Stimulus: Pressure to base of toes Galant Reflex Palmar grasp reflex Plantar grasp reflex -Feeding -Visual tracking -Midline use of hands -Billateral hand use -Rolling -Development of crawling -Can lead to skeletal deformities (scoliosis, hip subluxation, hip dislocation) -Ability to prop on arms in prone position -Attaining and maintaining hands and knees position -Crawling reciprocally -Sitting balance when looking around -Use of hands when looking at object in hands in sitting position -Ability to initiate rolling -Ability to prop on elbows with extended hips when prone -Ability to flex trunk and hips to come to sitting position from supine position -Often causes full body extension, which interferes with balance in sitting or standing -Development of sitting balance -Can lead to scoliosis -Ability to grasp and release objects voluntarily -Weight bearing on open hand for propping, crawling, protective responses -Ability to stand with feet flat on surface Rooting reflex Moro reflex Startle reflex Positive support reflex Walking (stepping) reflex Response: Toe flexion Normal age of response: 28 weeks gestation to 9 months Stimulus: Touch on cheek Response: turning head to same side with mouth open Normal age of response: 28 weeks gestation to 3 months Stimulus: Head dropping into extension suddenly for a few inches Response: Arms abduct with fingers open, then cross trunk into adduction, cry Normal age of response: 28 weeks gestation to 5 months Stimulus: Loud, sudden noise Response: similar to Moro response, but elbows remain flexed and hands closed Normal age of response: 28 weeks gestation to 5 months Stimulus: Weight placed on balls of feet when upright Response: Stiffening of legs and trunk into extension Normal age of response: 35 weeks of gestation to 2 months Stimulus: Supported upright position with soles of feet on firm surface Response: Reciprocal flexion/extension of legs Normal age of response: 38 weeks of gestation to 2 months -Balance reactions and weight shifting in standing -Oral-motor development -Development of midline control of head -Optical righting, visual tracking, and social interaction -Balance reactions in sitting -Protective responses in sitting -Eye-hand coordination, visual tracking -Sitting balance -Protective responses in sitting -Eye-hand coordination -Social interaction, attention -Standing and walking -Balance reactions and weight shift in standing -Can lead to contractures of ankles into PF -Standing and walking -Balance reactions and weight shifting in standing -Development of smooth, coordinated reciprocal movements of lower extremities Developmental Gross & Fine Motor Skills: Age Gross motor skills Fine motor skills Newborn to 1 month: 2-3 months 4-5 months 6-7 months 8-9 months Prone: physiological flexion, lifts head briefly, head to side Supine: physiological flexion, rolls partly to side Sitting: head lag in pull to sit Standing: Reflex standing and walking Prone: Lifts head 90° briefly, chest up in prone position with some weight through forearms, rolls prone to supine Supine: ATNR influence is strong, legs kick reciprocally, prefers head to side Sitting: Head upright, but bopping, variable head lag in pull to sitting position, needs full support to sit Standing: poor weight bearing, hips in flexion, behind shoulders Prone: Bears weight on extended arms, pivots in prone to reach toys Supine: Rolls from supine to side position, plays with feet in mouth Sitting: head steady in supported sitting position, turns head in sitting position, sits alone for brief periods Standing: bears all weight through legs in supported standing Prone: Rolls from supine to prone, holds weight on one hand to reach for toy Supine: Lifts head Sitting: Lifts head and helps when pulled to sitting position, gets to sitting position without assistance, sits independently Mobility: may crawl backward Prone: gets into hands-knees position Supine: does not tolerate supine position -Regards objects in direct line of sight -Follows moving onject to midline -Hands fisted -Arm movements jerky -Movements may be purposeful or random -Can see farther distances -Hands open more -Visually follows through 180° -Grasp is reflexive -Uses palmar grasp -Grasps and releases toys -Uses ulnar-palmar grasp -Approaches objects with one hand -Arm in neutral when approaching toy -Radial-palmar grasp “rakes” with fingers to pick up small objects -Voluntary release to transfer onjects between hands -Develops active supination -Uses inferior pincer grasp 10-11 months 12-15 months 16-24 months 2 years Sitting: moves from sitting to prone position, sits without hand support, pivots Standing: stands at furniture Mobility: crawls forward, walks along furniture (cruising) Standing: stands without support briefly, picks up object from floor Mobility: walks with both hands held, walks with one hand held, bear walk -Walks without support -Fast walking -Walks backward, sideways -Bends to look between legs -Creeps or hitches upstairs -Squats in play -kicks ball -Throws ball -Extends wrist actively -Points with index finger -Rides tricycle -Walks backward -Walks on tiptoe -Runs on toes -Hops on one foot -Turns knob -Opens and closes jar -12-15 piece puzzle -Fine pincer grasp developed -Marks paper with crayon -Builds tower -Folds paper -Strings beads -Holds crayon with thumb and fingers NM and Nervous Systems Pediatric Pathology Pathology Cerebral Palsy (CP) What is it Is an umbrealla term used to describe movement disorders due to brain damage that are nonprogressive and are acquired in utero, during birth or infancy. The brain Etiology CP can occur before or during birth secondary to a lack of oxygen, maternal infections, drug or alcohol abuse, placental abnormalities, toxemia, prolonged labor, Signs & Symptoms Spastic-indicating a lesion in the motor cortex of the cerebrum; upper motor neuron damage Athetoid-indicating a lesion involving the basal ganglia; cerebellum and Treatment Tx of CP is a life long process. Intervention includes ongoing family and caregiver education, normalization fo tone, stretching, strengthening, motor learning and damage decreases the brain’s abilility to monitor and control nerve and voluntary muscle activity. prematurity, and Rh imcompatibility. The etiology of acquired CP includes meningitis, CVA, seizures, and brain injury. Down Syndrome Is a genetic abnormality consisting of an extra 21 chromose, termed trisomy 21. Includes incomplete cell division of the 21st pair of chromosomes due to nondisjunction, translocation or mosaic classficiation. Advanced maternal age increases the risk of genetic imbalance. Duchenne Muscular Dystrophy Is a progressive disorder caused by the absence of the gene required to produce the musle proteins dystrophin and nebulin. Without dystrophin and nebulin, cell membranes weaken, myofibrils are destored, and muscle contractility is lost. Fat and connective The causative factor is inheritance as an X-linked recessive trait. The child’s mother is a silent carrier and only male offspring will manifest the disease. cerebellar pathways Distribution of Involvement: -Monoplegia-one extremity -Diplegia-bilateral LE involvement, however UE may be affected Hemiplegia-unilateral involvement of the upper and lower exremties Quadriplegia-involvment of the entire body Mental retardation, hypotonia, joint hypermobility, flattened nasal bridge, narrow eyelids with epicanthal folds, small mouth, feeding impairments, flat feet, scoliosis, congenital heart disease, and visiual and hearing loss. Characteristics usually manifest between 2-5 years of age. Progressive weakness, disinterest in running, falling, toe walking, excessive lordosis, and pseudohypertorphy of muscle groups (calves). Progressive impairment with ADLs and mobility developmental milestones, positioning, weight bearing activities, and mobility skills. Splinting, assistive devices, and specialized seating may be indicated. Surgical intervention may be required for orthopedic management or reduction of spasticity. Should emphasize exercise and fitness, stability, maximizing respiratory function, and education for caregivers. Surgical intervention may be indicated for cardiac abnormaities. Intervention focuses on family/caregiver education, respiratory function, submax exercise, mobility skills, splinting, orthotics, and adaptive equipment. Medical management includes the use of immunosuppressants, steroids, and surgical Spina Bifida tissue eventually replace muscle, and death usually occurs from cardiopulmonary failure prior to age 25, usually in the teenage years. Is a developmental abnormality due to insufficnet closure of the neural tube by the 28th day of gestation. Causative factors include: genetic predisposition, environmental influence, low levels of maternal folic acid, maternal hyperthermia, and certain classifications of drugs. Classifications of spinal bifida include: Spina bifida Occultaimpairment and nonfusion of the spinous processes of a vertebrae, however, the spinal cord and meninges remain intact. No associated disabilitiy. Spina bifida cystic-presents with a cyst like protrusion through the non-fused vertebrae, which results in impairment. 2 types of Cystica: 1. Meningoceleherniation of meninges and CSF into a sac that protrudes through begins around age 5 and the ability to ambulate slows. *Gower’s sign Proximal weakness first intervention for orthopedic impairments. Motor loss below the level of the defect, sensory deficits, hydrocephalus, Arnold-Chiari Type II malformation, osteoporosis, clubfoot, tethered cord syndrome, latex allergy, bowel and bladder dysfunction, and learning disabilities. PT emphasizes significant family teaching regarding positioning, handling, ROM, and therapeutic exercises. Skin care, strengthening, AD, splinting, wheelchair prescription. the vertebral defect. 2. 2. Myelomeningocel e-a severe form with herniation of meninges, CSF, and spinal cord extending through the defect in the vertebrae. Cyst may or may not be covered by skin. Neuromuscular Pathologies: Disease Alzheimer’s Disease Diagnosis Is a progressive neurological disorder that results in deterioration & irreversible damage within the cerebral cortex and subcortical areas of the brain. The loss of neurons results from the breakdown of several Contributing Factors Hyopthesized causes include lower levels of neurotransmi tterse, higher levels of aluminum within brain tissue, genetic inheritance, autoimmune disease, abnormal processing of Clinical Presentation Initially noted by a change in higher cortical functions characterized by subtle changes in memory, impaired concentration , and difficulty with new learning. During the middle stages, pt will Lab/Imaging Alzheimer’s disease presently cannot be confirmed until a postmortem biopsy revels the neurofibrillary tangles and amyloid plaques. MRI can be used to assess any abnormalities Management/Out come Drug therapies are usually short term in effect lasting 69 months. PT should focus on maximizing the pts remaining function and providing family and caregiver education. The therapist should attempt to create an emotional & physical environment that Amyotrophic Lateral processes that would normally sustain the brain cells. the substance amyloid, and virus. The risk of developing ↑ with age and a higher incidence in women. develop behavioral and motor problems such as aphasia, apraxia, perseveration, agitation and violent or socially unacceptable behavior that can include wandering. Eventually all ability to learn is lost and long-term memory also disappears. or signs of atrophy within the brain that is associated with Alzheimer’s disease or to rule out other medical conditions. Is a chronic degenerative Exact etiology Both upper and lower There are multiple tests provides the pt with the opportunity to experience success. Safety with functional mobility and gait training may be indicated in the early stages. Many pts require a long term care facility due to personality changes, aggressive behavior, and endstage complications. This is a chronic and progressive disorder and is the 4th leading cause of death of adults. The typical course of the disease averages between 7-11 years. The leading cause of death of a pt with Alzheimer’s disease is infection or dehydration. Management is based on Sclerosis (ALS) disease that produces both upper and lower motor neuron impairments. Demyelination, axonal swelling, & atrophy within the cerebral cortex, premotor areas, sensory cortex, and temporal cortex cause the symptoms of ALS. unknown, theories of causative factors that include genetic inheritance as an autosomal dominant trait, a slow acting virus, metabolic disturbances, and theories of toxicity of lead & aluminum. Familial ALS occurs in 510% of all cases. Risk for ALS is higher in men & usually occurs between 4070 years of age. motor neuron involvement. Lower motor neuron signs include asymmetric muscle weakness, cramping, and atrophy that are usually found within the hands. Muscle weakness due to denervation eventually causes significant fasiculations, atrophy, and wasting of the muscles. The weakness spreads throughout the body over the course of the disease and generally follows a distal to proximal used to assist with diagnosing ALS. Electromyogra phy assesses fibrillation and muscle fasciculations. Muscle biopsy verifies LMN involvement rather than muscle disease and a spinal tap may reveal a higher protein content in some pts with ALS. supportive care and symptomatic therapy. PT should focus on quality of life, low level exercise, ROM, mobility training, assistive/adaptive devices, wheelchair prescription, bronchial hygiene, and energy conservation techniques. ALS is usually a rapidly progressing neurological disease with an average course of 2-5 years with 2030% surviving longer than 5 years. Death usually occurs from respiratory failure. path. Upper motor neuron symptoms occur due to the loss of inhibition of the muscle. Incoordinatio n of movement, spasticity, colnus, and a positive Babinski reflex are some of the indicators of UMN involvement. Bulbar involvement is characterized by dysarthria, dysphagia, and emotional lability. A pt will ALS will exhibit fatigue, oral motor impairment, fasciulations, spasticity, Central Cord Syndrome (CCS) Is an incomplete SCI that most often results from a cervical hyperextension injury. Symptoms are secondary to damage to the central aspect of the spinal cord. CCS usually occurs from a fall but can occur from other forms of trauma such as MVA. Most common MOI is a hyperextensi on injury of the cervical spine. Other potential contributing factors in the development of CCS include cervical spondylosis, narrowing or congenital defect of the spinal canal, tumor rheumatoid arthritis or syringomyeli a. CCS predominatel y affects the population over 50 and greater motor paralysis, & eventual respiratory paralysis. CCS presents with motor loss that is greater in the UEs than in the LEs and is most severe distally in the UEs. This presentation is due to the damage that occurs within the central location of the spinal cord. Sensory loss found below the level of the lesion is usually limited, but can be variable. Sacral segments are usually unaffected. MRI is used to assess spinal cord impingement form bone or disk. CT scan of the spine will assess spinal canal compromise and the degree of impingement. X-rays can be utilized to assess potential fractures, dislocations, and degree of spondylotic deterioration. Rehab is initiated once the pt is medically stable. PT intervention should include pt and caregiver education, ROM, strengthening, endurance, balance, proximal stabilization ex, and functional mobility based on current function. If a pt ambulates, a platform attachment walker may be initially indicated since hand function is usually poor for grasp. Surgical intervention is rare. CCS is the most common incomplete SCI and accounts for ~30% of overall tetraplegia. incidence in men. Cerebral Palsy Is an umbrealla term used to describe a group of nonprogressive movement disorders that result from brain damage. Most common cause of permanent disability in children. Multifactorial & sometimes unknown. Risk factors are categorized as prenatal (80%), or perinatal and postnatal (20%). Factors can include maternal malnutrion, hypothyroidis m, infection, diabetes, and chromosome abnormalities . Perinatal factors include multiple or premature births, breech Bowel & bladder functions resolve in 5585% of pts with CCS after 6 months. CP is a NM disorder of posture and controlled movement. A child may present with high tone, low tone, or athetoid movement. CP is classified as monoplegia (one involved extremity), hemiplegia (unilateral involvement of the upper and lower extremities), and quadriplegia (all extremities). General characteristics Statistics indicated 77% of pts with CCS will ambulate. Older pts do not recover as well as younger ones. If CP is suspected through clinical findings, including seizures, an electroenceph alography (EEG) may be performed. Xray of the hp may rule out hip dislocation; blood and urine tests can be sued to investigate a metabolic cause of CP. Observation usually will diagnose CP secondary to the observed outward Life long team approach. PT for CP often uses neurodevelopmen tal treatment and sensory integration techniques. Treatment should include normalization of tone, family education, developmental milestones, positioning, stretching, strengthening, balance, mobility, specialized wheelchair seating and orthotic prescription. If a pt is going to ambulate, this will usually occur by the age of 8. CP is delivery, low birth weight, prolapsed cord. Post natal include CVA, head trauma, infection and brain tumor. The most common cause of CP is prenatal cerebral hypoxia. Down Syndrome (DS) (Trisomy 21) occurs when there is an error in cell division either through nondisjunction (95%), translocation (4%), or mosaicism (1%) and the cell nucleus results in 47 chromosomes. include motor delays, abnormal muscle tone, poor postural control, reflex abnormalities, high risk for hip dislocations, and perceptual skills. Pt may also have mental retardation (50-60%), hearing impairments, constipation. Some DS is the most theories common suggest than cause of MR. an increase in Pt will present maternal age with (and age of hypotonia, the oocyte) flattened may cause nasal bridge, predispositio almondn to errors in shaped eyes, meiosis. abnormally Environment shaped ears. al factors Simian line such as virus, (palmar characteristics . a non-progressive but permanent condition. Prognosis for mild to moderate CP is a near normal lifespan. 50% of children with severe CP die by the age of 10. During pregnancy a female can be tested for Alphafetoprotein, human chorionic gonadotropin, and unconjugated estrogen levels (the triple screen). Team approach that requires life long intervention. PT intervention play a role in developmental delay, hypotonia, laxity of ligaments, and poor strength are key areas of tx. Positioning and handling are key components in order to maximize paternal age, medical exposure, reproductive medications, and intrinsic predispositio ns have been associated with DS. crease), epicanthal folds, enlargement of the tongue, congenital heart disease, developmenta l delay, and a variety of MS disorders. Three diagnostic studies include chorionic villsu sampling, amniocentesis or percutaneous umbilical blood sampling. Detection of DS occurs in ~60-70% in the women tested that are carrying a baby with DS. After birth a chromosome analysis called a karyotype can be performed to confirm the suspected diagnosis. Pt will have AA (atlantoaxial) instability, sensory, hearing and proper alignment and to minimize pathological reflexes, malalignment, and instability. Individual with DS today have a longer life expectancy secondary to advances in medical care, however, it is still less than standard. Approx 80% reach the age of 55. Duchenne Muscular Dystrophy (DMD) Is a progressive NM degenerative disorder than manifests symptoms once fat and connective tissue being to replace muscle that has been destroyed by the disease process. The mutation of the dystrophin gene causes the symptoms of DMD. Inheritance as an X-linked recessive trait. The mother is the silent carrier of this disorder. Since it is a recessive trait, only male offspring will manifest the disorder while female offspring become carriers. Diagnosis occurs between 2-5 years of age of only males. The first symptoms include waddling gait, proximal muscle weakness, clumsiness, toe walking, excessive lordosis, pseudohypert rophy of the calf and other muscle groups, and difficulty climbing stairs. DMD primarily affects the shoulder girdle musculature, pects, delts, rectus abdominis, visual impairments. Electromyogra phy is used to examine the electrical activity within the muscles. A muscle biopsy can be performed to determine the absence of dystrophin and evaluate the muscle fiber size. DNA analysis and high serum creatinine kinase levels n the blood also assist with confirming the diagnosis. Treatment focuses on maintaining function of the unaffected musculature for as long as possible. PT is initially indicated to assist a young child with progression through the developmental milestones. PT should focus on maintaining available strength, encouraging mobility, adapting to the loss of function. And promoting family involvement in a home program. MMT and ROM should be evaluated on a consistent basis to determine the pattern and rate of disability. Orthotics, Ads, and wheelchair Erb’s Palsy A term used to denote an upper brachial plexus injury or palsy that usually results from a difficult birth. One side of the baby’s neck is stretched which damages the nerves. If the gluteals, hamstrings, and calves. Pt initially has difficulty getting off the floor, needing to use the Gowers’ maneuver. Approx 1/3 of pts have some form of learning disability secondary to the dystrophin abnormalities. There is usually rapid progression of this disease with the inability to ambulate by 10-12 years. There are 4 types of brachial plexus injuries: avulsion, rupture, prescription are areas that will require attention. Respiratory care will also become a vital part. DMD is a progressive disorder and progresses rapidly. Death occurs primarily from cardiopulmonary complications. Death usually takes place by the time a pt is a teenager or less frequently into their 20s. An x-ray or MRI may be performed to see if there is any damage to the bones and joints of PT is recommened for a pt with Erb’s palsy with focuses on increasing active & passive movement and promoting use to This type of injury is the most common palsy related to the brachial plexus. It primarly affects the muscles of the shoulder and elbow. The muscles affected are those supplied by cervical roots C5 & C6; axillary, lateral pectoral, upper and lower subscapular, suprascapular, and partial paralysis of the long thoracic and musculocutaneo us nerves. The result is loss of rotator cuff, deltoid, brachialis, coracobrachials, and biceps. upper nerves are affected the condition is termed Erb’s palsy. One theory suggests that congenital chicken pox or amniotic bands may also produce this condition. When it occurs in adults, the cause typically is an injury that has caused stretching, tearing, or other trauma to the upper brachial plexus network. The chance of an infant having a brachial plexus palsy is equally distributed neuroma, and neurapraxia, The clinical presentation is a flaccid paralysis that is nicknamed the “Waiter’s tip deformity” characterized by a loss of shoulder function, loss of elbow flexion, forearm pronation, and the hand positioned in a pinch grip manner. the neck and shoulder. The physician may also use an EMG or nerve conduction studies to see if any nerve signals are present. the weak UE for functional activities. If a pt has spontaneous recovery of active movements within 3-4 months, the caregivers are given a home program. If conservative tx fails, surgery is indicated. Surgery will not restore normal function. After surgery, the infant will wear a splint for ~3-4 weeks. Caregiver education is very important regarding positioning and handling to avoid further traction. Approx. 9 out of 10 infants with brachial plexus palsy can recover with conservative treatment. Since nerves grow at a rate of 1 inch per month, it may according to gender, gestational age, and race. Guillain-Barre Syndrome (GBS) Or acute polyneuropathy is a temporary inflammation and demyelinaton of the peripheral nerves’ myelin sheaths, potentially resulting in axonal degeneration. GBS results in motor weakness and in a distal to proximal progression, sensory impairment, and possible respiratory paralysis. Unknown, however it is hypothesized to be an autoimmune response to a previous respiratory infection, influenza, immunization , or surgery. Viral infections, cytomegalovi rus, bacterial infections, surgery and vaccinations have been associated with the development of GBS. Can occur at any age, there is a peak in frequency in the young adult population and again in adults that are between their 5th and 8th decades. Incidence is slightly greater in males than females and in Caucasians than African Americans. Pt will initially present with distal symmetrical weakness and will experience GBS can be diagnosed through a cerebrospinal fluid sample that contains high protein levels and little to no lymphocytes. Electromyogra phy will result in abnormal and slowed nerve conduction. take several months or even years for nerves repaired at the cervical spine to reach the muscles of the hand. May require hospitalization for treatment of symptoms. A tracheostomy may be performed for ventilation. PT should be initiated upon admission to the hospital with focus on PROM, positioning, and light exercise. During the acute stage a therapist must limit over exertion and fatigue to avoid exacerbation of symptoms. As the pt progresses, intervention may include orthotic, wheelchair or AD prescription, family teaching, gait training. The sensory impairments & transient paresthesias. The weakness will progress towards the upper extremities and head. The level of disability usually peaks within 2 to 4 weeks after onset. Muscle & respiratory paralysis, absence of DTRs. GBS can be life threatening if there is respiratory involvement. Huntington’s Disease (HD) AKA Huntington’s Chorea, is a neurological disorder of the CNS and is HD is genetically transmitted as an autosomal dominant The average age for developing symptoms ranges between 35 & MRI or CT scan may indicate atrophy or abnormalities within the pool may be indicated to initiate movement without the effects of gravity. PT may assist with recovery, but it can’t alter the course of the disease. PT may be required on an ongoing basis to assist w recover that can last from 3-12 months. Recover is slow and can last up to 2 years after onset. Although most pts experience full recovery, statistics indicated that 20% have remaining neurologic deficits and 3-5% die from respiratory complications. PT should maximize endurance, strength, balance, postural control, and functional characterized by degerneration & atrophy of the basal ganglia (specifically the striatum) and cerebral cortex within the brain. trait with the defect linked to chromosome four and to the gene identified as IT-15. The disease is usually perpetuated by a person that has children prior to the normal onset of symptoms & without knowledge that he/she possesses the defective gene. Genetic testing is able to identify the defective gene for HD prior to the onset of symptoms. 55. HD is a disease that produces a movement disorder, affective dysfunction, and cognitive impairment. Pt will initially present with involuntary choreic movements and a mild alteration in personality. Unintentional facial expressions such as a grimace, protrusion of the tongue, and elevation of the eyebrows are common. As the disease progresses gait will become ataxic and a pt experiences cerebral cortex as well as the basal ganglia. PET may be used to augment other testing and obtain info regarding blood flow, oxygen uptake, and metabolism of the brain. A DNA marker sutyd may be administered to determine if the autosomal dominant trait is present for HD. mobility. Pt education should include prone lying, stretching, prevention of deformity and contracture, and safety with mobility. As the disease progresses the degree of dementia will influence treatment and goals. HD is a chronic progressive genetic disorder that is fatal within 15-20 years after clinical manifestation. Late stages of the disease result in total physical and mental incapacitation. The pt usually requires an extended care facility due to the burden of care & physical, cognitive, and emotional Multiple Sclerosis MS produces patches of demyelination that decreases the efficiency of nerve impulse transmission. Symptoms vary Genetics, viral infections, and environment all have a role in the development choreoathetoi d movement of the extremities and trunk. Speech disturbances & mental deterioration are common. Late stage HD is characterized by a ↓ in IQ, dementia, depression, dysphagia, incontinence, inability to ambulate or transfer, and progression from choreiform movements to rigidity. Differs by geographic area, sex, and race. MS can be classified as relapsingremitting (85%), dysfunction. There is not a single testing procedure to diagnose MS early in the disease. MRI may assist with The goal of medical treatment is to lessen the length of exacerbations and maximize the health of the pt. PT includes based on the location & extent of demyelination of MS. It is theorized that a slow acting virus initiates the autoimmune response in individuals that have environment al and genetic factors of the disease. The incidence of MS is higher in Caucasians between 20 & 35 years and is nearly twice as common in women as in men. There is also a higher incidence of MS in temperate climates. secondary progressive, primary progressive, or progressive relapsing. Initial symptoms include visual problems, paresthesias, and sensory changes, clumsiness, weakness, ataxia, balance dysfunction, and fatigue. observation and establishing a baseline for lesions, evoked potentials may demonstrate slowed nerve conduction, and cerebrospinal fluid can be analyzed for an elevated concentration of gamma globulin and protein levels. regulation of activity level, relaxation and energy conservation techniques, normalization of tone, balance activities, gait training, core stabilization, & adaptive/assistive device training. Pt and caregiver education regarding safety, energy conservation, patterns of fatigue, and the use of AD is vital to the quality of life. Exercise in the morning when the pt is rested and to avoid fatigue. Factors that influence exacerbations include heat, stress, infection, trauma, and pregnancy. Most pts live with MS Parkinson’s Disease This syndrome occurs as a secondary effect or disorder from another disease process. Parkinsons’ Contributing factors that can produce symptoms of Parkinson’s include genetic The risk for developing increases with age, 1:100 are affected over the age of 75. Majority of There are no laboratory or imaging studies that initially diagnose Parkinson’s. for many years and die from secondary complications such as disuse atrophy, pressure sores, contractures, fractures, renal infection, and pneumonia. If left untreated 50% of pts will require a w/c within 15 years post diagnosis. Overall mortality rate and long-term outcome correlates to age at diagnosis, number of attacks & exacerbations, frequency & duration of remissions & type of MS The medical management of Parkinson’s disease relies heavily on pharmacological intervention. disease is a primary degenerative disorder and is a characterized by a decrease in production of dopamine (neurotransmitt er) within the corpus striatum portion of the basal ganglia. The degeneration bof the dopaminergic pathways creates an imbalance between dopamine and acetylcholie. This produces the symptoms of Parkinsons’s. defect, toxicity from carbon monoxide, excessive manganese or copper, carbon disulfide, vascular impairment of the striatum, encephalitis, and other neurodegene rative diseases such as Huntington’s disease or Alzheimer’s disease. pts are between 5079 years. Initially pts will notice a resting tremor in the hands (pill rolling) or feet that increases with stress and disappears with movement or sleep. Early in the disease process a pt may attribute symptoms to “old age” such as balance disturbances, difficulty rolling over and rising from bed, and impairment with fine manipulative movements seen in writing, bathing, & dressing. A CT scan or MRI may be used to rule out other neurodegener ative disease and obtain a baseline for future comparison. Dopamine replacement therapy (Levadopa, Siinemet, Madopar) is the most effective treatment in reducing symptoms. PT should include maximizing endurance, strength, and functional mobility. Verbal cueing and oral/visual feedback are effective tools to use with this population. PT is recommened on an intermittent basis. Parkison’s disease does not significantly alter a pts lifespan if the pt is diagnosed with a generalized form between 5060 years. As the disease progresses, Spina BifidaIncomplete Myelomening fusion of the ocele posterior vertebral arch with both meninges and spinal cord pts symptoms slowly progress and often include hypokinesia, sluggish movement, difficulty with initiating (akinesia) and stopping movement. Festinating and shuffling gait, bradykinesia, poor posture, dysphagia, and “cogwheel” or “lead pipe” rigidity of skeletal muscles.Mask like with no facial expression. The incidence Impairments varies by associated socioeconomi include motor c status, and sensory geographic loss below the area, and vertebral ethnic defect, however, there will be an exacerbation of all symptoms and significant loss of mobility. The inactivity & Deconditioning allows for complications and eventual death. Prior to birth a fetal ultrasound may identify the myelomening ocele defect in Immediate surgical intervention to repair and close the defect and for placement of shunt to alleviate protruding outside the neural arch. Characterized by a sac or cyst that protrudes outside the spine. background. The overall incidence is declining due to improved prenatal care. Prenatal care including recommende d amounts of folic acid, especially in the first 6 weeks of pregnancy, appears to be the most effective way to prevent neural tube defects. hydrocephalu s, ArnoldChiari type II malformation, clubfoot, scoliosis, bowel & bladder dysfunction, and learning disabilities. The higher the lesion the worse the prognosis is for survival. In 90% of the cases a shunt is required for hydrocephalu s. Approx 2/3 of children with myelomening ocele and shunted hydrocephalu s have normal intelligence and the other third demonstrate only mild retardation. the spine. Prenatal testing of alphafetoprot ein (AFP)in the blood will show and elevation in levels that indicate a probably neural tube defect at approx. week 16 of gestation. At birth an obvious sac will be present over the spinal defect. hydrocephalus. PT is initiated immediately and focuses on family education regarding positioning, handling techniques, ROM, and therapeutic play. Long term PT attempts to maximize functional capacity, skin care, strength, blance, and mobility, w/c prescription, orthotics. A pt with myelomeningocle has a near normal life expectancy as long as the pt receives consistent and thorough health care. Functional outcome of the pt depends on the level of injury, the amount of associated impairments, and Spinal Cord Injury— Complete C7 Tetraplegia After injury, C7 is the most distal segment of the spinal cord that both the motor and sensory components remain intact. Motor Vehicle Accidents, violence & falls are the top causes. Higher ratio of injury in men (80%) and Caucasians. The highest incidence of occurs between 1530 years of age. Regardless of intelligence, children exhibit difficulties with perceptual abilities, attention, problem solving, and memory. Spinal shock which is the total depression of all nervous system function below the level of the lesion occurs immediately following injury and may last for days. Include flaccid paralysis and loss of all reflexes & sensation. Surgical intervention the caregiver support that is provided. X-rays of the cervical spine observe the positioning and damage of the involved vertebrae. The results of imaging determine subsequent medical intervention including stabilization of the spine. The acute phase begins at injury and includes medically stabilizing the pt. Inpatient rehab (typically 6-8 weeks) should initially focus on ROM, positioning in bed, and cough, clearance of secretions, bronchial drainage, and incentive spirometry. Compensatory techniques, strengthening, muscle substitution, and may be required after injury in order to stabilize the spinal cord through decompressio n and fusion at the site of injury. A Halo device is commonly used with cervical injuries to stabilize the spine. As sock subsides, a pt will experience an ↑ in muscle tone below the level. A pt with C7 tetraplegia will also present with impaired cough and ability to clear secretions, altered breathing pattern and the use of momentum and the head-hips relationship should be utilized during all activities. Ongoing intervention should include mat skills, selfROM, transfer skills, and community reintegration. Typical outcomes at this level include independence with feeding, grooming, and dressing, selfROM, independent manual wheelchair mobility, independent transfers, and independent driving with an adapted automobile. Independent living with adaptive poor endurance. Spinal Cord Injury— Complete L3 Paraplegia A pt sustains primary damage to the spinal cord and surrounding tissues at the L3 level through the disruption of the membrane, displacement or compression of the spinal cord, & subsequent hemorrhage and vascular damage. After a complete injury at this level, L3 is the most distal segment Motor Vehicle Accidents, violence & falls are the top causes. Higher ratio of injury in men (80%) and Caucasians. The highest incidence of occurs between 1530 years of age. Pts specifically with a complete lesion at the L3 level typically have a least partial innervation of the gracilis, iliopsoas, quadratus lumborum, rectus femoris, and Sartorius. Pts have full use of their UEs and have hip flexion, adduction, and knee The evaluation of a pt with an acute lumbar spine fracture should include routine lab tests, such as CBC, and electrolytes. X-rays, CT scan, and MRI allows for bony and ligamentous injury diagnosis. equipment is possible. The triceps, extensor pollicis longs and brevis, extrinsic finger extensors, and flexor carpi radialis will remain the lowest innervated muscles. Life expectancy over 45 years of age. Stabilization of the pts airway in order to secure adequate oxygenation. All pts with spinal cord injury should immediately receive intravenous methylprednisolo ne since it has proven to control the amount of secondary damage and improve the neurological outcome. The pt may be placed in a thoracolumbar orthosis (TLSO) of the spinal cord that both the motor and sensory components remain intact. extension. with restriction of activities or undergo stabilization surgery followed by the use of a TLSO. Orthotic prescription (KAFOs or AFOs) is recommended once the pt has gained strength to assist with ambulation using crutches. A pt with L3 SCI will usually participate in 4-8 weeks of inpatient rehab immediately after injury and stabilization. The pt should be able to function independently from a w/c level and ambulation level. Outcome is based on the degree of injury, the pts mental capacity, outside support, emotional stability, and co- Thoracic Outlet Syndrome Is a term used to describe a group of disorders that presents with symptoms secondary to neurovascular compression of fibers of the brachial plexus. This usually occurs between the points of the interscalene triangle and the inferior border of the axilla. Compression of the nerves and blood supply can occur as they pass over the first rib. Results from compression and damage the brachial plexus nerve trunks, subclavian vascular supply, and/or the axillary artery. Contributing factors in the development of TOS include the presence of a cervical rib, an abnormal first rib, postural deviations or changes, body composition, chronic hyperabducti on of the arm, hypertrophy or spasms of the scalene Will present with symptoms based on nerve and/or vascular compression. Typical symptoms include diffuse pain in the arm most often at night, paresthesias in the fingers and through the upper extremities, weakness & muscle wasting, poor posture, edema, and discoloration. If the upper plexus is involved, pain will be reported in the neck and may radiate to the face and follow the X-ray will confirm the presence of a cervical rib or other bony abnormality. Nerve conduction velocity testing may be valuable if a neuropathy exists. Otherwise, diagnosis relies solely on a through history of a pts symptoms, provocative testing, and physical exam. Adson’s, wright, roos, sallen, Halstead maneuver, hyperabductio n. morbidities. Initially management takes a conservative approach, it that fails its followed by surgical intervention. PT require intervention to assist with modification of posture, breathing patterns, positioning in bed and at the work site, and gentle stretching. Should focus on pain magnt, strengthening (trap, levator, and rhomboids) joint mobs, body mechanics, flexibility. If a pt has positive result from PT there will not be any long term impairments, however if they persist for 3 to 4 months, surgery muscles, degenerative disorders, and an elongated cervical transverse process. Traumatic Brain Injury (TBI) Injury where the brain makes contact with the skull secondary to a sudden violent acceleration or deceleration impact. Can also occur secondary to anoxia as with cardiac arrest or near drowning. lateral aspect of the forearm into the hand. If the lower plexus is involved, pain is reported in the back of the neck and shoulder, which will radiate over the ulnar distribution of the hand. Falls and Altered motor vehicle consciousness accidents are (coma, the leading obtundity, causes. High delirium), risk groups cognitive and include ages behavioral 0-4, 15-19, deficits, and greater changes in than 65. personality, Males are at motor a greater risk. impairments, alterations in tone, speech and swallowing issues. may be warranted. PT should allow pts to return to previous activity within 4-8 weeks. CT scan or MRI should be performed immediately in order to rule out hemorrhage, infarction, and swelling. Xrays taken of the cervical spine can be used to rule out fx and potential for subluxation. An EEG, PET, and cerebral Medical mangt initiated at the site of injury or in the emergency room for life preserving measures. Once stable, PT rehab in initiated and treatment includes PROM for a comatose pt or pathfinding and high-level balance for a pt with mild injury. Mobility tranining, behavior modification, blood flow mapping may also be utilized for diagnosis and baseline data. serial casting, compensatory strategies, vestibular rehab, task specific activities, w/c seating. Outcome is based on the degree of primary and secondary damage. Many pts experience long term deficits that don’t allow them to return to their pre-injury lifestyle. NM Medications: Drug Action Indications Side effects Antiepileptic Agents Reduce or eliminate seizure activity within the brain. These agents attempt to inhibit the firing of certain cerebral neurons through various Seizure activity (partial, generalized, and unclassified seizures) Ataxia, skin issues, behavioral changes, GI distress, headache, blurred vision, weight gain Implication s for PT Therapists must have adequate knowledge of established protocols for Examples Seconal (secobarbital), Klonopin (clonazepam), Depakote (valproic acid), Dilantin (phenytoin), effects on the CNS. Chemical classifications include barbiturates, benzodiazepines, carboxylic acids, hydantoins, iminostilbenes, succinimides, and second generation drugs. Antispasticity Agents Promote relaxation in a spastic muscle. Spasticity is an exaggerated stretch reflex of the muscle that can occur after injury to the CNS. Spasticity is not a primary condition, but a secondary effect from CNS damage. Agents Increased tone, spasticity, SCI, CVA, MS Drowsiness, confusion, headache, dizziness, generalized muscle weakness, hepatotoxicity potential with Dantrium, tolerance, dependence responding to a seizure as well as potential side effects of antiepilepti c medication s. Pts with epilepsy may show greater sensitivity to environme ntal surroundin gs such as light or noise level. Therapists must balance the need to decrease spastic muscles with the loss of function that a pt may experience Tegretol (carbamazepine0 , Celontin (methsuximide), Neurontin (gabapentin) Lioresal (baclofen), Valium (diazepam), Dantrium (dantrolene), Zanaflex (tizanidine) bind selectively within the CNS or within the skeletal muscle cells to reduce spasticity. Cholinergic Agents Cholinergic direct stimulant agents mimic acetylcholine and bind directly to the Glaucoma, dementia due to Alzheimer’s disease, postoperative GI distress, impaired visual accommodati on, with the reduction of hypertonici ty. Once spasticity is reduced, therapists should focus on therapeutic handling techniques, facilitation, and strengtheni ng to promote overall mobility. Sedation may also alter the scheduling of therapy to allow for maximal participatio n. Pts may experience a ↓ in HR and dizziness. Direct: Duvoid (bethanechol), Pilocar (pilocarpine) Indirect: Aricept Dopamine cholinergic receptor to activate & create a response at the cellular level. Indirect acting cholinergic stimulants increase cholinergic synapse activity through the inhibition of acetylcholinesteras e (which normally destroys acetylcholine). The increase of acetylcholine at the synapse increases cholinergic synaptic transmission. ↓in GI motility, myasthenia gravis, reversal of anticholinergi c toxicity bronchoconstr iction, bradycardia, flushing, other parasympathe tic effects Assist to relieve the Parkinsons’ Arrhythmias Therapist would be aware of characterisi cs of both sympatheti c and parasympa thetic systems and notify the physician if pt begins to exhibit unexpected side effects. Pts with Alzheimer’s disease and myasthenia gravis may be better able to participate in therapeutic activities when taking cholinergic agents. Therapists (donepezil), Tensilon (endrophonium), Prostigmin (neostigmine), Cognex (tacrine) Sinemet or Replacement Agents symptoms of Parkinson’s disease secondary to the ↓ in endogenous dopamine. These agents are able to cross the bloodbrain barrier through active transport and transform to dopamine within the brain. disease, Parkinsonism (levadopa), GI distress, orthostatic hypotension, dyskinesias, mood and behavioral changes, tolerance & pts attain maximal benefit from scheduling therapy one hour after administrat ion of levadopa. Therapist must understand the debilitating effects of drug holidays and should monitor the pts BP frequently due to the potential for orthostatic hypotensio n. Madopar (levadopa), Symmetrel (amantadine) Muscle Relaxant Agents Promote relaxation in muscles that typically present with spasm that is Muscle spasm Sedation, drowsiness, dizziness, nausea, Therapists must be aware of the Valium (diazepam), Flexeril (cyclobenzaprine) a continuous, tonic contraction. Spasms typically occur secondary to a MS or peripheral nerve injury rather than CNS injury. vomiting, headache, tolerance, dependence potential side effects, however, maximize the potential for relaxation through therapeutic techniques and the use of modalities during treatment. Prevention of reinjury through stretching, posture retraining, and education should assist the pt to achieve desired outcomes. , Paraflex (chlorzoxazone) Neuromuscular Rehab: Grading Spasticity: Modified Ashworth Scale Grade 0 1 1+ 2 3 4 Description No increase in muscle tone Slight increase in muscle tone, minimal resistance at the end of ROM Slight increase in muscle tone, minimal resistance through less than half of the ROM More marked increase in muscle tone, through most of ROM, but affected part easily moved Considerable increase in muscle tone, passive movement difficult Affected part rigid in flexion or extension Balance: •Somatosensory Input: Somatosensory receptors are located in the joints, muscles, ligaments, and skin to provide proprioceptive information regarding length, tension, pressure, pain, and joint position. Proprioceptive and tactile input from the ankles, knees, hips, and neck provide balance information to the brain. Challenging the somatosensory system: examination of pressure and vibration; observation of a pt when changing the surface they are standing on. Examples would be slopes, uneven surfaces, standing on foam. •Visual Input: Visual receptors for perceptual acuity regarding verticality, motion of objects and self, environmental orientation, postural sway, and movements of the head/neck. Children rely heavily on this system for maintenance of balance. Challenging the visual system: examination of quiet standing with eyes open, observing balance strategies to maintain center of gravity with and without visual input. Assessment of potential visual field cuts, hemianopsia, pursuits, saccades, double vision, gaze control, and acuity is necessary. •Vestibular Input: The vestibular input provides the CNS with feedback regarding the position and movement of the head with relation to gravity. The labyrinth consists of three semicircular canals filled with endolymph and two otolith organs. Semicircular canals respond to the movement of fluid with head motion. Otoliths measure the effects of gravity and movement with regard to acceleration/deceleration. Challenging the vestibular system: examination of balance with movement of the head; testing such as Dix-hallpike maneuver, bithermal caloric testing, assessment for nystagmus, head thrust sign; testing of the vestibulocular reflex. Balance Reflexes: Vestibuloocular reflex (VOR) Vestibulospinal reflex (VSR) VOR allows for head/eye movement coordination. This reflex supports gaze stabilization through eye movement that counters movements of the head. This maintains a stable image on the retina during movement. VSR attempts to stabilize the body and control movement. The reflex assists with stability while the head is moving as well has coordination of the trunk during upright postures. Automatic Postural Strategies: Are automatic motor responses that are used to maintain the center of gravity over the base of support. These responses always react or respond to a particular stimulus. Ankle strategy: Hip strategy: The ankle strategy is the first strategy to be elicited by a small range and slow velocity perturbation when the feet are on the ground. Muscle groups contract in a distal to proximal fashion to control postural sway from the ankle joint. The hip strategy is elicited by a greater force, challenge or perturbation through the pelvis and hips. The hips will move (in the opposite direction from the head) in Suspensory strategy: Stepping strategy: order to maintain balance. Muscle groups contract in a proximal to distal fashion in order to counteract the loss of balance. The suspensory strategy is used to lower the center of gravity during standing or ambulation in order to better control the center of gravity. Examples of this include knee flexion, crouching or squatting. This strategy is often used when both mobility and stability are required during a task (such as surfing) Is elicited through unexpected challenges or perturbations during static standing or when the perturbation produces such a movement that the center of gravity is beyond the base of support. The lower extremities step and/or upper extremities reach to regain a new base of support. Vertigo is used to describe a sense of movement and rotation of oneself or the surrounding environment. It typically is a sensation of spinning, but can also present as liner motion or falling. Vertigo may have a peripheral or central origin. Characteristics of Central Vs. Peripheral Vertigo: Peripheral Episodic and short duration Autonomic symptoms present Precipitating factor Central Autonomic symptoms less severe Loss of consciousness can occur Neurological symptoms present including: -diplopia -hemianopsia -weakness -numbness -ataxia -dysarthria Pallor, sweating Nausea and vomiting Auditory fullness (fullness within the ears) Tinnitus Etiology of Central Vs. Peripheral Vertigo Peripheral Benign paroxysmal positional vertigo (BPPV) Meniere’s disease Infection Trauma/tumor Metabolic disorders (DM) Acute alcohol intoxication Central Meningitis Migraine headache Complications of neurologic origin post ear infections Trauma/tumor Cerebellar degeneration disorders (alcoholism) Multiple Sclerosis Benign paroxysmal positional vertigo (BPPV): this condition is comprised of repeated episodes of vertigo that occur subsequent to changes in head position. BPPV only lasts a few seconds and is typically first noted while in a recumbent position since it most commonly affects the posterior semicircular canal. The etiology is usually otoconia (canalith) that loosens and travels into the posterior semicircular canal, causing vertigo. Nystagmus is present and can be noted when assessing a patient using the Dix-Hallpink test. Pts with BPPV typically find it self-limiting and can be successfully treated with canalith repositioning maneuvers which are passive movements used to remove the otoconia from the canals, thus remediating the vertigo. Dix-Hallpike test: This maneuver is a vertiginous position test used in assessment and treatment. This test stimulates the posterior semicircular canal and attempts to determine if otoconia exist within the canal. If the pt experiences nystagmus and vertigo, the test is performed to determine if a pt presents with BPPV or a central lesion. Procedure: The initial positioning for the Dix-hallpike test where the pt starts in sitting with the legs extended on the table and head rotated 45° to one side. The pt is rapidly moved to a supine position with the head (still in 45° rotation) extended 30° beyond horizontal off the end of the table. The therapist continues to hold the pts head in this position for 20-30 seconds observing the potential for nystagmus. If nystagums exists, the direction of the eyes and appearance of the nystagmus can determine inner ear versus CNS lesion. Balance Tests and Measures: •Berg Balance Scale: this is a tool designed to assess a pts risk for falling. There are 14 tasks, each scored on an ordinal scale from 0-4. These tasks include static activities, transitional movements, and dynamic activities in sitting and standing positions. The maximum score is a 56 with a score less than 45 indicating an ↑ risk for falling. This tool can be used as one time examination for as an ongoing tool to monitor a pt who may be at risk for falls. •Fregley-Graybiel Ataxia Test Battery: A tool that consists of 8 test conditions used in the battery with each leg measured on 2 accounts, the time spent in each test position and the number of steps that a pt takes without falling. 5 trials of each condition are performed. The test conditions include: -stand on beam with eyes open -Stand on beam with eyes closed -walk on beam with eyes open -sharpened Romberg (heel-toe static positioning) -standing with eyes open -standing with eyes closed -standing on one leg with eyes closed -walking on the floor with eyes closed The therapist scores each condition on a pass/fail basis with normative data for comparison. This tool is best suited for pts with high level motor skills since each condition is challenging. Therapists use this tool to assess and treat balance dysfunction, however, pt performance does not assist the therapist to diagnose the cause of balance dysfunction. •Fugl-Meyer Sensorimotor Assessment of Balance performance Battery: this tool is designed as a subset of the Fugl-Meyer Physical Performance Battery and is designed to assess balance specifically for pts with hemiplegia. Each of the 7 items assessed is scored from 0-2, specific to each item with the maximum score being 14. Even though 14 is the best score that a person can receive, the pt still may not have normal balance. •Functional Reach Test: a single task screening tool used to assess standing balance and risk of falling. A person is required to stand upright with a static base of support. A yardstick is positioned to measure the forward distance that a pt can reach without moving the feet. Three trials are performed and averaged together. The following are age-related standard measurements for functional reach: 20-40 years: 14.5-17 inches 41-69 years: 13.5-15 inches 70-87 years: 10.5-13.5 inches A pt that falls below the age appropriate range for functional reach has an increased risk for falling. The outcome measure demonstrates high test-retest correlation and intrarater reliability •Romberg Test: this is an assessment tool of balance and ataxia that initially positions the pt in unsupported standing, feet together, upper extremities folded, looking at a fixed point straight ahead with eyes open. With the eyes open, 3 sensory systems (visual, vestibular, somatosensory) provide input to the cerebellum to maintain standing stability. If there is a mild lesion in the vestibular or somatosensory systems, the pt will typically compensate through the visual sense. Next the pt maintains the same standing posture, but closes the eyes. A pt receives a grade of “normal” if they are able to maintain the position for 30 seconds. An abnormal response occurs with the inability to maintain balance when standing erect with the feet together and the eyes closed. Pts may exhibit excessive sway or begin to fall. When the visual input is removed, instability will be present if there is a larger somatosensory or vestibular deficit producing the instability. If a pt demonstrates ataxia and has a positive Romberg test, this indicates sensory ataxia and not cerebellar ataxia. There is also a sharpened Romberg test where the pts balance is further assessed by performing in the same manner but with a heel-to-toe stance, typically with the non-dominant foot in front. The pt would first be tested with eyes open and then with the eyes closed. This modification increases the challenge to the vestibular and somatosensory systems. •Timed Get Up and Go Test: this is a functional performance screening tool used to assess a person’s level of mobility and balance. The person initially sits in a supported chair with a firm surface, transfers to a standing position, and walks approximately 10 feet. The pt must then turn around without external support, walk back towards the chair, and return to a sitting position. The pt is scored based on amount of postural sway, excessive movements, reaching for support, side-stepping or other signs of loss of balance. The 5 point ordinal rating scale designates a score of 1 as normal and a score of 5 as severely abnormal. In an attempt to increase overall reliability the use of time was implemented. Pts who are independent can complete the multi-task process in 10 seconds or less. Pts that require over 20 seconds to complete the process are at the limit for functional independence and may be at an increased risk for falling. Pts that require 30 seconds are at high risk for a fall. •Tinetti Performance Oriented Mobility Assessment: a tool used to screen pts and identify if there is an increased risk for falling. The first section assesses balance through sit to stand and stand to sit from an armless chair, immediate standing balance with eyes open and closed, tolerating a slight push in the standing position, and turning 360°. A pt is scored form 0-2 in most categories with a maximum score of 16. The second section assess gait at normal spend and at a rapid, but safe speed. Items scored in this section include initiation of gait, step length, and height, step asymmetry and continuity, path, stance during gait, and trunk motion. A pt is scored 0-2 for each with a maximum score of 12. The tool has combined maximum total of 28 with the risk of falling increasing as the total score decreases. A total score less than 19 indicates a high risk for a fall. Vestibular Rehab: Vestibular rehab is a therapeutic intervention that can be highly successful for pts with vestibular or central balance system disorders. Exercise protocols for vestibular retraining utilize compensation, adaption, and plasticity to increase the brain’s sensitivity, restore symmetry, improve vestibulocular control, and subsequently increase motor control and movement. Goals for vestibular Rehab: -Improve balance -Improve trunk stability -↑ strength and ROM in order to improve ms balance responses and strategies -↓the rate and risk of falls -Minimize dizziness Vestibuloocular Retraining Therapeutic Guidelines: -Vestibuloocular reflex (VOR) and vestibulospinal reflex (VSR) stimulation exercises -Ocular motor exercises -Balance exercises -Gait exercises -combination exercises (obstacle courses, functioning in a public place) -Habituation training exercises (use only with appropriate pts) -Individualize each program based on the pts specific impairments (rehab vs. compensation training) -Use of practice, feedback, and repetition are vital for skill refinement -Use of gravity, varying surface conditions, visual conditions, and environmental cues should be included in therapeutic planning -The center of gravity must be controlled at each stage of treatment -Strategy (hip, ankle, stepping, suspense) training should be implemented during treatment so that strategies become automatic responses -Force plate systems, electromyographic biofeedback, optokinetic visual stimulation, and videography are all technical systems that can provide feedback to motor learning during vestibular rehab -Foam, mirrors, rocker boards, BAPS boards, Swiss balls, foam rollers, tramplines, and wedges are lower “tech” treatment tools that are successfully used to vestibular rehab CVA Tests and Measures: There are various tests and measures to assess the different impairments secondary to CVA. Pts are administered specific tests based on clinical diagnosis and pt presentation. •National Institute of Health (NIH) stroke scale: assessment of an acute CVA relative to impairment •Functional Independence Measure (FIM): provides a level of burden through assessment of mobility and ADL management •Stroke Impact Scale: assessment of physical and social disability or level of impairment secondary to CVA •Fugl-Meyer Assessment of Physical Performance: motor, sensory, and balance impairment; also assesses pain and ROM Neurological Rehabilitation: Neuro rehab may incorporate a variety of treatments based on the pts pathology, problem list, and deficits. There are many forms of neurological rehab based on each construct’s beliefs regarding motor control and motor learning. A therapist must use therapeutic techniques that meet the individual pts therapeutic objectives and goals. The following are various theories of neurological rehab based on each theory’s interpretation of motor control and motor learning. Motor Control: is the study of the nature of movement; or the ability to regulate or direct essential movement. Historically, control was thought to arise from reflex or hierarchical models where the cortex was perceived as the highest functioning component of the system and spinal level reflexes were the lowest functioning components. New models of motor control challenge these theories and believe that there is a greater distribution of control and that the cortex is not solely at the top of the hierarchy. Theories in general should provide a framework to interpret the issue or behavior, guide clinical action and treatment, provide new ideas, and utilize working hypotheses for examination and intervention. There are multiple theories of motor control that each embrace abstract ideas regarding the actual control of movement and are based on a specifc interpretation of how the brain functions and interacts with other body systems. Some of the motor control theories include the Reflex theory, Hierarchical theory, Motor programming theory, Task-oriented theory, and ecological theory. ●Motor Learning: Motor learning is the study of the acquisition or modification of movement. Motor learning differentiates learning versus performance, provides guidelines for appropriate use of feedback, prioritizes the impact of practice as it relates to skill and movement, and also focuses on the transfer of learning across tasks and environments of practice. Two of the initial theories of motor learning include: •Adam’s closed loop theory: The first attempt at the creation of a comprehensive motor learning theory with the premise of sensory feedback as an ongoing process for the nervous system to compare current movement with stored information on memory of past movement; high emphasis on the concept of practice. •Schmidt’s schema theory: this theory was created in response to the limitations of the closed loop theory. Its main construct relies on open loop control processes and a motor program concept; promotes clinical value to feedback and importance of variation with practice. ●Three Stage Model of Motor Learning: Cognitive Stage: This is the initial stage of learning where there is a high concentration of conscious processing of information. The person will acquire information regarding the goal of the activity and being to problem solve as to how to attain the goal. A controlled environment is ideal for learning during this stage and participation is a must for the person to progress. Characterized by: -large amount of errors -inconsistent attempts -repetition of effort allows for improvement in strategies -inconsistent performance -high degree of cognitive work: listening, observing, and processing feedback Associative Stage: This is the intermediate stage of learning where a person is able to more independently distinguish correct versus incorrect performance. The person is linking the feedback that has been received with the movement that has been performed and the ultimate goal. A controlled environment is helpful but at this stage, the person can progress to a less structured or more open environment. Avoid excessive external feedback as the person should have improved internal or proprioceptive feedback for the task at hand. Characterized by: -decreased errors with new skill performance -decreased need for concentration and cognition regarding the activity -skill refinement -increased coordination of movement -large amount of practice yields refinement of the motor program surrounding the activity Autonomous Stage: this is the final stage of learning or skilled learning where a person improves the efficiency of the activity without a great need for cognitive control. The person can also perform the task with interference from a variable environment. Characterized by: -automatic response -mainly error-free regardless of environment -distraction does not impact the activity -the person can simultaneously perform more than one task if needed -extrinsic feedback should be very limited or should not be provided -internal feedback or self-assessment should be dominant Feedback: is imperative for the progression of motor learning. A pt will rely on both intrinsic and extrinsic feedback as it relates to movement. Feedback allows for correction and adaptation within the environment. Current research supports reducing the extrinsic feedback (fading of feedback) in order to ultimately enhance learning. Intrinsic (inherent Represents all feedback that comes to feedback): the person through sensory systems as a result of the movement including visual, vestibular, proprioceptive, and somatosensory inputs. Extrinsic Represents the information that can (augmented) be provided while a task or movement feedback: is in progress or subsequent to the movement. This is typically in the form of verbal feedback or manual contacts. Knowledge of Is an important form of extrinsic results: feedback and includes terminal feedback regarding the outcome of a movement that has been performed in relation to the movement’s goals. Knowledge of Is extrinsic feedback that relates to performance: the actual movement pattern that someone used to achieve their goal of movement. Practice: refers to repeated performance of an activity in order to learn or perfect a skill. Physical practice allows for direct physical experience and kinesthetic stimulation to assist with acquisition of the skill. Mental practice is the cognitive rehearsal of a task or experience without any physical movement. Massed practice: The practice time in a trial is greater than the amount Distributed practice: Constant practice: Variable practice: Random practice: Blocked practice: Whole training: Part training: of rest between trials The amount of rest time between trials is equal to or is greater than the amount of practice time for each trial Practice of a given task under a uniform condition Practice of a given task under differing conditions Varying practice amongst different tasks Consistent practice of a single task Practice of an entire task Practice of an individual component or selected components of a task Key terminology: Closed system model: Compensation: Habituation: Learning: Non-associative: Associative: Procedural: Declarative: Motor learning: This is characterized by transfer of information that incorporates multiple feedback loops and larger distribution of control. In this model, the nervous system is seen as an active “participant” with the ability to enable the initiation of movement as opposed to solely “reacting” to stimuli. The ability to utilize alternate motor and sensory strategies due to an impairment that limits the normal completion of a task. The decrease in response that will occur as a result of consistent exposure to non-painful stimuli. The process of acquiring knowledge about the world that leads to a relatively permanent change in a person’s capability to perform a skilled action. A single repeated stimulus (habituation, sensitization) Gaining understanding of the relationship between two stimuli, causal relationships or stimulus and consequence (classical, operant conditioning) Learning tasks that can be performed without attention or concentration to the task; a task is learned by forming movement habits (developing a habit through repetitive practice) Requires attention, awareness, and reflection in order to attain knowledge that can be consciously recalled (internal practice) The ability to perform a movement as a result of internal processes that Motor program: Open system model: Performance: Plasticity: Postural control: Recovery: Sensitization: Strategy: interact with the environment and produce a consistent strategy to generate the correct movement. It is the acquisition of, or modification of movement. A concept of a central motor pattern that can be activated by sensory stimuli or central processes. Motor programs are seen as containing the rules for creating spatial and temporal patterns of motor activity needed to carry out a given motor task. This is characterized by a single transfer of information without any feedback loop (reflexive hierarchial theory). In this theory, the nervous system is seen as awaiting stimuli in order to react. A temporary change in motor behavior seen during a particular session of practice that is a result of many variables, however, only one variable is focusing on the act of learning. Performance is not an absolute measure of learning since there are multiple variables that potentially affect performance. The ability to modify or change at the synapse level either temporarily or permanently in order to perform a particular function. The ability of the motor and sensory systems to stabilize position and control movement. The ability to utilize previous strategies to return to the same level of functioning. The increase in response that will occur as a result of a noxious stimuli. A plan used to produce a specific result or outcome that will influence the structure or system. ●Carr & Shepherd: Motor Relearning Approach: An approach developed by Janet Carr and Roberta Sheperd in the 1970’s that targets normal movement and how it is relearned after neurological insult. Carr and Shepherd’s construct is that factors that are involved with learning are also involved with relearning and should include: •Identification of a goal •inhibition of any unnecessary activity that does not relate to normal movement •the ability to adjust during activity to the effects of gravity and balance •proper body alignment •proper motivation •incorporate internal or mental practice as well as external or physical practice •feedback •knowledge of results A significant construct of this approach is centered around a therapist’s observation of the pt during examination in order to identify the variations in normal movement. Through critical assessment, the therapist is able to identify components of movement that are missing or abnormal and the corresponding interventions. Treatment relies on techniques inherent to this approach as well as other various approaches to neurological rehab. Intrinsic feedback through sensory, visual, proprioceptive or tactile channels as well as external feedback through an observer is necessary for the pt to influence their progress towards their goals. Key terminology: Closed motor skill: a skill that is performed under a stable and unchanging environment Knowledge of results: providing the pt with external feedback regarding a pts performance of a task. This can include observations as well as objective data and can be positive or negative in nature with the goal of influencing the learner. Open motor skill: a skill that is performed under a consistently changing environment Transfer of learning: An action cannot be separated from the environment that is performed in. A pt must be able to transfer the skill or motor task into different environments. ●Bobath: Neuromuscular Development Treatment (NDT): An approach developed by Karl and Berta Bobath based on the hierarchical model of neurophysiologic function. Abnormal postural reflex activity and abnormal muscle tone are caused by the loss of central nervous system control at the brainstem and spinal cord levels. The concept recognizes that interference of normal function within the brain caused by central nervous system dysfunction leads to a slowing down or cessation of motor development and the inhibition of righting reactions, equilibrium reactions, and automatic movements. The pt should learn to control movement through activities that promote normal movement patterns that integrate function. New assumptions that have been incorporated into NDT resulting from current motor control research include: •Postural control can be learned and modified through experience •Postural control uses both feedback and feed-forward mechanisms for execution of tasks •Postural control is initiated from a pts base of support •Postural control is required for skill development •Postural control develops by assuming progressive positions in which there is an increase in the distance between the center of gravity and base of support; the base of support should also decrease Key Terminology: Facilitation: a technique utilized to elicit voluntary muscular contraction Inhibition: a technique utilized to decrease excessive tone or movement Key points of control: specific handling of designated areas of the body (shoulder, pelvis, hand, and foot) will influence and facilitate posture, alignment, and control Placing: the act of moving an extremity into a position that the pt must hold against gravity Reflex inhibiting posture: Designated static positions that Bobath found to inhibit abnormal tone influences and reflexes. ●Brunnstrom: Movement therapy in Hemiplegia Movement therapy in hemiplegia developed by Singe Brunnstrom is based on the hierarchical model by Hughlings Jackson. This approach created and defined the term synergy and initially encouraged the use of synergy patterns during rehab. The belief was to immediately practice synergy patterns and subsequently develop combinations of movement patterns outside of the synergy. Synergies are considered primitive patterns that occur at the spinal cord level as a result of the hierarchial organization of the central nervous system. Reinforcing synergy patterns is rarely utilized now as research has indicated that reinforced synergy patterns are very difficult to change. Brunnstrom developed the seven stages of recovery, which are used for evaluation and documentation of pt progress. Key Terminology: -Associated reaction: an involuntary and automatic movement of a body part as a result of an intentional active or resistive movement in another body part -Homolateral synkinesis: a flexion pattern of the involved upper extremity facilitates flexion of the involved lower extremity. -Limb synergies: a group of muscles that produce a predictable pattern of movement in flexion or extension patterns. -Raimiste’s phenomenon: the involved LE will abduct with applied resistance to the uninvolved LE in the same direction -Souque’s phenomenon: Raising the involved UE above 100° with elbow extension will produce extension and abduction of the fingers Seven Stages of Recovery: Stage 1: No volitional movement initiated Stage 2: The appearance of basic limb Stage 3: Stage 4: Stage 5: Stage 6: Stage 7: synergies. The beginning of spasticity. The synergies are performed voluntarily; spasticity increases Spasticity beings to decrease. Movement patterns are not dictated solely by limb synergies. A further decrease in spasticity is noted with independence form limb synergy patterns. Isolated joint movements are performed with coordination Normal motor function is restored. ●Kabat, Knott, and Voss: Proprioceptive Neuromuscular Facilitation (PNF) PNF was introduced in the early 1950s using the hierarchial model as its framework. The original goal of treatment was to establish gross motor patterns within the central nervous system. This approach is based on the premise that stronger parts of the body are utilized to stimulate and strengthen the weaker parts. Normal movement and posture is based on a balance between control of antagonist and agonist muscle groups. Development will follow the normal sequence through a component of motor learning. This theory places great emphasis on manual contacts and correct handling. Short and concise verbal commands are used along with resistance throughout the full movement pattern. The PNF approach utilizes methods that promote or hasten the response of the NM mechanism through stimulation of the proprioceptors. Movement patterns follow diagonals or spirals that each possess a flexion, extension, and rotary component and are directed toward or away from midline. Key Terminology: -Chopping: a combination of bilateral UE asymmetrical patterns performed as a closed chain activity -Developmental sequence: a progression of motor skill acquisition. The stages of motor control include mobility, stability, controlled mobility, and skill. -Mass movement patterns: the hip, knee, and ankle move into flexion or extension simultaneously -Overflow: muscle activation of an involved extremity due to intense action of an involved muscle or group of muscles Upper Extremity: D1 Flexion: flexion/adduction/external rotation; verbal cues:”close your hand, turn, and pull your arm across your face.” (grabbing earring) D1 Extension: extension/abduction/internal rotation; verbal cues: “open your hand, turn, and push your arm down and out.” (throwing earring away) D2 Flexion: flexion/abduction/external rotation; verbal cues: “open your hand, turn and lift your arm up and out. (sword drawn) D2 Extension: extension/adduction/internal rotation; verbal cues: “close your hand, turn, and pull your arm down and across your body.” (put sword in holder) Lower Extremity: D1 Flexion: flexion/adduction/external rotation; verbal cues: “bring your foot up, turn, and pull your leg up and across your body” (frog sit) D1 Extension: extension/abduction/internal rotation; verbal cues: “push your foot down, turn, and push your leg down and out.” D2 Flexion: flexion/abduction/internal rotation; verbal cues: “lift your foot up, turn, and lift your leg up and out.” D2 Extension: extension/adduction/external rotation; verbal cues: “push your foot down, turn, and pull your leg down and in.” Levels of Motor Control: Mobility: The ability to initiate movement through a functional range of motion Stability: The ability to maintain a position or posture through co- contraction and tonic holding around a joint. Unsupported sitting with midline control is an example of stability. Controlled The ability to move within a weight bearing mobility: position or rotate around a long axis. Activities in prone on elbows or weight shifting in quadruped are examples of controlled mobility. Skill: The ability to consistently perform functional tasks and manipulate the environment with normal postural reflex mechanisms and balance reactions. Skill activities include ADLs and community locomotion. PNF Therapeutic Exercise Descriptions: Agonistic Reversals Controlled mobility, skill: An isotonic concentric (AR) Alternating Isometrics (AI) Contract-Relax (CR) Hold-relax (HR) Hold-Relax Active Movement (HRAM) contraction performed against resistance followed by alternating concentric and eccentric contractions with resistance. AR requires use in a slow and sequential manner, and may be used in increments throughout the range to attain maximum control. Stability: Isometric contractions are performed alternating from muscles on one side of the joint to the other side without rest. AI emphasizes endurance or strengthening. Mobility: a technique used to increase ROM. As the extremity reaches the point of limitation, the pt performs a maximal contraction of the antagonistic muscle group. The therapist resists movement for 8-10 seconds with relaxation to follow. The technique is repeated until no further gains in ROM are noted during the session. Mobility: an isometric contraction used to increase ROM. The contraction is facilitated for all muscle groups at the limiting point in the ROM. Relaxation occurs and the extremity moves through the newly acquired range to the next point of limitation until no further increases in ROM occur. The technique is often used for pts that present with pain. Mobility: a technique to improve initiation of movement to muscle groups tested at 1/5 or less. An isometric contraction is preformed once the extremity is passively placed into a shortened range within the pattern. Overflow and facilitation may be used to assist with the contraction. Upon relaxation, the extremity is immediately moved into a lengthened position Joint Distraction Normal Timing (NT) Repeated contractions (RC) Resisted Progression (RP) Rhythmic Initiation (RI) of the pattern with a quick stretch. The pt is asked to return the extremity to the shortened position through an isotonic contraction. Mobility: a proprioceptive component used to increase ROM around a joint. Consistent manual traction is provided slowly and usually in combination with mobilization techniques. It can also be used in combination with a quick stretch to initiate movement. Skill: a technique used to improve coordination of all components of a task. NT is performed in a distal to proximal sequence. Proximal components are restricted until the distal components are activated and initiate movement. Repetition of the pattern produces a coordinated movement of all components. Mobility: a technique used to initiate movement and sustain a contraction through the ROM. RC is used to initiate a movement pattern, throughout a weak movement pattern or at point of weakness within a movement pattern. The therapist provides a quick stretch followed by isometric or isotonic contractions. Skill: a technique used to emphasize coordination of proximal components during gait. Resistance is applied to an area such as the pelvis, hips, or extremity during the gait cycle in order to enhance coordination, strength or endurance. Mobility: a technique used to assist in initiating movement when hypertonia exists. Movement progresses from passive “let me move you” to active assistive “help me move you”, to slightly resistive “move against the resistance”. Rhythmical Rotation (RR) Rhythmic Stabilization (RS) Slow Reversal (SR) Slow Reversal Hold (SRH) Timing for Emphasis (TE) Movements must be slow and rhythmical to reduce the hypertonia and allow for full ROM. Mobility: a passive technique used to decrease hypertonia by slowly rotating an extremity around the longitudinal axis. Relaxation of the extremity will increase ROM. Mobility, stability: a technique used to increase ROM and coordinate isometric contractions. The technique requires isometric contractions of all muscles around a joint against progressive resistance. The pt should relax and move into the newly acquired range and repeat the technique. If stability is the goal, RS should be applied as a progression from AI in order to stabilize all muscle groups simultaneously around the specific body part. Stability, controlled mobility, skill: A technique of slow and resisted concentric contractions of agonists and antagonists around a joint without rest between reversals. This technique is used to improve control of movement and posture. Stability, controlled mobility, skill: Using slow reversal with the addition of an isometric contraction that is performed at the end of each movement in order to gain stability. Skill: used to strengthen the weak component of a motor pattern. Isotonic and isometric contractions produce overflow to weak muscles. ●Rood: This theory is based on Sherrington and the reflex stimulus model. Rood believed that all motor output was the result of both past and present sensory input. Treatment is based on sensorimotor learning. It takes into account the autonomic nervous system and emotional factors as well as motor ability. Rood used a developmental sequence, which was seen as “key patterns” in the enhancement of motor control. A goal of this approach is to obtain homeostasis in motor output and to activate muscles to perform a task independent of a stimulus. Exercise is seen as a treatment technique only if the response is correct and if it provides sensory feedback that enhances the motor learning of that response. Once a response is obtained during treatment, the stimulus should be withdrawn. Rood introduced the use of sensory stimulation to facilitate or inhibit responses such as icing, and brushing in order to elicit desired reflex motor responses. Sensory Stimulation techniques: Facilitation Inhibition -Approximation -Deep pressure -Joint compression -Prolonged stretch -Icing -Warmth -Light touch -Prolonged cold -Quick stretch -Resistance -Tapping -Traction Key Terminology: Heavy work: a method used to develop stability by performing an activity (work) against gravity or resistance. Heavy work focuses on the strengthening of postural muscles. Light work: a method used to develop controlled movement and skilled function by performing an activity (work) without resistance. Light work focuses on the extremities. Key patterns: a developmental sequence designed by Rood that directs pts mobility recover from synergy patterns through controlled motion. Integumentary Examination: Foundational Science: Integ is the body’s largest organ. The avascular epidermis is the most superficial layer of skin. The dermis, known as the true skin, is well vascularized, and is characterized as elastic, flexible, and tough. Key functions: Protection, sensation, thermoregulation, excretion of sweat, vitamin D synthesis Phases of Normal wound Healing: Normal wound healing occurs as damaged tissues move through distinct yet overlapping phases of repair. In chronic wounds, this progression is either interrupted or delayed causing the wound to become “stuck” in a particular phase of healing. Inflammatory Phase (1-10 days) Inflammation is the immune system’s initial Proliferative Phase (3-21 days) Maturation Phase (7 days - 2 years) response to a wound. Temporary repair mechanisms rapidly re-establish hemostasis through platelet activation and the clotting cascade. Debris and necrotic tissue are removed and bacteria are killed by mast cells, neutrophhils, and leukocytes. Processes occurring in the inflammatory phase establish a clean wound bed which signals tissue restoration and permanent repair processes to begin. Re-epithelialization typically begins within 24 hours at the wound borders, though visible signs are usually not observed earlier than 3 days after injury. The formation of new tissue signals the beginning of the proliferative phase. Capillary buds and granulation tissue begin to fill the wound bed creating a support structure for the migration of epithelial cells. Keratinocytes, endothelial cells, and fibroblasts are active and the collagen matrix is formed. Skin integrity is restored in the proliferative phase with wound closure occurring through epithelialization and wound contraction. The maturation, or remodeling phase is initiated when granulation tissue and epithelial differentiation being to appear in the wound bed. As the maturation phase progresses, mechanisms of fiber reorganization and contraction shrink and thin the scar. An immature scar will appear red, raised, and rigid while a mature scar will appear pale, flat, and pliable. Scar tissue is remodeled and strengthened though the processes of collagen lysis and synthesis. Newly repaired tissues have approximately 15% of pre-injury tensile integrity and should be protected to prevent re-injury. Over time, tensile integrity may increase as much as 80% of the pre-injury strength. Hypertrophic scarring, especially in relation to burn injuries, can significantly impact maturation phase progression. A burn without hypertrophic scarring will typically mature within 4-8 weeks; burns with hypertrophic scarring, however, may require up to two years to reach maturity. Wound Types: Acute wounds Abrasion Avulsion Incisional wound Laceration Penetrating Puncture Skin tear Is a wound caused by a combination of friction and shear forces, typically over a rough surface, resulting in the scraping away of the skin’s superficial layers. A soft tissue avulsion, sometimes referred to as degloving, is a serious wound resulting from tension that causes skin to come detached from underlying structures. Is most often associated with surgery and is created intentionally by means of a sharp object such as a scalpel or scissors. Is a wound or irregular tear of tissues often associated with trauma. Lacerations can result from shear, tension, or high force compression with the resultant wound characteristics dependent on the mechanism of injury. Can result from various mechanisms of injury and is described as a wound that enters the interior of an organ or cavity. Is made by a sharp pointed object as it penetrates the skin and underlying tissues. Typically, there is relatively little tissue damage beyond the wound tract, however, the risks of contamination and infection can be significant. Often results from trauma to fragile skin such as bumping into an object, adhesive removal, shear or friction forces. The severity of a skin tear can range from a flap like tear, that may or may not remain viable, to full-thickness tissues loss. Ulcers: Type Description Recommendations Arterial Insufficiency Ulcers Wounds resulting from arterial insufficiency occur secondary to inadequate circulation of oxygenated blood (ischemia) often due to complicating factors such as atherosclerosis. Venous Insufficiency Ulcers Wounds resulting from venous insufficiency occur secondary to impaired functioning of the venous system resulting in inadequate circulation and eventual tissue damage and ulceration. Neuropathic Ulcers Are a secondary complication usually associated with a combination of ischemia and neurophathy. Neuropathic ulcers are often associated with diabetes mellitus, however, any form of peripheral neuropathy poses an increased risk of wound development Also referred to as decubitus ulcers, result from sustained or prolonged pressure on tissue at levels greater than that of capillary pressure. Skin covering bony prominences is particulary susceptible to localized ischemia and tissue necrosis due to Pressure Ulcers -Rest, limb protection, risk reduction education, inspect legs and feet daily, avoid unnecessary leg elevation, avoid using heating pads or soaking feet in hot water, wear appropriately sized shoes with clean, seamless socks -Limb protection, risk reduction education, inspect legs & feet daily, compression to control edema, elevate legs above the heart when resting or sleeping, attempt active exercise including frequent ROM, wear appropriately sized shoes with clean, seamless socks -Limb protection, risk reduction education, inspect legs and feet daily, inspect footwear for debris prior to donning, wear appropriately sized off-loading footwear with clean, cushioned, seamless socks -Repositioning every 2 hours in bed, management of excess moisture, off-loading with pressure relieving devices, inspect skin daily for signs of pressure damage, limit shear and friction forces over fragile skin pressure. Pressure injury risk assessment tools (Braden Scale, Norton Scale) Characteristics of LE Ulcers: Arterial Ulcers Lower one third of leg, toes, web spaces, dorsal foot, lateral malleolus Venous Ulcers Proximal to the medial malleolus Appearance Smooth edges, well defined, lack of granulation tissue, tend to be deep Irregular shape, shallow Exudate Pain Minimal Severe Moderate/heavy Mild to moderate Pedal pulses Diminished or absent Normal Edema Skin Temp Tissue changes Normal Decreased Thin and shiny, hair loss, yellow nails Increased Normal Flaking, dry skin, brownish discoloration Miscellaneous Leg elevation increases pain Leg elevation lessens pain Location Neuropathic Ulcers Areas of the foot susceptible to pressure or shear forces during WBing Well-defined oval or circle, callused rim; cracked periwound tissue; little to no wound bed necrosis with good granulation Low/moderate None, however dysesthesia may be reported Diminished or absent, unreliable anklebrachial index with diabetes Normal Decreased Dry, inelastic, shiny skin, decreased or absent sweat and oil production Loss of protective sensation Wound Assessment Wound Classification by depth of injury: *Wounds that are not categorized as pressure or neuropathic ulcers (skin tears, surgical wounds, venous statisis ulcers) are classified based on the depth of tissue loss. Superficial wound: Partial-thickness wound: Full-thickness wound: Subcutaneous wound: Causes trauma to the skin with the epidermis remaining intact, such as with a non-blistering sunburn. A superficial wound will typically heal as part of the inflammatory process. Extends through the epidermis and possibly into, but not through the dermis. Examples include abrasions, blisters, and skin tears. A partial thickness wound will typically heal by re-epithelialization or epidermal resurfacing depending on the depth of injury. Extends through the dermis into deeper structures such as subcutaneous fat. Wounds deeper than 4 mm are typically considered full thickness and heal by secondary intention. Subcutaneous wounds extend through integumentary tissues and involve deeper structures such as subcutaneous fat, muscle, tendon or bone. Subcutaneous wounds typically require healing by secondary intention. Primary intention: Most common in acute wounds with minimal tissue loss. Smooth clean edges are reapproximated and closed with sutures, staples, or adhesives. Typically have minimal scarring, and heal quickly in uncomplicated progression. Examples: surgical incision, laceration, puncture, and superficial & partial thickness wounds. Secondary Intention: Permits wounds to close on their own without superficial closure. Wounds with characteristics such as significant tissue loss or necrosis, irregular on nonviable wound margins that can’t be reapproximated, infection or debris contamination. Require ongoing wound care and have larger scars. Examples: neuropathic, arterial, venous or pressure ulcers, most full thickness wounds, and chronically inflamed wounds. Tertiary Intention: AKA delayed primary intention. Wounds at risk for developing complications such as sepsis or dehiscence, may be temporarily left open. Once risk factors have been alleviated, the wound is closed by the usually primary intention methods. Wagner Ulcer Grade Classification Scale Grade 0 1 2 3 4 5 Description No open lesion, but may possess pre-ulcerative lesions; healed ulcers; presence of bony deformity Superficial ulcer not involving subcutaneous tissue Deep ulcer with penetration through the subcutaneous tissue, potentially exposing bone, tendon, ligament or joint capsule Deep ulcer with osteitis, abscess or osteomyelitis Gangrene of digit Gangrene of foot requiring disarticulation Pressure Ulcer Staging *A pressure ulcer describes a localized injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure or pressure in combination with shear/friction forces. Stage I StageII Stage III Stage IV Intact skin with non-blanchable redness of a localized area usually over a bony prominence. Darkly pigmented skin may not have visible blanching, but instead present as local coloration differing from the surrounding area. The area may be painful, firm, soft, warmer or cooler as compared to adjacent tissue. Stage 1 may be difficult to detect in individuals with dark skin tones. Partial-thickness tissue loss of the dermis presenting as a shallow open ulcer with red or pink wound bed. May present as an intact or ruptured serum filled blister or presents as a shiny or dry shallow ulcer without slough or bruising. This stage should not be used to describe skin tears, tape burns, perineal dermatitis, maceration or excoriation. Full-thickness tissue loss. Subcutaneous fat may be visible but tone, tendon or muscle are not exposed. Slough may be present, but does not obscure the depth of tissue loss. May include undermining and tunneling. Bone and tendon are not visible or directly palpable. The depth of a stage III pressure ulcer varies by anatomical location. For example, a stage III ulcer on the bridge of the nose, ear, occiput, and malleolus, where there is not significant subcutaneous tissue, can be quite shallow. In contract, areas with significant adipose tissue can develop extremely deep stage III pressure ulcers. Full-thickness tissue loss with exposed bone, tendon or muscle that is visible or directly palpable. Slough or eschar may be present on some parts of the wound bed. Undermining and tunneling may be present. Stage IV ulcers can extend into muscle and supporting structures (fascia, tendon, joint capsule) making osteomyelitis possible. Suspected Purple or maroon localized areas of intact skin or blood-filled blister due to damage of Deep tissue underlying soft tissue from pressure/and or shear forces. The area may be preceded by tissue injury that is painful, firm, mushy, boggy, warmer or cooler compared to adjacent tissue. Deep tissue injury may be difficult to detect in individuals with dark skin tones. The evolution may include a thin blister over a dark wound bed. The wound may further evolve and become covered by thin eschar. Evolution may be rapid, exposing additional layers of tissue even with optimal treatment. Unstageable Full-thickness tissue loss in which the base of the ulcer is covered by slough (yellow, gray, green, or brown) and or eschar (tan, brown, or black) in the wound bed. Until enough slough and/or eschar is removed to expose the base of the wound, the true depth, and therefore stage, cannot be determined. Stable (dry, adherent, intact without erythema or fluctuating appearance) eschar on the heels serve as “the body’s natural (biological) cover” and should not be removed. Exudate Classification: Serous Presents with a clear, light color and a thin, watery consistency. Serous exudates is considered to be normal in a healthy healing wound and is observed during the inflammatory and proliferative phases of healing. Sanguineous Presents with a red color and a thin, watery consistency. The red appearance of sanguineous exudates is due to the presence of blood which may become brown if allowed to dehydrate. Sanguineous exudates may be indicative of new blood vessel growth or the disruption of blood vessels. Serosanguineous Presents with a light red or pink color and a thin, watery consistency. Serosanguineous exudates is considered to be normal in a healthy healing wound and is typically observed during the inflammatory and proliferative phases of healing. Seropurulent Presents as cloudy or opaque, with a yellow or tan color and a thin, watery consistency. Seropurulent exudates may be an early warning sign of an impending infection and is always considred an abnormal finding. Purulent Presents with a yellow or green color and a thick, viscous consistency. Purulent exudates is generally an indicator of wound infection and is always considered an abnormal finding. Necrotic Tissue Types: *Necrotic tissue is dead tissue resulting from the localized physiological and enzymatic changes associated with cell death. Necrotic tissue is often documented and named by the specific type observed, and may also be referred to as devitalized or nonviable tissue. Eschar Described as dark or leathery, black/brown, dehydrated tissue that tends to be firmly adhered to the wound bed. Gangrene Refers to death and decay of tissue resulting from an interruption of blood flow to an area of the body. Some types of gangrene are also characterized by the presence of bacterial infection. Gangrene most commonly affects the extremities, but can also occur in muscles and internal organs. Hyperkeratosis Also referred to a callus, is typically white/gray in color and can vary in texture from firm to soggy depending on the moisture level in surrounding tissue. Slough Described as moist, stringy or mucinous, white/yellow tissue that tends to be loosely attached in clumps to the wound bed. Red-Yellow-Black System Red Color Wound Description Pink granulation tissue Yellow Most, yellow slough Black Black, thick eschar firmly attached Goals Protect wound, maintain moist environment Remove exudates and debris; absorb drainage Debride necrotic tissue Wound Terminology: Contusion An injury, usually caused by a blow, that does not disrupt skin integrity. The injury is characterized by pain, edema, and discoloration which appears as a result of blood seepage under the surface of the skin. Dehiscence The separation, rupture or splitting of a wound closed by primary intention. This disruption of previously approximated surfaces may be superficial or involve all layers of tissue. Dermis The vascular layer of skin located below the epidermis containing hair follicles, sebaceous glands, sweat glands, lymphatic and blood vessels, and nerve endings. Desiccated The drying out or dehydration of wound. Desiccation often results from poor dressing selection that does not control the evaporation of wound bed moisture. Desquamation The peeling or shedding of the outer layers of the epidermis. Desquamation normally occurs in small scales, although certain injuries and conditions, and medications may cause peeling in larger scales or sheets and extend to deeper layers of skin. Ecchymosis The discoloration occurring below intact skin resulting from trauma to underlying blood vessels and blood seeping into tissues. The discoloration is typically blue-black, changing in time to a greenish brown or yellow color. An area where ecchymosis is present is commonly referred to as a bruise. Epidermis The superficial, avascular epithelial layer of the skin that includes flat, scale-like squamous cells, round basal cells, and melanocytes which produce melanin and give skin its color. Erythema A diffuse redness of the skin often resulting from capillary dilation and congestion or inflammation. Friable Tissue that readily tears, fragments or bleeds when gently palpated or manipulated. Hematoma A localized swelling or mass of clotted blood confined to a tissue, organ or space usually caused by a break in a blood vessel. Hypergranulation Increased thickness of the granular layer of the epidermis that exceeds the surface height of the skin. Hyperpigmentation An excess of pigment in a tissue that causes it to appear darker than surrounding tissues. Hypertrophic scar An abnormal scar resulting from excessive collagen formation during healing. A hypertrophic scar is typically raised, red, and firm with disorganized collagen fibers. Keloid An abnormal scar formation that is out of proportion to the scarring required for normal tissue repair and is comprised of irregularly disturbed collagen bands. A keloid scar typically exceeds the boundaries of the original wound appearing red, thick, raised, and firm. Maceration The skin softening and degeneration that results from prolonged exposure to water and other fluids. Normotrophic scar Characterized by the organized formation of collagen fibers that align in a parallel fashion. Turgor The relative speed with which the skin resumes its normal appearance after being lightly Ulcer pinched. Turgor is an indicator of skin elasticity and hydration and normally occurs more slowly in older adults. An open sore or lesion of the skin accompanied by sloughing of inflamed necrotic tissue. Types of Burns: Thermal burns Electrical burns Chemical burns Radiation burns Caused by conduction or convection. Ex: hot liquid, fire or steam Caused by the passage of electrical current through the body. Typically there is an entrance and an exit wound. Complications can include cardiac arrhythmias, respiratory arrest, renal failure, neurological damage, and fractures. Ex. Lightning Occurs when certain chemical compounds come in contact with the body. The reaction will continue until the chemical is diluted at the site of contact. Sulfuric acid, lye, hydrochloric acid, and gasoline are examples. Occurs most commonly with exposure to external beam radiation therapy. DNA is altered in exposed tissues and ischemic injury may be irreversible. Complications may include severe blistering and desquamation, non-healing wounds, tissue fibrosis, permanent discoloration, and new malignancies. Zones of Injury: Zone of coagulation Zone of stasis Zone of hyperemia The area of the burn that received the most severe injury with irreversible cell damage. The area of less severe injury that possesses reversible damage and surrounds the zone of coagulation. The area surrounding the zone of stasis that presents with inflammation, but will fully recover without any intervention or permanent damage. Burn Classification: Superficial Burn Superficial PartialThickness Burn Involves only the outer epidermis, Area may be red with slight edema. Healing occurs without peeling or evidence of scarring in 2-5 days. Involves the epidermis and the upper portion of the dermis. The involved area may be extremely painful and exhibit blisters. Healing occurs with minimal to no Deep PartialThickness Burn Full thickness burn Subdermal Burn scarring in 5-21 days. Involves complete destruction of the epidermis and the majority of the dermis. The involved area may appear to be discolored with broken blisters and edema. Damage to nerve endings may result in only moderate levels of pain. Hypertrophic or keloid scarring may occur. In the absence of infection, healing will occur in 21-35 days. Involves complete destruction of the epidermis and dermis along with partial damage to the subcutaneous fat layer. Healing varies within weeks, with or without grafting, and/or months to heal. Involves the complete destruction of the epidermis, dermis, and subcutaneous tissue. Subdermal burns may involve muscle and bone and as a result, often require multiple surgical interventions and extensive healing time. Rule of Nines: Head and neck Anterior trunk Posterior trunk Bilateral anterior arm, forearm & hand Bilateral posterior arm, forearm, & hand Genital region Bilateral anterior leg and foot Bilateral posterior leg and foot 9% 18% 18% 9% 9% 1% 18% 18% Integumentary Pathology: Pathology Cellulitis What is it Is a fast spreading inflammation that occurs as a result of a bacterial infection of the skin and connective tissues. It can develop anywhere under the skin, but will typically affect the extremities. Etiology Caused by a particular bacterial infections including strep or staph. Predisposing factors to cellulitis include an increased age, immunosuppression, trauma, the presence of wounds or venous insufficiency. Signs & Symptoms Localized redness that may spread quickly, skin that is warm or hot to touch, local abscess of ulceration, tenderness to palpation, chills, fever, and malise Contact dermatitis Is a superficial irritation of the skin resulting from localized irritation (poison ivy, latex, soap, jewelry, sensitivity). This condition can be acute or chroic Occurs with exposure to mechanical, chemical, environmental or biological agents. Nickel, rubber, latex and topical antibiotics are Intense itching, burning and red skin in areas corresponding to the location of the irritation. Treatment Should be immediately referred to a physician for further assessment. Cellulitis requires pharmacological intervention using systemic antibiotics. Differential diagnosis should attempt to rule out DVT and contact dermatitis. PT may be warranted for wound care. Cellulitis can lead to sepsis or gangrene if not properly treated. Focus should be on identifying and removing the source of irritation. Topical steroid application is commonly employed. based on exposure to the precipitating agent. Contact dermatitis is a very common skin disease that can occur at any age. AKA dermatitis. Is used to describe a group of disorders that cause chronic skin inflammation typically due to an immune system abnormality, allergic reaction or external irritant. common agents. Gangrene (Dry) When there is a loss of vascular supply resulting in local tissue death. Fingers, toes, and limbs are most affected. Typically develops slowly and results in auto-amputation. Occurs most commonly in blood vessel disease, such as DM or atherosclerosis. It develops when blood flow to an affected area is impaired, typically as a result of poor circulation. Gangrene (wet) If there is an Can develop after a Eczema Is based on the particular form of the disorder. Infants and children are at a high risk for eczema but may outgrow it. Red or browngray, itchy, lichenified skin plaques that may be exacerbated by some topical agents such as soaps and lotions. Oozing and crusting of the patchy occurs in younger population. Dark brown or black nonviable tissue that eventually becomes a hardened mass. Pt will complain of cold or numb skin and they may present with pain. Swelling and pain Pharmacological interventions are variable from topical to oral. Cold compresses and other modalities may assist with reducting the itching. Extreme temps should be avoided. Serious medical condition and requires immediate medical intervention. Tx includes pharmacolocial intervention, surgery, and hyperbaric oxygen therapy. Serious medical associated bacterial infection in the affected tissue. Swelling resulting from the bacterial infection causes a sudden stoppage of blood flow. severe burn, frostbite or injury and requires immediate treatment since it tends to spread very quickly and can be fatal. at the site of infection, change in skin color from red to brown to black, blisters that produce pus, fever, and general malaise Onychomycosis Refers to a fungal infection that primarily affects the toenails & nailbeds. Yellow or brown nail discoloration; hyperkeratosis and hypertrophy of the nail causing it to partially detach from the nailbed. Plaque psoriasis Autoimmune disease of the skin and is most common of the 5 types of psoriasis. T cells trigger inflammation within the skin Acquiring a fungal infection is a common occurrence. Risk factors include manicures and pedicures with unsterile utensils, possessing nail injuries or deformities, excess skin moisture, wearing closed toe shoes, and an impaired immune response. Genetic predisposition to plaque psoriasis. Other factors may trigger psoriasis, such as injury to the skin, insufficient or excess sunlight, Red raised blotches that typically present in a bilateral fashion (over both knees or elbows). Tend to itch and flake. condition and requires immediate intervention. Surgical debridement and intravenous antibiotic treatment are typical. Manual debridement of the nail and topical antifungal medications are primary. Control symptoms and prevent secondary infection. Lifelong condition that can be effectively managed and controlled through Tinea pedis and produce an accelerated rate of skin cell growth. The skin cells accumulate in raised red patches on the surface of the skin. Athlete’s foot. Is a superficial fungal infection which causes epidermal thickening and a scaly skin appearance. This fungus is opportunistic and will rapidly multiply in a warm and most environment (between the toes) stress, excessive alcohol, HIV infection, smoking, and certain medications. Wearing closed toed shoes that don’t allow airflow, prolonged periods of moisture or wetness, excessive sweating, and possessing small nail or skin abrasions. This infection is contagious through direct contact. the various stages and exacerbations. Itching, redness, peeling skin between the toes, pain, odor, and in more severe cases breaks in skin continuity Pharmacological management includes topical or oral antibiotics depending on the severity of symptoms. May persist or recur and more longterm management may be required. Prevention includes drying of the feet when bathing or swimming, wearing sandals around public pools or showers, changing socks frequently, proper hygiene, and avoiding shoe wear that creates a moist environment. Integumentary Pathologies: Pathology Diagnosis FullThickness Burn This severe burn causes immediate cellular and tissue death and subsequent vascular destruction. Indicates complete destruction of the epidermis, dermis, hair follicle, and nerve endings, within the dermis; and also affects the subcutaneo us fat layer and underlying muscles, resulting in red blood Contributing Factor 75% of burns are a direct result from the pts actions. Higher risk for burns in children between 1 & 5 years as well as individuals over 70. Burns are currently the third leading cause of accidental death in all age categories with males having a higher overall frequency of injury. Clinical Presentation Characterized by a variable appearance of deep red, black or white coloring. Eschar form from necrotic cells and creates a dry and hard layer that requires debridement. Edema is present at the site of injury and in surrounding tissues. Hairs within this region of the burn are easily pulled from the follicle due to the destruction. An area of fullthickness burn does not have sensation or pain due to destruction of Lab/Imaging Blood work should include a complete blood count, electrolytes, blood urea nitrogen, creatinine, bilirubin, and arterial blood gases. This will indicate baseline data, systemic changes, level of shock, and metabolic complications . Bronchoscopy & pulmonary function tests may be indicated to assess airway damage and pulmonary insufficiency. Management/Outcom e Initial management includes medically stabilizing the pt. This emergent phase lasts 48-72 hours and concludes with regaining capillary permeability and hemodynamic stability. An autograft procedure is usually required for fullthickness burns. The rehab phase is a long term commitment that includes all aspects of functional recover. PT begins immediately following skin grafting and includes wound care, pulmonary exercises, positioning, splinting, and immobilization for the first 3-5 days. Early ambulation and mobility activities should be incorporated as soon as possible in cell destruction. free nerve endings, however there may be pain from adjacent areas that experience partial-thickness burns. During the initial stages the pt will experience thermoregulatio n impairment, SOB, electrolyte disturbances, poor urine output, and variation in level of consciousness. order to decrease complications. Continued PT should involve edema control, monitoring of any elastic garments, massage, stretching, hydrotherapy, ROM, debridement, relaxation techniques, progressive exercise, ambulation, and functional mobility training. The mortality rate has decreased over the last 2 decades due to improvement in burn care. Mortality rates are highest for children under 4 and adults over 65. Overall prognosis is dependent on factors such as cardiac pathology, alcoholism, PVD, and obesity. Garments may be worn up to 2 years after injury. Without significant complications a pt should achieve independence within a few months post injury. Pressure Ulcer Ischemia to the site, subsequent cell death, and tissue necrosis. A definition of unrelieved pressure is >32mm Hg of pressure to an area for more than 2 hours. Can occur at any time secondary to unrelieved pressure, but there are certain populations and risk factors that are associated with its development . Immobility is a leading factor and seen in pts with SCI, paralysis, hemiplegia, impaired cognition, poor nutrition, altered sensation, incontinence, decreased lean body mass, and infection. A pt will usually develop a pressure ulcer over a bony prominence with common sites including the greater trochanter, ischium, sacrum, and heel. A stage I is classified as an area of nonblanchable erythema of intact skin. State II is classified as a partial thickness wound involving the epidermis, dermis, or both. Does not extend through the entire dermis. Stage III is classified as an ulcer that extended into subcutaneous tissue, but not through fascia. Stage IV is classified as an ulcer that A diagnosis is made from visual inspection, however, blood studies such CBC, electrolyte, and protein levels, as well as tests for baceremia or sepsis may be indicated. Urinalysis and stool samples may be indicated to determine contributing factors in the development of the ulcer. Coagulation studies and tissue sampling may also be indicated. The Braden Scale, Gosnell Scale, or Norton Scale along with baseline Pt and caregiver education for the prevention of subsequent pressure ulcers is very important and should include skin inspection, positioning, and pressure relief techniques. Seat cushions, multipodus boots or specialized mattresses is also an important aspect of care of ulcers. Dressing for the ulcer may include nonocclusive or occlusive types. Nonocclusive include dry to dry, wet to wet, wet to dry or composite dressings. Occlusive dressings include semipermeable films, hydrocollooids, hydrogels, semipermeable foams, and alginates. A general exercise program should be provided daily. Pts should avoid the use of hot water and the use of massage extends through the fascia and deeper. It is a full-thickness wound that may damage muscles, bones, ligaments and/or tendons. measurement of size and depth of the ulcer. surrounding the site. Therapist should promote proper positioning techniques (such as positioning of the bed at less than 45° angle) in order to decrease friction and shear. Approx 60,000 pts die annually due to secondary complications from ulcers. However, many people that develop a pressure ulcer completely recover with no residual impairments. Types of Dressings: Dressings may be defined as either primary or secondary. A primary dressing is one that comes into direct contact with a wound. A number of primary dressings include a self-adhesive backing and not require a secondary dressing. Secondary dressings are placed directly over the primary dressing to provide additional protection, absorption, occlusion, and/or to secure the primary dressing in place. Type Hydrocolloids: Consist of gel-forming polymers (carboxymethylcellulose, gelatin, pectin) backed by a strong film or foam adhesive. The dressing does not attach to the wound itself but instead Indications Hydrocolloids are useful for partial and fullthickness wounds. The dressings can be used effectively with granular or necrotic wounds. Advantages -Provides a moist environment for wound healing -Enables autolytic debridement -Offers protection from microbial contamination Disadvantages -May traumatize surrounding intact skin upon removal -May tend to roll in areas of excessive friction -Cannot be used on infected wounds anchors to the intact surrounding skin. The dressings absorb exudates by swelling into a gel-like mass and vary in permeability, thickness, and transparency. Hydrogels: Consist of varying amounts of water and gel-forming materials such as glycerin. The dressings are typically available in both sheet and amorphous forms. Foam Dressings: Are comprised of a hydrophilic polyurethane base that contacts the wound surface and a hydrophobic outer layer. The dressings allow exudates to be absorbed into the foam through the hydrophilic layer. The dressings are most -Provides moderate absorption -Does not require a secondary dressing -Provides a waterproof surface Hydrogels are moisture retentive and commonly used on superficial and partialthickness wounds (abrasions, blisters, pressure ulcers) that have minimal drainage. Foam dressings are used to provide protection and absorption over partial and full-thickness wounds with varying levels of exudates. They can also be used as secondary dressings over amorphous hydrogels. -Provides a moist environment for wound healing -Enables autolytic debridement -May reduce pressure and diminish pain -Can be used as a coupling agent for ultrasound -Minimally adheres to wound -Some products have absorptive properties -Provide a moist environment for wound healing -Available in adhesive and non-adhesive forms -Provides prophylactic protection and cushioning -Encourages autolytic debridement -Provides moderate absorption -Potential for dressing to dehydrate -Cannon be used on wounds with significant drainage -Typically requires a secondary dressing -May tend to roll in areas of excessive friction -Adhesive form may traumatize periwound area upon removal -Lack of transparency makes inspection of wound difficult commonly available in sheets or pads with varying degrees of thickness. Semipermeable foam dressings are produced in adhesive and nonadhesive forms. Nonadhesive forms require a secondary dressing. Transparent Film: Film dressings are thin membranes made from transparent polyurethane with water-resistant adhesives. The dressings are permeable to vapor and oxygen, but are largely impermeable to bacteria and water. They are highly elastic, conform to a variety of body contours, and allow easy visual inspection of the wound since they are transparent. Gauze: Manufactured from yarn or thread and are the most readily available dressing used in inpatient environments. Gauze Film dressings are useful for superficial or partial-thickness wounds with minimal drainage (scalds, abrasion, lacerations) -Provides a moist environment for wound healing -Enables autolytic debridement -Allows visualization of the wound -Resistant to shearing and frictional forces -Cost effective over time -Excessive exudates accumulation can result in periwound maceration -Adhesive may traumatize periwound area upon removal -Cannot be used on infected wounds Gauze dressings are commonly used on infected or non-infected wounds of any size. The dressings can be used for wet-to-wet, wet-to- -Readily available and cost effective shortterm dressings -Can be used alone or in combination with other dressings and topical -Has a tendency to adhere to the wound bed traumatizing viable tissue on removal -Highly permeable -Requires frequent dressings come in many shapes and sizes (sheets, squares, rolls, packing strips). Impregnated gauze is a variation of woven gauze in which various materials such as petroalatum, zinc or anitmicrobials have been added). Alginates: Are derived from a seaweed extraction, specifically, the calcium salt component of alginic acid. Alginates are highly absorptive, but are also highly permeable and non-occlusive. As a result, they require a secondary dressing. Alginate dressings act as a hemostat and create hydrophilic gel through the interaction of calcium ions in the dressing and sodium ions in the wound exudate. moist or wet-to-dry debridement. agents -Can modify number of layers to accommodate for changing wound status -Can be used on infected or non-infected wounds dressing changes -Prolonged use decreases cost effectiveness -Increased infection rate compared to occlusive dressings Alginates are typically used on partial or fullthickness draining wounds such as pressure or venous insufficiency ulcers. Alginates are often used on infected wounds due to the likelihood of excessive drainage. -High absorptive capacity -Enables autolytic debridement -Offers protection from microbial contamination -Can be used on infected or non-infected wounds -Non-adhering to wound -May require frequent dressing changes based on level of exudates -Requires a secondary dressing -Cannot be used on wounds with an exposed tendon, joint capsule or bone Dressings from Most Occlusive to NonOcclusive Hydrocolloids Hydrogels Semipermeable foam Semipermeable film Impregnated gauze Alginates Traditional gauze Dressings from Most to Least Moisture Retentive Alginates Semipermeable foams Hydrocolloids Hydrogels Semipermeable films Topical Agents Used in Burn Care: Topical Agent Silver Sulfadiazine Silver Nitrate Povidone-iodine Mafenide Acetate Advantages -Can be used with or without dressings -Painless -Can be applied to wound directly -Broad-spectrum -Effective against yeast -Broad-spectrum -Non-allergenic -Dressing application is painless -Broad-spectrum -Penetrates burn eschar -May be used with or without occlusive dressings -Broad-spectrum -Penetrates burn eschar Disadvantages -Does not penetrate into eschar -Poor penetration -Discolors, making assessment difficult -Can cause severe electrolyte imbalances -Removal of dressings is painful -Not effective against pseudomonas -May impair thyroid function -Painful application -May cause metabolic acidosis -May compromise respiratory -May bused with or without occlusive dressings Gentamicin Nitrofurazone -Broad-spectrum -May be covered or left open to air -Bacteriocidal -Broad-Spectrum function -May inhibit epithelizlization -Painful application -Has caused resistant strains -Ototoxic -Nephrotoxic -May lead to overgrowth of fungus and pseudomonas -Painful application •Selective Debridement- involves the removal of only nonviable tissue. • Sharp Debridement- requires the use of a scalpel, scissors, and/or forceps to selectively remove devitalized tissue, foreign material or debris from a wound. Sharp debridement is most often used for wounds with large amounts of thick, adherent, necrotic tissue; however, it may be used in the presence of cellulitis or sepsis. • Enzymatic Debridement- refers to the topical application of an enzymatic preparation to necrotic tissue. Enzymatic debridement can be used on infected and non-infected wounds with necrotic tissue. Enzymatic debridement can be slow to establish a clean wound bed and should be discontinued once devitalized tissue is removed to avoid damage to adjacent healthy tissue. • Autolytic Debridement- refers to the use of the body’s own mechanisms to remove nonviable tissue. Common methods of autolytic debridement include the use of transparent films, hydrocolloids, hydrogels, and alginates. Autolytic debridement develops a moist wound environment that rehydrates necrotic tissue and eschar, facilitating enzymatic digestion of the nonviable tissue. •Non-selective Debridement- involves the removal of viable and nonviable tissue. •Wet-to-dry Dressings- refers to the application of moistened gauze dressing over an area of necrotic tissue. The dressing is allowed to dry completely and is later removed, along with any necrotic tissue that has adhered to the gauze. Wet to dry dressing are most commonly used on moderate amounts of exudate and necrotic tissue. This type of debridement should be used sparingly on wounds containing both necrotic and viable tissue since granulation tissue will be traumatized during the process. •Wound irrigation- Removes necrotic tissue from the wound bed using pressurized fluid. Pulsatile levage is an example of wound irrigation that uses a pressurized stream of irrigation solution. This type of debridement is most desirable for wounds that are infected or have loose debris. • Hydrotherapy- is most commonly employed using a whirlpool tank with agitation directed toward a wound requiring debridement. This process softens and loosens adherent necrotic tissue. PT must be aware of potential hydrotherapy side effects such as maceration of viable tissue, edema from dependent lower extremity positioning, and systemic effects such as hypotension. - Skin Care Products Therapeutic Moisturizers- Lotions are largely water-based and best used to replace skin moisture that has been lost either to the air or as a result of frequent hand washing. Creams are thicker water-based substances with higher concentrations of solids and oils than lotions. - Moisture Barriers- (e.g., ointment) Moisture barriers are designed to adhere to the skin and repel excess moisture from protected areas. They are frequently used to protect surrounding skin from a heavily draining wound or perineal tissue from exposure to incontinence. - Liquid Skin Portectants- (e.g., skin sealant) Liquid skin protectant is applied to skin and when dry it creates a thin plastic film protecting the skin from adhesive-related tissue damage. This thin barrier also offers some degree of moisture protection. - Skin Cleansers- skin cleansers are liquid agents typically intended for use on the skin of patients at risk of breakdown. Ingredients often have pH-balancing component that is especially beneficial for perineal cleansing in patients who are incontinent. - Wound Cleansers- Wound cleansers vary from simple saline solutions to more complex compositions with cytotoxicity. Many wound cleansers have the potential to cause inflammation; however, this quality is product dependent. Wound cleansers are not typically designed to remove necrotic tissue, but rather associated wound substances such as foreign materials, exudate and dried blood. Integumentary Interventions: Selective debridement: removal of only the nonviable tissues from a wound. Sharp Debridement: Requires the use of a scalpel, scissors, and/or forceps to selectively remove devitalized tissue, foreign material or debris from a wound. Sharp debridement is most often used for wounds with large amounts of thick, adherent, necrotic tissue, however, it may also be used in the presence of cellulitis or sepsis. Sharp debridement is the most expedient form of removing necrotic tissue. PTs are permitted to perform sharp, selective debridement as a procedural intervention. Enzymatic Debridement: Refers to the topical application of an enzymatic preparation Autolytic Debridement: to necrotic tissue. Enzymatic debridement can be used on infected and non-infected wounds with necrotic tissue. This type of debridement may be used for wounds that have not responded to autolytic debridement or in conjunction with other debridement techniques. Enzymatic can be slow to establish a clean wound bed and should be discontinued once devitalized tissue is removed to avoid damage to adjacent healthy tissue. Refers to the use of the body’s own mechanism to remove nonviable tissue. Common methods include the use of transparent films, hydrocolloids, hydrogels, and alginates. Autolytic debridement establishes a moist wound environment that rehydrates necrotic tissue and eschar, facilitating enzymatic digestion of the nonviable tissue. This type of debridement can be used with any amount of necrotic tissue, however, requires a longer healing period and should be not be performed on infected wounds. Non-selective Debridement (mechanical): involves the removal of both viable and nonviable tissue from a wound. Wet-to-dry dressings Refer to the application of a moistened gauze dressing over an area of necrotic tissue. The dressing is allowed to dry completely and is later removed, along with any necrotic tissue that has adhered to the gauze. Wet to dry dressings are most often used to debride wounds with moderate amounts of exudates and necrotic tissue. This type of debridement should be used sparingly on wounds containing both necrotic and viable tissue since granulation tissue will be traumatized in the process. Removal of dry dressings from granulation may cause bleeding and be extremely painful. Wound Irrigation Removes necrotic tissue from the wound bed using pressurized fluid. Pulsatle lavage is an example of wound irrigation that uses a pressurized stream of irrigation solution. This type of debridement is most desirable for wounds that are infected or have loose debris. Many devices permit Hydrotherapy variable pressure settings and provide suction for the removal of exudates and debris. Is most commonly employed using a whirlpool tank with agitation directed toward a wound requiring debridement. This process softens and loosens adherent necrotic tissue. PTs must be aware of potential hydrotherapy side effects such as maceration of viable tissue, edema from dependent LE positioning and systemic effects such as hypotension. Modalities & Physical Agents: Modality Indications Negative Pressure Chronic or acute Wound Therapy wounds which (NPWT): also cannot be closed referred to as by primary vacuum-assisted intention such as closure (V.A.C) is a dehisced surgical non-invasive incisions, fullwound care thickness wounds, modality used to partial-thickness facilitate healing burns, heavily and manage draining granular drainage. A sterile wounds, flaps, foam dressing is grafts, and most placed in the ulcer types. wound and sealed with an airtight secondary dressing which attaches via tubing to a vacuum pump with a reservoir container. Treatment Contraindications Malignancy within the wound, insufficient vascularity to sustain wound healing, large amounts of necrotic tissue with eschar present, untreated osteomyelitis, fistulas to organs or body cavities, exposed arteries or veins, and uncontrolled pain Advantages -Provides management of wound drainage -Maintains a moist wound environment -Decreases interstitial edema -Decreasees bacterial colonization -Increases capillary blood flow -Increases granular tissue formation -Enhances epithelial cell migration Disadvantages -Requires special supplies and training -Treatment can be painful -Not reimbursed in acute or long-term care settings protocols vary depending on wound characteriscis. Hyperbaric Oxygen: refers to the inhalation of 100% oxygen delivered at pressures greater than one atmosphere. Hyperbaric oxygen treatment is delivered in a closed chamber typically at pressures 2-3x that of the atmosphere, effectively reducing edema and hyperoxygenating tissues. Growth Factors: used in wound healing and are derived from naturally occurring protein factors. Osteomyelitis, diabetic wounds, crush injuries, compartment syndromes, necrotizing soft tissue infections, thermal burns, radiation necrosis, and compromised flaps and grafts. Terminal illness, untreated pneumothorax, active malignancy, pregnancy, seizure disorder, emphysema, and use of certain chemotherapy agents -Antibiotic effects -Stimulation of fibroblast production and collagen synthesis -Stimulation of growth factor release and epithelialization -Specialized equipment is not widely available -Cannot be used with active malignancy Neuropathic ulcers extending into or through subcutaneous tissue with adequate Wounds closed by primary intention, pts with known hypersensitivity to any component of the product or a -Adjunct to promote wound healing environment -Increases growth rate of new tissue -Costly -Poor reimbursement -Additional research is needed -Secondary These substances facilitate healing by stimulating the activity of specific cell types (neutrophils, endothelial cells, fibroblasts). Currently, only a limited number of growth factors have been approved by the FDA for topical wound healing applications. circulation to sustain wound healing. history of neoplasm at the application site. -Promotes cell division dressing required -Requires refrigeration -Limited number of products Burns: Pathophysiology: 1. Burn Injury: results from thermal, chemical, electrical, or radioactive agents 2. Burn wound, consists of 3 zones: a. Zone of coagulation: cells are irreversibly injured, cell death occurs b. Zone of stasis: cells are injured; may die without specialized treatment, usually within 24-48 hours c. Zone of hyperemia: minimal cell injury; cells should recover 3. Degree of burn: Burns are classified by severity, layers of skin damage Rule of 9’s: -Head and neck: 9% -Anterior trunk: 18% -Posterior trunk: 18% -Arms: 9% each -Legs: 18% each -Perimeum: 1% Classification by percentage of body area burned: 1. Critical: 10% of body with third degree burns and 30% or more with second degree burns; complications common (respiratory involvement, smoke inhalation) 2. Moderate: less than 10% with third-degree burns and 15% to 30% with second degree burns. 3. Minor: less than 2% with third degree burns and 15% with second degree burns. Complications of burn injury: 1. Infection: leading cause of death; gangrene may develop 2. Shock 3. Pulmonary complications: Smoke inhalation of hot smoke results in pulmonary edema and airway obstruction; suspect with burns of the face, singed nose hairs; pneumonia 4. Metabolic complications 5. Cardiac and circulatory complications 6. Integumentary scars Burn Management: 1. Emergency care: Immersion in cold water. If less than half the body is burned and injury is immediate; cold compresses may also be sued. Cover burns with sterile bandage or clean cloth; no ointments or creams. 2. Medical management a. Asepsis and wound care: b. Removal of charred clothing c. Wound cleansing d. T e. Topical medications reapplied one to 3 times daily (Ointments: bacitracin, polymyxin B, and Neomycin); Silver sulfadiazine: common topical agent, avoid at term pregnancy, on infants less than 2 months, and those with sulfa drug allergies. f. Dressings: prevents bacterial contamination, prevents fluid loss, and protects the wound. May additionally limit ROM. Dressings include: silver-impregnated, and gauze dressing g. Estabiilsh and maintain airway, adequate oxygenation, and respiratory function h. Monitor: arterial blood gases, serum electrolyte levels, urinary output, vital signs i. j. k. l. m. GI function: provide nutritional support Pain relief: morphine sulfate Prevention and control of infection: tetanus prophylaxis, antibiotics, standard precatution Fluid replacement therapy: prevention and control of shock. Post shock fluid and blood replacement Surgery: Grafts closure of the wound i. Allograft (homograft)-use of other human skin; cadaver skin; temporary grafts for large burns, used until autograft is available ii. Xenograft (heterograft)-use of skin from other species (pig skin) a temporary graft iii. Biosynthetic grafts: combination of collagen and synthetics iv. Cultured skin: laboratory grown form pts own skin v. Autograft: use of pts own skin vi. Split-thickness graft: contains epidermis and upper layers of dermis from donor site vii. Full-thickness graft: contains epidermis and dermis from donor site Rehab: Prevent or reduce the complications of immobilization. 1. Exercises to promote deep breathing and chest expansion; ambulation to prevent pneumonia 2. Positioning and splinting to prevent or correct deformities. a. Anterior neck: common deformity is flexion; stress hyperextension; position with firm (plastic) cervical orthosis b. Shoulder: common deformity is adduction and internal rotation; stress abduction, flexion, and external rotation; position with an axillary splint (airplane splint). c. Elbow: common deformity is flexion and pronation in extension with posterior arm splint. d. Hand: common deformity is a claw hand (intrinsic minus position); stress extension (15°), MP flexion (70°), PIP, and DIP extension, thumb abduction (intrinsic plus position) with resting hand splint. e. Hip: common deformity is flexion and adduction; stress hip extension and abduction; position in extension, abduction, neutral rotation. f. Knee: common deformity is flexion; stress extension; position in extension with posterior knee splint. g. Ankle: common deformity is plantar flexion; stress dorsiflexion; position with foot-ankle in neutral with splint or plastic ankle-foot orthosis. 3. Edema control: elevation of extremities, active ROM. 4. Active and passive exercise to promote full ROM. a. Combine with dressing changes, hydrotherapy; medication doses b. Post grafting: discontinue exercise for 3-5 days to allow grafts to heal c. Massage to help reduce scar formation; eg deep friction massage d. Resistive and strengthening exercises to correct loss of muscle mass and strength. e. Increase activity tolerance and cardiovascular endurance (ambulation) f. Promote independence in ADLs, all functional mobility skills g. Elastic supports to help control edema; pressure garments to help prevent hypertrophic scarring or keloid formation h. Management of chronic pain. 5. Provide emotional support 1. Edema management: a. Leg elevation and exercise (ankle pumps) b. Compression therapy; to facilitate movement of excess fluid from lower extremity c. Compression wraps: elastic or tubular bandages d. Paste bandages; Unna boot is a pliable, nonstretchable dressing impregnanted with ainc or calamine and gelatin e. Compression stockings, e.g. Jobst f. Compression pump therapy 2. Electrical Stimulation for wound healing: a. Used to improve circulation, facilitate debridement, and enhance tissue repair b. Continuous waveform application with direct current c. High-voltage pulsed current d. Pulsed biphasic current 3. Nutritional considerations: a. Delayed wound healing associated with malnutrition and poor hydration b. Albumin: normal is 3.5-5.5 mg/dl; less than 3.5=malnutrition c. BMI <21 with weight loss increased risk for pressure ulcer d. Provide adequate hydration e. Individuals with wounds require approximately 3 or more liters of water a day f. Pts on air-fluidized beds require greater hydration (40-60 ml/Kg a day) g. Provide adequate nutrition: frequent high calorie/high-protein meals; energy intake (25-35 kcal/kg/bodyweight) and protein 1.52.5 gm/kg body weight) h. Patients with trauma stress and burns require higher intakes. 4. Injury prevention or reduction a. Daily, comprehensive skin inspection, paying particular attention to bony prominences (sacrum, coccys, trochanter, ischial tuberosities, medial and lateral malleolus) b. Therapeutic positioning to relieve pressure and allow tissue reperfusion. i. In bed: turning or repositioning every 2 hours during acute and rehab phases ii. In wheelchair: wheelchair pushups every 15 minutes c. Use techniques to ensure skin protection, avoid friction, shear, or abrasion injury i. Lifting, not dragging ii. Use of turning and draw sheets; trapeze, manual, or electric lifts iii. Use of corn starch, lubricants, pad protectors, thin film dressings, or hydrocolloid dressings over friction risk sites. iv. Use of transfer boards for sliding wheelchair transfers d. Pressure-relieving devices (PRDs): i. Reduce tissue interface pressures ii. Static devices: use if pt can assume a variety of positions, examples: foam, air, or gel mattress overlays; whater-filled mattresses; pillows or foam wedges, protective padding (heel relief boots) iii. Dynamic devices: use if pt cannot assume a variety of positions; examples: alternating pressure air mattresses, fluidized air or high-air-loss bed. iv. Seating supports: use for chair-bound or wheelchair bound pts; examples: cushions made out of foam, gel, air, or some combination e. Avoid restrictive clothing; e.g. with rough textures, hard fasteners, and studs. Avoid tight-fitting shoes, socks, splints, and orthoses. f. Avoid maceration injury i. Prevent moisture accumulation and temperature elevation where skin contacts support surface. ii. Incontinence management strategies: use of absorbent pads, brief or panty pad, scheduled toileting, and prompted voiding, ointments, creams, and skin barriers prophylactically in perineal and perianal areas. g. Pt and caregiver education: i. Mechanisms of pressure ulcer development ii. iii. iv. v. vi. vii. Daily skin inspection and hygiene Avoidance of prolonged positions Repositioning, weight shifts, lifts Safety awareness during self-care Safety awareness with use of devices and equipment Importance of ongoing activity/exercise program Metabolic and Endocrine Systems: The metabolic system governs the chemical and physical changes that take place within the body enabling it to grow and function. Metabolism involves breakdown of the body’s complex organic compounds in order to generate energy for all bodily processes. It also generates energy for the synthesis of complex substances that form tissues and organs. During metabolism, organic compounds are broken down by a process called catabolism, while anabolism is the process that combines simple molecules for tissue growth. Many metabolic processes are facilitated by enzymes. The overall speed at which an organism carries out its metabolic processes is termed its metabolic rate (or when the organism is at rest, its basal metabolic rate). Metabolic System Pathology: Metabolic disorders are classified by the particular building block that is affected. An enzyme deficiency leads to accumulation of the substrate and a subsequent deficiency in the intended enzyme’s product. There are many different disorders that can occur genetically and these are grouped according to the substrate that has been affected (carbohydrates, amino acids). Inherited metabolic disorders can be diagnosed in utero via aminocentesis or chorionic villus sampling. Many inherited metabolic disorders will produce symptoms in a newborn including lethargy, apnea, poor feeding, tachypnea, vomiting, hypoglycemia, urine changes, and seizures. Symptoms that are immediately apparent indicate a more dangerous disorder. Pathology Phenylketonuria (amino acid/organic acid What is it Phenylketonuria (PKU) is a syndrome that Etiology This is an autosomal recessive inherited Signs & Symptoms Symptoms will typically present within a few Treatment Treated through dietary restriction of phenylalaine metabolic disorder consist of mental retardation as well as behavioral and cognitive issues secondary to an elevation of serum phenylalanine. There is a deficiency in the enzyme phenylalanine hydroxylase. Normally, excessive phenlalanine is converted to tyrosine by phenylalanine hydroxylase. When this process does not occur and there is an excess of phenylalanine, the brain is the primary organ that becomes affected. Children in the US are tested at birth for PKU and levels greater than 6mg/dl of phenylalanine require some form trait and is most common in Caucasian populations months of birth as the phenylalanine accumulates. If left untreated, severe mental retardation will occur. These children may also experience gait disturbances, hyperactivity, psychoses, abnormal body order, and display features that are lighter in coloring when compared to other family memberse. throughout the person’s lifetime. Adequate prevention will avoid all manifestations of the disease. Tay-Sachs Disease (lysosomal storage disorder) Mitochondrial Disorders of treatment. Is the absence or deficiency of hexosaminidase A. This produces an accumulation of gangliosides (GM2) within the brain. There are over 100 different forms of mitochondrial disease and each produces a different spectrum of disability and clinical manifestations. This disease is an autosomal recessive inherited trait and carried primarily in the Eastern European (Ashkenazi) Jewish population. Result from genetically inherited or spontaneous mutations in the DNA that lead to impaired function of proteins found within the mitochondria. At approx. 6 months of age, the child will start to miss developmental milestones and will continue to deteriorate in motor and cognitive skills. As symptoms progress, the pt develops significant mental retardation and paralysis, and will usually die by the age of 5. Symptoms vary depending on the type of mitochondrial disorder, however, can include loss of muscle coordination, muscle weakness, visual and hearing problems, learning disabilities, hear, liver and kidney disease, respiratory, There is currently no effective treatment for this condition. Genetic testing in high risk populations to identify the carriers prior to pregnancy is important in order to avoid this disorder. These diagnoses are relatively new and treatment is varied as the symptomatology and presentation of the disease. Treatment is aimed at alleviating the current symptoms and slowing the progression of the disease process. Wilson’s Disease (hepatolenticular degeneration) Wilson’s disease is a rare inherited disorder that is most common in eastern Europeans, Sicilians, and southern Italians, but may occur in any group. Wilson’s disease typically appears in people under 40 years old and symptoms can develop in children typically between 4-6 years of age. An autosomal recessive inherited trait that produces a defect in the body’s ability to metabolize copper. The copper accumulates over time within the brain, liver, cornea, kidney, and other tissues. neurological, and GI disorders, and dementia. Symptoms typically appear between the ages of 4 and 6 and include KayserFleischer rings surrounding the iris of the eye secondary to copper deposits, degenerative changes in the brain (especially with the basal ganglia), hepatitis, cirrhosis of the liver, athetoid movements, and ataxic gait patterns. There may also be emotional and behavioral changes as the copper continues to accumulate. Overtime, and with severe disease, there will be deformities of the MS system, Treatment consist of continual pharmacological intervention using vitamin B6 and Dpenicillamine as both promote the excretion of excess copper form the body. Treatment will also focus on prevention of hepatic disease since a pt will die from hepatic failure if the condition is left untreated. pathologic fractures, osteomalacia, muscle atrophy, and contractures. Acid-Base Metabolic Disorders: The process of metabolism is regulated by the endocrine and nervous systems. The rate of metabolism can be influenced by body temperature, exercise, hormone activity, and digestion activity. If proper fluid or acid-base balance is compromised, it can alter metabolic function and cause many signs and symptoms of the dysfunction. Disorder Metabolic Alkalosis What is it Is a condition that occurs when there is an increase in bicarbonate accumulation or an abnormal loss of acids. As a result, the pH rises above 7.45. Etiology Commonly occurs when there has been continuous vomiting, ingestion of antacids or other alkaline substances or diuretic therapy. It may also be associated with hypokalemia or nasogastric suctioning. Metabolic Acidosis Is a condition that occurs when there is an accumulation Commonly occurs with conditions such as renal Signs & Symptoms Nausea, diarrhea, prolonged vomiting, confusion, muscle fasciculations, muscle cramping, neuromuscular hyperexcitability, convulsions, paresthesias, and hypoventilation. If left untreated the pt can become comatose, experience seizures, and respiratory paralysis. Symptoms include compensatory hyperventilation, Treatment The most important interventions include managing the underlying cause, correcting coexisting electrolyte imbalances, and administering potassium chloride to the pt. Managing the underlying cause, correcting any of acids due to an acid gain or bicarbonate loss. As a result, the pH drops below 7.35. failure, lactic acidosis, starvation, diabetic or alcoholic ketoacidosis, severe diarrhea or poisoning by certain toxins. vomiting, diarrhea, headache, weakness, and malaise, hyperkalemaia, and cardiac arrhythmias. If left untreated the continued increase in acid can induce coma and eventual death. coexisting electrolyte imbalances, and administering sodium bicarbonate. Other Metabolic conditions: Osteomalacia, Osteoporosis, Paget’s Disease (SEE Other chart) Metabolic System Terminology: Aerobic metabolism: Anabolism: Adenosine Triphosphate (ATP): Catabolism: The ATP producing metabolic processes that are dependent on oxygen transported via the circulatory system. Aerobic metabolic functions typically provide energy for low intensity and/or longer duration activities. The metabolic process in which simple molecules (nucleic acids, polysaccharides, amino acids) are combined to create the complex molecules (proteins) needed for tissue and organ growth. The molecular unit within the body which transports the chemical compounds used for cellular metabolism. The metabolic process in which complex materials (proteins, lipids) are broken down in the body for the purpose of creating and releasing heat and energy. DNA A double helix molecule that contains the genes that provide the blueprint for all of (deoxyribonucleic the structures and functions of a living bening. acid): Gene: Metabolism: Mitochondria: Osteopenia: Osteopetrosis: pH: Pathology Breast Cancer A fundamental unit of heredity. The physical and chemical processes of cells burning fuel to produce and use energy. Examples include digestion, elimination of waste, breathing, thermoregulation, muscular contraction, brain function, and circulation. The part of the cell that is responsible for energy production. The mitochondria are also responsible for converting nutrients into energy and other specialized tasks. A condition presenting with low bone mass that is not severe enough to qualify as osteoporosis. Individuals with osteopenia may not have actual bone loss, but a naturally lower bone density than established norms. A group of conditions characterized by impaired osteoclast function which causes bone to become thickened but fragile. Osteopetrosis is an inherited condition that can vary widely in symptoms and severity. A measure of the hydrogen ion concentration in body fluid. Diagnosis Contributing Factor A mass that is Estrogen is composed of believed to malignant have some altered cells relationship to that proliferate the disease and spread process. Risk without factors include control. A gender, age, malignancy can young occur menarche, late anywhere menopause, within the family history, breast tissue, high alcohol however, the intake, high fat lump is usually diet, radiation found directly exposure, and behind the past history of areola in men cancer. Males Clinical Presentation Breast cancer makes up approx. 30% of all female cancers and is the 2nd leading cause of death in female cancers. Approx 70% of all breast cancer occurs in women over the age of 50. A pt will present with a lump in the breast that is Lab/Imaging Management/Outcome Mammography is used to detect the location and growth of a mass, however definitive diagnosis of breast cancer is made only after microscopic examination of a suspected mass by needle or excision biopsy. Ultrasound can Surgical management may range from excision of the mass (lumpectomy) to total radical mastectomy with axillary dissection. Chemotherapy, radiation therapy, and hormone therapies may used. PT may be indicated to assist with lymphedema management, postsurgical breathing exercises, positioning, pain management, strengthening and exercises, ROM, and is usually located behind the areola or in the outer upper quadrant of the breast in women. There may or may not be generalized discomfort in the area. account for less than 1% of all breast cancer cases. noticed by a physician (10%), or by the pt through self examination (90%). Breast cancer is initially otherwise asymptomatic. The breast may become painful, change shape, bleed from the nipple, and dimple over the area of the mass. Metabolic/Endocrine System Rehab: Rehab Considerations for pts with Inherited Metabolic disorders: -Must have an awareness of dietary restrictions -Pt and family training to prevent deleterious effects from the metabolic disease -Adapt treatment to facilitate developmental milestones within pt tolerance Rehab Considerations for pts with Acid-base disorders: -Recognize higher risk populations for imbalances such as pts with renal, cardiovascular, pulmonary disease; also be used to detect if a lump is filled with fluid or a solid mass. Sentinel lymp node mapping is used upon diagnosis to identify exact lymph node involvement. massage, intermittent compression, and pt education. The risk of recurrence is always present and should be monitored closely. Overall prognosis and ten-year survival rates for women are over 85% for stage I disease; 66% for stage II; 36% for stage III; and 7% for stage IV disease. burns, fever and sepsis; pts on mechanical ventilation; diabetes mellitus; pts currently vomiting with diarrhea or enteric drainage -Recognize signs of dehydration in a diabetic pt -Injury prevention during involuntary muscular contractions secondary to metabolic alkalosis -Recognize that pts using diuretic therapy may be at risk for potassium depletion -Recognize that Trousseau’s sign during blood pressure measurements may indicate calcium deficiency and the early stages of tetany Rehab considerations for pts with metabolic bone disease: -Must have awareness of signs of compression fx and of pts at higher risk for all forms of fx -Focus on both resistance training and endurance training to build bone density and increase strength -Avoid treatments that exacerbate the condition or place pts at risk for fx Rehab considerations for pts with Pituitary Dysfunction: -Ambulation/exercise encouraged within 24 hours of surgery (post tumor/gland removal) -Must demonstrate increased awareness for signs of hypoglycemia -Bilateral carpal tunnel syndrome, arthritis, osteophyte formation are common with hyperpituitarism -Orthostatic hypotension may be present with hypopituitarism -Bilateral hemianopsia that can occur with hypopituitarism requires special consideration during treatment Rehab considerations for pts with adrenal dysfunction: -Recognize signs of stress or exhaustion and avoid treatments that exacerbate the condition -Notify the physician with any signs of illness or increased intracranial pressure (papilledema), medications may need to be altered -Orthostatic hypotension is common secondary to long term cortisol therapy -Report sleep disturbances to the physician -Increased incidence of osteoporosis, bone fx, degenerative myopathy, tendon ruptures, ataxic gait -delayed wound healing may be common Rehab considerations for pts with thyroid dysfunction: -Recognize reduced exercise capacity and fatigue are typical -Avoid treatments that exacerbate the condition such as exercise in a hot acquatic or gym setting due to heat intolerance (Graves’ disease) -Avoid cardiovascular stress to eliminate secondary complications from hypotension, goiter, Graves’ disease -Provide close monitoring of vital signs -Recognize the effects of radioiodine therapy -Recognize the risk of rhabdomyolysis (hypothyroidism) Rehab considerations for pts with parathyroid dysfunction: -Must be familiar with all signs and symptoms of parathyroid dysfunction in order to refer pts to a physician if a change in their status occurs -Recognize symptoms of excessive or inadequate pharmacological treatment and side effects of the agents -Avoid treatments that exacerbate the condition -Recognize effects of hypercalcemia (hyperparathyroidism) and hypocalcemia (hypoparathyroidism) -Recognize the increased risk for fractures and effects form osteogenic synovitis (Achilles, triceps, and obturator tendons most affected) Rehab considerations for pts with DM: -Recognize the risk for peripheral neuropathies, small vessel angiopathy, tissue ischemia and ulcerations, impaired wound healing, tissue necrosis, and amputation -Recognize acute metabolic changes -Recognize the signs of sudden hypoglycemia and necessary treatment -Focus on consistent management of insulin intake, diet, and physical activity -Provide education on proper skin care, shoe evaluation, and shoe wear Endocrine System The endocrine system consists of endocrine glands (specialized ductless glands) that secrete hormones that travel through the bloodstream to signal specific target cells throughout the body. The hormones travel throughout the body to the target organs upon which they act. They will bind selectivity to receptor sites on the surface of the receptor cells. The endocrine system and nervous system both function to achieve and maintain stability of the internal environment (homeostasis). The systems are capable of working alone or in concert with each other. The endocrine and nervous systems work together to regulate metabolism, response to stress, sexual reproduction, blood pressure, and water & salt balances. Endocrine System -Secreting cells send hormones throught the bloodstream to signal specific target cells -Hormones diffuse into the blood and travel long distances to virtually every area of the body -Endocrine effectors consist of virtually all tissues -Regulatory effects are slow and tend to last for long periods Nervous System -Neurons secrete neurotransmitters to signal nearby cells that have an appropriate receptor site -Neurotransmitters are sent very short distances across a synapse -Nervous effectors are limited to muscle and glandular tissue -Regulatory effects appear rapidly and are often short lived Glands of the Endocrine System: Hypothalamus Is part of the diencephalon located below the thalamus and cerebral hemisphere. The hypothalamus connects to the pituitary gland through the infundibular or pituitary stalk. If it responsible for regulation of the autonomic nervous system (body temp, appetite, sweating, thirst, sexual behavior, rage, fear, blood pressure, sleep) and other endocrine glands thorough its impact on the pituitary gland. Pituitary Gland Normally the size of a pea and is located at the base of the brain just beneath the hypothalamus. The pituitary gland consists of two separate glands, the adenophypophysis (anterior) and the neurohypophysis (posterior). The pituitary gland is considered the most important part of the endocrine system since it releases hormones that regulate several other endocrine glands. This “master gland” is influenced by factors such as seasonal changes or emotional stress. The pituitary gland secrets endorphins that act on the nervous system and reduce a person’s sensitivity to pain. It also controsl ovulation and works as a catalyst for the testes and ovaries to create sex hormones. Thyroid Gland Is located on the anterior and lateral surfaces of the trachea immediately below the larynx and is shaped like a “bow tie” or butterfly with two halves (lobes); a right lobe and left lobe joined by an isthmus. The thyroid produces thyroxine and triiodothyronine that act to control the rate at which cells burn the fuel from food. An increase in thyroid hormones will increase the rate of the chemical reactions within the body. Parathyroid There are 4 parathyroid glands found on the posterior surface of the thyroid’s lateral Glands Adrenal Glands Pancreas Ovaries Testes lobes. These glands produce parathyroid hormone, which functions as an antagonist to calcitonin and is important for the maintenance of normal blood levels of calcium and phosphate. Parathyroid hormone increases the reabsorption of calcium and phosphate from bones to the blood. Secretion of parathyroid hormone is stimulated by hypocalcemia and inhibited by hypercalcemia. Normal clotting, neuromuscular excitability, and cell membrane permeability are dependent on normal calcium levels. The two adrenal glands are located on top each kidney; the outer portion is called the adrenal cortex and the inner portion is called the adrenal medulla. The adrenal cortex and the adrenal medulla secrete different hormones. The adrenal cortex produces corticosteroids that will regulate water and sodium balance, the body’s response to stress, the immune system, sexual development and function, and metabolism. The adrenal medulla produces epinephrine that increases heart rate and blood pressure when there is an increase in stress. The pancreas is located in the upper left quadrant of the abdominal cavity, extending from the duodenum to the spleen. The pancreas includes both endocrine and exocrine tissues. The islets of Langerhans are the hormone-producing cells of the pancreas. Alpha cells produce glucagon and beta cells produce insulin. These hormones work in combination to ensure a consistent level of glucose within the bloodstream and properly maintain stores of energy within the body. The ovaries are located in the pelvic cavity on each side of the uterus. The ovaries provide estrogen and progesterone that contribute to regulation of the menstrual cycle and pregnancy. Estrogen is secreted by the ovarian follicles that is responsible for the development and maintenance of female sex characteristics such as breast development and the cycles of the female reproductive system. Progesterone is produced by the corpus luteum and functions to maintain the lining of the uterus at a level necessary for pregnancy. The testes are located in the scrotum between the upper thighs. The testes secrete androgens (most importantly testosterone) that regulate body changes associated with sexual development and support the production of sperm. Endocrine System: Hormone, Function, & Regulation of Secretion Hypothalamus: Hormone Function Growth hormone-releasing Increases the release of growth hormone Target: pituitary gland hormone Growth hormone-inhibiting Decreases the release of growth hormone Target: pituitary gland hormone Gonadotropin-releasing Increases the release of hormone Target: pituitary gland luteinizing hormone and folliclestimulating hormone Thyrotropin-releasing hormone Increases the release of thyroid Target: pituitary gland stimulating hormone Corticotropin-releasing hormone Increases the release of Target: pituitary gland adrenocorticotropic hormone Prolactin-releasing hormone Stimulates the release of Target:pituitary gland prolactin Prolactin-inhibitory factor; Decreases the release of dopamine Target: pituitary gland prolactin Regulation of Secretion CNS feedback; circulating levels of hormones CNS feedback; circulating levels of hormones CNS feedback; circulating levels of hormones CNS feedback; circulating levels of hormones CNS feedback; circulating levels of hormones CNS feedback; circulating levels of hormones CNS feedback; circulating levels of hormones Pituitary: Hormone Growth Hormone Target: bone and muscle Follicle-stimulating hormone Target: ovaries and testes Luteinizing hormone Target: ovaries and testes Function Promotes growth and development; increases the rate of protein synthesis Promotes follicular development and the creation of estrogen in females; promotes spermatogenesis in males Promotes ovulation along with estrogen/progesterone synthesis from the corpus lutem in females; promotes testosterone synthesis in males Regulation of Secretion Hypothalamus Hypothalamus Hypothalamus Thyroid-stimulating hormone Target: thyroid gland Adrenocorticotropic hormone Target: adrenal cortex Prolactin Target: mammary glands Oxytocin Target: uterus and mammary glands Antidiuretic hormone Target: kidneys Adrenal Cortex: Hormone Adrogen Target: ovaries and testes Aldosterone (mineralocorticoid) Target: kidneys Cortisol (glucocorticoid) Target:GI system Adrenal Medulla: Hormone Epinephrine Target: cardiovascular and metabolic systems Increases the synthesis of thyroid hormones T3 and T4 Increases cortisol synthesis (adrenal steroids) Allows for the process of lactation Increases contraction of uterine muscles; promotes release of milk from mammary glands Increases water reabsorption; conserves water; increases blood pressure through stimulating contraction of muscles in small arteries Hypothalamus Function Increases masculinization; promotes growth of pubic hair in males and females Increases reabsorption of sodium ions by the kidneys to the blood; increase excretion of the potassium ions by the kidney into the urine Influences metabolism of food molecules; anti-inflammatory effect in large amounts Regulation of Secretion Influenced by the hypothalamic production and release of GnRH and Luteinizing hormone (LH) Low blood sodium level; high blood potassium level Function Increases heart rate and force of contraction; increases energy production; vasodilation in skeletal muscle Regulation of Secretion Sympathetic impulses form the hypothalamus in stress situation Hypothalamus Hypothalamus Nerve impulses from the hypothalamus; stretching of the cervix; nipple stimulation Decreased water content Adrenocorticotrophic hormone Norepinephrine Target: cardiovascular and metabolic systems Vasoconstriction in skin, viscera, and skeletal muscles Sympathetic impulses form the hypothalamus in stress situation Function Involved in the regulation of the female reproductive system and female sexual characteristics Regulation of Secretion Cyclical rise and fall of hormone levles Function Increases blood glucose by stimulating the conversion of glycogen to glucose Decreases blood glucose and increases the storage of fat, protein, and carbs Regulation of Secretion Hypoglycemia Function Increases blood calcium Regulation of Secretion Influenced by pituitary release of LH Function Involved in the process of spermatogeneiss and male sexual characteristics Regulation of Secretion Influenced by pituitary release of LH Function Involved with normal Regulation of Secretion Thyroid-stimulating hormone Ovaries: Hormone Estrogen, progesterone Target: uterus and mammary glands Pancreas: Hormone Glucagon Targets: liver Insulin Targets: all body systems Parathyroids: Hormone Parathormone Targets: bone, kidney, intestinal mucosa Hyperglycemia Testes: Hormone Testosterone Target: pituitary gland Thyroid: Hormone Thyroxine (T4), Triiodothyronine (T3) Targets: all tissues Calcitonin Targets: plasma development, increases cellular level metabolism Increases calcium storage in bone; decreases blood calcium levels Hypercalcemia Endocrine System Pathology: The endocrine system is multifaceted and can develop pathology in one or more areas due to hyperfunction or hypofunction or one or more glands. In many instances, it is the hypothalamus or the pituitary gland that affects the function of other endocrine glands when they experience direct or indirect dysfunction. Hyperfunction of an endocrine gland: usually secondary to overstimulation of the pituitary gland. This can also occur due to hyperplasia or neoplasia of the gland itself. Hypofunction of an endocrine gland: usually secondary to understimulation of the pituitary gland. This can also occur from congenital or acquired disorders. Hypopituitarism: This condition occurs when there is a decreased or absent hormonal secretion form the anterior pituitary gland. This is a rare disorder and symptoms are dependent on the age of the effected person and deficit hormones. Typical disorders may include short stature (dwarfism), delayed growth and puberty, sexual and reproductive disorders, and diabetes insipidus. Treatment is also based on the deficit hormones and usually includes pharmacolocial replacement therapy. Hyperpituitarism: This condition occurs when there is an excessive secretion of one or more hormones under the pituitary gland’s control (frequently growth hormone that produces acromegaly in adults). Disorders and symptoms are dependent on the hormone(s) that are affected. Some disorders include gigantism or acromegaly, hirutism galactorrhea (abnormal lactation in males or females), amenorrhea, infertility, and impotence. Treatment is hormone and site dependent and can include tumor resection, surgery, radiation therapy, and hormone suppression or replacement (if gland becomes dysfunctional after treatment) Pathology Addison’s Disease What is it Is a form of adrenal dysfunction that presents with Etiology When the adrenal cortex produces insufficient cortisol and aldosterone Signs & Symptoms Symptoms include a widespread metabolic dysfunction Treatment Primarily consists of long-term pharmacolocial intervention using Cushing’s Syndrome hyopfunction of hormones it is the adrenal cortex. termed Addison’s Subsequently, disease there is decreased production of both cortisol (glucocorticoid) and aldosterone. secondary to cortisol deficiency as well as fluid and electrolyte imbalances secondary to aldosterone dysfunction. The person may experience hypotension, weakness, anorexia, weight loss, altered pigmentation, and if left untreated this condition will result in shock and possible death. When the pituitary Symptoms evolve gland produces over years and can excessive include persistent adrenocorticotrophic hyperglycemia, hormone (ACTH) growth failure, with subsequent truncal obesity, hyper cortisolism, it purple abdominal is termed Cushing’s striae, moon disease. shaped face, buffalo hump posteriorly at the base of the neck, weakness, acne, hypertension, and male synthetic corticosteroids and mineralocorticoids. Is a form of adrenal dysfunction that presents with hyperfunction of the adrenal gland, allowing for excessive amounts of cortisol (glucocorticoid) production. Treatment may include pharmacological intervention to block production of the hormones, radiation therapy, chemo or surgery. Graves’ Disease Is the most specific cause of hyperthyroidism. Graves’ disease is most common in women over the age of 20, however, it occurs in men as well and can affect any age group Is caused by an autoimmune disease in which certain antibodies produced by the immune system stimulate the thyroid gland causing it to become overactive gynecomastia. Mental changes can include depression, poor concentration, and memory loss. Symptoms are consistent with hyperthyroid presentation. The classic signs of Graves’ disease include mild enlargement of the thyroid gland (goiter), heat intolerance, nervousness, weight loss, tremor, and palpitations. Also seen, enlargement in the area of the Adam’s apple resulting in difficulty eating and episodes of dyspnea, Abnormal protrusion of the eyes. Management includes pharmacological intervention and/or removal of the thyroid gland using radiation or surgical intervention. Hypothyroidism Depression/anxiety, increased lethargy, fatigue, headache, slowed speech, slowed mental function, impaired short-term memory Proximal muscle weakness, carpal tunnel syndrome, trigger points, myalgia, increased bone density, cold intolerance, paresthesias Dyspnea, bardycardia, CHF, respiratory muscle weakness, decreased peripheral circulation, angina, increase in cholesterol Anorexia, constipation, weight gain, decreased absorption of food and glucose Infertility, irregular menstrual cycle, increased menstrual bleeding Hyperthyroidism Tremors, hyperkinesis, nervousness, increased DTRs, emotional lability, insomnia, weakness, atrophy Hypoparathyrodism ↓bone resorption Hypocalcemia Elevated serum phosphate levels Shortened 4th and 5th metacarpals Hyperparathyroidism ↑ bone resorption Hypercalcemia Decreased serum phosphate levels Osteitis fibrosa, subperiosteal resorption, arthritis, bone deformity Nephrocalcinosis, renal hypertension, and significant renal damage Compromised breathing due to intercostal muscle and diaphragm spasms Cardiac arrhythmias and potential heart failure Increased NM activity that can result in tetany Chronic periarthritis, heat intolerance, flushed skin, hyperpigmentation, increased hair loss Tachycardia, palpitations, increased respiratory rate, increase in blood pressure, arrhythmias Hypermetabolism, increased appetite, increased peristalsis, nausea, vomiting, diarrhea, dysphagia Polyuria, infertility, increased first trimester miscarriage, amenorrhea Gout Decreased NM irritability Pancreas Dysfunction: Pathology Diagnosis Diabetes Mellitus Type 1 Persistent hyperglyce mia due to diminished or absent production of insulin. In type 1 DM, insulin is functionally absent due to the destruction of beta cells of the pancreas where the insulin would normally be produced. Contributing Factor Unknown, however there are several theories. It is an autoimmune process with strong genetic component. It is also believed that the genetic predispositio n in combination with an unknown factor, potentially environment al, triggers the ongoing cycle of destruction of the beta cells of the pancrease. Clinical Presentatio n Usually starts in children ages 4 or older, with the peak incidence of onset at 1113 years. A relatively high incidence also exists in people in their late 30s and early 40s. Common symptoms are polyuria, polydipsia, and polyphagia, along with nausea, weight loss, fatigue, blurred vision and dehydration Lab/Imaging Management/outco me A test of blood glucose levels will be necessary. Other testing includes urinalysis for glucose, ketones, and protein and a white blood cell count as well as blood and urine cultures to rule out infection. Usually require insulin via continuous pump or self-administered injection. Exercise is an important aspect in management of DM. Pts should exercise at 50-60% of their predicted maximum HR. Type 1 DM is associated with a high morbididty and premature mortality rate due to complications such as ischemic heart disease, PVD, chronic renal disease, reduced visual acuity and blindness. Type II DM This form of DM typically occurs in the population over the age of 40, however, there has been an increase in children diagnosed with type 2 secondary to a rise in obesity. This form of DM typically retains the ability to Type 2 DM occurs secondary to an array of dysfunctions resulting from the combination of resistance to insulin action and inadequate insulin secretion. This disorder is characterize d by hyperglycem ia when the body cannot . A fasting glucose reading of 126 mg/dl is also a sign of DM. This disease onset is usually sudden or within a short period of time. Obesity is found to contribute to this condition by increasing insulin resistance. Symptoms are relatively the same as with type 1, however, ketoacidosis does not occur since insulin is still typically produced. Treatment of type 2 DM includes blood glucose control through diet, exercise, oral meds, or insulin injections when necessary. Systemic Lupus Erythematosus produce some endogenous insulin. SLE is a connective tissue disorder caused by an autoimmun e reaction in the body. The primary manifestatio n of the condition is the production of destructive antibodies that are directed in the individual’s own body. The chronic inflammator y disorder produces a variety of symptoms depending properly respond to insulin. Genetic, environment al, viral, and hormonal contributing factors. Environment al include ultraviolet light exposure, infection, antibodies (penicillin and sulfa drugs), extreme stress, immunizatio n, and pregnancy. SLE can occur at any age, but the most common age group is 1540 years. More common in Diverse symptoms based on the involvement of the connective tissue throughout the body. Symptoms such as arthralgias, malaise and fatigue may persist even during a remission period. Common clinical presentatio n is butterfly rash across the cheeks and nose, red rash over light exposed areas, Microscopic fluorescent techniques are indicated to detect the presence of the antinuclear antibody (ANA) within the blood. A positive ANA test warrants an additional test for antideoxyribonu cleic acid antibodies. These two tests in combination with physical presentation support the presence of SLE. Focuses on revering the autoimmune response in order to avoid complications and exacerbations of symptoms. PT intervention is usually indicated after a period of exacerbation and includes a slow resumption of physical activities, energy conservation techniques, gradual endurance activities, and significant pt education regarding skin care, pacing, exercise, and strengthening. Human Immunodeficie ncy Virus on the severity and extent of involvement . women. Is a retrovirus that initially invades and destroys cells within the immune system; specifically CD4+ Tlymphocytes (t-cells). This virus also affects monocytes, macrophage s, and Bcells. Once the T-cells decrease beyond a specific level a pt will HIV is transmitted through contact with blood, semen, vaginal secretions, and breast milk. Contact can be sexual, perinatal or through contact with blood or body fluids that carry infected cells. Risk factors for contracting HIV include arthralgias, alopecia, pleurisy, kidney involvement , seizures, depression, fibromyalgia , and cardiac involvement . A pt will not immediately present with symptoms after the initial transmission of the infection. A pt can be symptom free for 1-2 years post infection or may exhibit flu-like symptoms including rash and fever. HIV immediately begins a latent phase HIV is diagnosed through various blood tests such as the enzymelinked immunosorbent test or Western blot test. Once diagnosed the lab results can also assist with classifying the stage of HIV infection. Early detection is important so that pharm intervention can be initiated and slow the progression of the virus. There is no cure for HIV, however, proper medical intervention can allow the virus to remain a manageable chronic condition. PT may be indicated during the course of HIV/AIDS due to secondary impairments. PT goals & intervention should include fitness, flexibility, stress management, begin to demonstrat e symptoms of the HIV infection. unprotected sexual relations, intravenous drug use or mother to fetus transmission . The largest risk factors for contracting HIV are homosexual male sex (46%), intravenous drug use (25%), and heterosexual sex (11%). where replication of the virus is minimal. The three phases of this disease process include asymptomat ic HIV, symptomati c HIV, and acquired immunodefi ciency syndrome (AIDS). relaxation, aquatic therapy, pain management, breathing exercises, and neuro rehab. Studies indicate that psychosocial factors influence progression of the virus as well as survival. Presently, the leading cause of death is kidney failure secondary to the extended drug therapies. Spotlight on safety: According to the American Diabetes Association, recommended blood glucose levels include 70-130 mg/dl prior to a meal and <180 mg/dl after a meal. Hyperglycemia: Early signs is blood glucose >180-200 mg/dl, increased thirst and frequent urination. Recognition of these early signs is crucial in preventing the dangerous onset of ketoacidosis, often referred to as a “diabetic come.” Symptoms include dyspnea, fruity breath odor, dry mouth, nausea, vomiting, confusion, and an eventual loss of consciousness. Hypoglycemia: Early signs is when blood glucose is <70 mg/dl, hunger, sweating, shaking, dizziness, clumsiness, and headache. If unaddressed, pts who become hypoglycemic may lose consciousness, at which point immediate medical attention is necessary. Hypoglycemia is often counteracted simply by ingestion of a glucose or carb rich substance (sugar, honey, juice, crackers). Pts with significant hypoglycemic issues may be advised by their physician to carry a glucose source of injectable glucagon with them at all times. Pharmacology of the Endocrine System: Drug Action Indications Hormone Replacement Therapy Hyperfuntio n Agents Bone mineral regulating Agents These agents restore normal endocrine function when endogenous production of a particular hormone is deficient or absent These agents manage hyperactive endocrine function to allow for inhibition of hormone function. This is accomplished through negative feedback loops or through hormone antagonists Attempt to enhance and maximize bone mass along with preventing bone loss or rate of Side effects Implications for PT Must be aware of side effects Examples ↓ in endogenous hormone secretion Vary by exogenous or synthetic hormone replacement used for treatment See specific hormone categories Hyperactive or excessive endocrine function, excessive hormone levels Vary depending on the use of hormone therapy Must be aware of signs of hyperfunction of particular hormones and side effects See specific hormones Paget’s disease, osteoporosis, hyperparathyrodi dism, rickets, hypoparathyroidi sm, osteomalacia GI distress, dyspepsia, dysphagia, anorexia, bone pain, cardiac Pts with bone mineralization deficit are at risk for fracture and side effects from drug Estrogens: Premarin; Calcium and vitamin D: Tums, Calderol; bone reabsorption. Typical agents can include estrogens, calcium and vitamin D, bisphosphonantes , calcitonin, and anabolic agents arrhythmias therapy. Should attempt to augment drug therapy through ambulation and other weight bearing activities that stimulate bone formation. Bisphospho nates: Fosamax, Boniva; Calcitonin: Cibacalcin Genitourinary System PT examination: (Consists of all the reproductive organs and the urinary organs. These are often considered together due to their common embryological origin) Anatomy and Function: Muscles of the Pelvic Floor Pelvic diaphragm Urogenital diaphragm Urogenital triangle Anal triangle Description Levator ani: pubococcygeus, puborectalis, iliococcygeus, & coccygeus (ischiococcygeus) Deep transverse perineal, urethrae sphincter Female:bulbocavernosus, ischiocavernosus, superficial transverse perineal Male: bulbospongiosus, ischiocavernosus, superficial transverse perineal Internal and external anal sphincter Genital System Female: External genitalia: Mons publis, labia majora, labia •Provides protection and hydration of vaginal minora, clitoris, vestibule of vagina, bulbs of vestibule, greater vestibular (Bartholin’s) glands, Skene’s gland Vagina: Musculomembranous tube connected to the cervis Uterus: hollow muscular organ Uterine tubes: Extend laterally from the ovaries to the uterus Ovaries: almond shaped glands suspended in the broad ligaments tissue and urethra •Receptacle for male sperm •Birth canal •Excretory duct for menstrual fluid •Houses the fetus during development •Provides transport for the ovum from the ovary for fertilization and implantation within the uterus •Produce hormones such as estrogen and progesterone •Storage of oocytes prior to ovulation Male: Penis Scrotum •External genitalia that expels urine during voiding and semen during the act of copulation •Cutaneous fibromuscular external sac for the testes, ductus deferens, epididymis, nerves, and blood vessels Testes •Produce sperm and hormones such as testosterone Dustus/vas •Carries sperm from the testes to the seminal vesicle to form the ejaculatory duct deferens Epididymis •Encased within the scrotum, stores sperm Seminal •Internal tubes that secrete a thick fluid to combine with sperm within the ejaculatory duct vesicles Prostate •Internal organ lying inferior to the bladder •Produces and secretes fluid to combine with sperm, seminal vesicle fluid, and bulbourethral gland fluid to create semen Renal System: two kidneys, two ureters, the urinary bladder, and the urethra that function to form and eliminate urine. Kidneys •Remove water, salt, and metabolic waste from the blood through excretion of urine Ureters Urinary bladder Urethra •Contribute to homeostasis including: acid-base balance, regulation of electrolyte concentrations, control of blood volume, and regulation of blood pressure through the control of hormones secreted into the blood stream. •Muscular tubes connecting the kidneys to the urinary bladder to transport urine •Temporary muscular reservoir for urine •Muscular tube for excretion of urine •Semen transport during ejaculation in males Genitourinary System Pathology Genital Components Uterus Vagina Prostate Penis Renal Components Kidneys Bladder Common Pathologies Cervical cancer, endometriosis, uterine prolpase Dyspareunia, vulvodynia, vulvovaginal candidasis (yeast infection) Prostatitis, prostate cancer Erectile dysfunction Common Pathologies Glomerulonephritis, nephrolithiasis, renal failure Cystocele, dysuria, hematuria, interstitial cystitis, neurogenic bladder, nocturia, polyuria, urgency, frequency, urinary incontinence, urinary tract infections Genitourinary Conditions/Pathology: Pathology Uterus: Endometriosis What is it Is the development of endometrial tissue, which normally lines the uterus, in extrauterine locations within Etiology Unknown. During each menstrual cycle the endometrial tissue bleeds causing subsequent scarring and adhesions. Signs & Symptoms Typically include moderate to severe lower abdominal, pelvic, or low back pain before or during menstruation, irregular Treatment PT may include manual techniques such as myofascial release, visceral mobilization and soft and deep tissue massage to the abdomen and pelvis. The most common location of growth occurs at the uterosacral ligaments. The level of pain does not always correlate with the severity of tissue growth. Uterine Prolapse Is the descent of the uterus and cervis into the vagina. The Baden-Walker System is the most widespread classification of prolapsed using a 5 point grading system ranging from no prolapsed to maximum descent of vaginal menstrual cycles, premenstrual spotting, dyspareunia, pain during defecation, and infertility. Typically consists of genetics, denervation or direct muscle trauma (labor & delivery) Primary symptoms include pelvic pressure that increases with exertion, urgency, frequency, urinary incontinenece, incomplete bladder empyting, discomfort, vaginal dryness or irritation, dysparenunia, and lower back pain break up scar tissue and adhesions. Mobility exercises are performed to sustain elongation of tissues. Relaxation exercises such as breathing routines and restorative poses are performed to regulate the pain cycle. TENS is also indicated. Surgery to remove scarring and a total hysterectomy may be recommended. PT may include pelvic floor muscle training using biofeedback, Kegel exercises, core strengthening exercises, body mechanics, and symptom dependent lifestyle modifications. In severe cases, an intravaginal tissue outside the body. that is relieved by lying down. Prostate: Prostatitis An inflammation of the prostate gland Most common include bacterial infection or the backup of prostate secretions within the gland. Penis: Erectile Dysfunction Also known as impotence, is estimated to range from 2585% in men with diabetes, which makes this population 3x more likely than the general population. Onset of ED in individuals Diabetes is a primary etiology, while other risk factors include CAD, HTN, hypothyroidism, hypopituitarism, multiple sclerosis, psychiatric disorders, excessive alcohol consumption, mechanical support device called a pessary may be indicated. Pt may require reconstructive surgery. Common Management symptoms include includes lifestyle watery urethral modifications, discharge, biofeedback urgency, training, stretching frequency, exercises, discomfort with myofascial urination, and pain techniques, and with ejaculation. bladder retraining. Pharmacological intervention such as antibiotics, alpha blockers or NSAIDS may be indicated. Primary symptom Pharmacological is the consistent intervention, inability to surgical maintain an intervention, erection adequate injections directly for sexual to the penis, and intercourse. Kegel exercises. with diabetes usually occurs 1015 years earlier than in men without diabetes. Kidneys: Renal Failure Renal failure is a condition where the kidneys experience a decrease in glomerular filtration rate and fail to adequately filter toxins and waste from the blood. There are two forms: acute and chronic renal failure. smoking, vessel disease, kidney disease, pharmacological side effects, & hormonal imbalances. Renal pathology typically occurs sencondary to DM or HTN, but can also occur from poison, trauma, and genetics. The nephrons are usually damaged and lose their ability to filter the blood. Renal failure can be classified as: Acute (damage occurs quickly) Chronic (damage occurs slowly) End-stage (nearly total or total renal failure, dialysis required) Acute: Sudden decline in renal function, increase in BUN and creatinine, oliguria, Nausea, vomiting, lethargy, weakness, hiccups, anorexia, ulceration within the GI tract, sleep disorders, headache, peripheral neuropathy, anemia, pruritis, osteomalacia, ecchymosis, pulmonary edema, seizures, and coma Includes management of primary etiology, pharmacological intervention, diuretics, nutritional etiology, hydration, hemodialysis and/or transfusions if applicable. Tx of chronic failure includes conservative management (slowing the process and assisting the body in its compensation). Nutritional support, hydration, avoidance of protein. Renal hyperkalemia, sodium retention Chronic: progressive deterioration in renal function, DM, HTN, interstitial nephritis, polycystic kidney disease Bladder: Neurogenic Bladder Is a dysfunction where there is damage to the cerebral control that allows for urinary dysfunction. If the urine cannot be properly released, there may be an increase in urinary tract infections and kidney damage. Diabetes, diminished bladder capacity, hyperactive detrusor muscle, CVA, other disease processes, infection, and nerve damage Frequent urinary tract infections, leakage of urine, inability to empty the bladder or loss of the urge to urinate when the bladder is full. Diagnosis should include an evaluation by a physician, X-rays, and urodynamics to assist with diagnosis. replacement therapy includes some form of hemodialysis and/or organ transplant. Peritoneal dialysis is a form of renal replacement therapy that uses the peritoneal cavity as a semipeermeable membrane between the dialysate fluid and blood vessels of the abdominal cavity. Dependent on the actual etiology with a goal of preventing bladder overdistention, UTIs, and renal damage. Pt education, bladder techniques, lower abdominal massage, temporary catheterization, pharmacological intervention, and a timed urination program may be indicated. Stress Urinary Incontinence (SUI) Urge Urinary Incontinence (UUI) Overflow Urinary Incontinence (OUI) Loss of urine due to activities that increase intraabdominal pressure, such as sneezing, coughing, laughing, running, and jumping. Loss of urine after a sudden, intense urge to void due to the detrusor muscle of the bladder involuntarily contracting during bladder filling. UUI is the most common incontinence in the geriatric population and among residents in long-term care facilities. Loss of urine when the intra-bladder pressure exceeds the urethra’s See page 686 in scorebuilders Detrusor muscle overactivity, overactive bladder syndrome, changes in the smooth muscle of the bladder, increased afferent activity, increased sensitivity of the detrusor to acetylcholide, and idiopathic. Also associated with MS, SCI, CVA, and parkinson’s. Triggered by certain events dut to a conditioned reflex. Two of the most common triggers are “key in the lock” when arriving home and running water. Behavior modification is the primary goal of treatment for this condition. Biofeedback, pelvic floor strengthening, and bladder retraining. (scheduled voiding) are key components. Caused by outflow obstruction secondary to a narrowed or Difficulty initiating the urine stream. One stream is initiated, its weak Surgical intervention if there is an obstruction. If capacity to remain closed due to urinary retention. Functional Urinary Incontinence (FUI) Is the loss of urine due to the inability or unwillingness of a person to use the bathroom facilities prior to involuntary bladder release. Urinary Tract Infections (UTI) Very common and occur within the general population, however there is a higher incidence in women and the geriatric population. obstructed urethra that results from a prolapsed pelvic organ, a stricture, an enlarged prostate, chronic constipation or neurological disease. A decreased level of mental awareness or a decrease in mobility. Occur when bacteria infiltrate the urethra or further into the bladder itself. Untreated, this type of infection and spread and cause a kidney infection (pyelonephritis). and presents with post void dribble. there is weakness of the detrusor muscles, double voiding is recommened for these pts as well as other strengthening measures. Impaired cognition Treatment should and/or mobility be directed to alleviate the underlying tissue. Improving mobility, modifying clothing style, increasing independence. Frequency of Early treatment urination, pain and has the best or burning with results. urination, cloudy Pharmacological urine, pressure treatment includes above the public bacteria-specific bone in women, antibiotics based shakiness, fever, on the bacteria back pain, and found in the fatigue. bladder. Pts are also encouraged to drink an excess of fluids to assist with treatment of the infections. Stages of Kidney Disease: Stage 1: Stage 2: Stage 3: Stage 4: Stage 5: Kidney damage with normal BFR (90 or greater) Mild decrease in GFR (60-89) Moderate decrease in GFR (30-59) Severe reduction in GFR (15-29) Kidney failure (GFR less than 15) Hemodialysis: -Treatment process for pts with advanced and permanent kidney failure -Kidney failure creates excess toxic waste, increase BP, retention of excess body fluids, and a decrease in red blood cell production. -Hemodialysis removes the blood from the body along with waste, excess sodium, and fluids. -The process cleanses the blood and returns it to the body. -A patient requires this process on average 3x per week and each visit requires 3-5 hours to complete the treatment. -Side effects that may be associated with dialysis include anemia, renal osteodystrophy, pruritus (itching), sleep disorders, (restless legs), and dialysis-related amyloidosis. Rehab considerations for pts with renal failure/dialysis: •Modify treatment plan based on fluid and electrolyte staus •Standard precautions should be followed at all times for protection •Recognize pts abilities post dialysis and potential for dehydration and hypotension •Monitor vital signs closely, however, avoid placement of the blood pressure cuff over the fistula •Avoid mobilization activities as they are contraindicated during dialysis •Energy conservation techniques and pacing skills should be incorporated into therapy Genitourinary System Terminology: Anuria Inadequate urine output in a 24 hour period; less than 100 ml (severe dehydration, shock, endstage renal disease) Benign A non-cancerous enlargement of the prostate gland that is progressive. Common in males prostatic over 60 and can interfere with normal voiding. hypertrophy Cystocele Ectopic Entometrium Glomerular filtration rate (GFR) Glomerulus Bulging of the bladder into the vagina Implantation of a fertilized ovum outside of the uterus (fallopian) tube is the most common site of an ectopic pregnancy) The inner lining of the uterus that is shed monthly in response to hormonal influence An estimate of the filtering capacity of the kidneys; volume of filtrate produced per minute by the kidneys The specialized tuft of capillaries that are needed for the filtration of fluid as blood passes through the arterioles of the kidneys Hematuria Presence of blood in the urine (cancer, faulty catheterization, serious disease) Impotence Impairment with ejaculation, orgasm, erection, and/or libido Myometrium The muscular outer layer of the uterus Nephrolithiasis The condition of developing kidney stones. There are various types of crystal formations that create stones. Nocturia Urinary frequency at night (DM, congestive heart failure) Oliguria Inadequate urine output in a 24 hour period; less than 400ml (acute renal failure, DM) Polyuria Large volume of urine excreted at one time (DM, chronic renal failure) Perimetrium The serous peritoneal coat of the uterus Radical A surgical procedure in which the entire breast, pectoral muscles, axillary lymph nodes, mastectomy and some skin are removed usually secondary to breast cancer Rectocele The bulging of the anterior wall of the rectum into the vagina secondary to weakening of the pelvic supporting structures Seminiferous Coiled tubes found within each lobe of the testes where spermatogenesis takes palce tubules Urea Major nitrogen-containing end product of protein metabolism normally cleared from the blood by the kidney into the urine Urinary Voiding more than 8x in a 24 hour period frequency Urinary Sudden desire to urinate that is stronger than usually and difficult to defer urgency 1st Practice Exam (3rd exam in Scorebuilders) 130. Gastrointestinal System: GI Anatomy and Function Upper GI Mouth Esophagus Stomach Initiation of mechanical and chemical digestion Transports food from the mouth to the stomach Grinding of food, secretions of hydrochloric acid and other exocrine functions, Secretions of hormones that release digestive enzymes from the liver, pancreas, and gallbladder to assist with digestion Lower GI-Small Intestine Duodenum Jejunum Ileum Neutralizes acid in food from stomach and mixes pancreatic and biliary secretions with food Absorbs water, electrolytes, and nutrients Absorbs bile and intrinsic factors to be recycled Lower GI-Large Intestine Ascending Colon Transverse Colon Descending Colon Sigmoid Rectus Anus Continues to absorb water and electrolytes; stores and eliminates undigested food as feces Gland Organs Gallbladder Liver Pancreas Stores and releases bile into the duodenum to assist with digestion Bile is produced and is necessary for absorption of lipid soluble substances, assists with red blood cell and vitamin K production, regulates serum levels of carbohydrates, proteins, and fats Exocrine-secretes bicarbonate and digestive enzymes into the duodenum; Endocrine-secretes insulin, glucagon, and other hormones into the blood to regulate serum glucose level. Gastrointestinal Pathology Pathology What is it Etiology Gastroesophageal Reflux Disease (GERD) GERD is the result of an incompetent lower esophageal sphincter (LES) that allows reflux or gastric contents. Erosive Gastritis Is the Weakness of the LES, Intermittent relaxation of the LES, Direct damage to the LES through NSAIDS, alcohol, infectious agents, smoking, and certain RX medications. Bleeding from Signs & Symptoms Heartburn, regurgitation of gastric content, belching, chest pain, hoarseness and coughing, esophagitis, and hematemesis. Symptoms Treatment Treatment is usually through pharmacological intervention. Is supportive Non-erosive Gastritis Peptic ulcer Disease inflammation of the gastric mucosa or inner layer of the stomach. Symptoms are similar to GERD, however, they tend to have a higher intensity. Is the inflammation of the gastric mucosa or inner layer of the stomach. Symptoms are similar to GERD, however, they tend to have a higher intensity. the gastric mucosa secondary to stress, NSAIDS, alcohol utilization, viral infection or direct trauma. include dyspepsia, nausea, vomiting and hematemesis. At times, the Pt may be asymptomatic with removal of the stimulus of the disease process and pharmacological interventions. This condition is usually a result of helicobacter Pylori infection The Pt is usually asymptomatic but will show symptoms if the gastritis progresses H. pylori is a carcinogen and must be treated aggressively. Pharmacological interventions are most common and typically include a proton pump inhibitor and antibiotics. Is a condition where there is a disruption or erosion in the GI mucosa. There is an imbalance between the Many ulcers are caused by the H. pylori infection and chronic NSAID use, Irritants that increase risk of ulcer Symptoms are dependent on the location and severity of ulceration and can include epigastric pain, burning or Treatment is usually through pharmacological intervention, however, in more severe cases, surgical intervention protective mechanisms of the stomach and the secretions of acids within the stomach. Diarrhea/constipation Malabsorption Syndrome Is defined as an abnormal frequency or volume of stool and can appear as a symptom of certain GI pathologies. Constipation is defined as the infrequent or difficult passage of stool, secondary to an increase in the hardness of the stool. Is a condition characterized by a group of pathologies where there is reduced include stress, alcohol, particular medications, foods, and smoking. heartburn, nausea, vomiting, bleeding, bloody stools and pain that comes in waves that is relieved by eating may be required. Malabsorption syndrome occurs secondary to defects in digestion Weight loss, chronic diarrhea, anemia, fatigue, abdominal bloating, Once diagnosed, treatment includes avoidance of the underlying cause for the intestinal absorption and inadequate nutrition and/or the inability of the intestinal mucosa to absorb the nutrients from digested food. steatorrhea, abdomal cramps, indigestion, bone pain, and excessive gas. Irritable Bowel Syndrome Consists of recurrent symptoms of the upper and lower GI system that interfere with the normal functioning of the colon. The etiology is unknow but one theory believes that the colon or large intestine may be sensitive to certain foods or stress. Diverticulitis Is a condition of having inflamed or infected diverticula. This occurs in approx. 2025% of the population that has The exact etiology of diverticulitis is unknown; however, a dominant theory is that the disease results from a low fiber diet. Abdominal pain, bloating or distention of the abdomen, nausea, vomiting, anorexia, changes in form and frequency of stool, and passing of mucus in the stool. Abdominal pain is the primary symptom, tenderness over the left side of the lower abdomen, cramping, constipation, nausea, fever, malabsorption, probiotics, antibiotics, dietary modification, and nutritional support including vitamins, minerals and electrolytes. Changes in life style and nutrition, decrease in stress, pharmacological interventions, adequate sleep, exercise, and psychotherapy may all assist in alleviating symptoms. Diet modification, controlling the underlying infection, and lowering internal colonic pressure through increased fiber diverticulosis. Hepatitis Is an inflammation process within the liver. Viral hepatitis is most common and is classified as hepatitis A,B,C,D,E, or G Cirrhosis of the Liver Is a condition where the healthy tissue of the liver is replaced with scar tissue that blocks the flow of blood through the organ and prevents the liver from properly functioning. Many instances of hepatitis are viral in nature. Other etiologies include a chemical reaction, drug reaction or alcohol abuse. Other viruses that can cause hepatitis include Epstein-Barr virus. The etiology is usually alcoholism or hepatitis C. Alcohol tends to block the normal metabolism of protein, fats, and carbs. chills, and vomiting can also occur. Fever, flu symptoms, abrupt onset of fatigue, anorexia, headache, jaundice, darkened urine, lighter stool, enlarged spleen, and liver and intermittent pruritus intake Acute viral hepatitis usually resolves wit medical treatment, but can become chronic in some cases. Chronic hepatitis may result in the need of a liver transplant. Fatigue, Treatment cant decreased reverse the appetite, process or nausea, damage, but can weakness, slow the abdominal pain, process. spider angiomas, Treatment is ascites, edema based on the in the LE, causative factors jaundice, and is gallstones, implemented increased until symptoms itching, cannot be ecchymosis, controlled, A bleeding , and liver transplant Cholecystitis and Cholelithiasis Refers to inflammation of the gallbladder that may be acute or chronic The most common etiology is gallstones that have become impacted within the cystic duct. Gallstones develop from hypomobility of the gallbladder, supersaturation of bile with cholesterol or crystal formation. increase in sensitivity to medications. Many times gallstones are asymptomatic, however, the most common symptom is right upper quadrant pain. Abdominal Pain Quadrant and Potential Etiologies Left upper Quadrant Right upper Quadrant Left lower Quadrant Gastric ulcer Hepatomegaly Perforated colon Perforated colon Duodenal ulcer Ileitis Pneumonia Cholecystitis Sigmoid Diverticulitis Spleen injury Pneumonia Kidney stone Spleen rupture Hepatitis Ureteral stone Aortic aneurysm Biliary stones Intestinal Obstruction may be necessary to sustain life. Treatment is not recommended for the patient with asymptomatic gallstones, but a low fat diet can decrease gallbladder stimulation if mild symptoms are present. Right lower Quadrant Kidney stone Ureteral stone Meckel diverticulum Appendicitis Cholecystitis Intestinal obstruction Gastrointestinal Pharmacology Name Antacid agents Action Are used to chemical neutralize gastric acid and increase the intragastric PH. Indication Episodic minor gastric indigestion or heartburn, peptic ulcer, GERD Side effect Acid rebound phenomenon, constipation, or diarrhea, may effect metabolism of other medications. Implication Since these agents are well tolerated there are no side effects that interfere with physical therapy. H2 receptor blockers Bind specifically to histamine receptors to prevent the istamineactivated release f gastric acid normally stimulated during food intake. Inhibit the H+K+ATPase Dyspepsia, acute and long term treatment of peptic ulcer, or GERD Headache, dizziness, mild GI distress, tolerance, arthralgia, acid rebound with dicontinuation of medicine. Since these agents are well tolerated there are no side effects that interfere with physical therapy. Dyspepsia, GERD Acid rebound when discontinued Since these agents are well tolerated Proton Pump Inhibitors Examples Aluminumcontaining: basaljel, Calcuim carbonatecontaining: tums, Magnesiumcontaining: Milk of magnesia, Sodium bicar. Containing: Bromo seltzer Tagament, Pepcid, Zantac Prevacid, nexium, prilosec, enzyme that blockes secreations of acid from gastric cells into the stomach Anticholinergics Block the effects of acetylcholine on parietal cells in the stomach and decrease the release of gastric acid. Antibiotics Are prescribed to treat H. pylori infection with the goal of facilitating more rapid healing of associated gastric ulcerations. Antidiarrheal Are used to Agents slow the serious debilitating effects of dehydration after prolonged use there are no side effects that interfere with physical therapy. protonix, acipHex Gastric ulcers Dry mouth, confusion, constipation, urinary retention PT should be aware of potential side effects in order to respond appropriately. Gastrozepin, Muscarinic cholinergic antagonist. H. pylori bacteria Hypersensitivity, PT should be nausea aware of potential side effects in order to respond appropriately. Metronidazole, tetracycline, clarithromycin, amoxicillin Prolonged diarrhea Constipation, Abdominal discomfort Donnagel, Kapectolin, peptpBismol, Motofen, Imodium Since these agents are well tolerated there are no side effects that interfere Laxative Agents associated with prolonged diarrhea. Are used to facilitate bowel evacuation and should be used sparingly Emetic agents Are used to induce vomiting Antiemetic Agents Are used to decrease symptoms of nausea and vomiting with physical therapy. To promote defecation Nausea, abdominal discomfort, cramping, electrolyte imbalance, dehydration, dependence, with prolonged use If the laxative was recently ingested physical discomfort may temporarily limit patient participation in therapy interventions. To induce With Therapy vomiting, inappropriate or should be usually prolonged usage deferred if a after dehydration, patient is ingestion electrolyte actively of a toxic imbalance, and vomiting substance upper GI erosion may occur Nausea Agent Antihistamine associated dependent, but antiemetic with can include agents motion sedation, frequently sickness, dysrhythmias, cause anesthesia, and pain sedative pain or effects which oncology can be treatment limiting to PT interventions Citrucel, Metamucil, colace, fleet Glycerin suppository, senokot Apomorphine, Ipecac Scopolamine, meclizine, dolasetron, phenergan. Gastrointestinal System Interventions/Rehab: Rehab considerations for pts with GI disease: -Recognize electrolyte imbalances from diarrhea, vomiting, and weight loss -Recognize the potential for orthostatic hypotension secondary to electrolyte imbalances -Increased risk for muscle cramping secondary to alteration in the sodium-potassium pumps -Potential for difficulty swallowing secondary to disk protrusion or esophageal pathology -Recognize that back pain and/or shoulder pain may be secondary to an acute ulcer or GI bleed -Observation of Kehr’s sign indicates free air or blood within the abdominal cavity Rehab considerations for pts with GERD: -Avoid certain exercise secondary to an increase in symptoms with activity; recumbency will induce symptoms -Recognize increased incidence of neck and head discomfort secondary to perception of a lump in the throat and subsequent compensation -Left sidelying preferred since right sidelying may promote acid flowing into the esophagus -Recognize conditions such as chronic bronchitis, asthma, and pulmonary fibrosis may all present with GERD -Consider that certain positioning during postural drainage may encourage acid to move into the esophagus Rehab considerations for pts with Gastritis: -pts with gastritis secondary to chronic NSAID use may be asymptomatic -Knowledge of blood in the stool should result in physical referral -Educate each pt to take medications with food and avoid certain types of food and drink -The pt should avoid all aspirin-containing compunds Rehab considerations for pts with Peptic Ulcer Disease: -Asymptomatic pts with history of ulcer should be monitored for signs of bleeding -Fatigue level, pallor, and exercise tolerance must be monitored for signs of bleeding -Recognize that heart rate increase or blood pressure decrease may be sings of bleeding -Recognize that back pain is a sign of perforated ulcer located on the posterior wall of the stomach and duodenum -Recognize that pain that radiates form the midthoracic area to the right upper quadrant and shoulder may signify blood and acid within the peritoneal cavity secondary to a perforated and bleeding ulcer Rehab considerations for opts with malabsorption syndrome: -Recognize increased risk for osteoporosis and pathologic fractures -Monitor fatigue level, pallor, bone pain, and exercise tolerance -Recognize weight loss and abdominal bloating -Recognize increased risk for muscle spasms secondary to electrolyte imbalances -Recognize increased risk for generalized swelling secondary to protein depletion Rehab considerations for pts with Irritable bowel syndrome: -Emphasize physical activity to assist with bowel function and relieve stress -Emphasize breathing techniques to assist in stress reduction and with breath holding patterns -Recognize that biofeedback training may be beneficial Rehab considerations for pts with diverticular disease: -Physical activity assists the bowel function and is extremely important during periods of remission -Breathing techniques will assist in stress reduction and with breath holding patterns -Avoid any increase in intra-abdominal pressure with exercise or activity -Back pain and/or referred hip pain must be examined for possible medical diseases Rehab considerations for pts with Hepatitis: -Heath care workers that are at risk for contact with hepatitis should receive all immunizations for HBV, and if exposed to blood or body fluids of an infected person must receive immunoglobulin therapy immediately -Standard precautions should be followed at all times for protection -Enteric precautions are required for pts with hepatitis A and E -Recognize that arthralgias may be noted, especially in older pts, and will not typically respond to traditional therapeutic intervention -Energy conservation techniques and pacing skills should be incorporated into therapy -Balance activities along with periods of rest, avoid prolonged bed rest, and provide pt education regarding signs of relapse or chronic hepatitis Rehab considerations for pts with cirrhosis of the liver: -Recognize that ascities may develop as well as fluid accumulation in the ankles and feet -Report any blood loss through nose bleeds, gum bleeds, tarry stools or excessive bruising -Avoid all activities that produce the valsalve maneuver (increase in intra-abdominal pressure) -Adequate rest is required to lower the demands on the liver and improve circulation; avoid unnecessary fatigue with therapeutic or daily activities Rehab considerations for pts with cholecystitis and cholelithiasis: -Must be familiar with all signs and symptoms of cholecystitis in order to refer pts to a physican if a change in their status occurs -Post surgical exercises and ambulation are appropriate post laparoscopic cholecystectomy such as breathing exercises, splinting while coughing, and mobility training Genitourinary System: Pathology Diagnosis Urinary Stress Involuntarily Contributing Factor Occurs from Clinical presentation Dribbling of Lab/Imaging Cystometry is Management/outco me Usually consists of Incontinence loss of urine. May occur during activities when there is an increase in abdominal pressure through straining, sneezing, coughing or lifting. a loss of strength and or integrity of the tissues that maintain bladder control. It is caused by weakness of the pelvic floor muscles. Risk factors include pregnancy, vaginal delivery, episiotomy, prostate or pelvic surgery, aging, DM, recurrent UTIs. Obesity (due to increased intraabdominal pressure) urine, urgency, frequency, nocturia, and a weak stream while voiding. used to evaluate bladder capacity, control, contractility, and sensation. During this procedure provocative stress testing will be performed when stress incontinence is suspected. Urodynamic testing observes the stability of the bladder and electromyogra phy observes bladder contractions. Urinalysis is used for DD to rule out infection, diabetes, and other conditions. convervative measures (PT) as a first line of defense followed my pharmacological and surgical interventions. PT intervention for pelvic floor muscle weakness that is ststed as 0/5-2/5 includes biofeedback, e-stim, bladder retraining, and therapeutic exercise. Pelvic floor muscle strengthing at this level includes facilitation and tapping of the pelvic floor muscles, overflow exercises uring the buttocks, adductors, and lower abdominals, and implementation of Kegel exercises. PT for muscle weakness graded 3-5-5/5 includes continued biofeedback and bladder retraining, weighted vaginal bones for resistance training, and implementation of pelvic floor muscle exercises during activities. Outpatient PT for urinary stress incontinence should alleviate pelvic floor weakness and involuntary leakage of urine within 8-12 weeks. Obstetric Musculoskeletal Pathology: Pathology What is it Coccydynia After childbirth the joint between the coccyx and sacrum can become hypermobile causing the soft tissue surrounding the coccyx to become painful. Etiology Subluxation during delivery, adherence to tear or episiotomy scar Signs & Symptoms Difficulty sitting on hard surfaces, referred pain to the low back, sacroiliac joint, hip, buttock, groin or rectum areas, pain with bowel movements, dyspareunia, and formation of hemorrhoids Treatment Heat, external joint mobilization, myofascial release, muscle energy techniques, biofeedback for pelvic floor muscle relaxation, postural training, abdominal strengthening exercises, stretching exercises for surrounding muscles and the use of a cushion for sitting. Diastasis Recti Is a separation of the rectus abdominis muscle along the linea alba that can occur during pregnancy. Testing for diastasis recti should be performed on all pregnant women prior to prescribing exercises that require the use of the abs. Hormonal changes in women may cause the separation. The therapist must note how many fingers fit into the separation and modify treatment accordingly. A pt is considered to have diastasis recti if the therapist detects a separation greater than the width of two fingers when the woman lifts her head and shoulders off the plinth. Piriformis Syndrome Refers to a persistent, severe radiating low back and buttock pain spanning from the sacrum to the hip and posterior thigh. However, controversy exits over piriformis syndrome’s efficacy as an accurate diagnosis. During pregnancy the piriformis may shorten or spasm due to postural changes and hip lateral rotation while walking. The primary symptom is sciatic paresthesia due to nerveentrapment as the sciatic nerve passes under or through the pirifiormis muscle. Stabilization and support with abdominal strengthening exercises, postural awareness exercises, and body mechanic training. A newborn can also have diastatis recti secondary to incomplete development, however, in infants this condition usually resolves itself without intervention. Manual techniques for correcting pelvic or sacral alignment such as METs, joint mobs, self-correction techniques for alignment, heat application, deep tissue massage, myofascial release, straincounterstrain, ab Symphysis Pubis Pain To prepare for delivery, the symphysis pubis joint become mobile in order to allow the joint to slightly separate during delivery. Postural adaptations, ligamentous laxity and complications during delivery or birthing of a large infant can result in more sever injury Sever pain in the symphysis pubis and SI joint as well as blood in the urine due to injury to the urethra or bladder neck. strengthening, stretching for piriformis, body mechanics, and postural education. Pharm intervention for pain, surgical intervention based on the degree of separation. Heat or ice if acute, manual techniques for correcting pelvic/sacral alignment. Lumbar stabilization and the use of a lumbo-pelvic brace or binder. •Women should not exercise in the supine position after the first trimester. •Prolonged periods of motionless standing should be avoided. •Left sidelying is the position of choice to reduce the pressure on the inferior vena cave, maximize cardiac output to enhance maternal and fetal circulation, and reduce the risk if incompetent cervix. Relative Contraindications to terminate exercise during pregnancy: -Severe anemia -Unevaluated maternal cardiac dysrhythmia -Chronic bronchitis -Poorly controlled type 1 DM -Extreme morbid obesity -Extreme underweight (BMI <12) -History of sedentary lifestyle -Poorly controlled HTN -Orthopedic limitations -Poorly controlled seizure disorder -Poorly controlled hyperthyroidism -Heavy smoker Absolute Contraindications to terminate exercise during pregnancy: -Hemodynamically significant heart disease -Restrictive lung disease -Incompetent cervix/cerclage -Multiple gestation at risk for premature labor -Persistent 2nd or 3rd trimester bleeding -Placenta previa after 26 weeks of gestation -Premature labor during the current pregnancy -Ruptured membranes -Preeclampsia/pregnancy-induced hypertension Pharmacology of the Genitourinary System: Pharm intervention is used for treating bladder symptoms related to urgency, frequency, infection, and pain. Drug Action Overactive bladder agents Relive the symptoms of an overactive bladder. This condition is noted by involuntary contractions of the bladder (detrusor muscle) Treat urinary tract infections, but are not traditional antibiotics or sulfonamide agents. These agents can be used independently or in combination to treat urinary infections. Urinary AntiInfective Agents Indications Urinary urgency, frequency, incontinence, nocturia Cystitis, urinary urgency, burning with urination, UTI, nocturia Side Effects Implications for PT GI distress, These agents nausea, do not typically dizziness, interfere with photosensitivity, rehab headache, constipation, pulmonary reactions GI distress, nausea, dizziness, photosensitivity, headache, constipation, rash These agents typically do not interfere with rehab Examples Ditropan (oxybutynin chloride), Detrol (tolterodine tartrate) Cinobac (cinoxacin), Furadantin (nitrofurantoin) System Interactions: Oncology-Cancer, malignancy, neoplasm, and tumor are all terms referring to abnormal uncontrolled cell growth within the body. There are more than one hundred different cancers of various types and tissue origins currently recognized, including lymphoma and hematologic cancers. Malignant cancer cells are characterized by their ability to grow uncontrollably, invade other tissues, remain undifferentiated, initiate growth at distant sites, and avoid detection and destruction by the body’s immune system. The origins of malignant cells vary widely from environmental factors and lifestyle choices to genetic predisposition. Carcinoma is a malignancy originating from the epithelial cells of organs. Carcinomas in specific organs may be named more specifically depending on the characteristics present. For example, large cell carcinoma, adenocarcinoma, and squamous cell carcinoma are all subsets of lung carcinoma. The American Cancer Society reports that at least 80% of all cancers in the US are carcinomas. Risk factors: Increasing Age Tobacco Use Alcohol Use Gender Virus exposure Environmental influence Poor diet Stress Occupational Hazards Ethnic Background Genetic influence Sexual/reproductive behavior General Signs & Symptoms of Cancer C-Change in bowel/bladder routine A-A sore that will not heal U-Unusual bleeding/discharge T-Thickening/lump develops I-Indigestion or difficulty swallowing O-Obvious change in wart/mole N-Nagging cough/hoarseness Cancer Prevention: Primary Prevention -Screening for high population -Elimination of modifiable risk factors Secondary Prevention Tertiary Prevention -Use of natural agents (teas, vitamins) to prevent cancer -Cancer vaccine -Early detection -Selective preventative pharmacological agents (Tamoxifen) -Multifactorial risk reduction -Prevent disability that can occur secondary to cancer and its treatment -Manage symptoms -Limit complications Tissue & Tumor Classification: Tissue Classification Epithelium: Protect, absorb, and excrete Pigmented Cells Connective Tissues: elastic, collagen, fibrous Examples -Skin, Lines internal cavities, Mucous membrane, Lining of bladder -Moles -Striated muscle, blood vessels, bone, cartilage, fat, smooth muscle Nerve Tissues: neurons, nerve fibers, dendrites, glial cells -Brain, nerves, spinal cord, retina Lymphoid Tissues -Wherever lymph tissue is Tumor Classification Carcinoma; Adenocarcinoma (glandular tissue) Malignant Melanoma Sarcoma, fibrosarcoma, liposarcoma, chondrossarcoma, osteosarcoma, hemangiosarcoma, hemangiosarcoma, leiomyosarcoma, rhabdomyosarcoma -Astrocytoma, Glioma, Neurilemic sarcoma, neuroblastoma, retinoblastoma Lymphoma Hematopoietic Tissues present throughout the body, lymph nodes, spleen, can appear in stomach, intestines, skin, CNS, bone and tonsils -Bone marrow, plasma cells Diagnostic tools: Family history Physical exam Pap smear Blood tests Radiography CT scan Bone scan Stool guaiac Biopsy Mammography Endoscopy Isotope scan Genitourinary System Intervention/ Rehab: Rehab considerations for pts with renal failure/dialysis: -Modify treatment plan based on fluid and electrolyte status -Standard precautions should be followed at all time for protection -Recgonize pts abilities post dialysis and potential for dehydration and hypotension -Monitor vital signs closely, however, avoid placement of the blood pressure cuff over the fistula -Avoid mobilization activities as they are contraindicated during dialysis -Energy conservation techniques and pacing skills should be incorporated into therapy -Leukemia, Myelodysplasia, Myeloproliferative syndromes, multiple myeloma Lifestyle Modifications to address bladder symptoms: -Daily fluid intake should be 2,500 mL, or 10 cups, to regulate excessively high or low fluid intake -Reduce bladder irritants including carbonated, caffeinated, and alcoholic beverages, spicy foods, citric juices, and artificial sweeteners. Caffeine reduction should be tapered slowly to avoid severe headaches. -Schedule voiding for every 3-4 hours to reduce bladder distension. An average person voids 6-8 times in a 24 hour period. A bladder diary assists with baseline measurements and goal setting -Regulate bowel function to prevent constipation and straining during bowel movements by monitoring dietary fiber, fluid intake, and exercise. -Avoid fluid intake 2-3 hours prior to bedtime to reduce nocturia. -A smoking cessation program may decrease the occurrence of coughing and subsequent bladder leakage. -A weight loss program, if moderately obese, may decrease pressure on the pelvic tissues and organs. Spotlight on Safety: Rehab Considerations for pts undergoing chemotherapy and radiation: -Strenuous activity should be initially avoided following implantation of radioactive seeds utilized for brachytherapy. Communication with the radiation oncologist and/or referring physician is imperative as further activity contraindications or precautions may be advised depending on the individual care. -Skin tattoos are used to guide beam alignment with external beam radiation. PTs must be cautious and defer interventions which may alter the position of alignment tattoos (taping interventions, certain soft tissue or myofascial mobilizations) -Irradiated skin requires special care to protect tissues prone to erythema, rash, and dry desquamation, as well as more painful wet desquamation and superficial burns. -Massage and heat are contraindicated over irradiated areas for a minimum of 12 months. -Certain chemotherapy agents may cause the pt to have a level of toxicity that requires staff and visitors to take additional precautions before making physical contact. -Pt vomiting during therapy should be reported to the nurse/physician, especially if the pt it taking antiemetic medications to control nausea and vomiting. Stage Stage 0 Stage I Stage II Stage III Stage IV Definition Early malignancy that is present only in the layer of cells in which it began. For most cancers, this is referred to as carcinoma in situ. Not all cancers have a stage 0. Malignancy limited to the tissue to origin with no lymph node involvement or metastatis. Malignancy spreading into adjacent tissues, lymph nodes may show signs of micrometastases. Malignancy that has spread to adjacent tissue showing signs of fixation to deeper structures. The likelihood of metastatic lymph node involvement is high. Malignancy that has metastasized beyond the primary site, for example, to bone or another organ. Oncology Pathology: Pathology What is it Brain Cancer May occur as a primary tumor arising from astrocytes, meninges, nerve cells, or tissues within the brain. Metastatic brain cancer occurs when a brain Etiology Most primary cancers outside of the brain metastasize to the brain during progression of the cancer. Signs & Symptoms Dependent on the tumor and typically progresses rapidly. Symptoms include headache, seizures, ↑ intracranial pressure, cognitive and emotional Treatment Surgical resection along with radiation or other combined therapies are typically indicated. Cervical Cancer Colorectal Cancer tumor develops as a consequence of cancer in another primary area of the body. Starts in the cells on the surface of the cervix, typically squamous cells. This precancerous condition is called dysplasia and is easily treatable. Annual cervical screening is recommended; diagnosis is made through a Pap smear. Prognosis is good with timely intervention. If dysplasia goes undetected, changes can develop into cervical cancer and metastasize to the bladder, intestines, lungs, and liver. Accounts for approx 15% of cancer deaths impairment, and ↓ motor and sensory function. The human papilloma virus (HPV) is the primary cause of cervical cancer; it is slow growing. Risk factors include smoking, maternal use of diethylstilbestrol (DES), African American ethnicity, oral contraceptive use, and certain sexually transmitted dieases. Asymptomatic during the early stages, however, symptoms can include abnormal bleeding, pelvic and low back pain, impairment with bladder and bowel function. Dependent on staging of the cancer and may include laser therapy, excision, cryotherapy or hysterectomy with adjunct chemotherapy or radiation. Risk factors include increasing age, history of polyps, Colon cancer does not provide early signs of disease Based on type and stage and may include surgical Lung Cancer Lymphoma (Hodgkin’s, nonHodgkin’s disease) annually. Adenocarcinoma and primary lymphoma accoudnt for the majority of intestinal cancers. ulcerative colitis, Crohn’s disease, fam history, and a diet high in fat and low in fiber. and the most prominent symptom is a continuous change in bowel habits. Bright red blood from the rectum is another prominent sign of colon caner. The pt may experience symptoms of fatigue, weight loss, anemia, and overt rectal bleeding. Is cancer of the epithelium within the respiratory tract. It is the most frequent cause of death from all cancers. Rapid metastasis can occur through the pulmonary vascular system, adrenal gland, brain, bone, and liver. Lymphoma is classified as cancer found in the Risk factors include smoking, environment, geography, occupational hazards, age, and fam history. Early symptoms include cough, sputum, and dyspnea. Progression may include adventitious breath sounds, chest pain, and hemoptysis. Risk factors for Hodgkin’s disease include association A painless lump is typically the first sign. Hodgkin’s resection of the tumor and potentially a portion of the bowel, with subsequent radiation therapy or chemo. Colostomy may be required. Prognosis is good for early diagnosis if the cancer is contained; prognosis is poor if it has metastasized. There is a poor prognosis secondary to expedited metastaiss (less than 14% for a 5 year survival rate). Surgical intervention along with combination therapies may be required. Hodgkin’s disease is one the most curable cancers Pancreatic Cancer lymphatic system and lymph tissues; lymphomas are categorized as Hodgkin’s disease or non-Hodgkin’s lymphoma. with Epstein-Barre virus, drug abuse, immunosuppressant use, obesity, chronic or autoimmune diseases. Risk factors for non-Hodgkin’s lymphoma include exposure to benzene (cigarette smoke), auto emissions, and pollution. disease is distinguished by the presence of Reed-sternberg cells and Hodgkin’s disease can metastasize to extralympthatic sites including the liver, spleen, and lungs. Prominent type of cancer with an extremely high mortality rate. Cancer of the exocrine cells within the ducts is the most common form of pancreatic cancer. It will metastasize to the liver, lungs, pleura, colon, stomach, and spleen. Risk factors include tobacco use, gender, increasing age, and cholecystectomy. Symptoms are very vague during the initial stages of the disease which often results in delayed diagnosis. Common symptoms include weight loss, jaundice, and epigastic pain that can radiate to the thoracic region. Advanced cancer depending on age, disease stage, overall health, and responsiveness to treatment. Treatment options are based on the pts age and staging classification and include chemo, radiation, stem cell transplant, and highly active antiretroviral therapy. NonHodgkin’s progression varies based on classification. Usually directed to assist in the relief of symptoms. Pancreatic cancer has a very poor survival rate with a mortality rate of almost 100%. Surgical resection along with chemotherapy and radiation assist to relieve symptoms. Prostate Cancer Skin Cancer Adenocarcinoma is the most common type of prostate cancer. Typically affects men over 50, it is the second highest cause of death from cancer in men. Diagnosis is found through prostate biopsy and prognosis is good with appropriate treatment. There is an approximate 10% fatality from this diagnosis. Basal cell carcinoma is a slow growing form of skin cancer that rarely metastasizes. It originates from the epidermis and is the most common form of Risk factors include age, high fat diet, genetic predisposition, African American descent, and exposure to cadmium. Sun exposure is a common cause, with risk factors including frequent sun exposure, light eyes, and fair skin. may present with severe pain that may indicated the cancer has metastasized. Most times this is asymptomatic until the cancer reaches the advanced stages. Symptoms include urinary obstruction, pain, urgency, and decreased stream/flow of urine. Open sores that can bleed or curst and remain for three or more weeks, reddish patches of skin, a shiny bump on the skin that is often pink, or a scar-like area that has Treatment varies and may include surgical incision of the prostate gland, radiation, or hormonal therapy; can metastasize to the bladder, MS system, lungs and lymph nodes. Prognosis is good, basal cell carcinoma can routinely be cured. Surgical excision may be required to remove the cancer cells. skin cancer. Malignant Melanoma Originates from melanocytes and can be classified as: superficial spreading, nodular, lentigo maligna or acral lentiginous melanomas. Peak incidence is between 40-60 years of age. Early diagnosis is vital to prognosis, as it can spread and metastasize quickly. Areas of metastases include the brain, lungs, liver, bone, and skin. poorly defined borders. Risk factors for Lesions can be malignant elevated on the melanoma include a surface of the skin history of blistering and appear sunburns prior to 20 keratotic or scaly. years of age, family Other symptoms history, when observing immunosuppression, the skin or a mole light eyes, fair skin, may include and a previous asymmetry, history of cancer. irregular borders, varied color, and a diameter of greater than 6mm. Pharmacology—Oncology Management: Drug Action Indications Alkylating Agents Bind the DNA strands together to prevent replication. If the DNA cannot Various malignancies Side Effects Vary by class of drugs and by specific agent; multisystem involvement with mild to severe side effects, This form of cancer is 100% curable with early diagnosis. Excision may solely be required with early treatment. If melanoma has metastasized, surgical intervention along with combination therapies may be required. Implications for PT Therapists must be aware of the chemo regimen and modify treatment based on the Examples Mustargen, Busulfex, Leukeran untwist, then it cannot divide and replicate its genetic code. These agents initiate cell death by disrupting DNA function and releasing enzymes that destroy the cell. Anitmetabolite Agents Impair biosynthesis of genetic material and interrupt the cellular pathways that synthezise the DNA and RNA. These agents create an imposter to the endogenous metabolites within the however, potential risks are typically warranted secondary to the diagnosis of malignancy Various malignancies, particularly rapidly dividing neoplastic cells Vary by class of drugs, potential risks are typically warranted secondary to the diagnosis of malignancy pts symptoms and side affects from cancer treatment. Extreme fatigue, GI distress, cancer pain and blood disorders are common. Therapists must provide support and encouragement without pushing the pt beyond their abilities. Therapists must be aware of the chemo regimen and modify treatment based on the pts symptoms and side affects from cancer treatment. Extreme fatigue, GI distress, cancer pain and blood disorders are Leustatin, Adrucil, Fludara, Trexall (methotrexate) body to form a nonfunctional genetic product that is incapable of reproduction. Antibiotic Agents Certain antibiotic agents are used with treatment of cancer due to their high toxicity and ability to interfere with DNA & RNA synthesis and subsequent cell division. Plant Alkaloid Agents in this Agents (Mitotic classification Inhibitors) are nitrogen based and largely derived from plants. They directly target the replication process prior to and during Various malignancies SOB, dysrhythmias, blood disorders, myelosuppression, pedal edema Various malignancies Vary by class of drugs, potential risks are typically warranted secondary to the diagnosis of malignancy common. Therapists must provide support and encouragement without pushing the pt beyond their abilities. Same as Adriamycin, previous Mithracin, Cosmegen Same as previous Oncovin, Taxotere, Taxol Hormones Biologic Response Modifier mitosis to inhibit cell division. This limits cell division and cancer growth in various types of malignancy. Certain hormones can exacerbate or facilitate proliferation of particular forms of cancer while other hormones can attenuate particular cancers. Hormones are typically used as adjunct therapy along with other form of treatment specific to the malignancy. Include interferons, interleukin-2, Various malignancies, particularly hormone sensitive neoplasms Masculinization in women, hot flashes, general catabolic effects Same as previous Nolvadex, Lupron, Casodex Various malignancies, particularly Vary by class of drugs, potential risks are typically Same as previous Proleukin, Avastin, Intron-A Agents Heavy metal compounds and monoclonal antibodies that are responsible for enhancing the body’s own ability to respond to neoplastic growth. These agents are not cytotoxic, but facilitate the pts immune response to destroy malignant tissues. Used as antineoplastic agents are also known as platinum coordination complexes. They act as askylating agents that inhibit DNA translation are replication. leukemias, lymphomas, Kaposi sarcoma, organ and tissue malignanicies warranted secondary to the diagnosis of malignancy Various malignancies, particularly epithelial malignancies, ovarian, testicular and bladder cancer Vary by class of drugs, potential risks are typically warranted secondary to the diagnosis of malignanc Oncology Terminology: Adjuvant Treatment provided, in addition to other cure- Same as previous Platinol, Paraplatin, Eloxatin Benign neoplasm Cancer Differentiated Cells Dysplasia Hyperplasia Malignant neoplasm Metaplasia Neoadjuvant Tumor (neoplasm) focused inverventions, with the intension of preventing cancer recurrence An abnormal cell growth that is usually slow growing and harmless, closely resembling the composition of adjacent tissues A group of diseases characterized by uncontrolled cell proliferation with mutation and spreading of the abnormal cells. The etiology is based on the type and location of the cancer. The most common causes include cigarette smoking, diet and nutrition, chemical agents, physical agents, environmental causes, viral causes, and genetics. Cells that have matured from a less specific to a more specific cell type An abnormal development of cells or tissue that is often an early sign of neoplasia An increase in cell number that may be normal or abnormal depending on additional characteristics An abnormal uncontrolled cell growth that invades and destroys adjacent tissues and may metastasize to other sites and systems of the body A change in a cell from one type to another that may be normal or abnormal Chemotherapy or radiation given prior to surgical oncology intervention An abnormal new growth of tissue that increases the overall tissue mass. Tumors are benign (noncancerous) or malignant (cancerous) as well as primary or secondary. Primary tumors form from cells that belong to the area of the tumor. Secondary tumors grow from cells that hae metastasized (spread) from another affected area within the body. Tumor classification is defined by cell type, tissue of origin, amount of differentiation, benign Undifferentiated cells versus malignant, and anatomic site. Cells which have not differentiated into a specific into a specific type (primitive, embryonic) or have no special structure or function. Psychological Disorders: Affective Disorders: are classified by disturbances in mood or emotion. States of extreme happiness or sadness occur and mood can alternate without cause. These extreme emotions can become intense and unrealistic. Depression: -Slower mental and physical activity; poor self-esteem -Immobilized from everyday activities; sadness, hopelessness, and helplessness -Desire to withdraw; delusions in severe cases Mania: -Constantly active -impulses immediately expressed -Unrealistic activity -Elation and self-confidence -Disagreement with a patient may produce patient aggression -Disorganized thoughts and speech -Very few pts are diagnosed with only manic disorder Bipolar: -Alternating periods of depression and mania -Females are at a greater risk; typically begins in a pts twenties Neuroses Disorders: refer to a group of disorders that are characterized by individuals exhibiting fear and maladaptive strategies in dealing with stressful or everyday stimuli. Pts with neuroses are not dealing with psychosis, do not have delusions, and usually realize they have a problem. Obsessive-Compulsive Disorder: -Obsessions-persistent thoughts that will not leave -Compulsions-repetitive ritual behaviors the pt cannot stop performing -Thoughts or ritual behaviors that interfere with daily living -Unable to control irrational behavior -Most commonly beings in young adulthood Anxiety Disorder: -Constant high tension; overreacts in certain instances -Presents with apprehension and chronic worry Acute anxiety attacks: -Lasts a few minutes in duration -Excitation of the sympathetic autonomic nervous system -Fear of impending doom or death -Shortness of breath, heart palpitations, dizziness, nausea -Initiated by unconscious and internal mechanisms Phobia Disorder: -Excessive fear of objects, occurrences or situations that is considerably out of proportion/irrational -Fear creates difficulty in everyday life -Subclassifications include agoraphobia, social phobia, and simple phobia; simple phobia is easiest to treat -May develop from traumatic experiences, observation, classical conditioning Dissociative Disorders: Develop when a person unconsciously dissociates (separates) one part of the mind from the rest. Psychogenic Amnesia: -Produced by the mind with no physical causes -Forgets all aspects of the past Multiple Personality: -A rare dissociative disorder; includes two or more independent personalities -Each personality may or may not know about the other -Causative factors are not understood; believed to allow a person to engage in behaviors that are against the pts morality and normally produce guilt Somatoform Disorders: are classified based on the physical symptoms present in each disorder. Somatization Disorder: -Primarily in women, has familial association, and often chronic and long lasting -Complaints of symptoms with no physiological basis -Symptoms usually lead to medications and medical visits and alter the pts life -Resembles hypochondriasis disorder Conversion disorder: -Physical complaints of neurological basis with no underlying cause -Paralysis is the most common finding; other findings include deafness, blindness, paresthesia -Frued believed this is mental anxiety transformed into physical symptoms -Diagnosis can be made once testing is negative for physical ailments Hypochondriasis Disorder: -Excessive fear of illness -Believes that minor illnesses or medical problems indicate a serious or life threatening disease Schizophrenia Disorders: Psychotic in nature and present with disorganization of thought, hallucinations, emotional dysfunction, anxiety, and perceptual impairments. Causative factors include traumatic events, genetic inheritance, biochemical imbalances, and environmental influence. Catatonic Schizophrenia: -Motor disturbances with rigid posturing -Episodes consist of uncontrolled movements, however, pts remain aware during episodes Paranoid Schizophrenia: -Delusions of grandeur; delusions of persecution -May believe they possess special powers Disorganized Schizophrenia: -Usually progressive and irreversible with inappropriate emotional responses; mumbled talking Personality disorders: is classified by observing a pts pattern of behavior, dysfunctional view of society, and level of sadness. Personality disorders are usually ongoing patterns of dysfunctional behavior. Psychopathic Personality: -Low morality, poor sense of responsibility, no respect for others -Impulsive behavior for immediate gratification; high frustration -Little guilt or remorse for all actions; inability to alter behavior, even with punishment -Expert liar Antisocial Behavior: -Results from particular causes (need for attention or involvement in a gang) -Typically has some concern for others -Blames other institution (family, school) for their actions -Symptoms are typically seen before 16 years of age -Violates the rights of others; lacks responsibility and emotional stability Narcissistic Behavior: -Incapable of loving others -Self-absorbed; obsessed with success and power -Unrealistic perception of self-importance Borderline Behavior: -Instability in all aspects of life -Can identify self from others -Uses projection, denial, defensiveness; unpredictable mood or behavior -Intense and uncontrolled anger; chronic feelings of emptiness Tips for interaction with an escalating patient: -Be empathetic when setting boundaries -Use a low, calm tone of voice when speaking -Do not respond defensively to pt comments -Offer choices, options or small concessions if appropriate -Do not force constant eye contact, allow the pt to look away -Be respectful and acknowledge the pts complaints or frustration -When speaking, wait for the pt to pause rather than raising your voice to be heard -Be aware of your supportive resources, including the option to leave the area if necessary -Avoid physical contact -Do not turn your back to an agitated or escalating pt -Do not allow an agitated or escalating pt to block your exit route -Maintain more space than usual between yourself and the pt for safety -Stand at an angle facing the pt so that it is easier to sidestep if necessary -Always stay at the same eye level as the pt (both standing, both sitting) -Keep hands out of your pockets both for self-protection and to avoid the appearance of concealment