managment of thyroid nodule
advertisement
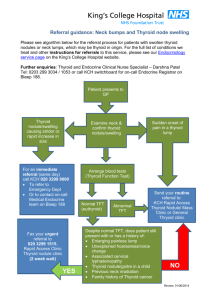
MANAGMENT OF THYROID NODULE A thyroid nodule is a discrete lesion within the thyroid gland. Thyroid nodules are four times more common in women than in men, and the incidence increases with age, radiation exposure, and reduced iodine intake. The prevalence of nodular thyroid disease has been reported to be 15% in areas of iodine deficiency. The majority of thyroid nodules are benign. Colloid nodules, cysts, and thyroiditis account for approximately 80%, and benign follicular and Hurthle cell adenomas account for 10% to 15% of all thyroid nodules. Only 5% of thyroid nodules are malignant. The challenge for a clinician is to distinguish patients with malignancy, who are treated surgically, from patients with benign disease, who are followed clinically. This is accomplished by a diagnostic approach that consists of routine fine needle aspiration biopsy (FNAB), a routine screening third-generation thyrotropin (thyroid-stimulating hormone [TSH]) level, and selective use of high-resolution ultrasound (US) and iodine-123 (I-123) thyroid scintigraphy. Laboratory Evaluation The only laboratory test that must be performed routinely in the evaluation of a patient with a thyroid nodule is a third-generation TSH level. In the majority of patients, the TSH level will be normal, indicating that the patient is euthyroid. 1) If TSH low : Approximately 10% of patients with a solitary nodule have a suppressed ( low) TSH level, which suggests a benign hyperfunctioning nodule. In these patients, a free thyroxine and a free triiodothyronine level should be measured. An I-123 thyroid scan is obtained to distinguish a hyperfunctioning (“hot”) nodule from a hypofunctioning (“cold”) nodule. If the thyroid scan confirms a functioning nodule in the setting of a low TSH, no further diagnostic evaluation is necessary. The incidence of malignancy in patients with a hyperfunctioning nodule is less than 1%. The patient can be treated with a thyroid lobectomy or with radioiodine ablation. Patients with thyrotoxicosis and a hypofunctioning nodule should undergo FNAB. 2) If TSH high : In patients with a dominant thyroid nodule and an elevated serum TSH level, a free T4 and serum antithyroperoxidase antibody level should be obtained. An elevated serum antithyroperoxidase antibody level is indicative of Hashimoto's thyroiditis. In these patients, an FNAB is indicated to rule out malignancy, including lymphoma, which accounts for a minority of thyroid cancers but is known to be associated with Hashimoto's thyroiditis. In patients with a family history of MTC or MEN 2, a basal serum calcitonin level should be obtained. Baseline levels of calcitonin greater than 100 pg/ml are highly suggestive of MTC. In patients without a history of familial MTC, routine calcitonin testing is not recommended because large studies of nodular thyroid disease have reported a prevalence of MTC of less than 1.5%. Fine Needle Aspiration Biopsy FNAB is the diagnostic procedure of choice in the evaluation of thyroid nodules, the routine use of FNAB has resulted in a reduction of unnecessary testing, and fewer operations. FNAB can be performed as either a palpation-guided or US-guided procedure. If the patient has a palpable nodule, an FNAB is performed at the initial clinic visit before any other diagnostic study. To perform an FNAB, the patient is positioned supine with the neck extended. The nodule is then identified and stabilized between the clinician's two fingers. Biopsy is then performed using a 22-gauge, 1.5-inch needle attached to a 10-ml disposable syringe. The needle is moved vigorously up and down while continuous suction is applied to the plunger of the syringe to disrupt the follicular epithelium. Aspirated material in the hub of the needle is then smeared on a slide and either fixed with alcohol or allowed to air dry. It is then submitted for staining and cytologic evaluation. It should be emphasized that this technique provides a cytologic rather than histopathologic diagnosis because it cannot provide any information about capsular or vascular invasion. Patients tolerate this procedure well, and it has a low rate of complications. The results of cytologic analysis of FNAB specimens are divided into four main categories: 1)nondiagnostic, 2) benign,3) suspicious for neoplasm, and 4) malignant (Table 1). In the absence of cytologic findings consistent with malignancy, a biopsy is considered adequate only if it contains at least 6 groups of 10 or more well-preserved follicular epithelial cells on one or more slides. Specimens not fulfilling these criteria are categorized as nondiagnostic. Nondiagnostic aspirates account for 10% to 20% of all FNAB results. Aspirates are more likely to be nondiagnostic if the nodule has a predominant cystic component or if the nodule is small or difficult to palpate. The reported incidence of malignancy is 5% to 10% in patients with a thyroid nodule and a nondiagnostic FNAB, and therefore a repeat FNAB should always be obtained. For patients with a nondiagnostic palpation-guided FNAB, a repeat FNAB can be obtained under ultrasound guidance. Using US guidance. In the majority of these patients, repeat FNAB confirmed a benign lesion and helped to avoid an unnecessary operation. If FNAB is persistently nondiagnostic, thyroid lobectomy is recommended with frozen section exam of the nodule. Table 1 -- Fine Needle Aspiration Biopsy Cytologic Diagnoses I. Nondiagnostic II. Benign a. Colloid nodule b. Adenomatous hyperplasia c. Thyroiditis III. Indeterminate or suspicious a. Consistent with a follicular neoplasm b. Consistent with a Hurthle cell neoplasm c. Suspicious for papillary carcinoma IV. Malignant a. Papillary carcinoma b. Medullary carcinoma c. Anaplastic carcinoma d. Lymphoma e. Metastatic carcinoma Repeat FNAB in a patient with an initial benign cytologic diagnosis may be of value when 1. the cytologic specimen contains abundant red blood cells that obscure the evaluation of the follicular cell nuclei, 2. a nodule is greater than 4 cm because of an increased risk of a sampling error, 3. a nodule is difficult to palpate raising concern for sampling error, 4. or a nodule undergoes progressive enlargement. Patients with a benign FNAB are asked to return in 6 months, at which time they are evaluated for an increase in nodule size or development of compressive symptoms. If the patient is asymptomatic and there is no change in the nodule size, follow-up with history, physical examination, and a screening serum TSH level is recommended at yearly intervals. Yearly US evaluation can provide objective measure of nodule size when necessary. Thyroidectomy is recommended for a progressive increase in nodule size and development of compressive symptoms. The false-negative rate for FNAB is 2% to 5%. Sampling errors tend to occur with particularly small or large nodules, hemorrhagic nodules, or multinodular glands. Cytologic analysis of FNAB specimens cannot differentiate benign and malignant follicular or Hurthle cell lesions. The risk of malignancy is approximately 20% in nodules with an FNAB interpreted as a follicular or Hurthle cell neoplasm. At present, there are no clinical, imaging, or cytologic features accurate enough to determine which patients have a malignancy; therefore patients require thyroid lobectomy to make a definitive diagnosis. If the final pathology reveals a clinically significant carcinoma, completion thyroidectomy is performed. Alternatively, patients are counseled regarding the 20% risk of their lesion being malignant and may be offered total thyroidectomy as their initial surgical procedure. Such an approach eliminates the need for reoperative surgery should the final pathology reveal malignancy; however, it guarantees that thepatient will require thyroid hormone replacement therapy. FNAB is malignant in approximately 5% of patients with a dominant thyroid nodule. Because the false-positive rate for patients with a malignant FNAB is 1% to 2%, definitive therapy is recommended on the basis of the cytologic result alone. The malignancies that FNAB can reliably identify include papillary, medullary, and anaplastic thyroid cancer. FNAB may also be helpful in diagnosing metastatic cancer and lymphoma. Diagnostic Imaging High-Resolution Ultrasound US is indicated for 1. evaluation of patients with nondiagnostic palpation-guided FNAB. In 50% of these patients, US facilitates obtaining a diagnostic aspirate. 2) 2. US is also useful in the evaluation of patients with nodules that are difficult to palpate. 3. a US examination is obtained preoperatively in patients with a thyroid nodule and a malignant FNAB to evaluate for abnormal lymph nodes in the central and lateral neck. Preoperative, high-quality US in these patients has been shown to detect lymph node or soft-tissue metastases in neck compartments believed to be uninvolved by PE in almost 40% of patients. Finding metastatic disease preoperatively alters the surgical procedure in these patients, facilitating complete resection of disease and helping to minimize local and regional recurrence. Although certain sonographic features should raise suspicion for malignancy, the presence or absence of these sonographic findings cannot reliably distinguish benign from malignant lesions. As a result, all patients with a nodule 1 cm or larger in size should be evaluated with FNAB. For lesions less than 1 cm in size however, such sonographic findings may help to determine which nodules warrant FNAB versus observation. Additional findings suggesting local invasion or the presence of lymph node metastases are worrisome for malignancy and warrant immediate FNAB, regardless of the nodule size. Sonographic findings suggestive of invasion include the extension of irregular hypoechoic lesions beyond the thyroid capsule or invasion of adjacent musculature. Additional Imaging Modalities Iodine-123 thyroid scintigraphy also has utility in selected patients with a thyroid nodule. On the basis of the pattern of radionuclide uptake, nodules are classified as hyperfunctioning (“hot”), isofunctioning, or nonfunctioning (“cold”). Hyperfunctioning nodules almost never represent malignant lesions. Isofunctioning and hypofunctioning nodules have a reported 5% to 10% risk of malignancy. Because more than 80% of nodules are hypofunctioning and only 5% to 10% are malignant, the predictive value of thyroid scintigraphy for the presence of malignancy is low. Because of the low specificity of I-123 thyroid scintigraphy, its routine use in the evaluation of patients with nodular thyroid disease is not recommended. Table -- Selected Indications for Iodine-123 Thyroid Scintigraphy in Patients with a Dominant Thyroid Nodule 1) Low TSH before performing FNAB . 2 FNAB consistent with a follicular neoplasm and a low serum TSH level . 3 Persistently nondiagnostic FNAB and a low serum TSH level source Current Surgical Therapy , J. L. Cameron, 9 th eddition, 2008 DR. S. ALDAQAL