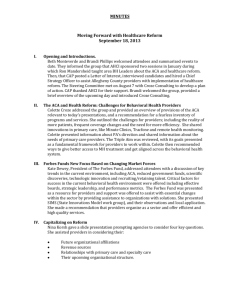
Minutes 8-7-2013 Pla.. - Conference of Allegheny Providers
advertisement
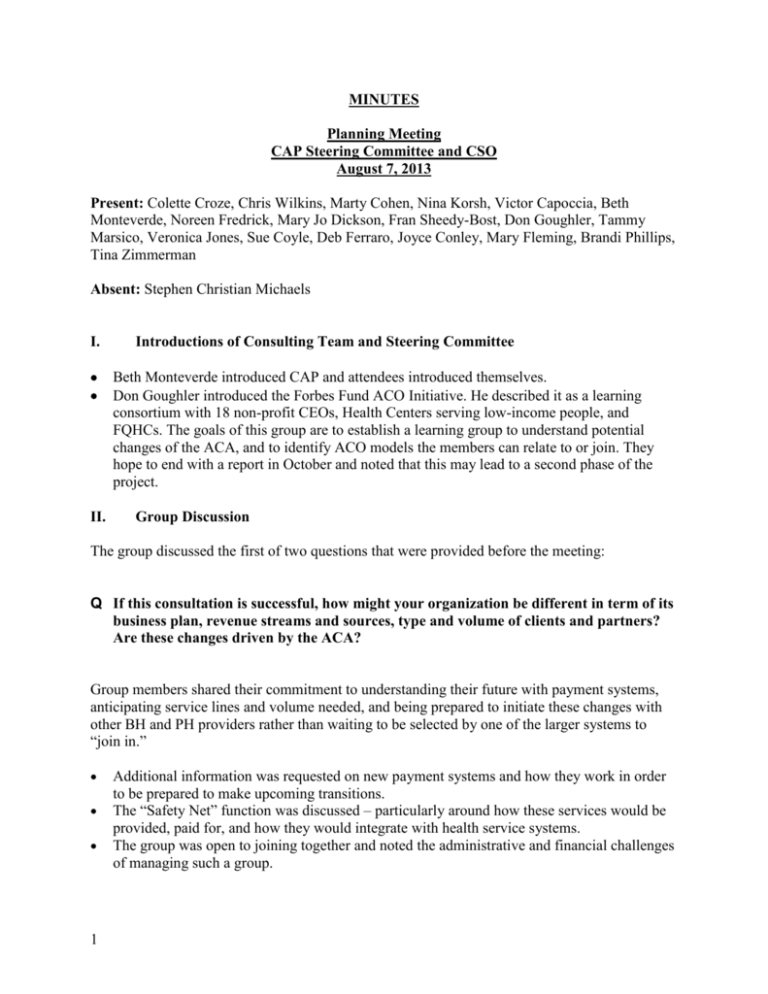
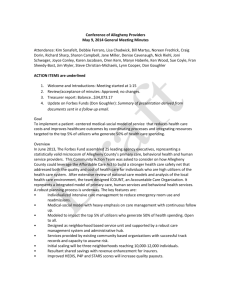
MINUTES Planning Meeting CAP Steering Committee and CSO August 7, 2013 Present: Colette Croze, Chris Wilkins, Marty Cohen, Nina Korsh, Victor Capoccia, Beth Monteverde, Noreen Fredrick, Mary Jo Dickson, Fran Sheedy-Bost, Don Goughler, Tammy Marsico, Veronica Jones, Sue Coyle, Deb Ferraro, Joyce Conley, Mary Fleming, Brandi Phillips, Tina Zimmerman Absent: Stephen Christian Michaels I. II. Introductions of Consulting Team and Steering Committee Beth Monteverde introduced CAP and attendees introduced themselves. Don Goughler introduced the Forbes Fund ACO Initiative. He described it as a learning consortium with 18 non-profit CEOs, Health Centers serving low-income people, and FQHCs. The goals of this group are to establish a learning group to understand potential changes of the ACA, and to identify ACO models the members can relate to or join. They hope to end with a report in October and noted that this may lead to a second phase of the project. Group Discussion The group discussed the first of two questions that were provided before the meeting: Q If this consultation is successful, how might your organization be different in term of its business plan, revenue streams and sources, type and volume of clients and partners? Are these changes driven by the ACA? Group members shared their commitment to understanding their future with payment systems, anticipating service lines and volume needed, and being prepared to initiate these changes with other BH and PH providers rather than waiting to be selected by one of the larger systems to “join in.” 1 Additional information was requested on new payment systems and how they work in order to be prepared to make upcoming transitions. The “Safety Net” function was discussed – particularly around how these services would be provided, paid for, and how they would integrate with health service systems. The group was open to joining together and noted the administrative and financial challenges of managing such a group. The size disadvantage of the MH providers and their lack of “experts” in compliance law, and/or legal or research departments were also noted. The Croze team noted that the public system must accommodate the speed at which major players are moving. BH providers must have a product and must show the value of the product. They supported the regrouping of providers and noted three emerging themes: independent organizations independent organizations with coordination in delivery of services a more formal network of providers The group discussed the terrain of healthcare in Pittsburgh: Providers identified the primary health systems as: UPMC, Allegheny Network (Highmark), Community Care, Medicare, and Medicaid Fee for Service. ID services are reimbursed from the State with negotiable rates. Prevention dollars (SA) have been flat and a small amount of education dollars flow into the system as the schools pay for MH care. As systems were identified, there was some discussion of 17 FQHCs in the area that are unaffiliated with the two large health systems. Most physicians in this area are affiliated with a health system or hospital and there are only a few small non-affiliated hospitals. Other issues: lack of a public planning process; health policy is driven by UPMC leadership (Jeff Romoff) and the 2 players are large employers with union support Q Exploration of current innovations in the local Pittsburgh market and how those innovations could position certain types of providers as competitors in the traditionally publicly funded network. A partial list of area “Patient Centered Medical Homes” was shared: MYCS piloting a medical home and bringing PH to the BH site Mercy Behavioral Health has an integrated care clinic Milestone has a CMS grant JHCF and PRHI sponsored delivery of The Wagner Chronic Care model to 4 regional sites using BH staff to offer Care Coordination and BH care. Regarding interventions in Care Coordination and Chronic Disease Management, the group reported: MYCS is assigning individuals with chronic medical conditions to treatment teams. Wesley Spectrum has been invited by Pediatric Alliance to develop a BH Clinical Home for children. 2 A small number of local ventures in payment reform were reported, though these projects have few financial details spelled out to date. Additionally, there was minimal consumer advocacy and few tele-health ventures. III. IV. One effort to move to a case rate (in the BH Home for Children) C-SNP (a program for clients with dual eligibility, MC/MCD) project with UPMC. Desired Outcomes Identified A different relationship with ACOs (or other groupings) of health providers Ability to manage an organization with various forms of payment To actively relate to primary care and related health services Better understanding of how to use “safety net services” and funds in concert with other reimbursement Identifying collaborations resulting in improved administrative efficiencies and holistic clinical services Bidirectional communication among all players Detailed Review of the Proposal and Tasks The following approach was agreed upon in terms of next steps: Phase One A day long learning session on September 18, 2013 Consultants will format as a large group meeting or develop breakouts Topic areas may include Financing Models, Culture Changes, and Relating to ACOs Up to three follow-up teleconferences Debriefing with Steering Committee Members Phase Two Add Board Member participation Consultants will present provider profiles, predict some upcoming scenarios and identify possible business pathways Providers will complete a self-assessment Phase Three Providers will opt in (or out) of the process Providers will obtain Board buy-in Providers will identify the groupings within which they want to collaborate Providers will identify their change team (within their agency and/or group) Consultants shared some keys for success; integration, invention, and market insertion and penetration along with one example of how these have been put to use. The group conversed 3 about decision making and the need to make decisions based on information and/or resources available at the time. Board Preparation: Colette suggested a framework for Board discussions, including the presentation of quality, access and economy of service as small steps that translate into improved financial health for the organization. Nina requested that the group also look at the NIATX site and learn about Rapid Cycle Change. Others offered BH Biz, and resources offered by the American College of Healthcare Executives as good sources of information about healthcare reform for providers. V. 4 Next Steps/Action Items The group will review materials and RSVP to the September 18th event The Consultants will continue to outline the next meeting and the upcoming calendar and will get this back to AHCI for dissemination in late August. AHCI to send invitation for September 18 Kick-Off meeting to BH, D&A and ID providers and county representatives. Croze Consulting to review Scope of Work and offer dates for future in-person and telephone meetings. AHCI to send Ron Mandersheid slides to Croze Consulting. AHCI to request provider data from providers who plan to attend September 18 meeting. AHCI to post minutes to CAP website.