Executive Staff and Clinical Director Morning Huddle Quality Focus
advertisement

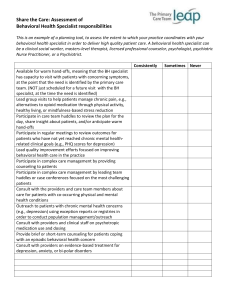
Best Practice Submission Executive Staff and Clinical Director Morning Huddle Quality Focus Points of Contact: MAJ (P) Matt Fandre, Army-Baylor Class of 2013, (931) 436-5146; Jon Turton, Interim CEO, (210) 297-5600; Tracy Sites, COO (210) 297-5600; Dr. Richard Marple, CMO (210) 297-5600 Group Involved with the project: The St. Luke’s Baptist Hospital A-Team (executive staff) & St. Luke’s Baptist Hospital Quality Team Submitted by MAJ (P) Matthew Fandre Executive Summary: St. Luke’s Baptist Hospital uses daily unit director huddles to disseminate key information and receive unit director reports. Previously, daily huddles consisted of sharing a safety story, reviewing the census on each floor, and making general announcements. After attending morning huddles at each of the other four Baptist Hospitals, I met with the members of the hospital A-team to design a revamp of morning huddles to increase director accountability, facilitate discharges, emphasize quality metrics such as core measures, and improve communication. After implementation, attendance increased, the meetings had greater purpose and utility, and the hospital demonstrated increases in core measures performance, greater patient discharge efficiency, and decreases in operating room turn-over time. Effective huddles with directed executive attention on important and key metrics can result in improvements if structured and run effectively. Competencies Addressed Strategic Planning Change Management Financial Management Strategic Communications Patient Safety St. Luke’s Baptist Hospital is a for-profit, freestanding, 280 bed hospital located in the medical center campus NW of San Antonio. St. Luke’s is also part of 5-hospital Baptist Health System in San Antonio and owned by Vanguard Health Systems in Nashville, TN. The major revenue generators for the hospital are elective surgeries and inpatient services. Although St. Luke’s has a growing L&D service line and NICU, the primary source of net income/high margin procedures is the elective outpatient surgeries. Objective of the Best Practice: Quality is the essential element for hospitals in the 21st century. Not only does quality incorporate effective clinical practice, it encompasses fiscal stewardship. Within civilian practices, the major sets of quality metrics are CMS’ Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) and Core Metric Measurements which are part of the Value Based Purchasing program. Failure to surpass quality percentile thresholds will result is loss of up to 2% of retained CMS payments for in-patient services. For St. Luke’s, the total amount potentially withheld is $700,000; $490,000 (70%) is from Core Measure performance. St. Luke’s Baptist Hospital and Baptist Health System utilizes daily direct meetings to disseminate key information, stress safety and quality and strengthen the culture. The goal of this best practice is to maximize the value of daily huddles to improve quality, performance and communication. Background: St. Luke’s Baptist Hospital began executive led morning safety huddles with all clinical directors in 2010. These stand-tos, named for the fact that no one sits during the huddle, were initially designed to focus on safety. The huddles then expanded to include snapshots of current patient census, core-measure patients, and distribution of key hospital operational information. Although the value of the huddles was rapidly evident in distributing information regarding the daily census and focus of the day, the meetings failed to generate longitudinal accountability for quality metrics from the clinical directors. Furthermore, additional emphasis on organizational values and culture was missing from these daily meetings. Literature Review: According to the Institutes of Healthcare Improvement (IHI), huddles “enable teams to have frequent but short briefings” in order to “stay informed, review work, make plans, and move ahead rapidly” (IHI, 2004). Huddles are not a new concept; even the casual observer of American football has observed these brief meetings in which the entire team is specifically focused on its current purpose. Huddles should have pre-set and consistent structure, occur at the same time and location, and a follow a limited agenda (Dingley, Daugherty, Derieg & Persing, 2008). Effective huddles result in fewer disruptions in the day, prioritization of effort for the day, and sharing of best practices. Multiple articles exist exploring the use of meetings to improve performance, meet productivity goals, or reach quality measurements; however, the articles found in my literature review focused on individual units or functional areas and not on huddles designed and led by the executive leadership level of a healthcare organization. Implementation Methods: In collaboration with St. Luke’s COO, I attended morning huddles at each of the other Baptist Health System hospitals to evaluate their processes and assess for innovative and effective methods of promoting quality focus and individual and department accountability. I presented my findings to the entire A-team (C-suite leadership) and led an hour long meeting in which the A-team collectively evaluated which metrics were most important and needed to be reported daily. To facilitate these new morning huddles, I created a daily huddle sheet (see Appendix A). The hospital key statistics section combines data from the daily house officer’s report, the system wide daily flash report, and the system discharge by noon report. This data is entered daily by the facility financial analyst. Additionally, the time of the huddle was moved from 0845 to 1000 to allow unit directors uninterrupted, meetingfree time to talk with their staff, handle patient and administrative issues and prepare for morning huddle. Finally, the new format allowed for the systematic delivery of key announcements and information to the directors and staff. The new structure was implemented on 5NOV12. After 30 days, quality data from CMS’ core measures and the facility rate for discharges by noon was evaluated for differences. Additionally, overall attendance and OR turn-over times were evaluated. Results: Resistance to the change in focus and increased director accountability was minimal. After a few days of refocusing the director’s responsibilities and priorities, the flow of the daily huddles was efficient and effective. Unit directors came prepared with their unit’s information and attendance increased without specific direction from the A-team. Additionally, A-team attendance also increased supporting the value and importance of this meeting. The greatest benefit from this transition was unit director accountability and their focus on priority metrics. Unfortunately, the effects of this change on many key metrics (HCAHPS, employee engagement scores, and staff turn-over) will take months to assess due to the delay in data reporting and infrequency of measurement. The pre-change and postchange data is displayed below. As shown by this data, improvement was evident in each area. Further analysis will be required to evaluate for effects on HCAHPS, employee engagement, and staff turn-over as well as to assess for longitudinal benefit. Attendance OR Turn-over time Core Measures Discharges by Noon Prior to implementation 16 directors and A-team 29 minutes 92.1% 10.8% Post implementation 29 directors and A-team 24 minutes 96.1% 16.8% Change 45% increase 17% decrease 4% absolute rate increase 36% increase Conclusion: As with any initiative, leader presence and focus will encourage and guide behaviors and actions. By deliberately focusing on unit director accountability, core measure performance, and discharge efficiency, the revamped morning huddles changed behavior and improved individual and organizational performance. Additionally, since implementation, we have witnessed improved attendance, greater overall meeting utility, and provided a structured method for information dissemination. In the future, as one focus area’s performance improves, executive leadership can use the huddles and the revised report to change the focus area and emphasize other metrics needing improvement (e.g. HCAHPS, annual evaluations, Joint Commission readiness). References Institute For Healthcare Improvement. 2004. Huddles. Retrieved from http://www.ihi.org/knowledge/Pages/Tools/Huddles.aspx accessed on 20 November, 2012. Dingley, C., Daugherty, R., Derieg M.K., Persing, R. 2008 Improving Patient Safety Through Communication Strategy Enhancements. In K. Henriksne, J.B. Battles, M.A. Keyes, M. L. Grady (Eds.), Advances in patient safety: New directions and alternative approaches, Vol. 3: Performance and Tools. Rockville, MD: Agency for Healthcare Research and Quality. Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK43663/#advances-dingley_14.r22 on 20 November, 2012.