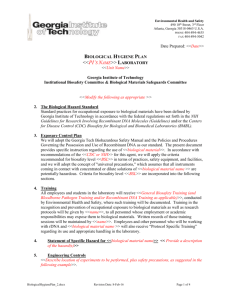
LABORATORY SPECIFIC EXPOSURE CONTROL PLAN

LABORATORY-SPECIFIC BIOHAZARD EXPOSURE CONTROL PLAN
I. GENERAL INFORMATION
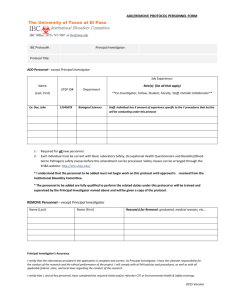
1. PRINCIPAL INVESTIGATOR INFORMATION: a. Name: b. Laboratory Location(s): c. Phone:
2. DATE OF PLAN PREPARATION/REQUIRED APPROVALS/SIGNATURES: a. Date: b. Principal Investigator: c. Research Safety Officer: d. Chairperson, VA CHBSC:
Deborah Smith
Medhi Wangpaichitr, Ph.D.
e. Date Plan approved:
3. HAZARD INFORMATION:
b. Location and use of storage:
c. Proposed use:
II. EXPOSURE DETERMINATION PROCEDURES
The Exposure Determination Form is appended as Appendix Form 1 to this Biosafety Plan. The form identifies all employees by job classification and anticipated exposure level for each position. A copy of the form is also posted in the laboratory work area for ready reference.
The Exposure Control Form is appended as Appendix Form 2 to this Biosafety Plan. This form lists actual tasks for each job classification having Level 1 exposure, and the personal protection equipment requirements when performing these tasks. A copy of the Exposure Control Form is also posted in the laboratory work area.
III. METHODS OF COMPLIANCE:
Page 1 of 9
LABORATORY PRACTICES AND PROCEDURES
A.
ACCESS INTO LABORATORY: a.
b.
Access into the laboratory is restricted at the discretion of the Principal Investigator
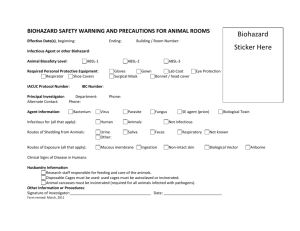
A BIOHAZARD warning sign is posted at the entrance to the laboratory and identifies: (1) the biohazards by name; (2) the specific nature of the health and safety risks associated with the named biohazards; (3) any restrictions and/or requirements for entry; and, (4) the name and contact number of the person to be notified in the event of an emergency.
B.
ENGINEERING CONTROLS: a.
Hand washing and eye wash facilities are located in the laboratory. Access to them b.
must be kept unblocked at all times.
Biohazard sharps-containers for deposit of contaminated sharps, including pipette tips c.
d.
and hard plastic, are readily accessible in all laboratory work areas.
A BSL-2 safety cabinet is located in the work area for use during experiments.
Containers, which can be closed, are available for deposit of liquid wastes capable of releasing liquids, or reusable items for subsequent safe transport to the e.
f.
decontaminated area. Red biohazard bag containers are available for deposit of solid disposable contaminated wastes (gowns, gloves, etc.)
Recommended personal protection equipment items are readily available in the work area.
An autoclave for waste decontamination is located in close proximity to the laboratory.
C.
SIGNAGE AND LABELING:
The following signage and labeling program is in effect. a.
A BIOHAZARD warning sign is posted at the entrance of all laboratory rooms where b.
biohazards are being handled and processed.
Specific items requiring labeling include: freezers, all containers for storage of biohazardous materials, biosafety cabinets, and disposal containers for sharps.
D.
WORK PRACTICE CONTROLS:
The following work practice controls apply to the laboratory. a.
Standard Practices/ Procedures:
(1) Universal precautions must be observed at all times.
(2) Only essential personnel are allowed in the laboratory work areas.
(3) Persons 18 years of age, or younger, are not permitted to work with any biohazardous material.
(4) Biohazardous materials must be stored in non-spill, air tight, puncture resistant containers, which have a label identifying contents.
(5) Hand washing is required following handling of biohazardous materials, and before leaving the laboratory.
(6) Doors are to be kept closed when work is in progress.
(7) Eating, drinking, smoking, etc. is not permitted in any laboratory work areas.
(8) Storage of food or drinks in refrigerators or freezers is prohibited, unless specifically identified for this purpose.
Page 2 of 9
(9) Mouth pipetting of biohazardous materials is strictly prohibited. Only mechanical devices are to be used.
(10) Procedures should always be performed in a manner which minimizes the creation of aerosols to reduce an exposure risk from inhalation.
(11) Personal protection equipment as recommended for certain tasks (see Exposure Control
Form and Special Practices) must be used.
(12) Personal protection equipment, including laboratory coats is always removed before leaving the laboratory. Disposable items (single-use) are to be deposited in the red biohazard bag container located in the work area.
(13) All biohazard solid wastes are to be sterilized by autoclaving prior to final disposal.
(14) Following completion of procedures, work bench surfaces are to be decontaminated with 10% bleach solution follow by 70% ethanol. b.
Special Practices:
(1) Only persons who have been advised of the specific biohazards associated with the research activity, and who have the appropriate training will be allowed to work in the laboratory.
(2) Use of cell lines must be performed in the Biosafety cabinet.
(3) Spills and accidents that result in overt exposure to any biohazardous material have to be immediately reported to the Principal Investigator. Medical evaluation, surveillance, and post-exposure treatment will be provided, as appropriate, and written records will be maintained.
E.
PERSONAL PROTECTION EQUIPMENT a.
Personal protection equipment available includes laboratory coats, disposable outer b.
c.
d.
garments, latex or nitrile gloves, safety glasses/goggles and surgical masks. The above equipment is available at no cost to you.
Hypoallergenic gloves will be made available if you are allergic to the gloves normally provided.
Disposable personal equipment is removed and placed in the red biohazard bag container before leaving the work area.
Soiled laboratory coats and uniforms are to be placed in designated laundry bags.
Laundering of these garments at home is not permitted.
F.
CLEANING AND DECONTAMINATION: a.
Cleaning Procedures:
(1) The laboratory is to be kept clean, orderly, and free of extraneous supplies and equipment.
(2) A cleaning schedule is appended as Appendix Form 3 to this Biosafety Plan. It specifies what is to be cleaned, the frequency of cleaning, cleansers and/or disinfectants to be used, the procedures of cleaning and any special instructions which may apply. A copy of the cleaning schedule is also posted in the work areas for ready reference.
(3) Household gloves can be worn when performing cleaning tasks.
Special practices:
1.
Prior to disposal, add an equal volume of 10% bleach solution to the liquid waste solution.
2.
All waste items must be autoclaved before disposal. b.
Spills Response Procedures:
(1) Reporting Requirements:
Page 3 of 9
(a) Any spill of a biohazardous material, regardless of degree, must be reported to the
Principal Investigator.
(2) Specific Procedures:
(a) A spill kit is located in the laboratory. It contains extra items of personal protection equipment, red biohazard disposal bags, absorbent materials, Sporicidin disinfectant, and other items necessary for the cleanup of accidental spills.
(b) Prompt containment of any spill should be standard practice.
(c) For minor spills (amount of material released is small, less than 10mls): Promptly confine the area of contamination by covering area with absorbent material, and disinfecting with Sporicidin or 10% bleach solution. Wait 30 minutes, then clean spill area. Use appropriate personal protection equipment during cleanup, and change gloves frequently.
For major spills (too large to handle by spill kit, or large area involved): Immediately evacuate the area and notify Principal Investigator, Research Safety Officer (X6602) and the Environmental, Health and Safety Office (X4220).
G.
DISPOSAL OF WASTES: a.
Appropriate containers for containment and disposal of biohazardous wastes must be b.
c.
readily accessible throughout the work area.
Sharps are deposited only in approved biohazard sharps disposal container. When filled
(3/4 capacity), secure cover in place and tape. Disinfect (10% bleach) surfaces prior to removal by Environmental Management Service for proper disposal. Never overfill or place hands into these containers.
Liquid wastes are placed in containers within a transport container. Liquid waste d.
e.
containers should only be filled to one-half maximum capacity. Following completion of work, containers are closed loosely and transported in a safe manner to the autoclave room. These wastes are to be autoclaved at a minimum of 15 min at 121 o C and 15 psi, followed by disposal through the sanitary sewer system.
Contaminated reusable materials are placed in an autoclavable, durable, transport container. Solid wastes capable of releasing liquids (e.g., culture plates) are placed in autoclavable biohazard bags in the same container. When work is completed, biohazard bags are close (tape loosely), and the transport container is transferred in a safe manner to the autoclave room. The container and contents are autoclaved at a minimum of 30 min at 121 o C and 15 psi, followed by a 10 to 15 dry cycle. Sterilized solid waste bags are discarded with other contaminated solid waste materials in red biohazard disposal bags.
Other contaminated sold waste materials are placed in red trash containers lined with red biohazard disposal bags. When filled, bags are closed securely (use twist ties), after which they are to be picked up by Environmental Management Service for proper a.
disposal.
H.
AUTOCLAVE PROCEDURES
Document in the autoclave log book the name of the operator, nature of the load, highest temperature reached, and length of time this temperature is maintained, and the results of the autoclave temperature-sensitive indicator tape which must be b.
attached to each load.
Sterility tests, using a biological sterilization indicator, are to be performed weekly to assure proper operation of the autoclave. The results of these tests are to be documented in the autoclave log book.
Page 4 of 9
c.
Immediately report any autoclave malfunction, and do not use until repairs have been made.
I.
PACKING AND SHIPPING OF HAZARDOUS MATERIALS a.
All laboratory personnel involved with packaging and shipping of hazardous chemical and/or biological samples/wastes are required to complete and regularly update an
IATA (International Air-Transport Association) approved course in proper shipping procedures. Various courses qualify including one at the U.S. Department of Veterans
Affairs VALO university site. Contact the Administrative Officer for Research about other certification routes.
IV. EXPOSURE INCIDENTS
A.
FIRST-AID MEASURES a.
For contact with intact skin, the area will be washed with soap and water for 10 minutes. If eyes or mucous membranes are affected flush with running water for 15 minutes. Notify the Principal Investigator and report to the Employee Health Office in b.
c.
room 1D182.
If exposure is the result of a clean cut, puncture, or needle-stick, bleeding will be stopped immediately. The area will be washed with soap and water, and the exposed individual will then report to Employee Health (1D 182) or Emergency Room (after hours) immediately. Notify the Principal Investigator.
If the exposure is a result from broken glass, bleeding will be stopped immediately. The area will be cleaned and washed with soap and water, and the exposed individual will then report to Employee Health (1D 182) or Emergency Room (after hours) immediately. Notify the Principal Investigator.
B.
EVALUATION AND FOLLOW-UP TREATMENT a.
Employees reporting a significant occupational exposure incident are provided immediate confidential medical evaluation and follow-up treatment through Employee b.
c.
d.
Health Office.
In the event of an exposure incident you should be prepared to describe the route of exposure and circumstances of the incident, and other relevant facts, which can aid in the medical evaluation.
The health care professional will conduct a thorough evaluation and recommend any follow-up treatment.
In order for anyone to obtain a copy of the Employee Health Medical Evaluation, a release of Medical Records form must be completed. The health care professional, however, may provide a written opinion to the Principal Investigator, if requested. This opinion will only disclose confirmation that you have been informed of the results of the evaluation and of any recommended follow-up treatment; specific details will not be provided.
C.
IMMUNIZATION PROGRAM a.
The hepatitis B vaccination is offered to all employees having direct contact with human blood or other potentially infectious materials. The vaccination program is administered through the Employee Health Office located in room 1D182.
Page 5 of 9
b.
c.
All employees are required to be enrolled in, and comply with, the requirements of the medical campus PPD - Skin-testing program.
Rabies and tetanus immunizations are offered to all animal-care technicians, and other personnel who have substantial contact with animals in the animal facility.
D.
REPORTING REQUIREMENTS a.
A written report concerning an exposure incident or injury must be submitted to the
Principal Investigator within 24 hours of occurrence. The report must detail the circumstances of the incident so that decisions regarding the appropriate corrective actions can be made and implemented. b.
a.
In all cases of an exposure incident certain forms and reports must be completed. Your cooperation is expected.
E.
INFORMATION AND TRAINING:
At the time of initial assignment you will be advised of the specific biohazards present in the workplace, and you will be provided specific training in procedures which are to be b.
followed in the laboratory room.
You will be provided access to relevant safety manuals and the laboratory-specific c.
d.
Biosafety Plan (this document).
You will be retrained in safety practices whenever laboratory or animal procedures are modified, or when new tasks or responsibilities are assigned that might affect your occupational exposure risk.
All personnel involved in this research project are required to attend medical campus and laboratory-specific health and safety training classes for biologic or other hazards. a.
You will be informed, in advance, of all such training classes.
F.
COMPLIANCE MONITORING:
Your work practices in the laboratory will be monitored periodically by the Principal
Investigator. b.
In the event that your practices are not in compliance as stipulated in this Biosafety
Plan, you will be so notified and retrained in the proper procedures to correct the c.
d.
deficiency. You will then be expected to follow the proper safety measures.
All incidents of non-compliance, and recommended corrective actions, will be documented in writing.
You should clearly understand that repeated incidents of non-compliance with required safety practices or mandated use of personal protection equipment will lead to disciplinary actions against you. Such actions may result in your reassignment to other duties or termination of your employment.
V. REFERENCES
1. Miami VA Medical Research Service, Research Service Biosafety Manual.
2. VA Infection Control Manual.
3. CDC/NIH Biosafety in Microbiological and Biomedical Laboratories, 5 th Edition, 2009.
VI. FORMS
1. Form 1: Exposure Determination Form
2. Form 2: Exposure Control Form
3. Form 3: Cleaning Schedule
Page 6 of 9
APPENDIX FORM 1.
1
EXPOSURE DETERMINATION
1 Position: List each employee, including PI, who works in the laboratory by job classification. Do not identify by name.
Anticipated exposure Level:
Level-I: Tasks performed involve routine, or have the potential for exposure to the identified biohazard, regardless of frequency or use of PPE, and which exists on the basis of position description or statement of function.
Level-II: Tasks performed do not involve routine, or have the potential or exposure to the identified biohazard, and Level-I tasks are not a condition of employment as based on position description or statement of function.
Page 7 of 9
APPENDIX FORM 2.
2
EXPOSURE CONTROL
2 Position: List only those positions identified on the Exposure Determination Form as having Level-I anticipated exposure.
Activity: For each listed position provide a brief description of each task or activity associated with an anticipated exposure to the identified biohazard. Unrelated tasks or activities must be listed separately. Examples include: preparation, manipulations, analysis of experimental material, transport of biohazardous agent or material, cleaning and decontamination, disposal of wastes.
PPE: For each task or activity, specify PPE and other requirements (use of safety transport containers, Biosafety cabinet, splash shield, etc.) which must be used to reduce or eliminate the occupational exposure risk to the identified biohazard. Hand washing and wearing of gloves are the minimum requirements.
Page 8 of 9
APPENDIX FORM 3.
3
CLEANING SCHEDULE
3 Work Area/Equipment: Individually list all work areas, equipment, or other items to be cleaned.
Frequency: For each work area, equipment, or other items listed, specify frequency of cleaning.
Procedure: Specify cleaning agent(s) (disinfectant) to be used, and procedures to be followed. Be sure to specify any special procedures that may apply.
Page 9 of 9