Executive summary to phase one consultation of the integrated
advertisement

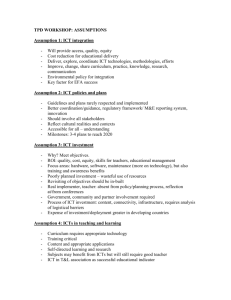
Executive summary following the outcome of the phase one consultation of the integrated services transformation of adults and older people’s mental health and community services The staff consultation on proposals to further integrate community and mental health services for adults and older people in Cambridgeshire and Peterborough took place between 22 June and 5 August. Staff, key stakeholders and partners were asked for their views on plans to better align these services to the needs of patients by reshaping them around the 108 GP practices in the county, with 16 neighbourhood teams (NTs), which sit underneath four integrated care teams (ICTs). Views were also sought on plans to redesign older people’s mental health services to deliver ‘stepped care’ therapy and dementia assessment and mental health professionals working in each neighbourhood team. Wider stakeholders were also engaged with, including Uniting Care, GPs, councils and others. The consultation was designed to engage with as many staff as possible, through 30 booked engagement events across the county which were all well attended. As set out in the engagement events, CPFT sought to undertake a true consultation: to listen, consider and respond. As a result, a significant amount of feedback was received that helped determine how the new proposed model of service provision would operate in practice, which has led to some revisions but at the same time staying true to the vision of the model. This executive summary restates how the NTs will work in practice and the amendments that have been made as a result of the phase one consultation feedback and is intended to accompany the Way Forward paper which explains the following in detail:- Direction of travel The formation of 16 NTs is phase one of a whole system transformation of community health services over the next five years. Once the full transformation of services is complete, community services will provide: A single point of contact for urgent referrals A 24/7 service for urgent referrals – Joint Emergency Team (JET) A single point of contact for planned referrals open to professionals and patients/carers A workforce that is equipped to work efficiently and effectively through use of mobile technology and agile working An estate that is lean, fit for purpose, has bases local to groups of GP practices and where people live A health and social care workforce that is skilled, equipped and confident, with opportunities to progress as clinicians, managers and leaders A career progression structure for non-registered staff who are encouraged to develop skills and competencies to achieve more responsible roles, including support to become registered practitioners, and where newly registered practitioners take up preceptorships within our teams A leadership and operational structure that is robust to support people to develop and progress A service model that has a culture of recovery, independence and self-management at its heart that actively identifies those most at risk of admission Teams that work with local community partners, especially primary care, social care and re-ablement services to support and develop resilient local communities. The transformation is designed to ensure that the statements below come to life: In 2018 patients and carers will say: o o o o “My care and support is personalised, joined up and co-ordinated around me.” “My care and support enables me to exercise choice, manage my own health and wellbeing and maintain my independence.” “My care is safe and effective and is given by caring, compassionate staff who work really well together around me.” “My care is delivered in the right place at the right time, any day of the week that I need it, close to my home.” In 2018 staff will say: o “This is the place to be, we are a real team, my skills are the best they’ve ever been and we are making a real difference to patients.” o “It reminds me why I joined the NHS.” How the neighbourhood teams will work in practice Once established and fully recruited to, 16 NTs will operate between 8am and 8pm, 365 days a year, each covering between 3 and 13 GP practices and populations of over-65s between 5,700 and 14,000. NTs are the physical and mental health care hub of the local community, integrated with GPs, primary care, social care and the third and independent sector, providing responsive, expert care and treatment to local people. Evidence based patient pathways under development for the main health conditions will ensure consistency across NTs and a case management model will ensure identification of those people most in need of co-ordinated care and at risk of hospital or care home admission. NTs will be led by a team manager of any profession and will comprise between 30 and 65 staff including integrated support workers, administrative staff, district nurses, mental health nurses, community matrons, occupational therapists and physiotherapists. They will provide a range of functions including case management, care co-ordination, integrated physical and mental health, integrated rehabilitation and mental health care, palliative care, supporting people to access personal budgets and building community resilience. NTs will work in partnership with their ICT colleagues including out of hours nursing, psychiatry, podiatry, dietetics, mental health therapy services, memory service, speech and language therapy and JET. Staff will operate within clear governance structures that support patient and staff safety, clinical effectiveness, efficient and productive practice, team and organisational learning, and staff and team development. ICTs and NTs will have a joined up approach to the management of all referrals through dedicated unplanned and planned referral services. Mental health social workers will work with the ICTs, line managed by the Head of Social Work for Older People. Referrals will be made via the locality mental health referral point. Health and social care will work together to ensure referrals are appropriately allocated, using the Care Programme Approach. Health funded mental health integrated workers will be in the NTs. Social care funded team support workers will be located with social workers in the ICTs. These team support workers will support the development of support plans and care packages, as well as provide practical support and interventions. The interface between older people’s social care and the NTs is crucial. Work is taking place with Cambridgeshire County Council and Peterborough City Council to develop the detail of an integrated model to align operating structures and processes, exploring the options for co-location where possible. Summary of the main changes as a result of the consultation Leadership and operational structure – concerns were raised about the capacity of senior managers to adequately support the 16 NTs and 4 ICTs. We have therefore worked with staff to develop an interim senior clinical and operational management structure to provide more robust support, which will be fully implemented after the phase 2 of the consultation with the proposed ICT staff. Neighbourhood teams band 7 team manager roles and development – comments were received about the scope and responsibilities of NT team manager roles, particularly the larger NTs. We have responded by proposing the enhanced clinical and operational management structure referred to above, which includes a band 8a manager working across NTs in each locality and more robust clinical supervision through band 8a nursing and allied health professional roles. We have also further expanded on the development programme for the individuals successfully appointed to these posts, which includes workshop days prior to the implementation of the NT’s and the formation of an Action Learning Set for at least the first six months of the operation of the NTs to support their ongoing development needs. Band 8a posts in phase 1 – feedback was received during the consultation about whether these posts should be included in phase one or phase 2 of the consultation. After careful consideration it has been decided that these posts will continue to be ‘at risk’ in phase one as their current roles will cease to exist when the NTs launch. They will be asked if they would like to apply for a band 7 role in phase one or defer a preference for a role until phase 2. Therapies – occupational therapists and physiotherapists were included in the first phase of the consultation, although it was acknowledged that where staff numbers were too small to effectively work in NTs staff would be asked how this might work in practice. Following discussions with therapy staff it was agreed that most occupational therapists and physiotherapists will be in the NTs, but that the following specialist teams will be part of the ICTs – community neuro rehabilitation, speech and language therapy and externally funded re-ablement posts within Greater Cambridge ICT. Reallocation of community matron (CM) roles – it has been decided to retain the community matron role in NTs, which reflects their expertise and experience, although it is anticipated that there will be an expansion of case management and care co-ordination across all staff groups in time. The consultation allocated a community matron to each NT, but following feedback it was decided that it was more clinically appropriate to better align them to population size. This has seen a reduction of one CM in Greater Cambridgeshire and increase of one in Ely and the Fens. Mental health amendments – a small number of minor adjustments were made which are described in section 5 of the Way Forward paper. Administrative staff – these staff are crucial to the success of the integrated care model and we were keen to hear their views on how this might work in practice. We are working with representatives from each locality to review the administrative staff structure within NTs, ICTs and the planned care centre. The proposals will be part of the phase 2 consultation. Job descriptions – we received a lot of comments about job descriptions (JDs) after developing seven generic core JDs. Following the consultation feedback we have worked with staff side and professional groups to more fully reflect specific professional roles and registered qualifications. At the same time we have developed a generic job description for bands 2-4 Integrated Care Workers who will support the multidisciplinary NTs. Team bases and agile working – the estates team has met with staff to understand the accommodation requirements for the 16 NT bases and 4 ICT bases. Key principles that have been agreed are that: ICT bases will be in each locality supporting NTs NTs will be co-terminus with GP surgery clusters Scaled to suit staff working patterns and improved IT for agile working Cost benefits to reduce overheads and improve efficiencies. Work is on-going to confirm bases and timescales for occupancy. Agile working is also a key enabler for the new model so we will trial 100 new mobile devices which allow remote access to SystmOne. Shift patterns and the management of rotas – it is anticipated that NTs will eventually operate 8am-8pm, 7 days a week, and that staff will be rostered to cover these hours, taking into account peak demand periods. Although staff were not formally consulted on this during phase 1, it is likely they will be consulted on extended hours in the future. Workforce model The below tables illustrate the clinical workforce model for the NT’s and the mental health element of the ICT’s which are the elements of the services included in the phase 1 consultation. These tables reflect the changes made as part of the consultation as discussed on the previous pages. Neighbourhood team workforce ICT Fenland Peterborough Huntingdon Cambridge Therapist MH NT Community (OT/ Specialist Manager Matron Phsyio) practitioner NT Nurse B7 B7 B7 B7 B6 Wisbech 1 1 1 6 2 Fenland 1 2 1 5 Isle of Ely 1 1 1 8 Borderline Central 1 1 1 4 Peterborough City 1 1 1 1 5 2 Peterborough City 2 1 1 1 7 Borderline 1 1 1 7 Huntingdon Central 1 1 1 5 2 St Neots 1 1 1 6 St Ives 1 1 1 7 Cambridge East 1 1 1 4 Cambridge City North 1 1 1 6 Cambridge South Villages 1 1 1 2 2 Cambridge North Villages 1 1 1 4 Cambridge City South 1 1 3 1 Cambridge City 1 1 3 NT Key OT – Occupational Therapist MH – Mental Health CPN – Community Psychiatric Nurse SW – Social Worked ISW – Integrated Support Worker MH Therapists CPN/OT/ (OT/ SW Physio) NT Nurse B6 B6 B5 2 8.9 16 2 3.8 13 2 7 19 2 1 10 2 2 13 2 3 16 1 2.5 17 2 2.5 12 2 4.1 15 2 5.6 16 1 3 9 1 5 14 2 2.9 6 1 3 10 1 3.5 8 1 2.5 8 MH CPN/OT/ Therapists SW (OT/Physio) ISW B5 B5 B4 1 1 1 1 1 1 0 1 1 1 0 1 1 1 1 1 1 1 1 1 1 1 1 1 0 1 0.5 1 1 1 0 1 MH ISW B4 5 4 6 3 4 5 5 4 4 5 3 4 2 3 ISW B3 MH ISW B3 5 1 4 1 6 4 1 5 6 3 6 4 1 4 1 5 3 4 1 2 3 2 2 2 2 0 1 3 0.6 0.6 0 ISW B2 10 8 11 6 8 10 10 7 9 10 6 8 4 6 5 5 Mental Health Integrated Care Team workforce Band 8d 8b 8a 8a 7 7 6 6 6 6 5 5 4 3 3 Role Mental Health Therapist MH Therapist MH Nurse MH Therapist MH Therapists OT MH Lead MH Therapists Young people with dementia nurse Lead for dementia carers support service Memory assessment worker Memory assessment worker Psychological Wellbeing Practitioner (PWP) Social care young people with demntia resource worker Social Care funded support worker PWP Therapy assistant Huntingdon Ely and Fens ICT ICT ICT ICT ICT ICT ICT ICT ICT ICT ICT ICT ICT ICT ICT Borderline and Peterborough Greater Cambridge 1 1 0.5 1 1.5 1 0.5 1 1.5 1 0.5 1 3 1 0.5 1 2 1 1 1 1 1 2 2 2 1 2 1 2 1 2 1 1 1 1 1 2 1 1 1 2 2 1 2 1