Preventing the development of donor specific antibodies in kidney
advertisement

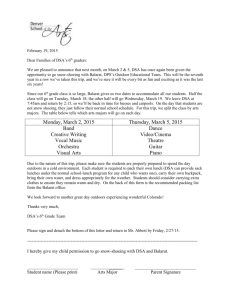
O35 PREVENTING THE DEVELOPMENT OF DONOR SPECIFIC ANTIBODIES IN KIDNEY TRANSPLANT RECIPIENTS THROUGH OPTIMAL IMMUNOSUPPRESSION – A RETROSPECTIVE ANALYSIS OF A SINGLE CENTRE TRANSPLANT UNIT Hughes, S1,2, Worthington, J 1, Strickland-Hodge, B 2, DeFrietas, D 1 ¹CMFT, Manchester, ²School of Healthcare, Leeds University INTRODUCTION: Life-long potent immunosuppression is prescribed following transplantation to prevent host detection of the allograft with ensuing rejection and subsequent failure of the organ. Detection of newly formed (de novo) donor specific antibodies (DSA) in the serum of transplant recipients indicates host immunity directed towards the allograft and has been shown to be responsible for late allograft failure. De novo DSA have been associated with underimmunosuppression, particularly in non-adherent patients. This study aimed to demonstrate that sub-optimal immunosuppression post-transplant was associated with the development of de novo DSA. METHODS: This retrospective case-control study compared immunosuppression regimes in de novo DSA positive patients, in a regional transplant centre (n=45), with DSA negative recipients with similar allograft dysfunction. All patients were tested for DSA due to unexplained graft dysfunction, defined as proteinurea or raised serum creatinine. The total immunosuppression prescribed in the 12 months prior to testing was measured as well as documented by clinician of patient non-adherence. Baseline factors between the two groups, including time from transplant, age, induction therapy, acute rejection and HLA mismatch, showed no significant difference. Sub-therapeutic dosing was defined as consecutive tacrolimus levels less than 4.5ng/ml, consecutive ciclosporin less than 50ng/ml, mycophenolate less than 50% of recommended dose or azathioprine less than 1mg/kg/day. All prednisolone doses were recorded for each patient. RESULTS: Patients with de novo DSA were shown to be exposed to a significantly lower immunosuppression burden in the 12 months prior to testing (p=0.0022). This was most notable with CNI treatment, where sub-therapeutic serum CNI levels were associated with de novo DSA detection (p=0.0011; RR 2.27 95% CI 1.3-3.97). A trend towards lower mycophenolate use was seen in DSA positive group but this was not significant. Steroids did not appear to affect de novo DSA development in this study. De novo DSA development severely affected allograft survival, with 14/49 and 1/48 graft failures in the DSA positive and negative group respectively. The median allograft survival post-DSA testing was of 36 months. The addition or increasing of immunosuppression post-DSA detection by clinicians was shown to have no effect on allograft survival however a larger study is required to confirm this. CONCLUSION: This single centre analysis demonstrates that sub-optimal immunosuppression is associated with the detection of de novo DSA in a kidney transplant population. Low levels of CNI through sub-optimal dosing or non-adherence was associated with the development of de novo DSA in this single centre study. Mycophenolate failed to show a significant association with de novo DSA development, probably due to the low use in the population study and due to the difficulty detecting non-adherence of mycophenolate (mycophenolate therapeutic drug monitoring is not performed at the local centre). Drug minimisation and patient nonadherence of maintenance immunosuppression should be reviewed in each transplant recipient to prevent de novo DSA development and subsequent allograft dysfunction.