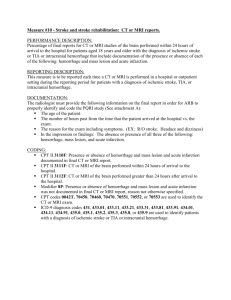
Imaging-Considerations-Intracranial
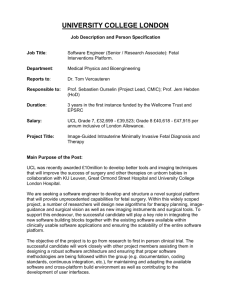
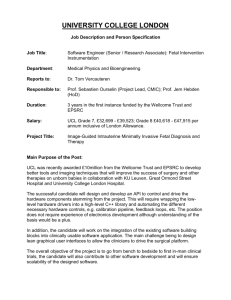
advertisement
Imaging Considerations The ultrasound images of intracranial bleeding are variable and depend upon location and time. [1] Parenchymal lesions demonstrate an irregular echogenic mass while epidural lesions tend to be cystic. [1] In either case, the application of color flow Doppler should indicate no flow within the mass. Other ultrasound findings in intracranial hemorrhage include: irregular echogenic brain mass, intraventricular echogenic foci or periventricular echodensities; ventriculomegaly; and posthemorrhagic hydrocephalus (PHH). [6] With massive intra-parenchymal hemorrhage, hyperechoic lesions in the lateral ventricle are seen and hydrocephalus is common. [2] Look for signs of fetal anemia and hydrops since this finding is present when there is a significant bleed. In those cases, peak systolic velocity of the middle cerebral artery may be useful in confirming anemia. MRI may be more accurate in diagnosis and is able to define the grade of the lesion better than ultrasound. [1] An increase in signal activity is noted with MRI T1-weighted images. A change from low to high intensity was noted with T2 weighted MRI signals after 4 weeks. [3] MRI can be used for imaging and dating fetal intracranial hemorrhage. Variable ultrasound and MRI findings are associated with this complication, depending upon the age and location of the hemorrhage.[3] About 1% of fetuses will demonstrate echogenic material within the frontal horns and while this finding may resolve, there is some association with ventriculomegaly and porencephaly. [4] Finally, in fetuses at risk for placental insufficiency the finding of intraventricular echodensities may predict poor outcome if the findings persist during the neonatal period. [5] 1. Ultrasound Obstet Gynecol. 2001 Oct;18(4):335-42. Fetal intracranial hemorrhage: is minor maternal trauma a possible pathogenetic factor? Strigini FA, Cioni G, Canapicchi R, Nardini V, Capriello P, Carmignani A. Source Division of Obstetrics and Gynecology, University of Pisa, Italy. f.strigini@obgyn.med.unipi.it Abstract OBJECTIVE: The occurrence of fetal intracranial hemorrhage before labor has been repeatedly observed. The aim of this study was to evaluate the sonographic appearance of fetal intracranial hemorrhage in relation to its location. Possible causative factors were also evaluated. DESIGN: Five consecutive cases of fetal intracranial hemorrhage were identified at a single ultrasound unit between 1996 and 1999. In uteromagnetic resonance imaging was also performed in four of these cases. Autopsy was performed after pregnancy termination or intrauterine fetal death (one case of each), and neurological follow-up was initiated in the three surviving infants. RESULTS: Hydrocephaly was the predominant sonographic finding associated with intraventricular or subependymal hemorrhage; sonography provided the correct diagnosis in the former (two cases), whereas magnetic resonance imaging was necessary in the latter. Massive intraparenchymal hemorrhage was depicted as an irregular echoic mass, whereas extradural hemorrhage had a cystic appearance. History of minor maternal physical trauma without maternal or placental injury was elicited in all cases. Ultrasound examinations performed before or shortly after the trauma were available in all cases and showed normal fetal anatomy. CONCLUSIONS: The sonographic appearance of fetal intracranial hemorrhage is variable, depending on its location. Even though sonography detected an intracranial anomaly in all cases, magnetic resonance imaging was necessary to establish the hemorrhagic nature of isolated subependymal and extradural hemorrhage. The similarity of histories involving minor maternal physical trauma in all cases, together with the absence of any known factor predisposing to fetal hemorrhage, may suggest that trauma is at least a contributing factor to the pathogenesis of fetal intracranial hemorrhage. Free Article PMID: 11778992 [PubMed - indexed for MEDLINE] 2. Taiwan J Obstet Gynecol. 2006 Jun;45(2):135-41. Fetal intracranial hemorrhage (fetal stroke): report of four antenatally diagnosed cases and review of the literature. Huang YF, Chen WC, Tseng JJ, Ho ES, Chou MM. Source Department of Obstetrics and Gynecology, Taichung Veterans General Hospital, Taichung, Taiwan. Abstract OBJECTIVE: Neonatal intracranial hemorrhage (ICH) has been estimated to be high in premature infants, occurring in approximately 40% of infants of less than 32 weeks' gestation. However, the true incidence of ICH in utero has not been determined. We present our experience with four cases of fetal ICH (fetal stroke), which was detected prenatally by ultrasonography (US). MATERIALS AND METHODS: Four cases of fetal ICH were identified over a 2-year period at the prenatal unit of Taichung Veterans General Hospital, Taiwan. Prenatal and neonatal sonograms, computed tomography (CT) scan or magnetic resonance imaging (MRI), medical records, and the clinical course were assessed retrospectively. In each case, a series of initial and follow-up obstetric sonograms were available. Fetal stroke was recognized by several sonographic features: irregular echogenic brain mass, intraventricular echogenic foci or periventricular echodensities; ventriculomegaly; and posthemorrhagic hydrocephalus (PHH). A detailed investigation for possible etiology of fetal ICH was performed in all cases. RESULTS: Transabdominal US showed hyperechoic lesions in the lateral ventricle and ventriculomegaly in three of the four fetuses, and a massive intraparenchymal hemorrhage in the remaining one. Three fetuses were born vaginally and one by cesarean section due to an enlarged head circumference. Abnormal nonstress tests and abnormal flow velocity waveforms in the umbilical and middle cerebral arteries were present in two cases. Intrapartum fetal death and neonatal death occurred in the first two cases associated with maternal preeclampsia at 31 and 27 weeks, respectively. In the remaining two infants, the one in case 3 underwent ventriculoperitoneal shunting, which developed normally at the age of 18 months. The other infant in case 4 had PHH after suspicious choroids plexus hemorrhage, and the detailed information regarding the cause of neonatal death was not available. CONCLUSION: This small series demonstrate that an antenatal diagnosis of fetal stroke with intraventricular hemorrhage Grades III and IV or with brain parenchymal involvement appears to be associated with poor neurologic outcome. Due to the significant neonatal neurologic impairment and potential medicolegal implications of antepartum fetal ICH, it follows that obstetricians and sonographers should be familiar with predisposing factors and typical diagnostic imaging findings of rare in utero ICH events. PMID: 17197354 3.J Reprod Med. 1997 Aug;42(8):467-72. Fetal intracranial hemorrhage. Imaging by ultrasound and magnetic resonance imaging. Kirkinen P, Partanen K, Ryynänen M, Ordén MR. Source Department of Obstetrics and Gynecology, University of Kuopio, Finland. Abstract OBJECTIVE: To describe the magnetic resonance imaging (MRI) findings associated with fetal intracranial hemorrhage and to compare them with ultrasound findings. STUDY DESIGN: In four pregnancies complicated by fetal intracranial hemorrhage, fetal imaging was carried out using T2-weighted fast spin echo sequences and T1-weighted fast low angle shot imaging sequences and by transabdominal ultrasonography. RESULTS: An antepartum diagnosis of hemorrhage was made by ultrasound in one case and by MRI in two. Retrospectively, the hemorrhagic area could be identified from the MRI images in an additional two cases and from the ultrasound images in one case. In the cases of intraventricular hemorrhage, the MRI signal intensity in the T1-weighted images was increased in the hemorrhagic area as compared to the contralateral ventricle and brain parenchyma. In a case with subdural hemorrhage, T2-weighted MRI signals from the hemorrhagic area changed from low-to high-intensity signals during four weeks of follow-up. Better imaging of the intracranial anatomy was possible by MRI than by transabdominal ultrasonography. CONCLUSION: PMID: 9284007 4.J Ultrasound Med. 2009 Dec;28(12):1629-37. What is the clinical importance of echogenic material in the fetal frontal horns? Hines N, Mehta T, Romero J, Levine D. Source Department of Radiology, Beth Israel Deaconess Medical Center, Boston, MA 02215, USA. Abstract OBJECTIVE: The purpose of this study was to evaluate the importance of echogenic material in the fetal frontal horns. METHODS: This was a Health Insurance Portability and Accountability Act-compliant, Institutional Review Boardapproved retrospective study. In part 1 of the study, prenatal sonography, prenatal magnetic resonance imaging (MRI), and birth outcomes of 17 fetuses (mean gestational age, 19 weeks; range, 15-34 weeks) with prospective echogenic material in the frontal horns were assessed. In part 2, 400 consecutive sonographic fetal surveys (mean gestational age, 19 weeks; range, 15-38 weeks) were reviewed to determine the incidence. In part 3, 2 independent reviewers assessed the appearance of the frontal horns in 40 fetuses (20 with suspected intraventricular hemorrhage from parts 1 and 2 and 20 who were interpreted to have normal findings in part 2). RESULTS: Part 1 of the study showed that suspected hemorrhage was unilateral in 13 fetuses and bilateral in 4. Additional findings by sonography were grade 4 intraventricular hemorrhage (n = 2), ventriculomegaly (n = 2), and porencephaly (n = 1). An additional finding by MRI was porencephaly in 1 fetus. In part 2, echogenic material in the frontal horns was identified in 3 of 400 fetuses (0.8%). In part 3, hemorrhage was probably or definitely present in 11 of the 20 fetuses with abnormalities; material looked like a cyst in 6; and normal choroid was in an abnormal position in 2 and a normal position 1. Of 19 fetuses with abnormalities, 14 had a posteriorly symmetric choroid; 9 had material of different echogenicity compared with the choroid; and 17 had an expanded frontal horn. Birth outcomes were abnormal in 7, including platelet abnormalities (n = 2), hemorrhage on imaging or pathologic examination (n = 2), extraventricular hemorrhage (n = 3), and ventriculomegaly (n = 3). CONCLUSIONS: The incidence of echogenic material in the frontal horns is less than 1%. This does not represent the normal location of the choroid plexus and may represent hemorrhage, which may resolve without sequelae or result in ventriculomegaly and porencephaly. PMID: 19933475 5. Ultrasound Obstet Gynecol. 2005 Sep;26(3):233-43. 7Ultrasound Obstet Gynecol. 2003 Aug;22(2):110-20. Peri- and intraventricular cerebral sonography in second- and third-trimester high-risk fetuses: a comparison with neonatal ultrasound and relation to neurological development. van Gelder-Hasker MR, van Wezel-Meijler G, de Groot L, van Geijn HP, de Vries JI. Source Department of Obstetrics and Gynecology, VU University Medical Centre, Amsterdam, The Netherlands. Marja.Hasker@vumc.nl Abstract OBJECTIVES: To determine whether periventricular leukomalacia (PVL) and peri- and intraventricular hemorrhages can be detected in fetuses at risk for preterm birth and to establish the clinical significance of this finding. METHODS: Prenatal cerebral sonography was performed in 26 fetuses at risk for uteroplacental insufficiency on the day of inclusion into the study and weekly until delivery. Neonatal cerebral ultrasound examination was performed within 24 h of birth and biweekly until discharge. The infants underwent standardized neurological examinations. RESULTS: During 30 observations, 21/26 fetuses presented in a cephalic position. Successful visualization in the coronal and sagittal planes was significantly correlated with that of a control population (r = 0.615; 95% CI, 0.390-0.771). In 20/21 fetuses at least one observation was adequate for analysis. Eleven cerebral abnormalities were found in nine fetuses, periventricular echodensities in four, intraventricular hemorrhage in two, and localized thalamic densities in five. In six of these infants ultrasound abnormalities persisted after birth. Neurological follow-up at 24 months demonstrated abnormalities in three infants, two infants were normal and one was lost to follow-up. The three infants with normal ultrasound results after birth had a normal follow-up. Five infants with normal antenatal ultrasound results showed ultrasound abnormalities during the neonatal period; four of them developed PVL Grade 1 and one developed PVL Grade 2. The follow-up of two of these infants was normal, two died and one developed spastic tetraplegia. Abnormal antenatal brain sonography was significantly correlated with gestational age at birth (r = 0.487; P = 0.029). CONCLUSION: Peri- and intraventricular echodensities can be detected reliably before birth in fetuses at high risk for uteroplacental insufficiency. When abnormalities persist, there is a high risk for an adverse outcome. Copyright 2003 ISUOG. Published by John Wiley & Sons, Ltd. PMID: 12905502 Free full text