Annual Report 2013/14 - University Hospitals Bristol NHS
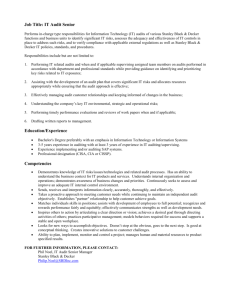
advertisement
Clinical Audit Annual Report 2013/14 Report by: Stuart Metcalfe, Clinical Audit & Effectiveness Manager. Date: June 2014. Introduction from the Chair of Clinical Audit Group ............................................................................ 3 1. Report from the Clinical Audit & Effectiveness Manager ................................................................. 4 1.1 Clinical Audit & Effectiveness Team ................................................................................................................................ 4 1.2 Clinical Audit Group ........................................................................................................................................................ 4 1.3 Forward Planning ........................................................................................................................................................... 4 1.4 Annual Quality Report .................................................................................................................................................... 5 1.5 National and Regional Involvement ............................................................................................................................... 5 2. Programme Key Performance Indicators ......................................................................................... 6 2.1 Introduction and explanation of statistics ...................................................................................................................... 6 2.2 Summary ‘dashboard’ of Key Performance Indicators ................................................................................................... 7 2.3 Comment on Key Performance Indicators ...................................................................................................................... 8 3. Divisional summaries and tables ..................................................................................................... 9 3.1 DIAGNOSTICS & THERAPIES ............................................................................................................................................ 9 3.2 MEDICINE ...................................................................................................................................................................... 16 3.3 SPECIALISED SERVICES .................................................................................................................................................. 24 3.4 SURGERY, HEAD AND NECK .......................................................................................................................................... 29 3.5 WOMEN’S AND CHILDREN'S ......................................................................................................................................... 38 3.6 NON-DIVISION SPECIFIC ................................................................................................................................................ 49 Appendix A - UH Bristol Clinical Audit Staff (as at April 2014) ............................................................. 50 Appendix B - Clinical Effectiveness & Outcomes Strategy Action Plan ................................................. 51 Appendix C - Progress against Clinical Audit Forward Programme 2013/14 ........................................ 53 Appendix D - University Hospitals Bristol Clinical Audit Forward Programme 2014/15 ........................ 55 Appendix E - National audit participation (extract from Quality Report 2013/14) ............................... 70 Clinical Audit Annual Report 2013/14 Page 2 Introduction from the Chair of Clinical Audit Group Clinical Audit is an essential tool to assess and improve the standards of care that we deliver. Used skilfully it brings together professionals from many disciplines to improve the quality of clinical services. Over the last year we have been challenged to assure both the Board and the Non- Executive Directors that the Trust’s clinical audit program is meeting the needs of UH Bristol. In response to this we have reviewed our processes, tried to ensure that our activity aligns to corporate and board objectives and that there is greater ownership and visibility of audit within the Divisions. I would like to thank Start Metcalfe for the extraordinary amount of work he has done to provide Divisions with the information they require to support and develop their audit activity. This year’s report again shows a clinical audit programme with a balance of projects initiated in response to guidance issued by the National Institute for Health and Care Excellence (NICE), the National Patient Safety Agency (NPSA), the Medical Royal Colleges, and projects initiated in response to local priorities. Scrutiny of outcomes and action reports at each meeting of the Clinical Audit Group has continued this year. We hope that this adds value to the projects and helps facilitates the implementation of actions where appropriate. I would like to thank the Clinical Audit & Effectiveness Team for all their work in producing these reports and for their dedication to the successful running of the clinical audit programme. You will see many examples in this annual report of positive outcomes of clinical audit projects and we will continue to build on this in the future. I would also like to thank all the Clinical Audit Convenors for their role in leading the clinical audit programme within their Divisions and specialties and for their involvement in the work of the Clinical Audit Group on behalf of the Trust. Finally we are embarking on a survey to understand better how clinical audit functions in comparable trusts. This is a significant undertaking, but one we hope will be invaluable in informing how we should take our service forward. The results of this should be available later in the year and will be reported to Clinical Audit Group and the Trust Audit Committee. Anne Frampton Chair, Clinical Audit Group Clinical Audit Annual Report 2013/14 Page 3 1. Report from the Clinical Audit & Effectiveness Manager 1.1 Clinical Audit & Effectiveness Team During the financial year 2013/14, clinical audit at University Hospitals Bristol NHS Foundation Trust was supported by a team of 3.8 whole time equivalent (WTE) Clinical Audit Facilitators (CAFs) and one 0.8 WTE Clinical Audit Clerk, employed by the Trust Services Division. Additional support is provided by a number of other staff employed by the Clinical Divisions with a specific remit for clinical audit; primarily data management for individual national clinical audit projects. The Clinical Audit & Effectiveness Team (CAET) also includes a designated NICE Manager with a remit for coordinating assurance information relating to the implementation of NICE guidance in all its forms. Full details of the team and the Divisions/specialties they support can be found at Appendix A of this report. In March 2013, the CAET completed the final phase of a ‘lean’ exercise as part of the Trust’s Transformation Programme; the centralisation of the Team, physically located within Trust Headquarters. Having previously been located within clinical areas, this was a major change for the service and for the CAFs. I would like to thank the team for their part in embracing this change with vigour and enthusiasm. Outside the process of centralisation, a number of other workstreams were agreed as part of this lean exercise. These workstreams, along with other actions relating to the function of clinical audit, were incorporated into an overall Clinical Effectiveness and Outcomes Strategy agreed in May 2013. The progress of actions relating to clinical audit has been monitored by the CAG and the position at the end of the year can be found at Appendix B. 1.2 Clinical Audit Group The Clinical Audit Group (CAG) is the Trust’s lead group in relation to all matters relating to the practice of clinical audit, supporting both the ‘Clinical Effectiveness’ and ‘Patient Safety’ dimensions of the NHS model of Quality. The Group met five times during the financial year 2013/14 to enable discussion of core business, i.e. annual forward plans, quarterly key performance indicators and project progress reports on registered activity. At each meeting, the CAG reviews summary outcomes and actions reports from completed clinical audit projects to ensure that results are clear and that robust action plans have been produced. Where this is not the case, the CAG will seek further clarity from the project lead or from within the CAET before accepting the project as complete. There are also instances where the Group determines that the outcomes would be relevant to the work of other corporate governance/risk groups or other areas of the Trust. In this case, the Group will recommend wider dissemination of the results as necessary. The CAG reports into the Trust Clinical Quality Group on a quarterly basis, highlighting any relevant risk issues. 1.3 Forward Planning Each year, Clinical Divisions/specialties agree a programme of planned clinical audit activity for the forthcoming financial year. This process is co-ordinated by the CAET and overseen by the CAG. Each year’s plan reflects agreed priority projects, based on considerations such as anticipated Trust/Divisional quality objectives, National Clinical Audits, Commissioning priorities, national guidance (NICE, Patient Safety Alerts, Royal College) and local clinical priorities. Progress against this plan is closely monitored by the CAET and CAG (as is all registered activity) and reported to the CAG and the Trust Audit Committee. Overall progress against this plan can be found at Appendix C, with further Divisional/specialty detail found within Section 3 of this report. The past year of reporting to our the Audit Committee has prompted a number of challenges about how best to use the information that we report and how best to provide the necessary assurances the committee require. The team has worked hard over the year to try and meet these requirements, developing new Clinical Audit Annual Report 2013/14 Page 4 reporting processes as the year has gone on. Standard reporting into Divisions/specialties is in the process of being implemented to allow more visibility of activity and better help the Team highlight/manage exceptions where the progress of projects is not as expected. The process has also highlighted further opportunities to improve our Clinical Audit Project Management database. This work will continue throughout the next financial year. The annual clinical audit forward plan for 2014/15 has been put together after wide consultation with clinical/nursing staff and Divisional Quality/Safety Groups. To improve compliance with the plan, progress will be monitored not only by the Clinical Audit Group but through regular reports into these Quality/Safety Groups. Projects have been prioritised based on priority areas for clinical audit as outlined within the Healthcare Quality Improvement Partnerships (HQIP) ‘Clinical Audit Programme Guidance’. The full plan can be found at Appendix D 1.4 Annual Quality Report A mandated statement about participation in national clinical audits has been included in the Trust’s Quality Report for 2013/14. The relevant extract has been reproduced at Appendix D of this report. As outlined within this statement, the Trust has a duty to provide information on the actions taken and improvement made as a result of clinical audit activity. This information can be found within the changes and benefits section of Divisional reports (Section 3 of this report) 1.5 National and Regional Involvement The Clinical Audit & Effectiveness Manager is the current Chair of the South West Audit Network (SWANS); a regional forum bringing clinical audit professionals together to share best practice through presentations, discussion and networking. This work is supported by the Healthcare Quality Improvement Partnership (HQIP). The Chair of SWANS also represents the network on the National Quality Improvement & Clinical Audit Network (NQICAN – previously the National Audit Governance Group), a national peer group consisting of representatives from regional clinical audit networks/forums, including representation from the Department of Health and Royal Colleges. NQICAN works closely with the Department of Health, HQIP, NICE and other relevant national bodies to further the development of clinical audit within the NHS. Stuart Metcalfe, Clinical Audit & Effectiveness Manager Clinical Audit Annual Report 2013/14 Page 5 2. Programme Key Performance Indicators 2.1 Introduction and explanation of statistics All project information for this report is taken from the UH Bristol Clinical Audit Project Management Database. The statistics presented are based on registered activity during the financial year 2013/14. This includes projects started in previous years and not yet complete as well as projects newly registered in 2013/14. The definition of terms used as KPIs is outlined below: Project registered before start Ongoing monitoring (continuous) audit Re-audit NICE guidance National Interface Proposal form completed and approved before commencing a project. The continuous collection of data in order to measure practice. Ongoing audit should involve regular review of data and implementation of changes in practice (where necessary) in order to improve performance. The repetition of an audit project in order to measure whether practice has improved since the initial audit. Audits relating to standards/recommendations from the National Institute of Health and Care Excellence. Denotes national audits, e.g. those audits part of the National Clinical Audit & Patient Outcome Programme (NCAPOP), audits required for the annual Quality Report and other Royal College/other professional bodies’ national audits. Audit of care across organisational boundaries in the patient pathway, e.g. patient referrals in from primary care to UH Bristol. Multi-specialty Involving a specialty/specialties other than the specialty under which the project has been registered. Multi-professional Involving more than one profession (e.g. nurses and doctors). Projects with patient Involvement Patients/carers involved in one or more of the following: identification of audit topic; developing audit idea/project design; carrying out audit project; receiving audit results. Clinical Audit Annual Report 2013/14 Page 6 2.2 Summary ‘dashboard’ of Key Performance Indicators Project registered before start On-going (continuous) monitoring Re-audits Abandoned Deferred NICE guidance Projects with patient involvement National Interface Multi-specialty Multi-professional Completed projects Action Plan produced Confirmed good/acceptable practice # Report produced 41 93% 4% 25% 2 0 4% 3% 7% 0% 25% 41% 37 86% 14% 97% Medicine 91 57 72% 3% 15% 2 0 25% 3% 14% 0% 16% 33% 46 96% 4% 93% Non-division specific 3 0 0% 33% 0% 1 0 0% 0% 0% 0% 67% 33% 2 100% 0% 50% Specialised Services 47 22 77% 13% 21% 6 0 28% 2% 13% 0% 19% 23% 14 86% 14% 71% Surgery, Head and Neck 118 62 82% 10% 31% 13 5 8% 8% 12% 3% 22% 25% 42 76% 24% 71% Women and Children's 173 72 79% 23% 29% 16 1 15% 3% 6% 0% 21% 49% 77 96% 3% 70% TOTAL (2013/14) 507 254 80% 13% 26% 40 6 15% 4% 10% 1% 21% 37% 218 90% 9% 80% TOTAL (2012/13) 513 N/A N/A 13% 26% 58 15 16% 5% 10% 1% 28% 46% 194 90% 10% 78% New in year 75 Total number of projects * Diagnostic and Therapy * In progress (including ongoing monitoring audits) or completed during the year, this includes projects started in previous years and not yet complete. All percentages are based on this total, apart from those in the last four columns which are based only on clinical audits completed during the year. # please note: this statistic applies only to projects where an action plan was not produced, i.e. there will also have been a number of projects which produced an action plan, but where practice was nevertheless identified as being of an acceptable standard Clinical Audit Annual Report 2013/14 Page 7 2.3 Comment on Key Performance Indicators As one can see from the above table, the results of many of the indicators remain similar to the previous year, as does the level of overall activity. It is encouraging that the number of abandoned and deferred projects decreased since the previous report despite the changes in remits of the CA&ET. Of notable acceptation to this overall trend in 2013/14, is the percentage of projects with multi-specialty and multi-disciplinary input. Although not reported here, performance has remained fairly constant over the last three years at around 27% and 45% respectively. There is no obvious reason for this decrease and further investigation will be undertaken to try and determine why this is the case. Although the number of new projects started/registered is monitored as part of bi-monthly CAG reporting, this is the first time that the overall figures have been included in the annual report. Hence there is no comparative figure shown. Also included this year but not previously, is an indicator outlining the proportion of activity registered before starting. Given the change in the work and areas covered by the team as a result of centralisation, it is encouraging to see that the majority of projects have been discussed and registered appropriately before starting. Where possible, CAFs will do their best to obtain a formal report at the end of each individual project but this is not always possible for a number of reasons. What is of vital importance however, is obtaining information on the outcomes of the work undertaken and the actions necessary to improve practice where the need is identified. To this end, the fact that the Trust can demonstrate that an action plan was produced in all but 1% of projects completed is a good achievement. Clinical Audit Annual Report 2013/14 Page 8 3. Divisional summaries and tables The following section aims to provides further details of Divisional clinical audit , including relevant key performance indicators. 3.1 DIAGNOSTICS & THERAPIES The following chart shows the status at year end of those projects identified as priorities for audit as part of the forward planning process in 2013/14. Full details of the status of individual projects on this plan can be found within table 1 of this section. Progress of planned projects Complete In progress Not started 100% 80% 60% 40% 20% 0% 1 2 3 4 2 3 Diagnostic Services 4 Therapy Services Prioritisation category The chart below shows the status at year end of all registered projects (excluding those classified as ongoing monitoring). Some projects will have started and finished within the financial year, some will have been started but have yet to complete and are therefore rolled over. The figures also include projects that commenced in previous years but have now been abandoned, those that previously commenced but were completed in 2013/14 and those previously commenced but not completed by the end of 2013/14. Individual project status at year end 20 18 16 15 13 10 10 8 4 5 2 1 2 0 0 Diagnostic Services New in year/Completed Clinical Audit Annual Report 2013/14 New in Year/Roll-over Therapy Services Rolled-over/Abandoned Rolled-over/Completed Rolled-over/Roll-over Page 9 Percentage of projects egistered before start 100% Make up of project project team 1 5 100% 80% 80% 60% 60% 24 40% 40% 10 20% 20% 46 23 0% 17 14 Diagnostic Services Therapy Services 0% Diagnostic Services TRUE Therapy Services FALSE Multi-professional Percentage National Audit 100% 80% 80% 60% 60% 40% 40% 0% Multi-specialty Neither Percentage re-audit 100% 20% 8 2 17 39 20% 46 5 24 Diagnostic Services Therapy Services 12 7 Diagnostic Services Therapy Services 0% TRUE FALSE TRUE FALSE Guidance/standards type audited 35 31 30 25 20 15 12 11 9 10 9 5 2 1 0 Diagnostic Services Therapy Services NICE Other National Local Percentage report produced 100% Unclassified Percentage action plan produced 1 100% 5 80% 80% 60% 60% 40% 40% 20% 20% 30 6 0% 26 6 Diagnostic Services Therapy Services 0% Diagnostic Services TRUE Clinical Audit Annual Report 2013/14 Therapy Services FALSE Yes No - Confirmed good practice Page 10 Table 1 Title Sub-Specialty Lead Priority Start date Status Q4 Audit of the management of patients with haemoglobinopathies Laboratory Haematology Tom Latham (Blood and Transplant audit programme) 1 Q3 Not started Audit of patient information and consent (Blood and Transplant Laboratory Haematology Tom Latham audit programme) 1 Q4 Not started Compliance with transfusion procedures Laboratory Haematology Tom Latham 2 Q1 In progress Transfusion information availability Laboratory Haematology Tom Latham 2 Q1 Not started Audit of microbiology sampling in stillbirth post mortems Histopathology Craig Charles Platt 2 Q2 In progress Audit of double-reporting protocol in colorectal cancer biopsies Histopathology Golda ShelleyFraser 2 Q2 In progress Supplementary reports after MDT meetings Histopathology Rob Pitcher 2 Q2 Not started Audit of reporting of Cutaneous Malignant Melanoma at UHBristol Histopathology Nidhi Bhatt 2 Q2 In progress Diagnosis of malignancy in endometrial curettage and subsequent resection specimen Histopathology Joya Pawade 2 Q1 In progress Lung frozen section and paraffin diagnosis Histopathology Nidhi Bhatt 2 Q2 Completed Percentage of pre-treatment non-small cell carcinoma not otherwise specified (NSCLC-NOS) Histopathology Nidhi Bhatt 2 Q1 Completed Turnaround time for reporting of biopsies suspected Inflammatory Bowel Disease Histopathology Pramila Ramani 2 Q4 In progress Placenta request forms and macroscopic reporting Histopathology Corina Moldovan 2 Q3 In progress Prophylaxis in orthopaedic surgery Microbiology Martin Williams 4 Q3 Not started Diagnosis and Initial Management of Suspected Communityacquired Bacterial Meningitis in Adults Microbiology Ed Barton 4 Q2 In progress An audit of the use and management of blood glucose point of care testing results in UH Bristol Clinical Biochemistry Paul Thomas/ Graham Bayly 2 Q3 Not started CT radiation dose audit Medical Physics & Bioengineering Ian Negus 2 Q1 Completed Nutritional screening of upper gastro-intestinal surgical patients Nutrition & Dietetics in pre-op clinic Tom Lander/Clare Evans 3 Q2 Not started Nutritional Screening Nutrition & Dietetics Rachel Cooke 2 Q1 In progress Parenteral Nutrition within Critical Care Nutrition & Dietetics Rebecca Pooley 3 Q2 In progress Documentation Audit Physiotherapy/ Occupational Therapy Linda Clarke/Scott Allan 2 Q4 Not started South West Quality and Patient Safety Improvement Programme Pharmacy (Medicines Management) Kevin Gibbs 2 Q1 In progress Re-audit compliance with prescribing policy Medicines Codes Chapter M2 Pharmacy Anne Edwards 2 Q2 Completed Audit of the prescribing and monitoring of sliding scale heparin infusions Pharmacy Jacqueline Criper 2 Q3 In progress Vancomycin prescribing audit Pharmacy Elizabeth Jonas 2 Q2 Not started Audit of adherence to the pharmacy prescription endorsing policy Pharmacy Elin Wallis 2 Q1 Completed Audit of medicines reconciliation on transfer between adult intensive care unit (ICU) and post-ICU wards. Pharmacy John Warburton 3 Q2 In progress Re-audit of insulin prescribing to agreed prescribing bundle Pharmacy Kevin Gibbs 3 Q4 Not started Audit of medicines reconciliation on discharge Pharmacy Emily Marshall 2 Q2 In progress Clinical Audit Annual Report 2013/14 Page 11 Audit of consultant names on in-patient prescription charts and Pharmacy out-patient prescription forms Kevin Gibbs 2 Q1 In progress Home visit for cystic fibrosis patients on home intravenous antibiotics Physiotherapy Jo Bond-Kendall 4 Q1 In progress Re-audit Glasgow Hearing Aid Benefit Profile Audiology Regina Smith 3 Q1 Completed Standards for and outcomes of videofluoroscopy referral Speech and Language Therapy Vicki Weekes 3 Q2 Not started Radiological interpretation recording in notes Radiology Sally King 3 Q2 In progress Appropriateness of radiographic markers Radiology Simon Brown 3 Q3 In progress Vascular interventional radiology outcome data Radiology Amit Goyal 3 Q1 Completed The following activity was also in progress during the financial year (either rolled over from previous year or not identified through plan): Ref Provisional Title of Project Status Diagnostic Services - Audiology (Adult) 3347 Re-audit of Real Ear Measurements 2012 Completed 3472 The completion of Glasgow Hearing Aid Benefit Profile in 2012 Completed Diagnostic Services - Laboratory Medicine/Histopathology 3138 Adherence to double reporting protocol in reporting lung pathology Completed 3216 Quality of perinatal autopsy in the South-West of England Completed 3325 Turnaround time for reporting of biopsies of suspected Inflammatory Bowel Disease Completed 3435 Regional audit of percentage of pre-treatment non-small cell carcinoma not otherwise specified (NSCLC-NOS) Completed 3436 Audit of placenta request forms and macroscopic reporting In Progress 3534 Diagnosis of malignancy in endometrial curettage and resection specimen In Progress 3596 HER2 testing for gastric cancer Completed 3608 Re-auditing the reporting of Cutaneous Malignant Melanoma at UH Bristol In Progress 3609 Microbiology sampling in stillbirth post mortems – Re-audit 2012 Completed 3627 Audit of frozen section practice in thoracic pathology In Progress 3688 Re-audit turnaround time for reporting of biopsies of suspected Inflammatory Bowel Disease In Progress 3689 Receptor Status in invasive breast cancer reported in UH Bristol in relation to national guidelines In Progress 3707 Turnaround time in reporting of skin specimens 2012-2013 In Progress Diagnostic Services - Laboratory Medicine/Infection Control 733 Infection Control Ward/Department audit Ongoing Project 992 Are all Trust employees complying with the Infection Control Hand Hygiene Policy? Ongoing Project 3013 Infection Control Environment and Equipment Audit 2011-2012 Ongoing Project 3495 Prospective audit of linen handling and management at ward level 2013 Completed 3540 Vascular Access Management in Intensive Care Completed 3606 Hand Hygiene Environment: a trust-wide audit of clinical and non-clinical areas In Progress 3633 Trust-wide Spot Check Sluice/Commode/Toilet Audit In Progress 3662 Documentation Audit of the recording of Peripheral Venous Cannula in adult ward areas trust wide In Progress 3709 Re-auditing management of discharge information for patients with an infection/colonisation In Progress Diagnostic Services - Laboratory Medicine/Laboratory Haematology 2912 Audit of medical patients with Hb>8g/dl receiving red cell transfusion Clinical Audit Annual Report 2013/14 Completed Page 12 3014 National Comparative Audit of the Medical Use of Blood Completed 3172 National comparative audit of the labelling of blood samples for transfusion - NHS Blood and Transplant Completed 3451 Audit of consent gained for transfusions as per SaBTO guidelines In Progress 3452 Use of red blood cell transfusion in haematology patients – a prospective audit Completed 3541 Re-audit of use of red blood cell transfusion in haematology patients – a prospective audit Completed Diagnostic Services - Laboratory Medicine/Microbiology 3308 Is the antimicrobial management of Hospital Acquired Pneumonia consistent with local antibiotic guidelines at UH Bristol? Completed 3326 Audit of clinical liaison for alert organism results in microbiology Completed 3433 Audit of the blood culture contamination rate at UH Bristol Completed 3434 Diagnosis and Initial Management of Suspected Community-acquired Bacterial Meningitis in Adults In Progress 3648 Laboratory diagnosis, sample processing and clinical management of invasive candidaemia In Progress Diagnostic Services - Medical Physics & Bioengineering 2832 The handover of radiology equipment 2010 - 2011 Abandoned 2911 National Computed Tomography Radiation Dose Audit Completed 3696 Computed Tomography Patient Radiation Dose Audit – Level 2, BRI Completed Therapy Services - Nutrition & Dietetics 3116 Nutrition paperwork audit: a trust wide audit of the key prompts of CQC outcome 5 Completed 3267 Audit of nasogastric feeding practice on Cardiac Intensive Care Unit In Progress 3274 Dietetic Record Card Audit 2012 Completed 3533 Nutrition: key prompts of CQC outcome 5. A bi-annual audit. In Progress 3637 Audit of Parenteral Nutrition within Critical Care In Progress Occupational Therapy 3290 Audit of the Early Supported Discharge Team for Stroke Professional Standards In Progress Therapy Services - Pharmacy 2975 Audit of discharge referrals received by the Postal Anticoagulant Monitoring Service In Progress 3027 Re-auditing missed doses for critical medication in medical and surgical divisions of UH Bristol Completed 3055 An Evaluation of Insulin Prescribing Safety in a Teaching Hospital Completed 3107 Intravenous to oral antibiotic switch – audit of practise within University Hospitals Bristol NHS Foundation Trust In Progress 3345 Audit on the use of the Potassium Supplementation Standing Order In Progress 3466 An audit of adherence to the continuous vancomycin infusion guideline for ITU Completed 3475 Reauditing compliance with prescribing policy – Medicines Codes Chapter M2 Completed 3483 Audit of the Pharmacy prescription endorsing procedure In Progress 3615 Audit of consultant name on prescription charts In Progress 3624 Audit of the prescribing and monitoring of intravenous unfractionated heparin infusions In Progress 3625 Blood test screening prior to commencement of significant cardiovascular drugs In Progress 3679 Audit of medicines reconciliation on transfer from adult ICU or HDU to post-ICU wards In Progress 3699 Audit of inpatient prescription chart In Progress 3706 Audit of Medicines Reconciliation at Discharge In Progress Therapy Services - Physiotherapy 3289 Are Anterior cruciate ligament reconstruction patients adhering to the UH Bristol rehabilitation protocol? In Progress 3384 Acute Stroke Therapy Service against NICE Stroke Quality Standard 5 In Progress 3656 Home intravenous antibiotic standards for the Cystic Fibrosis multidisciplinary team In Progress Clinical Audit Annual Report 2013/14 Page 13 Therapy Services - Radiology 2957 Audit of reporting standards of MRI of sacroiliac joints in arthritis Abandoned 3054 Minimising eye dose in paediatric CT head Completed 3062 Movement artefact in MRI scans for rectal cancer staging Completed 3156 A re-audit into the Cardiac Magnetic Resonance Imaging (MRI) Perfusion Service Completed 3238 Re-auditing non-anaesthetist conscious sedation during interventional radiology procedures Completed 3255 Abdominal ultrasound examinations performed and reported by Advanced Practitioner Sonographers with or without discussion with Consultant Radiologist Completed 3321 Audit of accuracy of CT staging of mesothelioma Completed 3327 Audit of radiation dose delivered for routine high resolution CT in adults Completed 3328 National Audit of Standards for the NPSA and RCR Safety Checklist for Radiological Interventions In Progress 3348 National Audit of Appropriate Imaging Completed 3437 Audit of GP neuroimaging requests Completed 3482 Vascular interventional radiology outcome data Completed 3686 Annual re‐audit of image guided lung biopsies Completed 3708 Quality of MRI lumbar spine examinations at University Hospitals Bristol In Progress 3725 Subarachnoid haemorrhage and the use of diagnostic lumbar puncture In Progress Therapy Services - Speech & Language Therapy 3401 Re-auditing management of adult dysphagia patients 2012 In Progress The following section summarises the changes, benefits or actions introduced as a result of completed audits within the Division/specialties. 3347 This audit demonstrated that the process of recording of real ear measurement was broadly in line with recommendations. Audiologists have been reminded that all information must be recorded on the database especially reasons for sounds not recorded. 3472 This audit demonstrated that the completion of Glasgow Hearing Aid Benefit Profile was properly completed. Staff have been further educated to always document specific reasons of not completing the Profile. 3138 This audit showed good adherence to the double reporting protocol in the reporting of lung pathology. 3216 Clinicians have been advised of the importance of including clinical information in consent form for perinatal autopsy and the value of examination of placenta together with the stillbirth baby in this regional audit. 3325 As a result of this audit, short codes for macroscopy and a short list of SNOMED codes for Inflammatory Bowel Disease were developed in order to improve turnaround time for reporting of biopsies of suspected IBD. 3435 This audit demonstrated that the Trust is meeting national standards relating to histological classification of lung cancers as non-small cell carcinoma not otherwise specified prior to treatment (< 20%). 3596 This audit determined that gastric cancer patients managed at UH Bristol received HER2 testing as recommended by best international practice. Cases referred to UH Bristol were reported in a timely manner. 3609 The improvement of routine heart blood swab and lung sampling taken from stillbirths for microbiology and virology was evident in this re-audit. The locally agreed guidelines (including collecting viral PCR samples from the lung) which are informed in part by national standards, are being followed. 3495 This audit demonstrated that the general principles/processes for linen handling are being followed on most wards. A poster has been developed to be displayed on the ward trolley/cupboard to show designated coloured bags to be used. 3540 This audit highlighted the importance of documenting central venous line insertions on the Innovian database and making use of standardised infusion line labels. Current dressing practice has also been reviewed to establish how lines can be secured more effectively. 2912 This audit led to the promotion/practice of single unit transfusion as established best practice by the Patient Blood Management Group. 3014 Local transfusion guidelines were updated as a result of this national audit of the medical use of red cells. Data monitoring based on laboratory records in order to provide continuous monitoring of improvement is being carried out. 3172 Junior doctors are now educated in the correct procedure of labelling of blood samples for transfusion via the Trust’s induction programme as a result of this audit. A process for rejecting any samples not labelled correctly has been Clinical Audit Annual Report 2013/14 Page 14 developed. 3452 The audit of red blood cell transfusion in haematology patients helped to promote single unit transfusions. 3541 As a result of this audit, the junior doctor induction programme has been modified to ensure communication of key recommendations within the Trust’s blood transfusion guidelines (especially red cell transfusion in haematology patients). A process for reinforcing these recommendations at the point of blood transfusion request has also been developed. 3308 The Hospital Acquired Pneumonia Management guidelines were revised as a result of this audit. Better patient MRSA screening is also being addressed by the Trust’s MRSA Recovery Plan. 3326 As a result of this audit, the laboratory guideline for the liaison of alert organism results was updated to reflect agreed changes in practice. 3433 The Trust’s blood culture policy is to be reviewed and modified (including closer links to Department of Health best practice guidelines. Regular feedback on blood culture contamination rates will be provided to the Emergency Department and Medical Assessment Unit. 2911 This audit demonstrated that doses from CT scans are within the range seen locally and nationally. Early indications are that UHBristol’s doses are in line with the rest of the country. 3696 This audit demonstrated that mean radiation doses for standard size patients in Computed Tomography is within required levels (less than both local and national diagnostic reference levels). 3116 A single audit tool for nutrition paperwork was created as a result of this audit. This will be completed across the Trust wide to cross check ward based results and monitor progress in compliance with the key prompts of CQC Standards. 3027 The Administration of Medicine Operating Procedure and UH Bristol Medicine Code Chapter M9 were amended as a result of this audit. The time frame for administration of critical medications and the management procedure of missed doses have been clarified. 3055 As a result of this audit, a specific subcutaneous insulin prescribing chart has been designed and implemented throughout the Trust. Guidance for all prescribers to cover the insulin prescribing bundle and the new insulin chart has also been written and disseminated. 3466 The vancomycin infusion template in ITU is to be modified to include “First level after 15hrs” and a drop down box of named prescribers has been added to Innovian system as a result of this audit. Vancomycin prescribing information will also be included in Innovian induction training. 3475 A visual aid to the Trust’s prescribing policy has been developed and is to be given out at junior doctor induction to help promote good prescribing practice. 3054 A single protocol for paediatric CT head scanning was agreed as a result of this audit into minimising eye dose in paediatric CT head scans. 3062 As a result of this audit, a cost and logistical analysis of the introduction of hyoscine butylbromide in patients undergoing MRI scans for staging of rectal cancer was carried out as part of a general review of standards and technique. 3156 This re-audit audit into the Cardiac Magnetic Resonance Imaging (MRI) Perfusion Service demonstrated acceptable practice. 3238 This re‐audit of non‐anaesthetist conscious sedation during interventional radiology procedures demonstrated that changes previously implemented had been effective and that procedures and process had improved. 3255 This audit has led to extra training for Advanced Practitioner Sonographers on abdominal ultrasound scanning and the use of reporting protocols. 3321/ 3327 Protocols for CT scanning of the chest in adults (including mesothelioma imaging) are being rewritten as a result of this audit. This will help maintain improve image quality, standardise technique aim for minimal dosage. 3348 This national audit run by the Royal College of Radiologists demonstrated that imaging at UH Bristol was appropriate. 3437 As a result of this audit into the management of headache in young people and adults, GP requests for CT head will be changed to MRI head as a way to reduce radiation dose for patients under 50 years old. 3482 The outcomes measured in this audit of vascular interventional radiology demonstrated acceptable practice. Further audits will be extended to include all interventional radiologists which will improve the study population size and increase complication accuracy. 3686 This annual re-audit of image guided lung biopsies demonstrated acceptable practice. CRIS codes have been condensed for interventional chest procedures. Clinical Audit Annual Report 2013/14 Page 15 3.2 MEDICINE The following chart shows the status at year end of those projects identified as priorities for audit as part of the forward planning process in 2013/14. Full details of the status of individual projects on this plan can be found within table 1 of this section. Progress of planned projects Complete 100% 80% 60% 40% 20% 0% 1 In progress Not started 1 1 1 2 5 3 13 3 2 2 2 3 2 1 1 1 5 2 3 1 Emergency Department Medical Specialties Prioritisation category The chart below shows the status at year end of all registered projects (excluding those classified as ongoing monitoring). Some projects will have started and finished within the financial year, some will have been started but have yet to complete and are therefore rolled over. The figures also include projects that commenced in previous years but have now been abandoned, those that previously commenced but were completed in 2013/14 and those previously commenced but not completed by the end of 2013/14. Individual project status at year end 25 22 20 20 20 15 10 10 3 5 3 6 4 1 1 0 Emergency Department (Adult) Medical Specialties New in year/Abandonded New in year/Completed New in Year/Roll-over Rolled-over/Abandoned Rolled-over/Completed Rolled-over/Roll-over Percentage of projects registered before start 100% 100% 15 80% 60% Make up of project team 9 80% 43 60% 40% 40% 20% 15 3 5 25 Emergency Department (Adult) Medical Specialties 20% 11 56 0% 0% Emergency Department (Adult) TRUE Clinical Audit Annual Report 2013/14 Medical Specialties FALSE Multi-professional Multi-specialty Neither Page 16 Percentage National Audit Percentage re-audit 100% 100% 80% 80% 60% 60% 40% 40% 15 63 8 20% 5 17 60 3 11 Emergency Department (Adult) Medical Specialties 20% 0% 0% Emergency Department (Adult) TRUE Medical Specialties FALSE TRUE FALSE Guidance/standards type audited 30 28 25 20 19 20 15 15 10 5 4 4 1 0 Emergency Department (Adult) NICE Medical Specialties Other National Local Unclassified Percentage report produced Percentage action plan produced 1 100% 80% 2 100% 80% 2 60% 60% 40% 40% 20% 20% 4 39 0% 6 38 Emergency Department (Adult) Medical Specialties 0% Emergency Department (Adult) TRUE Medical Specialties FALSE Yes No - Confirmed good practice Table 1 Title Sub-Specialty Lead Paracetamol Overdose (College of Emergency Medicine) Emergency Department Paul Reavely 1 Q3 In progress Severe Sepsis (College of Emergency Medicine) Emergency Department Lisa Munro Davis 1 Q3 In progress Radiology reporting Emergency Department Emma Redfern 2 Q3 In progress Consultant Sign Off (College of Emergency Medicine) Emergency Department Anne Frampton 1 Q1 Completed Community Acquired pneumonia Acute Medicine/ Emergency Department Richard Jeavons 3 Q3 Not started Clinical Audit Annual Report 2013/14 Priority Start date Status Q4 Page 17 Child protection/C4C Emergency Department Lead to be confirmed 2 Q3 Not started Chest Drain Emergency Department Phil Cowburn 3 Q3 In progress Sedation Emergency Department Rob Stafford 2 Q3 In progress Prescribing Emergency Department Becky Thorpe 2 Q2 In progress Pancreatitis Emergency Department Paul Reavely 3 Q3 In progress Severe sepsis Acute Medicine/ Emergency Department Jessica Triay 3 Q3 In progress National Hip Fracture Database (NHFD) Care of the Elderly Rachel Bradley 1 Q1 In progress National Audit of Dementia Care of the Elderly Julie Dovey 1 Q4 Not started Stroke National Audit Programme (SSNAP) Care of the Elderly Sarah Caine 1 Q1 In progress VTE prophlaxis management Care of the Elderly Peter Murphy/ Sarah Caine 2 Q2 Not started Thrombolysis management Care of the Elderly Peter Murphy/ Sarah Caine 2 Q2 In progress Management of genital herpes Contraception and Sexual Andrew Leung Health 3 Q3 Not started Management of early syphilis Contraception and Sexual Andrew Leung Health 3 Q3 Not started Management of late syphilis Contraception and Sexual Andrew Leung Health 3 Q3 Not started Management of lymphogranuloma venereum Contraception and Sexual Andrew Leung Health 3 Q3 Not started HIV testing in patients with lymphoma Contraception and Sexual Helen Wheeler Health 3 Q3 Not started HIV pepse audit of SARC patients Contraception and Sexual Rachel Westwick Health 3 Q3 In progress BASE – Sexual Health Outreach services Contraception and Sexual Nikki Jeal Health 3 Q3 Completed Integrated service at Bristol Sexual Health Centre Contraception and Sexual Judith Berry Health 3 Q3 Not started HIV Partner Notification Contraception and Sexual Andrew Leung Health 3 Q3 Not started Emergency IUD Contraception and Sexual Leonor HerreraHealth Vega 3 Q3 Not started Emergency contraception Contraception and Sexual Leonor HerreraHealth Vega 3 Q3 Not started Audit of NICE guidance on management of patients with psoriasis Dermatology David de Berker 2 Q1 Completed Audit of completeness of excision of non-melanoma skin cancer Dermatology in Bristol Dermatology Adam Bray 2 Q1 In progress Audit of notification of GPs of patient melanoma diagnosis within 24 hours Dermatology Gemma Gregory 2 Q1 In progress National Inpatient Diabetes Audit (NIDA) Diabetes and Endocrinology Bushra Ahmed 1 Q2 In progress Management of multiple endocrine neoplasia Diabetes and Endocrinology Karin Bradley 3 Q2 Not started Management of hypoglycaemic events Diabetes and Endocrinology Karin Bradley 3 Q3 Not started Prevalence and management of benign hypercalcaemia Diabetes and Endocrinology Karin Bradley 3 Q3 Not started Audit of Adult Outpatient Diabetes Care Diabetes and Endocrinology Natasha Thorogood 2 Q2 In progress Clinical Audit Annual Report 2013/14 Page 18 TA64 Growth hormone deficiency (adults) Diabetes and Endocrinology Karin Bradley 2 Q3 Completed National Inflammatory Bowel Disease audit Gastroenterology Tom Creed 1 Q1 In progress National COPD audit Respiratory Nabil Jarad 1 Q4 In progress British Thoracic Society audit programme Respiratory Lead to be confirmed 1 Q3 Complete Bronchoscopic lung volume reduction with airway valves for Respiratory/Thoracic Surgery Nabil Jarad/Tim Batchelor 2 Q3 In progress Oxygen prescription Respiratory Liz Gamble 3 Q2 Completed Suspected lymph node tuberculosis audit Respiratory Sarah Mungall 3 Q1 Not started Rheumatoid arthritis Rheumatology Robert Marshall 2 Q1 Completed The following activity was also in progress during the financial year (either rolled over from previous year or not identified through plan): Ref Provisional Title of Project Status Emergency Department (Adult) 3040 Chest drain procedure carried out in the Emergency Department In Progress 3068 Observation unit prescribing audit Completed 3111 re-audit of patient vital signs in the adult Emergency Department (ED) In Progress 3130 Consultant sign off (College of Emergency Medicine) Completed 3300 Renal Colic (College of Emergency Medicine) Completed 3363 Fractured Neck of Femur (College of Emergency Medicine) In Progress 3412 Re-audit of the initial management of sepsis In Progress 3440 Audit of quality of GP letters from patients discharged from the Emergency Department Completed 3468 Management of out of hospital cardiac arrest Completed 3488 Management of primary spontaneous pneumothorax in emergency medicine. In Progress 3516 An audit of palliative care practices in the BRI ED In Progress 3543 National Audit of Seizure Management (NASH) Completed 3544 Paracetamol Overdose (College of Emergency Medicine) In Progress 3558 Audit of the Emergency Departments' Pancreatitis Management In Progress 3559 Missed Doses in ED In Progress 3591 Ensuring time critical radiological findings ordered from the ED are reviewed in a timely manner In Progress 3592 To audit the results of radiology imaging requested in the Emergency Department In Progress 3593 Management of head injuries presented to the BRI Emergency Department In Progress 3597 Chest Drain re-audit (initial audit ID 3040) In Progress 3660 Procedural sedation in the Emergency Department In Progress Medical Specialties/Acute Medicine 2738 Clotting and D dimer use in the Medical Assessment Unit Abandoned 3411 Defining the diagnosis of subarachnoid haemorrhage (SAH) Completed 3453 Review of the medical response to acutely ill patients determined by Early Warning Scores (EWS) Completed 3563 Prescription and documentation of Non-invasive Ventilation (NIV) therapy Completed Clinical Audit Annual Report 2013/14 Page 19 Medical Specialties/Care of the Elderly 2968 Audit of Appropriateness of Blood Transfusions Completed 3104 Timely brain imaging for stroke patients Completed 3177 The Acute Management of Hyponatraemia Completed 3353 Post-operative care of over 80 year olds after elective surgery (NCEPOD recommendations) Completed 3487 Audit of Parkinson Medication Prescribing and Administration Completed 3489 Audit of Stroke Re-admissions September 2012 - February 2013 Abandoned 3524 An audit of appropriate thrombolysis for stroke patients In Progress 3526 OLP001 - National Audit of Dementia (NAD) Completed 3550 Stroke Thrombolysis Audit In Progress 3564 An audit of the diagnosis and treatment of Urinary Tract and catheter associated infections in patients over 65 years in the Bristol Royal Infirmary In Progress 3651 Audit on the accuracy of respiratory rate and its effects on EWS In Progress 3652 Assessment of the management of anaemia perioperatively in patients undergoing total hip replacements for fractured In Progress neck of femur 3677 Management of patients with a fracture neck of femur who take novel oral anticoagulation medication (NOAC) In Progress 3678 Management of patients with a fractured neck of femur who take warfarin anticoagulation medication In Progress 3720 Use of Abbey pain scale in patients with dementia and delirium over the age of 75 years In Progress Medical Specialties/Contraceptive & Sexual Health Services (CASH) 2990 Quick Starting Contraception following the administration of progestogen-only emergency contraception Completed 2995 An audit of Long Acting Reversible Contraceptives (LARC) Problem Management at Bristol Sexual Health Completed 3167 Audit of HIV testing among patients with Hepatitis B and/or Hepatitis C infection attending the Hepatology clinic Completed 3205 Sexual Health Outreach services – occupational health needs of women selling sex on the street in Bristol Completed 3251 Audit of the Management of Epididymo-orchitis at Bristol Sexual Health Centre In Progress 3344 The use of the Patient Group Direction for the Progestogen-Only Sub-Dermal Contraceptive Implant (Nexplanon®) at Bristol Sexual Health Service Completed 3525 Audit of the management of gonorrhoea infection in patients who attend Bristol sexual health services Completed 3551 Audit of HSA1 form for CQC standard compliance and early medical abortion protocol UK In Progress 3629 HIV PEPSE proforma audit In Progress 3641 Re-audit of quick starting contraception following implementation of a 'Quick starting Contraception' check list into the emergency contraception form In Progress 3650 Re-audit of patient records for under 18s in Sexual Health Services in Bristol In Progress Medical Specialties/Dermatology 3360 Regional audit of TL01 therapy for chronic or guttate plaque psoriasis Completed 3367 NICE technology appraisal TA180 Ustekinumab for the treatment of adults with moderate to severe psoriasis Completed 3467 Implementing NICE guidance for the assessment and management of psoriasis Completed 3486 Audit on legibility of patient dermatology notes Completed 3518 An audit on informed consent in Dermatological Surgery Completed 3519 Management of recurrent and incompletely excised Basal Cell Carcinoma Completed 3521 Dermatology Outpatient Waiting Times Completed 3522 Methotrexate monitoring in psoriasis patients Completed 3536 Re-audit of the quality indicators in a teledermatology service Completed 3569 Skin Cancer Complete Excision Rates Audit Ongoing Project 3601 Retrospective audit of patients on anticoagulants undergoing dermatological procedures Completed 3649 Melanoma Pathway Audit In Progress Clinical Audit Annual Report 2013/14 Page 20 Medical Specialties/Diabetes & Endocrinology 3263 Audit of inpatient management of diabetic foot problems Completed 3266 NICE technology appraisal TA203 Liraglutide for the treatment of type 2 diabetes Completed 3336 National Diabetes Inpatient Audit In Progress 3478 Audit of the management of hyperglycaemia in acute coronary syndromes Completed 3485 Audit of Adult Outpatient Diabetes Care at the UH Bristol General Diabetes clinics In Progress 3698 Re-audit of the management of hyperglycaemia in acute coronary syndromes In Progress 3723 Audit of Growth Hormone replacement in adults with Growth Hormone Deficiency In Progress Medical Specialties/Gastroenterology & Hepatology 2603 LTC004 - National Adult Inflammatory Bowel Disease Audit In Progress 3122 NICE technology appraisal TA187 Infliximab and adalimumab for the treatment of Crohn’s disease Completed 3306 Audit of missed doses of medication on ward 11 Completed 3600 Re-Audit of when antibiotics prescribed and when given on ward 11 Completed 3670 Adherence of Hepatitis B screening in patients with Inflammatory Bowel Disease (IBD) starting Immunosuppressive Therapy In Progress Medical Specialties/General Medicine 3118 Duplication of drug prescription / Inappropriate rapid re-dosing in ED and MAU Completed 3198 Audit of the management of cellulitis Completed 3598 An Audit of patients admitted with Acute Alcohol Withdrawal In Progress 3355 Audit of DVT Diagnosis through the Thrombosis Clinic Completed Medical Specialties/Liaison Psychiatry 3197 Re-auditing depression with a chronic physical health problem Completed 3528 Improving DNA rates in Liaison Psychiatry Outpatient Clinics In Progress 3589 Audit of frequent attenders with self-harm to the Emergency department Completed Medical Specialties/Respiratory 3291 Blood glucose monitoring in Cystic Fibrosis patients during first 48 hours of admission to cystic fibrosis unit In Progress 3354 Bronchectasis audit (British Thoracic Society) In Progress 3462 Isolation in Patients with Possible Pulmonary Tuberculosis Completed 3520 Non-Invasive Ventilation (British Thoracic Society) In Progress 3523 An audit of smoking cessation advice given to current smokers Completed 3599 British Thoracic Society (BTS) Emergency Oxygen Audit 2013 Completed 3722 National Chronic Obstructive Pulmonary Disease (COPD) audit In Progress Medical Specialties/Rheumatology 3406 NICE technology appraisal TA161 Secondary prevention of osteoporotic fragility fractures in postmenopausal women In Progress 3447 NICE TA130 Rheumatoid arthritis - adalimumab, etanercept and infliximab Completed 3697 Does current blood test monitoring lead to treatment change in Ankylosing Spondylitis patients on TNFi In Progress The following section summarises the changes, benefits or actions introduced as a result of completed audits within the Division/specialties. 3440 This audit demonstrated that the quality of GP letters from patients discharged from the Emergency Departed exceeded those reported nationally. To improve the quality further, education sessions were conducted for staff highlighting the requirements of a good letter and the need to accurately record key information on Medway. 3468 A post cardiac care bundle document was written to aid the management of post cardiac arrest patients presenting to the emergency department as a result of this audit. Clinical Audit Annual Report 2013/14 Page 21 3601 This audit demonstrated good compliance standards for not stopping anticoagulants prior to surgery. The need to develop clear guidelines with nursing staff on post-operative management of patients on agents that alter blood coagulation was recognised and implemented. 3462 Education sessions were conducted for all Medical Assessment Unit nursing teams regarding a new protocol and which patients should be considered for isolation for possible pulmonary TB as a result of this audit. Consultants have been reminded to review chest x-rays on post take ward rounds. 3104 This audit led to the introduction to ‘Direct to CT’ for all pre-alerted patients as part of the ‘Stroke 90’ project to help improve compliance with timings of brain imagining within 1 hour and 24 hours of arrival. 3453 Awareness of the importance of the timely and appropriate escalation of patients to clinical staff for patients with a EWS>=4 was highlighted to all medical staff at presentations as a result of this audit. Further improvements on the documentation of ceiling of care, critical care consideration and discussions with the next of kin were highlighted. 3167 This audit demonstrated that the documentation of whether patients who are Hep B surface antigen positive are offered a HIV test within 6 months of attendance needed to improve. Educational presentations were made to all doctors in the department to ensure this test is offered to appropriate patients and documented if declined. 3118 This audit led to an amendment to the drug chart section of the Emergency Department notes to make it clearer when drugs have already been given in the ED. 3667 Excellent results against standards except for the provision of written information about psoriasis and the treatment and care were demonstrated through this audit. A new assessment proforma detailing information giving was implemented was implemented to improve standards further. 3263 As a result of this audit, a single inpatient diabetes foot pathway is to be introduced along with a CQUIN for an inpatient Diabetes Specialist Nurse for Specialised Services. 3563 This audit highlighted the need for improvement in the documentation of Non-Invasive Ventilation (NIV) therapy. Education of junior doctors regarding areas for improvement was conducted. A NIV prescription chart has been designed and implemented. 3122 In addition to confirming our compliance with relevant NICE guidance on the use of two drugs in Crohn's disease, this audit has led to improvements in the way that we document such treatment, which better informs a patient's annual review. 2968 This audit led to teaching sessions on appropriate blood transfusion to new doctors following clarification and agreement as to which guidelines to follow. 3411 The need to develop a lumbar puncture proforma to aid documentation was identified through this audit. Recommendations to keep a lumbar puncture trolley (containing all required equipment) in the MAU and Ambulatory Acer Units are in the process of being implemented. 3447 This audit demonstrated good compliance against standards for the treatment of patients with Rheumatoid Arthritis. A nurse referral form (for completion by the doctor who refers the patient for biological therapy) to ensure 2 DMARDs have already been tried was implemented. Patient review dates will be recorded in the Cellma database. 3177 A local clinical guideline for the management of hyponatraemia is in the process of being developed as a result of this audit. 3344 As a result of this audit areas of poor documentation of key information were identified, highlighting the need to amend the progesterone only sub dermal contraceptive implant proforma. The service is moving towards an electronic patient record which will improve the recording of this clinical information. 3205 Poor compliance regarding documentation of care offered and patient information taken resulted in the development of a clinical guideline for the ‘One25’ sexual health clinic and an agreement amongst clinical staff on the development of history taking/testing frequency guidelines. 3600/ 3306 This re-audit showed an increase in compliance for antibiotics given within 1 hour of prescribed time on ward 11. Teaching sessions were given following first audit (ID 3306) to all clinical staff. Stock levels on wards were also reviewed. 3355 This audit led to the implementation of a protocol for the management of upper limb DVT. 3360 This multi-centre audit identified a delay in patients starting treatment across both centres as the 90% target was not met for starting treatment within 6 weeks. Results were fedback to both teams and re-audit recommended. The audit demonstrated that all pre-phototherapy checks are completed and all patients referred urgently are seen within the three week recommended timeframe. 3197 This complex audit highlighted areas of inappropriate prescribing which lead to teaching sessions and dissemination of information across both secondary and primary care. 3198 The Trust Cellulitis guidelines were updated as a result of this audit. Clinical Audit Annual Report 2013/14 Page 22 3589 Care plans for the treatment of self-harm patients presenting to the Emergency Department have been reviewed and amended as a result of this audit. More defined criteria regarding review dates, patient and relevant others participation in the implementation of the plans and whether it was shared with the GP have been included. 3522 This audit demonstrated good compliance with standards for baseline blood measurements but also highlighted areas of improvement in baseline chest X-Rays and conducting weekly bloods until dose is stabilised. A nurse led nutrition and monitoring clinic for methotrexate with scope for consultant referrals for drug monitoring with blood tests/BP/urinalysis was introduced. Education sessions for all staff on documenting contraceptive advice given and the need to order chest X-rays and to weigh the patient are being introduced. 3523 This rapid cycle audit was conducted three times with continuous improvements against standards for smoking cessation advice given at each cycle. An education programme including presentations, posters and leaflets was delivered to all doctors involved in the medical take, 3519 Audit identified that discussions of incompletely excised Basal Cell Carcinomas (BCCs) are not always discussed at the Multidisciplinary Team meetings (MDT). The need to use one system for requesting histology reports of skin biopsies was identified and is being researched. Recommendations made for the use of the UK national minimum dataset for pathology reporting of BCCs. 3478 A proforma for the diabetes management of patients with hyperglycaemia after acute coronary syndrome was implemented as a result of this audit. 3525 This audit demonstrated generally very good compliance against standards for the management of gonorrhoea. The service is moving towards an electronic patient record (EPR) therefore additional tick boxes for ‘test offered’ and ‘written information offered’ will be included in the EPR as a prompt. 2995 A mail merge letter template outlining possible treatment regimes for LARC bleeding problems has been designed as a result of this audit. A BSH pathway for identifying gynaecological pathology and when to refer is in development. 3487 An alert sticker for the drug charts of people with Parkinson’s Disease (PD) was developed and introduced as a result of this audit. Staff education on the importance of correct prescribing and administration of PD drugs was conducted. Pharmacy will ensure that medications are always available, including out of hours, with back up supplies in emergency drug store. 3266 This audit led to the development of a local policy (in agreement with the local NICE Commissioning College) for patients who can have liraglutide in combination with insulin. 3486 This audit has led to the development of an electronic proforma on Medway to improve documentation of information for dermatology patients 2990 As a result of this audit, Patient Group Directives updated to include guidance on quick starting contraception. The emergency contraception proforma has also been updated to include check boxes for key discussion points with patients. Staff training has been undertaken on guidelines at both central and community sites. 3518 This audit demonstrated that information relating to consent was generally documented for dermatological surgery. Booking letters have been amended to include ‘top tips’ to help improve practice further. 3521 This audit of outpatient waiting times demonstrated that approximately 80% of patients are seen within 30 minutes of arrival in clinics. A number of modifications to the waiting room have been made to improve patient comfort and appointment letters updated to include warning of potential long waits. 3536 Improved compliance of quality indicators in teledermatology was demonstrated by this re-audit. Web links have been included in feedback to GPs with tips on photographic techniques along with the use of GP reflective learning templates to aid further improvements. 3467 Lead dermatology nurse and consultant provided Psoriasis Area and Severity Index (PASI) and Psoriasis Epidemiological Screening Tool (PEST) workshops for rheumatology and dermatology teams as a result of this audit. PEST, PASI and Dermatology Quality Life Index (DQLI) packages have been designed and are available in clinic. Clinical Audit Annual Report 2013/14 Page 23 3.3 SPECIALISED SERVICES The following chart shows the status at year end of those projects identified as priorities for audit as part of the forward planning process in 2013/14. Full details of the status of individual projects on this plan can be found within table 1 of this section. Progress of planned projects Complete 100% 80% 60% 40% 20% 0% In progress Not started 1 2 5 2 4 1 1 2 1 Cardiac Services 2 Oncology, Heamatology & Palliative Medicine Prioritisation category The chart below shows the status at year end of all registered projects (excluding those classified as ongoing monitoring). Some projects will have started and finished within the financial year, some will have been started but have yet to complete and are therefore rolled over. The figures also include projects that commenced in previous years but have now been abandoned, those that previously commenced but were completed in 2013/14 and those previously commenced but not completed by the end of 2013/14. Individual project status at year end 9 10 9 7 8 6 6 3 4 3 2 2 1 2 1 1 1 0 Cardiac Services Oncology & Clinical Haematology & Palliative Medicine New in year/Abandonded New in year/Completed New in Year/Roll-over Rolled-over/Abandoned Rolled-over/Completed Rolled-over/Roll-over Percentage of projects registered before start 100% 80% 5 Make up of project team 100% 80% 7 60% 60% 40% 40% 20% 14 19 20% 16 13 3 2 5 6 Cardiac Services Oncology & Clinical Haematology & Palliative Medicine 0% 0% Cardiac Services TRUE Clinical Audit Annual Report 2013/14 Oncology & Clinical Haematology & Palliative Medicine FALSE Multi-professional Multi-specialty Neither Page 24 Percentage National Audit Percentage re-audit 100% 100% 80% 80% 60% 60% 40% 20% 16 23 5 1 40% 18 17 20% 4 6 Cardiac Services Oncology & Clinical Haematology & Palliative Medicine 0% 0% Cardiac Services Oncology & Clinical Haematology & Palliative Medicine TRUE TRUE FALSE FALSE Guidance/standards type audited 10 8 8 8 8 8 6 4 4 4 4 2 1 0 Cardiac Services Oncology & Clinical Haematology & Palliative Medicine NICE Other National Local Percentage report produced Percentage action plan produced 100% 1 100% 80% 80% 4 60% 60% 40% 40% 20% Unclassified 3 1 20% 7 0% 2 10 Cardiac Services Oncology & Clinical Haematology & Palliative Medicine 0% Cardiac Services TRUE Oncology & Clinical Haematology & Palliative Medicine FALSE Yes No - Confirmed good practice Table 1 Title Sub-Specialty Lead Adult Cardiac Surgery (ACS) Cardiac Surgery Alan Bryan 1 Q1 In progress Acute Coronary Syndrome/Acute Myocardial Infarction (MINAP) Cardiology Julian Strange 1 Q1 In progress National Cardiac Arrhythmia Audit (HRM) Cardiology Tom Johnson 1 Q1 In progress National Heart Failure Audit (HF) Cardiology Angus Nightingale 1 Q1 In progress Adult Coronary Angioplasty Cardiology Tom Johnson 1 Q1 In progress TA230 Myocardial infarction (persistent ST-segment elevation) bivalirudin Cardiology Julian Strange 2 Q3 Not started Clinical Audit Annual Report 2013/14 Priority Start date Status Q4 Page 25 Sutureless Aortic Valve Replacement Cardiac Surgery George Asimakopoulos 2 Q3 Not started National Lung Cancer Audit (NLCA) Oncology/Respiratory Adam Dangoor 1 Q1 In progress VTE Prophylaxis/risk assessment Haematology Amanda Clarke 1 Q2 In progress NICE TA193 Leukaemia (chronic lymphocytic, relapsed) rituximab Haematology Jenny Bird 1 Q2 Completed An audit of Identification of patients in the last year of life and advance care planning in respiratory disease Palliative Medicine/ Respiratory Colette Reid 2 Q1 Completed An audit of Identification of patients in the last year of life and advance care planning in patients with dementia Palliative Medicine Colette Reid 2 Q1 Completed An audit of Identification of patients in the last year of life and advance care planning in patients with advanced cancer Palliative Medicine Colette Reid 2 Q1 Completed An audit of Identification of patients in the last year of life and advance care planning in frail elderly patients Palliative Medicine Colette Reid 2 Q1 Not started An audit of interventions and investigations in the last week of life Palliative Medicine Colette Reid 2 Q1 Completed The following activity was also in progress during the financial year (either rolled over from previous year or not identified through plan): Ref Provisional Title of Project Status Cardiac Services/Cardiac Surgery 3304 Early and long-term outcome of mitral valve surgical procedures in adult patients In Progress 3305 Audit of transaortic sutureless aortic valve implantation outcomes - a Bristol Heart Institute experience Abandoned 3307 The effect of arterial cannulation strategy (axillary vs. femoral vs. ascending aortic) on outcomes following aortic surgery Abandoned 3471 Clinical outcomes after second time cardiac re-operations and complex aortic procedures Abandoned 3505 Anticoagulation management for patients with new onset atrial fibrillation after Coronary Artery Bypass Graft surgery Completed Cardiac Services/Cardiology 2910 Audit of Echocardiographic follow-up after Aortic Valve Replacement (AVR) Abandoned 2933 Management of Pregnant Patients with Aortopathy Completed 2960 Should we still be screening patients with Coarctation of the Aorta for Intracranial Aneurysms? A re-audit. In Progress 3262 NICE technology appraisal TA95 Implantable Cardioverter Debfibrillators (ICDs) for the treatment of arrhythmias In Progress 3301 Poor nutrition links to higher incidence of pressure ulcers for inpatients. Are patients being educated? In Progress 3374 Audit of implantable devices used in cardiac rhythm management at University Hospitals Bristol In Progress 3375 Outcomes following VT ablation In Progress 3465 Audit of Percutaneous Balloon Mitral Valvuloplasty In Progress 3480 Effectiveness of paroxysmal and persistent atrial fibrillation ablation In Progress 3557 Ambulatory blood pressure monitoring audit Completed 3654 Simvastatin and calcium channel blocker prescription In Progress 3655 Renin-Angiotensin-Aldosterone System (RAAS) medication prescription In Progress 3665 Documentation of TR Band removal and radial artery occlusion rate post coronary intervention via the radial route In Progress 3700 Audit of Non ST segment elevation myocardial infarction (NSTEMI) pathway In Progress 3701 Conscious Sedation for Transoesophageal Echocardiography In Progress Oncology & Clinical Haematology/Clinical Haematology 3639 Audit of the new Trust guidelines for the management of febril neutropaenia In Progress 3695 Consent for chemotherapy for patients diagnosed with Acute Myeloid Leukaemia (AML) In Progress Clinical Audit Annual Report 2013/14 Page 26 Oncology & Clinical Haematology/Oncology 2999 Keyworkers for Teenagers and Young Adults with cancer Completed 3057 Trastuzumab in advanced breast cancer NICE TAG 34/CG 81 Completed 3119 Use of Sunitinib in advanced/metastatic renal cell carcinoma - re-audit of NICE TA169. Completed 3285 An audit of weekly checks documentation undertaken within the Radiotherapy Department at the BHOC Completed 3297 Adjuvant use of Docetaxel in Breast cancer - NICE TA 109/CG 80/ASWCS Completed 3322 Intravenous contrast during radiotherapy planning Completed 3351 Completeness of chemotherapy pre assessment and administration charts In Progress 3352 GCSF (Neulasta) and treatment of febrile neutropenia (FN) post TAC chemotherapy in breast cancer patients - re-audit Completed 3378 Management of Metastatic Spinal Cord Compression - re-audit NICE CG75/92/29 In Progress 3389 Neutropaenia Sepsis - re-audit Abandoned 3490 Neo-adjuvant treatment in breast cancer Abandoned 3553 An audit to assess the prevention of corticosteroid-induced osteoporosis in patients with CNS tumours In Progress 3554 Referral of 15-24 year old patients with cancer to the TYA MDT In Progress 3613 A re-audit of weekly checks documentation undertaken within the radiotherapy department at the BHOC In Progress 3621 An audit of Post Radio-iodine Ablation follow-up for differentiated thyroid cancer In Progress 3630 Audit of patient monitoring practice in patients receiving Abiraterone acetate and prednisolone for metastatic castration resistant prostate cancer In Progress Oncology & Clinical Haematology/Palliative Medicine 3399 Audit of end of life discussions in patients with COPD Completed 3416 Audit of ‘Do not attempt resuscitation’ documentation (part of a BNSSG-wide audit) In Progress 3727 National Care of the Dying Audit – UH Bristol version 2014 In Progress The following section summarises the changes, benefits or actions introduced as a result of completed audits within the Division/specialties. 3505 This audit has led to increased awareness of anticoagulaton management for patients with new onset atrial fibrillation after coronary artery bypass graft surgery. Staff have been advised to calculate patients’ CHADS-2 score and base their anticoagulation strategy on this. 2933 New regional referral guidelines were sent out to district general hospitals in South West that the risk of aortopathy in pregnancy should be discussed with patients with Marfan’s Syndrome. Early to the regional centre for assessment or advice was agreed to be a good approach. 3557 This audit demonstrated acceptable compliance with recommendations outlined in NICE guidance for the treatment of hypertension. The number of daytime blood pressure readings used to calculate average daytime ambulatory blood pressure was found to be undertaken as required. 3352 This audit demonstrated that all patients were treated as per local neutropenic sepsis guidelines. The TAC protocol has been amended as per cancer network guidelines. 3057 The addition of a chemocare on-screen prompt to check and record HER2 status has been implemented as a result of this audit. A Trastuzumab prescribing checklist has also been designed and implemented for doctors to act as an aide memoire. 3297 Excellent compliance with standards for breat cancer treatment was demonstrated by this audit. The need for a future prospective audit has been identified for patients who are node positive/high risk who did not receive a taxane. 3119 As a result of this audit, a proforma has been developed and implemented for patients starting Sunitinib to improve future compliance with NICE guidelines. 3285 This audit has led to the establishment of a working sub group to improve compliance of the completion with weekly radiotherapy checks. This multidisciplinary group will review the current protocol and form. A re-audit following implementation of an updated protocol and form will be undertaken. 3322 This audit has led to further staff education to emphasise to all medical staff that IV contrast is available for CT scans and should be used for planning tumour sites as recommended by Royal College of Radiologists (2004) guidance. 2999 The need to improve documentation of a named key worker for patients in the Teenage and Young Person Service was identified through this audit. This service is in the process of being developed and the results of this audit will be Clinical Audit Annual Report 2013/14 Page 27 incorporated into the new service. 2997 Areas for improvement in prescribing documentation were identified as a result of this audit. Results have been widely circulated and presentations made to help raise awareness of the issues and to improve practice. 3399 This audit identified areas for improvement regarding discussion with patients about End of Life care (EOL) and communication with the GP. Amendments have been made to the ICE system to make ‘Discussions around end of life care’ a mandatory field. The Palliative Care Team now attends respiratory board rounds to help with the management of these patients and a process for sending letters to GPs regarding EOL discussion has been implemented. 3644 This audit identified areas for improvement regarding documentation of communication with GP and the offer to patients and relatives to participate in advance care planning for patients with dementia. Education and awareness to all appropriate staff to improve these areas of care has been undertaken. Ward board rounds are now used to identify those patients with dementia thought to be in the last year of life. 3491 This audit identified areas for improvement regarding standards to manage patients with advanced cancer. Results have been widely circulated and presentations made to help raise awareness of the issues and to improve practice. Clinical Audit Annual Report 2013/14 Page 28 3.4 SURGERY, HEAD AND NECK The following chart shows the status at year end of those projects identified as priorities for audit as part of the forward planning process in 2013/14. Full details of the status of individual projects on this plan can be found within table 1 of this section. Progress of planned projects Complete In progress Not started 100% 80% 3 60% 3 3 40% 3 1 1 2 2 3 1 3 Anaesthesia, Critical Care & Theatres 6 1 1 2 1 1 1 2 4 2 3 4 0% 1 3 2 4 20% 1 3 Dental Services 6 2 2 Ophthalmology 2 4 Surgical Specialties Prioritisation category The chart below shows the status at year end of all registered projects (excluding those classified as ongoing monitoring). Some projects will have started and finished within the financial year, some will have been started but have yet to complete and are therefore rolled over. The figures also include projects that commenced in previous years but have now been abandoned, those that previously commenced but were completed in 2013/14 and those previously commenced but not completed by the end of 2013/14. Individual project status at year end 14 12 10 8 6 4 2 0 12 11 9 8 8 7 6 8 8 5 2 1 1 3 2 1 Anaesthesia, Critical Care & Theatres 1 1 1 Adult Surgical Specialties 1 1 2 1 Ophthalmology 1 Dental & Maxillofacial Surgery (inc. ENT) New in year/Abandonded New in year/Completed New in year/Deferred New in Year/Roll-over Rolled-over/Abandoned Rolled-over/Completed Rolled-over/Deferred Rolled-over/Roll-over Percentage of projects registered before start 3 100% 80% 12 11 4 6 Make up of project team 100% 80% 8 60% 60% 40% 40% 20% 20% 14 26 23 34 0% 15 2 5 14 5 14 2 10 11 0% Anaesthesia, Adult Surgical Ophthalmology Dental & Critical Care & Specialties Maxillofacial Theatres Surgery (inc. ENT) TRUE Clinical Audit Annual Report 2013/14 FALSE 31 5 4 Anaesthesia, Adult Surgical Ophthalmology Dental & Critical Care & Specialties Maxillofacial Theatres Surgery (inc. ENT) Multi-professional Multi-specialty Neither Page 29 Percentage National Audit Percentage re-audit 100% 100% 80% 80% 60% 60% 40% 16 20% 40% 23 6 13 39 1 26 1 6 20% 0% 17 23 5 6 28 14 12 0% Anaesthesia, Adult Surgical Ophthalmology Dental & Critical Care & Specialties Maxillofacial Theatres Surgery (inc. ENT) TRUE Anaesthesia, Adult Surgical Ophthalmology Dental & Critical Care & Specialties Maxillofacial Theatres Surgery (inc. ENT) FALSE TRUE FALSE Guidance/standards type audit 25 22 20 16 14 15 8 10 12 10 5 5 5 11 7 3 3 2 0 Anaesthesia, Critical Care & Theatres Adult Surgical Specialties NICE Other National Ophthalmology Local Unclassified Percentage report produced Percentage action plan produced 100% 100% 1 80% 5 60% Dental & Maxillofacial Surgery (inc. ENT) 6 1 3 1 80% 5 60% 40% 40% 20% 7 2 7 20% 14 0% 6 2 7 17 0% Anaesthesia, Adult Surgical Ophthalmology Dental & Critical Care & Specialties Maxillofacial Theatres Surgery (inc. ENT) TRUE Anaesthesia, Adult Surgical Ophthalmology Dental & Critical Care & Specialties Maxillofacial Theatres Surgery (inc. ENT) FALSE Yes No - Confirmed good practice Table 1 Title Sub-Specialty Lead Emergency Laparotomy Anaesthesia/Surgery Rachel Craven/ Jane Blazeby 1 Q3 In progress SPINT/ASAP audit Anaesthesia Frances Forrest/ Rachel Bradley 2 Q1 In progress Abbey pain chart for patients with dementia/cognitive impairment Anaesthesia/Acute Pain Team Lead to be confirmed 2 Q3 Not started Presence of essential emergency information in theatres Anaesthesia Diana Terry 3 Q3 Not started Safe prescribing and completion of drug charts Anaesthesia Diana Terry 2 Q3 Not started Clinical Audit Annual Report 2013/14 Priority Start date Status Q4 Page 30 South West Quality and Patient Safety Improvement Programme Theatres (Critical Care) Sanjoy Shah 2 Q1 In progress Adult critical care case mix programme (ICNARC CMP) Critical Care Tim Gould 1 Q1 In progress Potential Donor Audit Critical Care Fran O’Higgins 1 Q1 In progress ALung Hemolung Respiratory Assist System Critical Care Tim Gould 2 Q1 Not started Audit of medication errors on ICU Critical Care John Warburton 2 Q1 In progress Audit of blood transfusion practice Critical Care Dan FreshwaterTurner 3 Q1 Not started Audit of appropriate PPI prescribing Critical Care Tim Gould 3 Q1 Not started Liz Varian 2 Q1 In progress South West Quality and Patient Safety Improvement Programme Theatres (Perioperative Care) National Head & Neck Cancer (DAHNO) Oral and Maxillofacial Surgery Ceri Hughes 1 Q1 In progress Pre-formed metal crown failure rates Primary Care Dental Service Katherine Walls 4 Q4 In progress Dental undergraduate treatment plans (re-audit) Restorative Dentistry Rob Jagger 4 Q2 Completed Extraction of first permanent molars (re-audit) Child Dental Health Sarah Dewhurst 4 Q1 Completed Salivary gland imaging (re-audit) Dental Radiology Jane Luker/ Rebecca Davies 4 Q3 In progress Condition of surgical margins in resections for cancer of the oral Oral and Maxillofacial cavity and oropharynx Surgery Ceri Hughes 4 Q4 Not started Primary Care Unit protocols for patients with suspected coagulation defects Oral Medicine / Oral Surgery Sarah Ellison/Tony Brooke 4 Q4 Not started Primary Care Unit patient satisfaction (re-audit) Oral Medicine Tony Brooke 4 Q3 Not started Mental Capacity Act Hospital wide Sarah Foy/Tony Brooke 3 Q3 Not started Endoscopic sinus surgery outcomes (re-audit) Adult ENT Claire LangtonHewer 4 Q3 Not started Turbinate surgery Adult ENT Claire LangtonHewer 4 Q3 Not started Implantation of multifocal intraocular lenses during cataractsurgery Cornea and Cataract Phil Jaycock 2 Q4 Not started Boston Type 1 Keratoprosthesis Cornea and Cataract Derek Tole 2 Q1 Completed Intraocular lens insertion for correction of refractive error with preservation of the natural lens guidance Cornea and Cataract Phil Jaycock 2 Q4 Not started TA229 Macular oedema (retinal vein occlusion) – dexamethasone Medical & Surgical Retina Claire Bailey 2 Q1 In progress Deep Sclerectomy (non-penetrating glaucoma filtration surgery) Glaucoma Rani Sebastian 2 Q1 In progress Selective Laser Trabeculoplasty (SLT) Glaucoma Rani Sebastian 2 Q4 Not started Trabeculectomy outcomes Glaucoma John Sparrow/ Peter Tsangaris 4 Q1 Not started Microbial Keratitis re-audit Cornea and Cataract Derek Tole/Stuart Cook 4 Q2 In progress Cataract Outcomes Cornea and Cataract Derek Tole 3 Q1 Completed A&E 4 hour breaches and follow-ups A&E & Primary Care Derek Tole/Rafik Girgis 3 Q3 Not started Lucentis outcomes Medical & Surgical Retina Adam Ross (Cons) 3 Q2 Not started Clinical Audit Annual Report 2013/14 Page 31 Referral and treatment times for Diabetic retinopathy and maculopathy Medical & Surgical Retina Outcomes of nasolacrimal duct probing (re-audit) Abosede Cole/ Kate Powell 3 Q4 Not started Paediatrics, Oculoplastics Amanda Churchill and Squint 4 Q1 Not started Documenting Non-Accidental Injury Paediatrics, Oculoplastics Cathy Williams and Squint 4 Q2 Completed Paediatric Eye Service Satisfaction Survey Paediatrics, Oculoplastics Amanda Churchill and Squint 4 Q2 Completed Discharge of paediatric patients from orthoptic department Orthoptics and Optometry Ann Starbuck/ Estelle Bishop 4 Q1 Not started Assessment of orbital trauma patients (re-audit) Orthoptics and Optometry Ann Starbuck/ Estelle Bishop 4 Q2 Not started Instilling of dilating drops in children for refraction and fundus and media examination Orthoptics and Optometry Ann Starbuck/ Estelle Bishop 4 Q3 Not started Visual outcomes in Congenital cataract patients Orthoptics and Optometry Sarah Smith 4 Q2 Not started National Bowel Cancer Audit (NBOCAP) Colorectal Rob Longman 1 Q1 In progress SECCA (Radiofrequency Ablation for Feacal Incontinence) Colorectal Paul Sylvester 2 Q3 In progress CT-guided guidewire localisation of impalpable lung lesions before minimal access surgical excision Thoracic Tim Bachelor 2 Q3 In progress National Joint Registry (NJR) Trauma & Orthopaedics Sanchit Mehendale 1 Q1 In progress Trauma (TARN) Trauma & Orthopaedics Matt Thomas 1 Q1 In progress National Oesophago-Gastric Cancer Audit (NAOGC) Upper GI Paul Barham 1 Q1 In progress VSGBI Vascular Surgery Database Vascular Peter Lamont 1 Q1 In progress NICE TA167 Abdominal aortic aneurysm - endovascular stent grafts Vascular Marcus Brooks 1 Q1 Completed Carotid interventions (CIA) Vascular Peter Lamont 1 Q1 In progress Fenestrated endovascular aortic stent graft for juxta-renal abdominal aortic aneurysm repair (F-EVAR) Vascular Marcus Brooks 2 Q3 Not started The following activity was also in progress during the financial year (either rolled over from previous year or not identified through plan): Ref Provisional Title of Project Status Adult Ear, Nose and Throat (ENT) 3079 ENT urgent clinic letters Abandoned 3080 Accuracy of MRI scans in the detection of primary and recurrent cholesteatoma Abandoned 3125 Coding by Theatre staff Completed 3270 Tympanomastoid Surgery Abandoned 3278 Current practice in septoplasty Completed 3469 Antibiotic prescribing - re-audit Completed 3474 ENT Outpatient procedures coding Completed 3646 Provision of patient information in ENT: informed consent In Progress 3657 Infectious mononucleosis screening in tonsillitis Completed 3685 ENT Hot clinic referrals In Progress 3079 ENT urgent clinic letters Abandoned Clinical Audit Annual Report 2013/14 Page 32 Anaesthesia & Critical Care & Theatres – Anaesthesia 2959 Fasting times in trauma surgery Abandoned 3449 Completion of pre-operative anaesthetic review documentation. Completed 3517 An audit of the alarm settings on anaesthetic machines in Bristol Royal Infirmary Completed 3658 Obstetric Anaesthesia Documentation Audit In Progress 3666 An audit of analgesia prescribing in acute medical and surgical admissions with renal impairment Completed 3687 Lung protective ventilation in theatres In Progress 3422 Appropriateness of referrals to pain management programme (PMP) Completed 3494 Management of patients undergoing major lower limb amputation - Severn deanery project In Progress 3530 Chronic pain- Audit of record keeping standards during epidural injections for the management of spinal origin pain In Progress 3669 Frequency and Severity of Complications of Ophthalmic anaesthesia in Cataract surgery In Progress 3705 Safety of epidural catheter removal as part of the acute pain management In Progress 1704 Dural Puncture Ongoing Project 2906 Obesity in Obstetric Anaesthesia [re-audit of 1966] Abandoned 3457 Caesarean section anaesthesia: technique and failure rate [re-audit of 1703] Completed 3643 Adequacy of Post Caesarean Section Pain Relief [re-audit of 1170] Completed 3719 Hyperglycaemia in theatre recovery In Progress Anaesthesia & Critical Care & Theatres – Critical Care Services 537 Potential Donor Audit (PDA) Ongoing Project 3365 Stress ulcer prophylaxis on discharge from ITU, appropriate or inappropriate? Completed 3400 Delayed and out of hours discharges from ITU In Progress 3445 Are packed red cell transfusions on intensive care compliant with BCSH guidelines in non-bleeding patients Abandoned Anaesthesia & Critical Care & Theatres – Theatres 3719 Hyperglycaemia in theatre recovery In Progress Dental Services 3313 Are Cone Beam Computerised Tomography (CBCT) scans using the smallest volume necessary to answer the clinical question? Completed 3424 Local anaesthetic written prescriptions referred to the school of hygiene Completed Dental Services/Oral & Maxillofacial 2879 Identification and management of bisphosphonate therapy patients presenting to the oral and maxillofacial surgery department [related to 2750] Abandoned 3077 Maxillofacial trauma referrals Deferred 3330 Quality of radiographs received with Oral Surgery referrals Completed 3366 Incidence of inferior dental/ lingual nerve sensory damage post mandibular third molar extractions In Progress 3387 Information given to patients taking Bisphosphonates about Bisphosphonate Related Osteonecrosis of the Jaw (BRONJ) Completed 3675 An audit to assess the success rate of surgical endodontics (apicectomy) within the oral surgery department In Progress 3713 Quality of clinical coding in oral and maxillofacial surgery In Progress 3717 Oral & Maxillofacial Trauma - audit of timescales for emergency treatment In Progress Dental Services/Oral Medicine 2850 How effective are our glycerol blocks in achieving pain control in trigeminal neuralgia? Abandoned 3317 Histopathological Diagnosis in Oral Medicine [re-audit] In Progress 3595 Quality of Clinical Information on Biopsy Request Forms In Progress Clinical Audit Annual Report 2013/14 Page 33 Dental Services/Orthodontics 3157 Management of orthodontic patients with a history of dental trauma to incisor teeth In Progress 3226 Lost orthodontic appliances [re-audit] Completed 3248 New patient referrals to the orthodontic department. Completed 3607 Undiagnosed caries in patients referred for Orthodontic treatment Completed 3623 Photography consent and photographic quality in the orthodontic department Completed Dental Services/Paediatric Dentistry 3155 Quality of record-keeping for paediatric dental trauma patients Completed 3331 Extraction of first permanent molars of poor prognosis in children [re-audit of 2545] Completed 3357 Fluoride: are we following the national guidelines? [re-audit of 2430] In Progress 3386 Users’ views of the paediatric dental clinic [re-audit of 2263] Completed 3481 Patient satisfaction with paediatric general anaesthetic services for dental treatment Deferred Dental Services / Restorative Dentistry 2773 Endodontic referrals received at Bristol Dental Hospital Completed 3082 Quality of life of patients with total prostheses before and after treatment with conventional dentures in Bristol Dental Hospital In Progress 3163 Patient satisfaction of Dental GA care pathway for Special Care patients In Progress 3224 Dental implant treatment at Bristol Dental Hospital In Progress 3292 Are radiographs utilised on new patient periodontal clinics appropriate to aid periodontal diagnosis? In Progress 3341 Prescriptions, special trays and wax rims for complete denture construction [re-audit of 3147] Completed 3420 Head and Neck Cancer: Is radiotherapy being delayed by dental screening and subsequent extractions? In Progress 3430 Restorative undergraduate treatment plans In Progress 3431 Implant-retained over-denture complications at Bristol Dental Hospital Completed 3459 Quality of dental screening and DPT fluoride prescriptions in the management of head and neck oncology patients In Progress 3529 Caries prevention regimes given to head and neck oncology patients following oncological therapy Deferred 3555 Radiographs taken by Undergraduates carrying out Endodontics Completed 3661 The quality of Endodontic referral radiographs received at the Bristol Dental Hospital In Progress 3680 Denture care for inpatients In Progress Ophthalmology / General 2893 Post-cataract endophthalmitis rate at Bristol Eye Hospital 2005 to 2010 [re-audit of 1125] Completed 3364 Clinical coding of oculoplastic and vitreoretinal procedures In Progress Ophthalmology / A&E and Primary Care 3165 Record-keeping for child casualty patients at BEH [re-audit of 2836] In Progress Ophthalmology / Cornea & Cataracts 2872 Ocular biometry [re-audit of 2362] In Progress 3072 Incidence and causes for 2 lines of Snellen Visual Acuity loss following phacoemulsification and intraocular lens implantation [re-audit of 2001] Abandoned 3181 Descemet’s Stripping Automated Endothelial Keratoplasty (DSAEK): Visual Acuity outcomes and Complications In Progress 3388 Boston Type 1 Keratoprosthesis - initial outcomes report to Clinical Effectiveness Group Completed 3423 Cataract outcomes 2012 [re-audit of 3195] Completed 3703 Re-audit of microbial keratitis at Bristol Eye Hospital In Progress 3718 Cataract outcomes audit 2013 [re-audit of 3423] In Progress Clinical Audit Annual Report 2013/14 Page 34 Ophthalmology / Glaucoma & Shared Care 3011 Blindness in glaucoma patients Completed 3302 Glaucoma outpatient follow up appointments at Bristol Eye Hospital [re-audit 2012] In Progress 3390 Deep Sclerectomy (non-penetrating glaucoma filtration surgery) Completed Ophthalmology / Medical & Surgical Retina 2829 Management of non-ischaemic Central Retinal Vein Occlusion (CRVO) at Bristol Eye Hospital [re-audit of 1917] Completed 3160 Time frame of patients’ journey in Age Related Macular Degeneration (AMD) service Completed 3418 Maculopathy Referrals from Bristol and Weston Diabetic Eye Screening Programme In Progress 3417 Referral and Treatment Times for patients with suspected Proliferative Retinopathy In Progress Ophthalmology / Orthoptics & Optometry 3235 Orthoptic new case referrals Completed 3287 Reception vision screening In Progress Ophthalmology / Paediatrics, Oculoplastics & Squint 2313 Adult Squint Surgery Outcomes In Progress 2925 Referrals from Paediatric Rheumatology of children diagnosed with Juvenile Idiopathic Arthritis to the Eye Hospital for Completed uveitis screening Impact of neuro-ophthalmic disorders on the Bristol Eye Hospital paediatric service Completed 3010 Paediatric Eye surgery service: parental and patient satisfaction. Deferred 3161 Basal Cell Carcinoma patient consultation and treatment times in the oculoplastics department In Progress 3179 External dacryocystorhinostomy audit [re-audit of 2312] Deferred 3229 Surgical Outcome of Correction of Exotropia in Children In Progress 3288 Nurse-Led Botox treatment for Blepharospasm, Hemi facial spasm and entropion at Bristol Eye Hospital. Completed 2838 Adult Surgical Specialties 3236 Streamlining discharge in Elective Surgery: An Audit of Criteria Led Discharge In Progress 3343 Is Foundation doctors’ understanding of IV fluid prescribing adequate? In Progress 3371 Surgical Ward Rounds in the BRI: When, who and how often? In Progress 3415 Are we following UH Bristol guidelines for gentamicin prescribing in adults? In Progress Adult Surgical Specialties / Lower GI Surgery 3227 Reversal of ileostomies Completed 3342 Are we following the NCEPOD recommendations for emergency surgery in Octogenarians? In Progress 3383 Re-admission to hospital of patients waiting for surgery on "hot gall bladder" laparascopic cholycystectomy waiting list In Progress Adult Surgical Specialties / Orthopaedics (T&O) 2592 Health Protection Agency - Surgical Site Infection Surveillance Ongoing 2908 Audit of acute pain management for hip fracture patients Completed 3397 Daycase Hand Surgery at South Bristol Community Hospital: cancellations and patient experience In Progress Adult Surgical Specialties / Thoracic Surgery 3280 Thoracic Surgery lobectomy patients – why are patients staying longer than 5 days in hospital? In Progress Adult Surgical Specialties / Upper GI Surgery 2817 Audit on the Management of Acute Pancreatitis Completed 2852 Pre-Operative Emergency Patient Audit (PEPA) Completed 2904 Evaluating the use of PET/CT (Positron Emission Tomography/Computed Tomography) in the staging of Oesophageal Cancer In Progress Adult Surgical Specialties / Vascular Surgery 2680 Can pre-operative Carotid Duplex screening reduce the risk of stroke following cardiac bypass? Clinical Audit Annual Report 2013/14 In progress Page 35 The following section summarises the changes, benefits or actions introduced as a result of completed audits within the Division/specialties. 3125 This audit demonstrated high accuracy of procedure coding by Clinical Coding staff for patients undergoing ENT surgical procedures. 3278 Following this audit of sepoplasty it was decided that an increased number of day case operations was needed to reach target. This will be done by changing to morning operations and providing more open appointments. It was also agreed that further work was needed to better understand reasoning behind post op bleed/unwell patients after surgery 3469 This re-audit demonstrated significant improvement in antibiotic prescribing within ENT practice. 3474 This audit of ENT Outpatient procedures coding resulted in the re-design of the outpatient outcome form to make this clearer for staff to complete and to assist correct charging for outpatient procedures 3657 This audit led to the creation of a new departmental policy for infectious mononucleosis screening for tonsillitis. This should result in a cost saving from targeting infectious mononucleosis screening more effectively. 3449 A new chart with an expanded pre-operative section has been introduced throughout clinical areas as a result of this audit. 3517 Following this audit of anaesthetic machine checks it was decided to update the Trust’s guidance on levels for machine alarms (as advised by the Association of Anaesthetists of Great Britain and Ireland). The Medical Equipment Management Organisation service now checks with the Department of Anaesthesia to ensure that individual levels are set rather than the manufacturer defaults. 3666 Guidelines have been revised as a result of this audit into analgesia prescribing in acute medical and surgical admissions with renal impairment. 3422 The audit has led to updated referral criteria being developed for the Pain Management Programme, more in line with Pain Society guidance. These have been widely cascaded and are expected to lead to more efficient use of clinical resources. 3457 This audit demonstrated good compliance with recommendations for the use of regional anaesthesia (RA) during caesarean section and rates of conversion from regional to general anaesthetic during the procedure, indicating that pain was well controlled by RA for the majority of patients. 3643 This audit demonstrated high patient satisfaction with pain-relief provided following a caesarean section, as well as clinical best practice in prescription of non-steroidal anti-Inflammatory drugs. 3313 This audit was used as evidence to support a business proposal for purchasing a small volume Cone Beam CT machines for Bristol Dental Hospital. 3424 This audit of local anaesthetic written prescriptions referred to the school of hygiene led to the development of a local policy to help standardise practice. 3330 The referral proformas for oral surgery patients have been redesigned as a result of this audit to help improve the quality of radiographs received. 3387 Following this audit of information given to patients taking Bisphosphonates about Bisphosphonate Related Osteonecrosis of the Jaw (BRONJ), it was agreed that a revised patient leaflet should be implemented. Posters have been developed for use in the oral surgery department detailing the key points of information about BRONJ that must be relayed to the appropriate patients. 3226 To improve the service, the laboratory work card has been re-designed to include a check box to determine whether new or remake orthodontic appliances are required. 3248 New orthodontic department guidelines outlining referral criteria have been introduced as a result of this audit. It was also agreed with the oncology department to produce a similar patient information leaflet to hand out to relevant patients in new patient oncology clinics. 3607 This audit confirmed good practice in treatment of undiagnosed caries in patients referred for orthodontic treatment. General Dental Practitioners have been further educated in the form of helpful reply letters with feedback and referral guidelines with re-referrals. 3623 Following this audit of photography consent and photographic quality in the orthodontic department, it was agreed that a single universal site should be available to store start and end photographs. 3155 As a result of this audit, the trauma form has been re-designed to help improve the quality of record-keeping for paediatric dental trauma patients. A re-audit is currently underway. 3331 This re-audit demonstrated improvements in practice for children having tooth extractions of first permanent molars of poor prognosis. Further awareness of standards was highlighted through presentations. 3386 As a result of this audit into the user views of paediatric dental clinics, a new clinic flow sheet has been introduced to provide more information to patients. Clinical Audit Annual Report 2013/14 Page 36 2773 This audit of endodontic referrals received at Bristol Dental Hospital demonstrated good adherence to standards. 3341 This re-audit of prescriptions, special trays and wax rims for complete denture construction has led to the agreement of criteria for the production of special trays and wax rims. Results have been disseminated and the prosthetics laboratory management will hold training session in order to encourage good practice. 3431 This audit demonstrated that implant-retained over-denture complications at Bristol Dental Hospital were within agreed rates. 3365 This audit has led to the creation of new local guidelines for the management of patients prescribed stress ulcer prophylaxis on ITU. 3364 This audit demonstrated good practice in the clinical coding of oculoplastic and vitreoretinal procedures. 3388 The results of this audit of a new interventional procedure agreed by the Trust (Boston Type 1 Keratoprosthesis) demonstrated that outcomes were within published guidance. 3423 This annual audit of cataract outcomes demonstrated good practice against nationally benchmarked outcome data. 3011 This audit demonstrated that the management of blindness in glaucoma patients was being treated appropriately. 3390 This audit confirmed that patients undergoing Deep Sclerectomy (non-penetrating glaucoma filtration surgery) were being treated appropriately. 3417 This audit identified the need for improvements in referral and treatment times for patients with suspected Proliferative Retinopathy. Local retinopathy guidelines have been re-written and re-audit planned. 3418 This audit identified the need for improvements in referral and treatment times for patients with suspected Proliferative Retinopathy. Local retinopathy guidelines have been re-written and re-audit planned 3287 The Trust has changed from the use of the Snellen to logMAR vision test as a result of this his audit of reception vision screening. 3010 This audit of the paediatric eye surgery service demonstrated good levels of parental and patient satisfaction. 3391 As a result of this audit into non-accidental Head Injury in children (ophthalmological review), guidelines were created for the referral to a Paediatric Ophthalmologist where concern exists. It was also agreed that the proforma available from the Royal College of Paediatrics and Child Health and The Royal College of Ophthalmologists for accurate description and documentation of clinical history and findings should be adopted. 3626 This audit of compliance with hand hygiene guidance on Ward 2 led to the design a more up to date poster as a visual prompt to hand hygiene on entry to and exit from the ward. Posters will be more strategically placed near the swipe card access points and the dispensers themselves. It was also decided to re-locate the shelf much nearer the hand gel dispenser so that it may fulfil its initial purpose. 3415 This audit of gentamicin prescribing led to the re-design of the current drug chart and the identification and implantation of further nurse training. Clinical Audit Annual Report 2013/14 Page 37 WOMEN’S AND CHILDREN'S 3.5 The following chart shows the status at year end of those projects identified as priorities for audit as part of the forward planning process in 2013/14. Full details of the status of individual projects on this plan can be found within table 1 of this section. Progress of planned projects Complete 100% 80% 60% 40% 20% 0% In progress Not started 4 4 7 4 7 19 1 1 3 2 3 2 2 9 2 1 2 3 Children's Services Women's Services Prioritisation category The chart below shows the status at year end of all registered projects (excluding those classified as ongoing monitoring). Some projects will have started and finished within the financial year, some will have been started but have yet to complete and are therefore rolled over. The figures also include projects that commenced in previous years but have now been abandoned, those that previously commenced but were completed in 2013/14 and those previously commenced but not completed by the end of 2013/14. Individual project status at year end 40 35 32 30 17 20 12 11 10 13 11 6 10 2 1 0 Children's Services Women's Services New in year/Completed New in Year/Roll-over Rolled-over/Abandoned Rolled-over/Completed Rolled-over/Deferred Rolled-over/Roll-over Percentage of projects registered before start 100% 80% Make up of project team 100% 24 80% 24 3 28 60% 60% 40% 40% 20% 55 7 20% 80 41 0% 42 42 Children's Services Women's Services 0% Children's Services TRUE Clinical Audit Annual Report 2013/14 Women's Services FALSE Multi-professional Multi-specialty Neither Page 38 Percentage National Audit Percentage re-audit 100% 100% 80% 80% 60% 60% 40% 36 40% 95 65 9 4 Children's Services Women's Services 20% 0% 86 20% TRUE 18 33 Children's Services Women's Services 0% FALSE TRUE FALSE Guidance/stand type audited 60 49 50 40 30 20 24 25 20 19 11 15 10 10 0 Children's Services Women's Services NICE Other National Local Percentage report produced Unclassified Percentage action plan produced 100% 100% 15 80% 1 1 1 80% 8 60% 60% 40% 40% 20% 20% 37 17 0% 50 24 Children's Services Women's Services 0% Children's Services TRUE Women's Services FALSE Yes No - Confirmed good practice No Table 1 Title Sub-Specialty Lead Congenital heart disease (CHD) Cardiac Surgery Andrew Parry National Diabetes Audit (NDA) Priority Start date Status Q4 1 Q1 In progress Diabetes & Endocrinology Christine Burren 1 Q2 In progress National Inflammatory Bowel Disease audit Gastroenterology Christine Spray 1 Q1 In progress Paediatric Intensive Care (PICANet) Intensive Care Peter Davis 1 Q1 In progress Renal Registry (UKRR) Nephrology Carol Inward 1 Q2 In progress Epilepsy 12 (Childhood Epilepsy) Neurology Phil Jardine 1 Q1 In progress Clinical Audit Annual Report 2013/14 Page 39 National Neonatal Audit Project Neonatal Intensive Care Pam Cairns 1 Q1 In progress Vermont-Oxford Benchmarking Project Neonatal Intensive Care David Harding 2 Q1 In progress Audit of Anaesthetic Record Keeping (to include detailed audit of documentation of consent process) Anaesthesia Gail Lawes 3 Q2 In progress Audit of the provision of Anaesthetic Preoperative Information Anaesthesia Steve Sale 3 Q2 In progress Re-audit of Antibiotic Policy Compliance Audit Anaesthesia Bev Guard 3 Q2 Completed Cochlear Implants Audiology Liz Midgley 1 Q1 In progress Hospital passport Cross Hospital Sara Palmer 2 Q3 Not started Audit of growth monitoring practice Endocrinology Liz Crowne 1 Q1 Complete An audit of the physical and psychological management of selfharm in the emergency department Emergency Department Lisa Goldsworthy 3 Q1 In progress Audit of paediatric asthma management Emergency Department Nick Sargant 1 Q1 Completed Consultant sign off for febrile children < 1 year old in the ED Emergency Department Mark Lyttle 1 Q1 In progress An audit of the Management of Head Injury in the Children’s Emergency Department Emergency Department Mark Lyttle 3 Q1 In progress An audit of the Management of Children in the Children’s Emergency Department with Suspected Urinary Tract Infection Emergency Department Will Christian 3 Q2 In progress Neonatal resuscitation Neonatology Ward Managers 2 Q3 Not started Immediate Care of the Newborn (Joint project with Obstetrics and Midwifery) Neonatology Jackie Moxham/ Anoo Jain 2 Q1 Not started Newborn feeding (Joint project with NICU) Neonatology Joan Beales 2 Q1 In progress Examination of the Newborn (joint project with Obstetrics and Midwifery) Neonatology Wendy Ring/Anoo Jain 2 Q3 In progress Support for Parents (Joint project with Obstetrics and Midwifery) Neonatology Jackie Moxham/ Anoo Jain 2 Q2 Completed Anaemia in Chronic Kidney Disease 3b to 5 Nephrology Moin Saleem 3 Q2 Not started Dialysis Access Complications Nephrology Jane Tizzard 3 Q2 In progress Care of patients on Dialysis Nephrology Jan Dudley 3 Q2 In progress Management of Renal Bone Disease Nephrology Martin Mraz 3 Q2 Not started Prescription of Dialysis Line Locks Nephrology Rebekah Rogers 3 Q2 Not started Vancomycin – monitoring and dose adjustment Pharmacy Jenny Haylor 2 Q3 In progress Patient administration and compliance issues when prescribed Proton Pump Inhibitors Pharmacy Nicola Singh 2 Q3 Not started Accurate CRIS documentation of consultant checks Radiology David Grier 3 Q3 Not started Genetic Haemoglobinopathy screening (re-audit) Clinical Genetics Jessica Bailey 3 Q3 In progress Key identifiers in dictation Clinical Genetics Ingrid Scurr 3 Q1 In progress Case note peer review Clinical Genetics Alan Donaldson 3 Q3 Not started West of Britain Group joint audit – probably Lynch syndrome screening Clinical Genetics Alan Donaldson 3 Q3 Not started Total Laparoscopic Hysterectomy (TLH) Gynaecology Caroline Overton 2 Q3 In progress Clinical Audit Annual Report 2013/14 Page 40 Swab management on CDS / Handover to Theatres Obstetrics/Midwifery Bryony Strachan/ Emma Treloar 2 Q3 In progress Care of Women in Labour Obstetrics Emma Treloar/ Belinda Cox 2 Q1 In progress Intermittent Auscultation Obstetrics/Midwifery Emma Treloar/ Belinda Cox 2 Q1 In progress Continuous Electronic Fetal Monitoring Obstetrics/Midwifery Emma Treloar/ Belinda Cox 2 Q1 In progress Fetal Blood Sampling Obstetrics/Midwifery Emma Treloar/ Belinda Cox 2 Q1 In progress Use of Oxytocin Obstetrics/Midwifery Emma Treloar/ Belinda Cox 2 Q1 In progress Caesarean Section Obstetrics/Midwifery Emma Treloar/ Belinda Cox 2 Q1 In progress Induction of Labour Obstetrics/Midwifery Emma Treloar/ Belinda Cox 2 Q2 Complete Severely Ill Women Obstetrics/Midwifery Emma Treloar/ Belinda Cox 2 Q1 Complete High Dependency Care Obstetrics/Midwifery Emma Treloar/ Belinda Cox 2 Q1 In progress Vaginal Birth after Caesarean Section Obstetrics/Midwifery Emma Treloar/ Belinda Cox 2 Q1 In progress Operative Vaginal Delivery Obstetrics/Midwifery Rachna Bahl/Lisa Damsell 2 Q1 In progress Multiple Pregnancy and Birth Obstetrics/Midwifery Rachna Bahl/Lisa Damsell 2 Q4 In progress Perineal Trauma Obstetrics/Midwifery Rachna Bahl/Lisa Damsell 2 Q3 In progress Shoulder Dystocia Obstetrics/Midwifery Rachna Bahl/Lisa Damsell 2 Q1 In progress Obstetric Haemorrhage Obstetrics/Midwifery Rachna Bahl/Lisa Damsell 2 Q1 In progress Pre-existing Diabetes Obstetrics/Midwifery Rachna Bahl/Lisa Damsell 2 Q3 Not started Obesity Obstetrics/Midwifery Rachna Bahl/ SJ Sheldon 2 Q1 Not started Mental Health Obstetrics/Midwifery SJ Sheldon/ Rachel Liebling 2 Q3 In progress Handover of Care (Onsite) Obstetrics/Midwifery Sarah-Jane Sheldon 2 Q1 In progress Non-Obstetric Emergency Care Obstetrics/Midwifery Rachna Bahl/Lisa Damsell 2 Q3 Not started Neonatal resuscitation Obstetrics/Midwifery Ward Managers/ CDS WP 2 Q3 Not started Immediate Care of the Newborn (Joint project with NICU) Obstetrics/Midwifery Jackie Moxham/ Anoo Jain 2 Q1 Not started Newborn feeding (Joint project with NICU) Obstetrics/Midwifery Joan Beales 2 Q3 In progress Examination of the Newborn (Joint project with NICU) Obstetrics/Midwifery Wendy Ring/Anoo Jain 2 Q3 Not started Bladder Care Obstetrics/Midwifery Jackie Moxham 2 Q3 In progress Support for Parents (Joint project with NICU) Obstetrics/Midwifery Jackie Moxham/ Anoo Jain 2 Q2 Complete Recovery Obstetrics/Midwifery Claire Dowse 2 Q1 Not started Clinical Audit Annual Report 2013/14 Page 41 The following activity was also in progress during the financial year (either rolled over from previous year or not identified through plan): Ref Title of Project Status Children’s Services/Anaesthesia 2746 Audit of compliance with antibiotic guidelines for surgery Completed 2822 Administration of sedative premedication to children Completed 3098 BRCH PONV and Pain Management up to 6 hours post day surgery with next day Telephone follow up In Progress 3250 Pre op fasting in children undergoing surgery in the BRHC In Progress 3409 Re-audit of compliance with antibiotic guidelines for surgery with particular reference to antibiotic prophylaxis in theatre In Progress 3410 Audit of Anaesthetic Record Keeping In Progress Children’s Services/Cardiac Services 3202 Re-audit of anti-coagulation therapy for children in Cardiac Services In Progress 3208 Quality and interprebility of faxed ECGs In Progress 3246 Perioperative management of Blalock-Tausig Shunt audit In Progress 3380 3408 Follow up and complications associated with aortic valvuloplasty via axillary cut-down for critical aortic stenosis in neonates An audit of the management of children with respiratory synctial virus who are undergoing cardiopulmonary bypass surgery for Chronic Heart Disease In Progress In Progress Children’s Services/Dietetics 2966 Meeting nutritional needs, standards and quality of care in paediatrics: Outcome 5 compliance In Progress 3105 Paediatric Dietetic input for Paediatric Diabetes Completed Children’s Services/Emergency Department 3029 The College of Emergency Medicine Consultant Sign Off Audit Completed 3106 Audit of antimicrobial prescribing practice on the children's ward following presentation to the Children's Emergency Department Completed 3117 Management of non-blanching rashes presenting to the Children's Emergency Department Completed 3221 Observations in the paediatric Emergency Department Completed 3222 Improving adolescent care in the paediatric Emergency Department Completed 3243 Nasal ciliary brushings in the management of primary ciliary dyskinesia In Progress 3320 Handover from the paediatric Emergency Department to BRHC wards In Progress 3376 Management of non-bleaching rash in the paediatric Emergency Department In Progress 3379 Paediatric sedation in the ED In Progress 3393 College of Emergency Medicine - consultant sign off In Progress Children’s Services/Paediatric Endocrinology 2818 Audit of insulin tolerance tests performed on the clinical investigation unit at Bristol Royal Hospital for Children Completed 3296 Diabetic Ketoacidosis in accordance with the Southwest Paediatric Diabetes Regional Network Integrated Care Pathway guidelines from 2007-2012. In Progress Children’s Services/Gastroenterology 2490 United Kingdom National Inflammatory Bowel Disease Audit In Progress 3377 Infliximab and Adalimumab use in children with crohns disease In Progress Children’s Services/Paediatric Intensive Care 72 Regional Audit of Critical Care Outcomes (Audit of Critically Ill Children) Ongoing 2548 PICU Discharge delay audit 2010 In Progress 2639 Audit of the Documentation of Information & Clinical Observations on the Bristol Paediatric Observation Chart Completed 3392 Audit of resuscitation documentation at BRHC In Progress Clinical Audit Annual Report 2013/14 Page 42 Children’s Services/Paediatric Nephrology 2285 Retrospective audit of anaemia in paedatric patients with CKD stage 5 disease 2003- 7 In Progress 2745 Audit of dialysis access service and complications (01/01/09 - 30/06/10) In Progress 2924 Pre-Renal Transplantation immunization and investigations In Progress 2970 Urinary Tract Infection Audit of NICE guidance - Healthcare Quality Improvement Partnership (HQIP) In Progress 2988 Compliance with current guidelines for MRSA screening on the paediatric nephrology ward Completed 3002 Audit of patients with Stage 4 Chronic Kidney Disease (2010-11) In Progress 3385 Gentamicin prescribing in paediatrics In Progress 3402 Audit of Management of Hyperlipidaemia in Children with CKD Stage 4 & 5 In Progress 3403 Renal replacement therapy (dialysis) in children at the BRCH (2011/12) In Progress Children’s Services/Neurology 3398 Epilepsy12 - UK Collaborative audit of healthcare for children and young people with suspected epileptic seizures In Progress Children’s Services/Paediatric Oncology 2687 Audit of bone marrow transplant febrile neutropenia guidelines In Progress 3069 An audit of prescribing against NHSLA standards for BMT inpatients and outpatients In Progress 3359 Audit of paediatric sickle cell management In Progress 3370 Aseptic Non Touch Technique (ANTT) in IV practice 2012-13 In Progress Children’s Services/Paediatric Respiratory 2106 British Paediatric Respiratory Society / British Thoracic Society Asthma Audit In Progress 2434 Parental satisfaction in a nurse led paediatric clinic Completed 2769 Inpatient nebuliser adherence Completed Children’s Services/Paediatric Rheumatology 3045 3170 Management of community acquired pneumonia (CAP) in Bristol Royal Hospital for Children British Thoracic Society Guidelines Waiting times for patients listed for intra - articular joint injections for Juvenile Idiopathic Arthritis using BSPAR standards of care In Progress In Progress Children’s Services/Paediatric Surgery 3194 Audit of patients undergoing oesophagogastric dissociation surgery In Progress 3200 International, multicentre audit of outcomes following appendicectomy Completed 3318 Children who ‘did not attend’ (DNA) Paediatric General Surgery and Paediatric Urology outpatient clinic appointments In Progress Women’s Services/Gynaecology 3413 Key identifiers in dictation In Progress 231 The collection of regional gynaecological cancer for the purposes of audit and improvement of management Ongoing 1945 National audit of invasive cervical cancers Ongoing 2740 Documentation and information given following insertion of the Levonorgestrel Releasing Intrauterine System (Mirena IUS) Completed 3016 Continuous audit of laparoscopic hysterectomy Ongoing 3063 Management of ovarian cancer In Progress 3228 Management of patients at joint Gynaecology-Haematology Clinic Completed 3271 Hysteroscopy - mode of anaesthesia Completed 3272 Timing of misoprostol prior to transcervical surgical procedures in Gynaecology In Progress 3311 Colposcopy - treating to cure Completed 3316 Treatment standards in colposcopy for high grade disease Completed 3338 Senior house officer pre-operative ward round checks In Progress Clinical Audit Annual Report 2013/14 Page 43 Women’s Services/Obstetrics & Midwifery 633 Audit of blood usage on Central Delivery Suite Ongoing 1638 A series of audits of UNICEF UK Baby Friendly Initiative best practice standards Ongoing 2321 2730 National Screening Committee Audit Haemoglobinopathies, Infectious Diseases, Downs Screening and Newborn Blood spot - NICE CG 62 Re-audit of the implementation of Modified Obstetric Early Warning Score (MEOWS) charts at St Michael’s Hospital Delivery Suite (CNST 3.2.8) Ongoing Ongoing 2762 Pleuro-amniotic shunt for fetal pleural effusion (NICE IPG190) In Progress 2795 Perineal tear audit (CNST 3.3.5a) Ongoing 2801 Pregnancies in Women with Prosthetic Heart Valves and Therapeutic Anticoagulation 2007 – 2010 Completed 2802 Antenatal and Intrapartum management of very preterm labour Completed 2803 Bristol Stillbirth audit - continuous Ongoing 2833 HIV testing in Pregnancy (re-audit) Ongoing 2841 Management of Cardiac problems in pregnancy In Progress 2853 Compliance with procedures for swab, needle and instrument counts Ongoing 2927 Beta-blocker use in Cardiac Antenatal Patients Completed 2929 Re-audit of diagnosis and management of obstetric cholestasis Completed 2956 Emergency department admissions of pregnant women (CNST 3.4.10) Completed 2964 Induction of labour (CNST 3.2.7) Completed 3015 Management of operative vaginal delivery: including multiple instrument use and failed operative vaginal delivery (CNST 3.3.3) In Progress 3026 Re-audit of management of pre-existing diabetes – local standards Completed 3041 Re-audit of clinical risk assessment – Labour (CNST 3.4.7) In Progress 3064 Re-audit of prophylaxis in women with venous thromboembolism (CNST 3.3.8b) Completed 3090 Enhanced recovery in gynaecological surgery In Progress 3133 Complex twins seen in fetal medicine department In Progress 3134 TORCH screening at St Michael's Hospital Completed 3142 Management of women who deliver preterm In Progress 3149 Height of fundus measurement Completed 3212 Post natal bladder care Completed 3239 Intrapartum care for women with cardiac disease In Progress 3240 Midwife Examination of the Newborn re-audit Completed 3244 Compliance with Mulitple Pregnancy Guideline – NICE CG129 In Progress 3298 Induction of labour process - going beyond CNST In Progress 3299 Management of placenta accreta In Progress 3315 Maternity outlier alert for 'maternal non-elective readmissions' In Progress 3334 Appropriate use of fast bleep system for Caesarean section In Progress 3335 Labour ward staffing (CNST 3.1.6) Completed 3337 Gestational diabetes follow up fasting blood sugar- Re-audit In Progress 3350 Management of thrombocytopenia in pregnancy In Progress 3362 Management of newborn where group B streptococcus present in mother or baby – re-audit (CNST 3.5.4) Completed 3405 Post-caesarean section infection In Progress Clinical Audit Annual Report 2013/14 Page 44 The following section summarises the changes, benefits or actions introduced as a result of completed audits within the Division/specialties. 3203 Following this audit of management of croup at Bristol Royal Hospital for Children, the availability of patient information leaflets has been increased and further training to staff provided highlighting assessment of severity and acting appropriately. There has also been communication with GPs regarding the use of ambulances for moderate / severe croup. 3346 Following this audit of azathioprine prescribing in paediatric dermatology patients, the British Society of Paediatric Rheumatology patient information and advice regarding sun protection was introduced. 3368 Following this audit of smoking advice to parents of wheezy children, parent smoking status and advice fields are to be included on the wheeze proforma. 3549 Following this audit of compliance of intravenous fluid administration with local guidelines it was confirmed that the prescription guideline has been incorporated into the general paediatric induction programme. It was also agreed that nurses should be consulted on future re-audit, which should take into account amount of time patient is continuously on iv fluids. 3340 This audit resulted in a clarification of local guidelines for the treatment of neonates with heart murmur and improvements to referral proforma. 3570 This audit of charts - fluid and infusion prescription and recording in NICU highlighted the need for further training/teaching sessions. These are in the process of being arranged. 3604 This audit demonstrated good compliance in Neonatal Intensive Care with standards relating to prescription of gentamicin, independent checks of preparation and administration, and timeliness of administration. 3098 The results of this audit of management of pain and post-operative nausea and vomiting were very positive with the majority of audit standards met and overall satisfaction on the care, pain and post-operative nausea/vomiting management being reported as good to excellent. Parents frequently praised both medical and nursing staff for their care and diligence during their hospital experience. 3250 Following this audit of pre op fasting in children undergoing surgery, clear fluid intake is being encouraged in the period greater than two hours before operation start time. 3409 Following this re-audit of compliance with local antibiotic guidelines for surgery it was agreed that induction information for new juniors should include the need to document antibiotics on drug chart. The need to document "knife to skin" time and antibiotic prescribing is to be considered when re-designing anaesthetic charts. 3461 This audit determined that LMX is to remain 1st line topical local anaesthetic for cannulation in children’s theatres. The scope should be explored for keeping Ametop in stock for when cannulation / bloods are needed in < 1 hour. 3638 It was agreed that a local guideline should be introduced as a result of this audit of temperature control of paediatric patients in the peri-operative period. It was agreed that active warming should always be used from induction when anaesthetic time is prolonged, or if patient is high risk. 3208 Following this audit of quality and interprebility of faxed ECGs it was agreed to switch from faxed to scanned ECGs. 3246 Following this audit of perioperative management of Blalock-Tausig Shunt surgery it was agreed that a proforma checklist be introduced and a consensus view on use of pre-operative aspirin be pursued. 3247 Following this re-audit of anti-coagulation therapy for children in Cardiac Services, healthcare staff have been educated regarding warfarin guidelines and a warfarin handbook has been produced. 3408 Following this audit of the management of children with respiratory synctial virus undergoing cardiopulmonary bypass surgery for CHD it was agreed guidelines should be reviewed. 3506 Following this audit of Fetal Cardiology Screening and Diagnostic Service it was agreed trainees should be encouraged to record outcomes of neonatal echo and link them with maternal records for future audit purposes. This should be done for both normal and abnormal scans. Ways of linking outcome data of children with normal scans into HeartSuite (a local clinical database) should be explored. 3320 Following the audit of handover from the Children's Emergency Department to inpatient wards, a new "handover sheet" was introduced. 3379 Following this audit of paediatric sedation in the Emergency Department, a patient information leaflet for sedation has been produced. This includes a form for parents to sign, indicating that they have read the leaflet and understood it. 3428 Following this audit of compliance of management of severe asthma in children with national and local guidelines, local guidelines are being reviewed. Awareness of the Acute Asthma Management Guideline is being promoted in the Emergency Department and in General Paediatric teaching. 3460 Following this audit of the GP Phone Advice Service, information about the GP advice line has been added to the induction checklist in the Children's Emergency Department introductory handbook. Reminders and extra column have Clinical Audit Annual Report 2013/14 Page 45 been incorporated in the Telephone Log template. 3500 Following this audit of assessment and management of paediatric burns before referral to South West Children’s Burns Service, it was agreed a checklist should be developed with involvement of "Burns” team. 3501 Following this audit of time taken to reach decision to admit (and subsequent time to admission) in the Children's Emergency Department, it was recommended that a non-clinical nurse (or a nursing co-ordinator) role be introduced and that the scope for criteria led discharges be reviewed. 3182 Following this audit of vitamin D deficiency and management in children with type 1 Diabetes Mellitus, local guidelines were amended to include specific details of blood samples and quantities needed at point of diagnosis of type 1 diabetes. There was also liaison with biochemistry department to improve blood sampling practice. 3296 Following this audit of diabetic ketoacidosis versus the Southwest Paediatric Diabetes Regional Network guidelines, it was agreed patients admitted with Diabetic Ketoacidosis be managed in a designated HDU bed. Training is to be provided for HDU nurses in using the SW Integrated Care Pathway. This audit is to be presented at South-West Paediatric Diabetes Network meeting. 3373 This audit has led to the redesign of local records to allow for easier and more consistent recording of treatment and monitoring details, accessible to the wider clinical team. 3502 Following this audit of the transition between paediatric and adult endocrine services, a summary sheet has been developed to be used for each transitioning patient. A patient information booklet on the transition process is being developed and work is in progress with the special needs team to create a specific pathway for identified patients 3507 Following this audit of auxology screening carried out on the paediatric wards it was recommended that a working group be established to cascade auxology training. This training should outline that all children whose height is below the third percentile should be highlighted to medical staff (regardless of their weight) and that there should be clear guidelines to inform medical staff of further action if abnormal growth is identified. 3377 Following this audit of Infliximab and Adalimumab use in children with crohns disease it was agreed to introduce a checklist at end of the infliximab guideline to help record whether consent has been obtained, risks have been discussed and whether a history of TB has been taken. 3207 Following this audit of peritoneal dialysis in post-operative cardiac patients, a Peritoneal Dialysis Prescription and observation booklet which contains all the information necessary for a child receiving Peritoneal Dialysis has been introduced. 3394 Following this audit of red cell transfusion practice in paediatric intensive care it was recommended that education be provided to both medical and nursing staff as to guidelines for blood product transfusion. The guidelines are to be amended to include new units for measurement of Haemoglobin, from g/dl to g/l. 2745 The results of this audit of dialysis access service and complications were shared with the aim of stimulating good practice 2970 Following this audit of urinary tract infection, the local guideline has been amended to include questions regarding risk factors, and re-audit of one of criteria has been initiated. 3382 This audit of recombinant human growth hormone use in children with chronic kidney disease demonstrated high compliance with the majority of the standards. It was agreed attempts should continue to optimise nutritional and metabolic status prior to treatment. 3402 Following this audit of management of hyperlipidaemia in children with chronic kidney disease, it was agreed the possibility of programming the Proton System for reminders to check lipids should be investigated. Clinicians have been encouraged to monitor lipids regularly and it has been agreed that patients with low density lipoprotein levels above specified cut off be referred to a dietician for advice. 3527 Following this audit of care of patients undergoing renal transplantation at Bristol Royal Hospital for Children, feedback was provided to theatres that the 18 hour cold ischaemia times must not be exceeded. Information regarding the possible consequences of intraoperative hypotension was disseminated 2687 Following this audit of bone marrow transplant febrile neutropenia guidelines, it was recommended that teaching registrars regarding vancomycin and antibiotic use should be introduced. The audit results will be considered further when reviewing neutropenia guidelines. 3359 This audit of compliance of paediatric sickle cell management with national standards recommendations led to the creation of a standard immunisation letter to be sent to GP surgeries with the clinic letter. A copy will be given to the parent in clinic. 3441 This re-audit of non-operative reduction of intussusception showed good compliance with relevant standards and the best success rate in 20 years of audit. 3463 This audit of imaging the renal tract in children with urinary tract infection demonstrated good compliance with relevant standards. Results were presented to clinicians, highlighting NICE guidance and availability of Trust guidelines. Clinical Audit Annual Report 2013/14 Page 46 3479 This audit of radiology reporting times for paediatric inpatient and A+E plain films demonstrated good compliance of with Royal College of Radiologist’s guidance, increasing during the course of 2012/2013. 3603 Following this audit of cranial ultrasound scans performed on PICU for patients with congenital heart disease, it was agreed that arterial and venous doppler should be performed on cranial ultrasounds as a routine measure. The current PICU guidelines for cranial and renal ultrasound in congenital heart disease are to be reviewed. 3045 Following this audit of the management of community acquired pneumonia for children admitted to Bristol Royal Hospital for Children, further work was initiated to assess management in Paediatric Emergency Department 3243 Following this audit of nasal ciliary brushings in the management of primary ciliary dyskinesia it has been agreed that referral form data be copied into patient notes. 3395 This national audit of asthma management resulted in further education for ward staff regarding discharge planning, written information, inhaler technique and the need for asthma action plans & follow up. 3170 Following this audit of waiting times for patients listed for intra-articular joint injections for Juvenile Idiopathic Arthritis, more dates have been made available for general anaesthesia. A pathway is being formulated to establish any delays in listing patients for joint injections. 3150 Following this audit of management and outcomes of isolated preputial reconstruction in distal hypospadias, local consensus has been reached regarding the prescription of prophylactic antibiotics. 3201 Following this audit of antibiotic prescribing in appendicectomy at the Bristol Royal Hospital for Children, it was decided to continue with the changed antibiotic policy for children with perforated and/or gangrenous appendicitis. Results of this audit were presented at the British Association of Paediatric Surgeons 2013 conference. 3358 Following this audit of consent to examination or treatment in Children's Services, it was agreed and emphasised that abbreviations should not be used on consent forms. 3496 Following this audit of VTE prophylaxis (follow up of non-compliant cases), posters have been designed and put up around the department to promote awareness of prescribing appropriately. 3511 This rapid cycle audit demonstrated improvement over three audit cycles in the use of the agreed format for key identifiers when dictating letters in Clinical Genetics. 3338 This audit demonstrated considerable improvement in the documentation of pre-operative ward round checks by junior doctors in gynaecology patients. 3426 This audit led to the implementation of a standardised proforma to improve documentation and increased access to support from a psychologist for gynaecology patients with Vaginal Agenesis. 3429 This audit has led to further work to improve the treatment pathway for patients with vulval abscess, reducing the need for overnight stays and long waits prior to operations. 3438 This audit demonstrated good compliance with waiting time standards for suspected gynaecological cancers. 3531 This audit demonstrated substantial improvement in meeting National Screening Committee standards for timeliness of treatment for high grade disease in the Colposcopy department. 2762 Following this audit of pleuroamniotic shunt for fetal pleural effusion, it was decided that a dataset should be agreed to record key information for babies requiring pleuroamniotic shunts. 3142 This audit demonstrated good levels of compliance with appropriate use of the actim partus test and the prescribing of steroids for threatened pre-term labour. 3244 As a result of this audit, local guidelines were amended to follow NICE recommendations for multiple pregnancy and a patient information leaflet was developed as a result of this audit. 3299 As a result of this audit, a local guideline for cases of placenta accreta was produced. This guideline is based on recommendations from the Royal College of Obstetrics and Gynaecology. 3312 This audit led to the development and approval of a specific consent form for caesarean section, designed to include all aspects recommended in Royal College of Obstetrics and Gynaecology guidelines. The form also includes a list of preprinted risks and checks to help ensure that patients are aware these risks and have the opportunity to ask further questions. 3315 A range of changes were implemented to improve data quality as a result of this audit. Guidelines and patient information have been revised and patient pathways for maternal non-elective readmissions at St Michael's Hospital have been reviewed. 3334 This re-audit demonstrated that, where the new ‘Fast Bleep’ system was used, it was effective at helping staff to meet the 30 minute target from decision for Category 1 caesarean section to delivery. 3337 This audit demonstrated some improvement in proportion of women with gestational diabetes having some kind of diabetes test postnatally. Further work is underway to incorporate further testing information for GPs in electronic discharge summaries. 3405 This audit led to a wide-ranging campaign to improve clinical management of mild pyrexia during and after labour and to Clinical Audit Annual Report 2013/14 Page 47 cut sepsis including the production and audit of clear guidance on diagnosis and use of antibiotics in urinary tract infection 3464 As a result of this audit, changes have been made to the documentation for antenatal HIV screening of women to improve compliance with UK National Screening Committee standards. 3509 This audit has led to further service improvement work to increase capacity to manage patients with hyperemesis gravidarum as daycase patients rather than inpatients where appropriate. This will reduce pressures on beds on Ward 78 and improving patient experience. 3510 This audit demonstrated that women who attended the Day Assessment Unit (DAU) for their appointment at Term +10 days and who had a concerning finding were offered induction within one day, in accordance with NICE recommendations. Revisions were made to the DAU profoma to help improve documentation at these appointments in future. 3547 This audit demonstrated good support from midwives for parents of children with an unexpected poor outcome at birth. 3635 This audit demonstrated that referrals for medical review are being made where appropriate. 3275/ This audit/re-audit led to improvements in documentation of key information required to comply with Human 3477 Fertilisation and Embryology Act in the Reproductive Medicine department at St Michael's Hospital. Clinical Audit Annual Report 2013/14 Page 48 3.6 NON-DIVISION SPECIFIC Title Area Lead Priority Start date Status Q4 Audit of Staff Support and Being Open Policy (Duty of Candour) and follow up re-audit 6/12 later Trust Services Anne Reader 1 Q1 Completed Audit of Serious Incident Policy and Policy for the Management of Incidents and follow up re-audit 6/12 later Trust Services Anne Reader 1 Q1 In progress Audit of Policy for the Management of Incidents and follow up re-audit 6/12 later Trust Services Simon Harrison Boyle/Mel Fewkes 1 Q1 In progress Audit of VTE Policy and follow up re-audit 6/12 later Haematology Anne Reader/ Amanda Clarke 1 Q2 In progress Medicines Storage Pharmacy Steve Brown 2 Q4 Not started Inpatient prescribing audit Pharmacy Helen Badham 3 Q2 In progress South West Quality and Patient Safety Improvement Programme Nursing (General Ward) Anne Reader/ Catherine Hughes 2 Q1 In progress National Cardiac Arrest Audit (NCAA) Resuscitation Services Jo Bruce Jones 1 Q1 In progress Inpatient documentation audit Record Keeping Jane Luker 2 Q3 Completed Dementia Screening Nursing Natalie Godfrey 1 Q1 In progress Ward transfers for patients with cognitive impairment Nursing Natalie Godfrey 1 Q3 In progress Learning disabilities risk assessment/reasonable adjustments Nursing Lorna Hayes 2 Q3 In progress Patient Safety Thermometer Nursing Helen Morgan 1 Q1 In progress Ward based monthly monitoring work (EWS scores and other measures) Nursing Helen Morgan 2 Q2 In progress The following activity was also in progress during the financial year (either rolled over from previous year or not identified through plan): Status 2369 Provisional Title of Project Specialty Saving Lives – a programme to reduce healthcare associated infections Sub-Specialty The Prevention of Hospital Acquired Thrombosis [CQUIN target] 3323 Dementia screening (CQUIN) Completed Ref 1510 Ongoing project Abandoned The following section summarises the changes, benefits or actions introduced as a result of completed audits within the Division/specialties. 3724 This audit/re-audit of the Trust staff support and being open policy (duty of candour) led to changes to the Trust’s Root Cause Analysis template to better record whether staff are informing patients/families when incidents occur. Improvement in practice was demonstrated and further amendments to the template will be made. 2945 This Trust wide audit of medical record keeping showed that practice needs to be improved. A programme of ‘spot’ audits has been implemented. It was agreed that the audit methodology and the standards measured should be completely revised to focus on the key issues. These revisions are in line with standards outlined by the Royal College of Physicians ‘Generic Record Keeping’ guidance. 3095 As a result of this audit of dementia screening, guidelines have been developed to reflect the screening required to identify known dementia, delirium and possible dementia. Assessment labels for the confusion assessment method (CAM) to assess for delirium, Abbreviated Mental Test Score (AMTS) to provide baseline of cognitive function, and dementia case finding question to screen for a possible dementia have been developed and added to the Trusts EROS system. Work is underway to include the above assessments in clerking proformas and also to adapt e-discharge summary to capture / record dementia screening status at discharge. Clinical Audit Annual Report 2013/14 Page 49 Appendix A - UH Bristol Clinical Audit Staff (as at April 2014) Division Specialty Clinical Audit Facilitator Laboratory Medicine Dr Joya Pawade Medical Physics & Bioengineering agnostics & Therapy Isabella To Pharmacy Adult Therapies Isabella To Medical Specialties Trudy Gale Emergency Services Specialised Services Surgery & Head & Neck Mr Phil Quirk Mr Kevin Gibbs Usual contact is Head of Service Radiology Medicine Clinical Audit Convenor Dr John Hughes Dr Rachel Bradley Dr Anne Frampton Cardiac Services Isabella To Dr Richard Bateman Oncology & Haematology Trudy Gale Dr Charlie Comins Anaesthesia Dr Frances Forrest Critical Care Dr Dan Freshwater-Turner General Surgery Chrissie Gardner Trauma & Orthopaedics Mr Doug West Mr Steve Mitchell Dental Services & Maxillo-facial Surgery Mr Tony Brooke Ophthalmology Mr Derek Tole Adult ENT Ms Claire Langton-Hewer Obstetrics & Gynaecology Jonathan Penny Women & Children’s Neonatology Children’s Services Other staff Richard Hancock Ms Naomi Crouch Dr Will Christian Stuart Metcalfe Clinical Audit & Effectiveness Manager (1.0) James Osborne Michael Aldridge NICE Manager (1.0) Clinical Audit Clerk (0.8) Membership of the Clinical Audit Group Dr Anne Frampton (Chair) Stuart Metcalfe (Clinical Audit and Effectiveness Manager) Chris Swonnell (Head of Quality - Patient Experience and Clinical Effectiveness) James Osborne (NICE Manager) Clinical Audit Convenors - see above Clinical Audit Annual Report 2013/14 Page 50 Appendix B - Clinical Effectiveness & Outcomes Strategy Action Plan Objective Action Lead Timescale Measure of success Status 1.1 Relocate Clinical Audit Facilitators to Trust Headquarters and commence new remits as outlined/agreed through consultation Stuart Metcalfe, Clinical Audit & Effectiveness Manager May 2013 Positive feedback from CAET and Divisions (review due in December 2013) Completed Stuart Metcalfe, Clinical Audit & Effectiveness Manager May 2013 Appointment of new Clinical Audit Facilitator Completed Jon Penny, Clinical Audit Facilitator July 2013 Demonstrated reduction of database fields and time taken to register projects Completed Richard Hancock, Clinical Audit Facilitator August 2013 Re-issue of project documentation Completed Jon Penny, Clinical Audit Facilitator August 2013 Website updated/testing of links to documents Completed 2.4 Explore further options for database design with the Trust IM&T department Jon Penny, Clinical Audit Facilitator April 2014 Decision will be reached on whether to continue to use an MS access Completed database or alternative 3.1 Re-design/create an appropriate dashboard or register to provide a clear summary of participation in national clinical audit Stuart Metcalfe, Clinical Audit & Effectiveness Manager September 2013 Evidence of regular receipt of (previously revised revised dashboard/register at to February 2013) Clinical Audit Group (CAG) 1. To re-structure the Clinical Audit & Effectiveness Team 1.2 Appoint to vacant Clinical Audit Facilitator post (CAET) (Medicine/Oncology) 2.1 Rationalise content of clinical audit database to eliminate unnecessary data fields and expedite speed of project registration 2. To improve the efficiency of the 2.2 Re-design clinical audit project documentation registration/ reporting process of 2.3 Update website (external/internal) with new clinical audit documentation links projects 3. To ensure that the results from national clinical audits are reported and acted upon appropriately Completed Comment: Project database re-designed and national audit register report created. Ongoing development will continue as necessary. 3.2 Improve the process of cascading national clinical audit reports to clinical leads upon publication, requesting that summary outcomes and actions are developed Stuart Metcalfe, Clinical Audit & Effectiveness Manager April 2014 (revised completion date June 2014) Responses to national clinical reports will be received by CAG within six months of publication, with exceptions reported to Clinical Quality Group In progress Comment: The paper based summary form has been re-designed. There has been an improvement in the number of national audit summaries received reviewed by CAG (six over the last two meetings). A KPI as outlined above will be added to the register for June CAG meeting and reported thereafter. Clinical Audit Annual Report 2013/14 Page 51 4.1 Consult as to how to improve process and relevance of annual forward programme Stuart Metcalfe, Clinical Audit & Effectiveness Manager September 2013 Process reviewed and agreed by Clinical Audit Group, introduced to coincide with timetable for development of Divisional quality objectives and Operating Plans Completed 4. To review system Comment: Amended process for agreeing the annual forward plan agreed with CAG and CQG. Consultation period extended until May 2014 to better ensure for planning annual that Divisional/Corporate clinical audit objectives are included clinical audit Process reviewed and agreed by programme Stuart Metcalfe, Clinical November 2013 Clinical Audit Group, introduced to 4.2 Introduce updated forward planning process Audit & Effectiveness (previously revised coincide with timetable for Completed Manager to January 2014) development of Divisional quality objectives and Operating Plans Comment: Final plan to go to CAG in June, then CQG in July 5.1 Agree participation in the Foundation Doctor and core medical trainee training programmes and agree delivery with CAET 5.2 Review and update current training materials where required and re-launch clinical audit workshop 5. To review, refresh and re-launch clinical audit training Stuart Metcalfe, Clinical Audit & Effectiveness Manager September 2013 Jon Penny, Clinical Audit Facilitator November 2013 (revised completion date September 2014) Participation in programme Completed Re-launch of workshop In progress Comment: Workshop slides partially reviewed. Member of the CA&E Team attending a ‘Train the Trainer’ workshop in June 2014 provided by HQIP to further review local content against this training. 5.3 Explore alternative options for training delivery (including eLearning and condensed delivery) Chrissie Gardner, Clinical Audit Facilitator January 2014 (revised completion date January 2015) Clarification of options and decision made as to alternative training options In progress Comment: Member of the CA&E Team attending a ‘Train the Trainer’ workshop provided by HQIP to further review. We will use the re-introduction of the workshops to help determine other delivery options. Links to HQIP elearning and other training guides will be available via nternal and external websites by the end of June 2015 6. To ensure divisional scrutiny of ‘outcomes and actions’ reports following completion of clinical audit projects 6.1 Clarify current lines of reporting and enhance arrangements if and where required Stuart Metcalfe, Clinical Audit & Effectiveness Manager / Divisions July 2013 (revised completion date August 2014) Documented evidence of appropriate divisional scrutiny of outcomes and actions reports In progress Comment: Standard Divisional/specialty reports created (status of projects in progress/outcome and actions and outstanding actions from completed projects). Reports well received in Divisions of Medicine and Surgery. Outcomes and actions already reviewed by Children’s Governance Group. Clinical Audit Annual Report 2013/14 Page 52 Appendix C - Progress against Clinical Audit Forward Programme 2013/14 226 projects on the plan were due to have commenced by the end of the financial year. The Table below shows that overall, 152 (67%) of these projects commenced as planned. Critically, 47 out of 50 (94%) Priority 1 projects had either commenced or been completed. Two national audits identified as part of the 2013/14 planning process had been due to commence during the year but have subsequently been withdrawn at national level. The Trust did not participate in one project, an audit of patient information and consent (Blood and Transplant audit programme) due to organisation issues at NHSBT. It should be noted that although this project was listed as P1, it is not part of the mandatory National Clinical Audit & Patient Outcome Programme (NCAPOP) and no penalty applies for nonparticipation. Division Priority P1 Status (Q4) Complete In progress Not started P1 Total P2 P2 Total P3 3 Total 4 Complete In progress Not started Complete In progress Not started Complete In progress Not started 4 Total Total D&T Spec 1 7 SHN 1 10 W&C 2 9 NDS 1 7 2 2 5 12 5 22 2 4 3 9 Med 2 7 1 10 3 8 2 13 2 4 14 20 8 4 11 1 8 7 16 1 11 4 23 11 38 1 9 6 16 8 1 3 1 5 2 1 3 36 43 15 65 14 % projects commenced to planned timescale 3 7 P1 94% 7 8 4 3 11 18 53 P2 71% P3 44% Total 7 40 3 50 18 54 29 101 6 18 30 54 4 5 12 21 226 1 1 P4 42% All 67% The graph below shows the overall percentage of projects commenced to timescale. Figures for the previous year’s plan have been included as a comparator. Priority P1 P2 P3 P4 Overall % commenced to timescale 11% (83% in 2012/13 to 94% in 2013/14) 10% (61% in 2012/13 to 71% in 2013/14) No change (44% in 2012/13 and 44% in 2013/14) 25% (17% in 2012/13 to 42% in 2013/14) 7% (60% in 2012/13 to 67% in 2013/14) Clinical Audit Annual Report 2013/14 Page 53 The graphs below show planned activity (i.e. the number of projects due to have started) against actual activity (the number of projects in progress or complete) per quarter over the full year. Planned and actual trajectories for all activity and for those projects categorised as priority 1 and 2 are also plotted. Clinical Audit Annual Report 2013/14 Page 54 Appendix D - University Hospitals Bristol Clinical Audit Forward Programme 2014/15 All the projects within the programme have been identified through consultation as priorities for the Trust. This is not an exhaustive list of clinical audit activity that will take place throughout 2014/15; other projects may be facilitated by the Clinical Audit & Effectiveness Team over the year according to on-going priorities and available resources. Each of the audits in the programme has been listed according to the categories below. These are based on priority areas for clinical audit as outlined within the Healthcare Quality Improvement Partnerships (HQIP) ‘Clinical Audit Programme Guidance’. Priority 1 Priority 2 Failure to deliver on these externally driven audits may carry a penalty for the Trust (either financial or in the form of a failed target or non-compliance with standards). Audits within this section relate to or support the following priorities: Many of these audit projects emanate from Trust governance issues or high profile local initiatives although no penalties exist for non-participation. Audits within this section relate to or support the following priorities: New national targets and existing commitments (e.g., participation in heart disease audits, stroke, Myocardial Ischaemia). Participation in the National Clinical Audit & Patient Outcome Programme (NCAPOP) or Quality Accounts DoH statutory requirements, e.g. infection control monitoring. CQUINS or other commissioner priorities. Board assurance requirements External accreditation schemes, e.g. NHS Litigation Authority, cancer peer review. Clinical Effectiveness activity (e.g. following the introduction of new procedures). Patient Safety issues (including NPSA/safety alerts). National Confidential Enquiries (NCEs). Clinical Risk issues e.g. serious untoward incidents/adverse incidents. Priority 3 Priority 4 These projects have been identified within Divisions/specialties/services as important pieces of work. Audits within this section relate to or support the following priorities: It is important that to maintain a degree of locally initiated projects by clinical staff; these projects can lead to real improvements in patient care as well as providing valuable education for junior staff but do not necessarily fall into any of the other categories. Participation in national audits not part of NCAPOP (e.g. Royal College initiated) Demonstrating compliance with CQC outcomes. Guidance from professional bodies (e.g. Royal College) Audits of NICE guidance. Local guidelines/policies Identified through consultation with Trust members Other/Clinician Interest (based on criteria such as high cost, high risk, potential for change, patient involvement etc). Please note that the contact in the ‘Lead’ column may not be the person who will carry out this audit, but the senior clinician proposing and supervising a project which they plan to delegate to a junior member of staff to carry out (who would then become the project lead). Clinical Audit Annual Report 2013/14 Page 55 Division of Diagnostics & Therapies Sub-Specialty Lead Rationale/comment Priority Q Start Use of blood in patients with Sickle Cell Disease Laboratory Haematology Tom Latham National Audit (Quality Accounts) 1 Q2 Supplementary reports to identify discrepancies in paediatric tumours Histopathology Pramila Ramani Link to Board Assurance Framework/Corporate Objectives 2 Q2 Placentas microscopy in 2013 Histopathology Craig Charles Platt National guidance (RCPath Tissue Pathway 2011) 3 Q3 Re-auditing the quality of perinatal autopsy in South-West of England Histopathology Corina Moldovan National guidance (RCPath guidelines for autopsy practice 2002 and 2006) 3 Q3 Assessment of clinical information of the specimen request forms Histopathology Alica Torres National guidance (RCPath) 3 Q1 Turnaround time for urgent biopsies Histopathology Joya Pawade Departmental/service objective 2 Q1 Supplementary report for gynaecology pathology Histopathology Joya Pawade Departmental/service objective 2 Q2 Re-auditing frozen section practice in thoracic pathology Histopathology Nidhi Bhatt Departmental/service objective Re-audit ID 3627 2 Q4 Timing of antibiotic prophylaxis in cardiac surgery Microbiology Mbiye Mpenge Local guidance (antibiotic guidelines) 3 Q1 Procalcitonin testing in acute medical admissions Microbiology Richard Brindle Link to Board Assurance Framework/Corporate Objectives 2 Q3 Prophylaxis in orthopaedic surgery Microbiology Martin Williams To ensure patients are getting the correct prophylaxis 4 Q4 Audit of management of hyponatraemia Clinical Biochemistry Paul Thomas Patient Safety Trust guideline 2 Q2 Audit of Hand hygiene facilities Infection Control Joanna Hamilton-Davies External accreditation/regulation (links to CQC Outcome work) 2 Q1 Audit of Environment Infection Control Joanna Hamilton-Davies National guidance (DoH) 2 Q1 Medical Physics & Bioengineering Ian Negus National guidance (Requirement of IRMER) 2 Q3 Title Laboratory Medicine Medical Physics & Bioengineering CT radiation dose audit of L3 scanner Nutrition & Dietetics Clinical Audit Annual Report 2013/14 Page 56 Adherence to Enteral Tube Feeding Clinical Guideline in Critical Care Nutrition & Dietetics Rebecca Pooley Local guidance 3 Q2 ‘Nutrition Deep Dive audit’ an audit into the key observational prompts of the Nutritional Care Policy’ Nutrition & Dietetics Rachel Liston External accreditation/regulation (links to CQC Outcome work) 3 Q3 Occupational Therapy & Physiotherapy Outpatients Julie Packman National guidance (NHS Constitution – Improving waiting times for outpatient services) 3 Q2 Safer Care South West (Medicines Management) Pharmacy Kevin Gibbs Clinical audit/monitoring arising from individual workstreams 2 Q1 Re-audit of insulin prescribing to agreed prescribing bundle Pharmacy Kevin Gibbs Re-audit after implementation of new drug chart and guidance in 2013. 3 Q4 Vancomycin prescribing audit Pharmacy Emily Marshall Identified through patient safety/risk/incident reporting 2 Q2 Oral methotrexate treatment on adult patients (except oncology) in Pharmacy UHBristol Helen Badham National guidance (NPSA alert 3+13) 2 Q1 Physiotherapy Sarah Brown National guidance (Core standards for Intensive care units) 3 Q2 Audiology Regina Smith Outcomes monitoring - to assess the primary outcome measures as part of a quality assurance programme 2 Q1 Speech and Language Therapy Vicki Weekes National guidance (RCSLT) 3 Q3 An audit of radiation dose of 128-MDCT coronary CT angiography Radiology Stephen Lyon National guidance (Ionising Radiation Medical Exposures Regulations 2000) 2 Q1 Radiographers protocolling of CT scan Radiology Will Loughborough Identified through patient safety/risk/incident reporting 2 Q2 Radiological interpretation recording Radiology Sally King Rollover from 2013-14. 3 Q2 Sub-Specialty Lead Rationale Priority Q Start Emergency Department Lead to be confirmed National Audit (Quality Accounts) 1 Q2 Occupational Therapy ‘Patient pending’ process – Waiting list initiative Pharmacy Physiotherapy Physiotherapy standards in Intensive care unit Audiology Re-audit Real Hearing Measurement Speech & Language Therapy Standards for and outcomes of videofluoroscopy referral Radiology Division of Medicine Title Emergency Department Mental Health (College of Emergency Medicine) Clinical Audit Annual Report 2013/14 Page 57 Older People (College of Emergency Medicine) Emergency Department Lead to be confirmed National Audit (Quality Accounts) 1 Q2 National Audit of Seizure Management Emergency Department Lead to be confirmed National Audit (Quality Accounts) 1 Q2 Discharge Summary - observation ward Emergency Department Lead to be confirmed Commissioning requirement (CQUIN) Link to Board Assurance Framework/Corporate Objectives 1 Q2 Subarachnoid Haemorrhage Emergency Department Lead to be confirmed National guidance (National Confidential Enquiry) 3 Q2 Electronic sign off of results Emergency Department Lead to be confirmed Identified through patient safety/risk/incident reporting 2 Q2 Central Lines Emergency Department Lead to be confirmed Identified through patient safety/risk/incident reporting 2 Q2 Head injury Emergency Department Lead to be confirmed Local guidance 3 Q2 Fluid prescribing Emergency Department Lead to be confirmed National guidance (NICE) 2 Q2 Lower limb prophylaxsis for DVT in lower limb POP Emergency Department Lead to be confirmed National guidance 2 Q2 National Hip Fracture Database (NHFD) Care of the Elderly Rachel Bradley National audit (NCAPOP) 1 Q1 National Falls Prevention Audit (FFFAP) Care of the Elderly Rachel Bradley National audit (NCAPOP) 1 Q1 Enhanced Recovery Programme and Hip Fracture Care of the Elderly Rachel Bradley Link to Board Assurance Framework/Corporate Objectives 2 Q2 Male osteoporotic hip fractures at the BRI Care of the Elderly Theresa Allain Local concern/practice improvement 3 Q1 Notes Audit Care of the Elderly Margaret MacMahon External accreditation/regulation (links to CQC Outcome 21) 2 Q1 National Audit of Dementia Care of the Elderly Julie Dovey National audit (NCAPOP) 1 Q4 Stroke National Audit Programme (SSNAP) Stroke care Sarah Caine National audit (NCAPOP) 1 Q1 Management of syphilis Contraception and Sexual Health Andrew Leung National guidance (BASHH and local guidelines) 3 Q3 Integrated service at Bristol Sexual Health Centre Contraception and Sexual Health Judy Berry Local concern/service provision issue 3 Q1 Management of PID Contraception and Sexual Health Karla Blee National guidance (BASHH and local guidelines) 3 Q1 Medical Specialties Clinical Audit Annual Report 2013/14 Page 58 Epididymo-orchitis Contraception and Sexual Health Andrew Leung National guidance (BASHH and local guidelines) 3 Q1 Re-audit of long-acting reversible contraception (LARC) Contraception and Sexual Health Leonor Herrera-Vega National guidance (BASHH and local guidelines) 3 Q3 Re-audit of emergency contraception Contraception and Sexual Health Leonor Herrera-Vega National guidance (BASHH and local guidelines) 3 Q3 Audit of completeness of excision of non-melanoma skin cancer in Bristol Dermatology Dermatology Adam Bray Outcomes monitoring - ongoing quality indicator/per review outcome measure in cancer management. 2 Q1 Audit report on Basal Cell Carcinoma (BCC) waiting times for surgery depending on site Dermatology David DeBerker National guidance 3 Q1 Assessment of the non-Basal Cell Carcinoma skin cancers treated on a Basal Cell Carcinoma pathway Dermatology David DeBerker National guidance 3 Q1 National Diabetes Audit (NDA) Diabetes and Endocrinology Natasha Thorogood National audit (NCAPOP) 1 Q1 Outpatient coding for endocrinology as per specialist CQUIN for endocrinology Diabetes and Endocrinology Karin Bradley Commissioning requirement (CQUIN) 2 Q1 Adherence of Hepatitis B screening in patients with Inflammatory Bowel Disease (IBD) starting Immunosuppressive Therapy Gastroenterology/ Hepatology Aileen Fraser National guidance (NICE CG165) 3 Q1 Suicide Audit Liaison Psychiatry Salena Williams National guidance (National Confidential Inquiry into Suicide and Homicide for people with Mental Illness) 3 Q1 National COPD audit Respiratory Nabil Jarad National Audit (NCAPOP) 1 Q1 Plural procedures (British Thoracic Society audit programme) Respiratory Roly Jenkins National Audit (Quality Accounts) 1 Q1 Adult Bronchiectasis (British Thoracic Society audit programme) Respiratory Nabil Jarad National Audit (Quality Accounts) 1 Q3 Audit of Sweat test follow up for Ivacaftor use in CF Respiratory Kathryn Bateman Local concern 3 Q3 Audit of Annual review points against CF trust guidelines Respiratory Kathryn Bateman Local concern 3 Q3 Audit of adherence to CT Trust Guidelines for CF related low bone mineral density Respiratory Kathryn Bateman Local concern 3 Q3 Smoking cessation advice Respiratory Kathryn Bateman Re-audit CAID 3523 3 TBC Isolation in Patients with Possible Pulmonary Tuberculosis Respiratory Sarah Mungall Infection control risk Rheumatoid & Early Inflammatory Arthritis Rheumatology Robert Marshall National audit (NCAPOP) 1 Q1 Clinical Audit Annual Report 2013/14 Page 59 The use of Tocilizumab in rheumatoid arthritis Rheumatology Matthew Roy National guidance (NICE TA247) 3 Q1 TA104/125 Psoriatic arthritis - etanercept, infliximab & adalimumab Rheumatology Roopa Prasade Commissioning priority (NICE College) 1 Q3 Sub-Specialty Lead Rationale Priority Q Start Adult Cardiac Surgery (ACS) Cardiac Surgery Alan Bryan National audit (NCAPOP) 1 Q1 Acute Coronary Syndrome/Acute Myocardial Infarction (MINAP) Cardiology Julian Strange National Audit (NCAPOP) 1 Q1 National Cardiac Arrhythmia Audit (HRM) Cardiology Tim Cripps National Audit (NCAPOP) 1 Q1 National Heart Failure Audit (HF) Cardiology Angus Nightingale National Audit (NCAPOP) 1 Q1 Adult Coronary Angioplasty Cardiology Tom Johnson National Audit (NCAPOP) 1 Q1 TA230 Bivalirudin - Myocardial infarction (persistent ST-segment elevation) Cardiology Julian Strange Commissioning priority (NICE College) 1 Q3 Prescribing audit on critical medicine Cardiac Intensive Care Richard Bateman Identified through patient safety/risk/incident reporting 2 Q2 Impact of the Anaesthetist on Mortality During Cardiothoracic Surgery Cardiac Anaesthesia James Hillier National Audit (Other) 3 Q1 Audit of missed appointments at a tertiary referral centre Cardiology Julian Strange Links to productive outpatient work 3 Q2 Patient outcomes in Chest Pain Clinics Cardiology Jenny Tagney National guidance (NICE CG95) 3 Q2 The usage of Ivabradine for treating chronic heart failure Cardiology Phoebe Sun National guidance (NICE TA267) 3 Q1 Audit of quality of stress echo service Cardiology Angus Nightingale National guidance (British Society of Echo-cardiography) 3 Q2 Percutaneous closure of patent foramen ovale for the secondary prevention of recurrent paradoxical embolism in divers Cardiology Mark Turner National guidance (NICE IPG372) 3 Q2 Audit of management of heart failure post primary percutaneous coronary intervention (PCI) Cardiology Angus Nightingale National guidance (NICE) 3 Q2 Re-audit of prescribing in hypertension Cardiology Angus Nightingale National guidance (NPSA) 2 Q2 Division of Specialised Services Title Cardiac Services Clinical Audit Annual Report 2013/14 Page 60 Oncology & Haematology National Lung Cancer Audit (NLCA) Oncology/Respiratory Adam Dangoor National Audit (NCAPOP) 1 Q1 TA129 Multiple myeloma - bortezomib Oncology/Haematology Jenny Bird Commissioning priority (NICE College) 1 Q3 High dose rate brachytherapy for treatment of localised prostate cancer Oncology Amit Bahl/Pauline Humphrey New approved interventional procedure 2 Q3 Stereotactic Ablative Body Radiotherapy for peripheral lung tumours Oncology Charlie Commins New approved interventional procedure 2 Q4 PCA pump audit Oncology/Haematology Tracey Arthur Identified in BHOC Clinical Governance Meeting 2 Q2 Extravasculation Audit Oncology/Haematology Rae Herrington Identified in BHOC Clinical Governance Meeting 2 Q3 Patient Information - Pressure Sores Oncology/Haematology Jane Bailey Identified in BHOC Clinical Governance Meeting 2 Q1 Drug chart audit Oncology/Haematology Charlie Comins Local concern 3 Q3 Audit of Aprepitant for control of chemotherapy induced nausea and vomiting Oncology/Haematology Helen Brookes Re-audit CAID 2777 3 Q3 Audit of completion of pregnancy status and fertility status on the radiotherapy form Oncology Jancis Kinsman Re-audit CAID 2963 3 Q3 Medical documentation re-audit Oncology/Haematology Charlie Comins Re-audit CAID 2998 3 Q3 Use of PCI for patients with small cell lung cancer Oncology Paula Wilson Local concern 3 Q3 CHART Audit Oncology Gareth Ayre National Audit (Other) 2 Q1 Haemoglobinopathies - Patients with recommended immunisations Haematology up-to-date Anndeloris Chacon/ Kim Bealing National guidance (quality standards for Haemoglobinopathy services) 3 Q1 Audit of regular pen V or equivalent Haematology Anndeloris Chacon/ Kim Bealing Local concern 3 Q1 An audit of patients attending in acute pain receiving first dose of analgesia within 30 mins of arrival Haematology Anndeloris Chacon/ Kim Bealing Local concern 3 Q1 Thalassaemia audits - monitoring of iron overload including imaging and new iron related complications Haematology Anndeloris Chacon/ Kim Bealing Local concern 3 Q1 Palliative Medicine Colette Reid National guidance (End of Life Care) 3 Q3 Palliative Care Advanced Care Planning Clinical Audit Annual Report 2013/14 Page 61 Usage of the Treatment Escalation Protocol (TEP) Palliative Medicine Rachel McCoubrie National guidance (National Confidential Enquiry) 2 Q4 Sub-Specialty Lead Rationale Priority Q Start An audit of analgesia prescribing in acute medical and surgical admissions with renal impairment. Acute Pain Nilesh Chauhan Local guidance (introduction of new guideline) 2 Q4 Emergency Laparotomy Anaesthesia/Surgery Rachel Craven /Jane Blazeby National Audit (NCAPOP) 1 Q1 Perioperative Anaphylaxis Anaesthesia Nic Harvey National Audit (Other) 3 Q2 Coagulation and epidural removal Anaesthesia Nic Harvey Identified through patient safety/risk/incident reporting 2 Q1 Safer Care South West (Critical Care) Critical Care Sanjoy Shah Clinical Audit/Monitoring arising from individual workstreams 2 Q1 Adult Critical Care Case Mix Programme (ICNARC CMP) Critical Care Tim Gould National Audit (Quality Accounts) 1 Q1 Trauma (TARN) Critical Care Matt Thomas National Audit (Quality Accounts) 1 Q1 Potential Donor Audit Critical Care Fran O’Higgins National Audit (Quality Accounts) 1 Q1 ALung Hemolung Respiratory Assist System Critical Care Tim Gould New approved interventional procedure 2 Q2 ‘Knowing the Risk’ Pre op assessment Ben Howes National guidance (National Confidential Enquiry) 3 Q2 Safer Care South West (Perioperative care) Theatres Liz Varian Clinical Audit/Monitoring arising from individual workstreams 2 Q1 Surgical Site Marking Theatres Andy Hollowood Identified through patient safety/risk/incident reporting 2 Q3 National Head & Neck Cancer (DAHNO) Oral and Maxillofacial Surgery Ceri Hughes National audit (NCAPOP) 1 Q1 Bisphosphonate related osteocronosis of the jaw (BRONJ) Oral and Maxillofacial Surgery Carla Fleming/ Chris Bell Re-audit CAID 3387 3 Q2 Smoking cessation advice Oral Medicine Natalie Edwards Re-audit CAID 3186 3 Q2 Division of Surgery, Head and Neck Title Anaesthesia, Critical Care & Theatres Dental Services Clinical Audit Annual Report 2013/14 Page 62 Audit of new trauma form in paediatric dentistry Paediatric Dentistry Rebecca John Re-audit CAID 3155 3 Q1 Sickle cell Paediatric Dentistry Sarah Dewhurst Local guidance (revision of guideline) 3 Q2 Compliance with DNA Policy Orthodontics Nikki Attack External accreditation/regulation (area of improvement identified by CQC) 2 Q3 Periodontal screening in adult orthodontic patients Orthodontics Kate House National guidance 3 Q3 Radiograph Quality Assurance in Out of Hours Dental Service Primary Care Dental Service Katherine Walls Service priority 3 Q2 Tooth survival and restorative status of undergraduate root treated Restorative Dentistry teeth Dominic O’Sullivan Local guidance (introduction of new guideline) 3 Q2 Fluoride DPT prescriptions Restorative Dentistry Roger Yates/James Ban Re-audit CAID 3459 3 Q3 Periodontal radiographs Restorative Dentistry Roger Yates /James Ban Re-audit CAID 3292 3 Q3 Active Middle Ear Implant (Vibrant Soundbridge) Adult ENT Stephen Broomfield New approved interventional procedure 2 Q4 Injection Snoreplasty Adult ENT Ade Oluwasanmi New approved interventional procedure 2 Q4 A&E 4 hour breaches and follow-ups A&E & Primary Care Rafik Girgis Significant waiting time targets for Trust. Assess improvement since previous audit 3 Q3 Implantation of multifocal intraocular lenses during cataract surgery Cornea and Cataract Phil Jaycock New approved interventional procedure 2 Q2 Intraocular lens insertion for correction of refractive error with preservation of the natural lens guidance Cornea and Cataract Phil Jaycock New approved interventional procedure 2 Q2 Microbial Keratitis re-audit Cornea and Cataract Derek Tole Re-audit CAID 3703 4 Q1 Cataract Outcomes Cornea and Cataract Derek Tole National guidance (Royal College led initiative relating to revalidation of cataract surgeons) 3 Q1 Deep Sclerectomy (non-penetrating glaucoma filtration surgery) Glaucoma Rani Sebastian New approved interventional procedure 2 Q3 Selective Laser Trabeculoplasty (SLT) Glaucoma Rani Sebastian New approved interventional procedure 2 Q3 Trabeculectomy outcomes Glaucoma John Sparrow/Peter Tsangaris Outcomes minitoring 4 Q2 ENT Ophthalmology Clinical Audit Annual Report 2013/14 Page 63 Lucentis outcomes Medical & Surgical Retina Adam Ross National guidance (NICE TA155) 2 Q3 Management of endophthalmitis Medical & Surgical Retina Adam Ross Identified through patient safety/risk/incident reporting 2 Q1 TA287 Aflibercept - 1st line wet AMD Medical & Surgical Retina Claire Bailey Commissioning priority (NICE College) 1 Q3 TA274 Ranibizumab - Diabetic Macular Oedema Medical & Surgical Retina Claire Bailey Commissioning priority (NICE College) 1 Q3 Assessment of orbital trauma patients Orthoptics and Optometry Ann Starbuck Re-audit 4 Q3 Periorbital filler injection Paediatrics, Oculoplastics and Squint Mano Sira New approved interventional procedure 2 Q2 Outcomes of nasolacrimal duct probing (re-audit) Paediatrics, Oculoplastics and Squint Amanda Churchill Re-audit CAID 1508 4 Q1 IV fluid management All specialties Meg Finch-Jones National guidance (NICE CG174) 2 Q1 National Bowel Cancer Audit (NBOCAP) Colorectal Surgery Rob Longman National audit (NCAPOP) 1 Q1 SECCA (Radiofrequency Ablation for Feacal Incontinence) Colorectal Surgery Paul Sylvester New approved interventional procedure 2 Q2 Thoracic Society Returns Thoracic Surgery Tim Batchelor National audit (Other) 3 Q1 CT-guided guidewire localisation of impalpable lung lesions before minimal access surgical excision Thoracic Surgery Tim Batchelor/Doug West New approved interventional procedure 2 Q2 Left cardiac sympathetic denervation Thoracic Surgery Tim Batchelor New approved interventional procedure 2 Q2 Lung volume reduction surgery through a bronchoscope Thoracic Surgery/Respiratory Doug West /Nabil Jarad Medicine New approved interventional procedure 2 Q2 Bronchoscopic lung volume reduction using Lung Volume Reduction Coil Thoracic Surgery/Respiratory Doug West/Nabil Jarad Medicine New approved interventional procedure 2 Q2 VATS sleeve lobectomy Thoracic Surgery Gianluca Casali New approved interventional procedure 2 Q3 Cardiac denervation for VT Thoracic Surgery Tim Batchelor/Graham Stuart New approved interventional procedure 2 Q3 Thoracic Surgery lobectomy patients – why are patients staying longer than 5 days in hospital. Thoracic Surgery Tim Batchelor Trust objective – links to patient flow 2 Q2 National Joint Registry (NJR) Trauma & Orthopaedics Sanchit Mehendale National audit (NCAPOP) 1 Q1 Adult Surgical Specialties Clinical Audit Annual Report 2013/14 Page 64 British Orthopaedic Standards for Trauma (BOAST) Fracture Service Trauma & Orthopaedics Steve Mitchell National guidance 3 Q2 National Oesophago-Gastric Cancer Audit (NAOGC) Upper GI Surgery Paul Barham National audit (NCAPOP) 1 Q1 Oesophageal brachytherapy Upper GI Surgery Paul Barham New approved interventional procedure 2 Q3 Endoscopic vacuum therapy for perforation/ leakage in the oesophagus Upper GI Surgery Dan Titcomb New approved interventional procedure 2 Q3 Microwave ablation for the treatment of liver metastases Upper GI Surgery Meg Finch-Jones New approved interventional procedure 2 Q4 Insertion of wound catheters for post-operative pain control Upper GI Surgery Reyad Abbadi/Jeremy Bewley New approved interventional procedure 2 Q4 VSGBI Vascular Surgery Database Vascular Surgery Marcus Brooks National Audit (NCAPOP) 1 Q1 Surgical site infection Vascular Surgery Marcus Brooks National guidance (NICE CG74) 3 Q1 Management of incidental AAA Vascular Surgery Marcus Brooks National guidance (AAA screening programme) 3 Q1 Sub-Specialty Lead Rationale Priority Q Start Paediatric Early Warning Scores All areas/specialties Hazel Moon Identified through patient safety/risk/incident reporting 2 Q1 Any topics for audit arising from Child Death Reviews All areas/specialties James Fraser Identified through patient safety/risk/incident reporting 2 Q4 Re-audit of pain after cardiac surgery Anaesthetics Richard Beringer No specific rationale provided 4 Q4 Preoperative medical clerking Anaesthetics Philippa Seal National guidance (AAGBI) 3 TBC Re-Audit of Anaesthetic Record Keeping Anaesthetics Bev Guard National guidance (RCOA standard and CQC AAGBI ‘Consent for Anaesthesia’ Guidelines) 3 Q2 Anaesthetic Pre-admission Information re-audit Anaesthetics Steve Sale National guidance (AAGBI / RCOA / RCN ‘Best Practice’ Guide for management of epidurals) 3 Q2 Re-audit pre-op fasting Anaesthetics Bev Guard Local guidance (introduction of new guideline) 3 Q3 Division of Women’s & Children’s Title Children’s Services Clinical Audit Annual Report 2013/14 Page 65 Patient management post identification of bilateral permanent childhood hearing impairment v national screening programme standards. Audiology Joanne O’Connell National guidance (Newborn Hearing Screening Programme) 3 Q3 Re-Audit of Hearing aid Review Clinics v national and local standards Audiology Dawn O'Dwyer National guidance 3 Q3 Child Protection Child Protection Lisa Goldsworthy Identified through patient safety/risk/incident reporting 3 TBC Congenital heart disease (CHD) Cardiac Services Andrew Parry National Audit (NCAPOP) 1 Q1 Re-audit of anti-coagulation Cardiac Services Pat Weir Identified through patient safety/risk/incident reporting 2 TBC Communication abnormal laboratory results to Ward Cardiac Services Andrew Parry Identified through patient safety/risk/incident reporting 2 TBC Clinical data/information correlation audit Cardiac Services Serban Stoica Area for cost saving 3 Q2 National Diabetes Audit (NDA) Diabetes & Endocrinology Christine Burren National Audit (NCAPOP) 1 Q1 Re-audit growth hormone use Diabetes & Endocrinology Liz Crowne National guidance (NICE TA188) 3 Q2 Fitting Child (College of Emergency Medicine) Emergency Department Lead to be confirmed National Audit (Quality Accounts) 1 Q3 Trauma (TARN) Emergency Department Nick Sergeant National Audit (Quality Account) Service Requirement 1 Q1 EZ-IO needles Emergency Department Lead to be confirmed Identified through Child Death Review 2 TBC "Did not wait" policy Emergency Department Lead to be confirmed Local guidance 3 TBC Bereavement counselling Emergency Department Francis Edwards External accreditation/regulation (identified from CQC enquiry to Trust) 2 Q1 UTI sample collection and lab delivery - re-audit Emergency Department Will Christian Re-audit ID 3552 2 Q1 Provision of information leaflets and advice Emergency Department Nick Sergeant Identified through patient safety/risk/incident reporting 2 Q2 National Inflammatory Bowel Disease audit Gastroenterology Christine Spray National audit (NCAPOP) 1 Q1 Re-audit Infliximab and Adalimumab use in children with Crohns disease Gastroenterology Christine Spray National guidance (NICE TA187) Re-audit ID 3377 3 Q3 Kawasaki disease General Paediatrics Alison Kelly/ Jon Forsey Local Guideline 3 Q1 Clinical Audit Annual Report 2013/14 Page 66 Iv fluid prescription chart audit General Paediatrics Elenor Tickner / Alison Kelly Re-audit ID 3549 3 Q1 Use and usefulness of bronchiolitis patient information leaflet General Paediatrics Reg Bragonier Identified through patient complaints process 2 Q1 Aseptic non-touch technique for Central Venous Lines Haematology/ Oncology Wendy Saegenschnitter No specific rationale provided 4 Q1 Peripheral blood stem cell harvest on solid tumour patients in 2012/2013 Haematology/ Oncology Balveer Kaur No specific rationale provided 4 Q1 Review of admissions of cancer patients to PICU Haematology/ Oncology Barbara Torres No specific rationale provided 4 Q1 Review of antiemetic medication use for inpatient chemotherapy Haematology/ Oncology Indril Dey No specific rationale provided 4 Q1 Re-audit of antiemetic policy following review Haematology/ Oncology Vanessa Mcleland No specific rationale provided 4 Q3 Fungal infection in leukaemia Haematology/ Oncology Peter Wassaa No specific rationale provided 4 Q1 Blood product use in cancer patients Haematology/ Oncology Peter Wassaa No specific rationale provided 4 Q1 Re-immunisation post chemotherapy- Haematology/ Oncology Frankie Toussaint No specific rationale provided 4 Q1 Pneumococcal vaccination in Sickle cell patient Haematology/ Oncology Michelle Cummins No specific rationale provided 4 Q4 Paediatric Intensive Care (PICANet) Intensive Care (Paediatric) Peter Davis National Audit (NCAPOP) 1 Q1 National Neonatal Audit Project (NNAP) Intensive Care (Neonatal) Pam Cairns National audit (NCAPOP) 1 Q1 Vermont-Oxford Benchmarking Project Intensive Care (Neonatal) David Harding National Audit (other - National/International quality improvement project) 2 Q1 Compliance with heel-prick blood sampling guideline Intensive Care (Neonatal) Anoo Jain Local concern 4 Q2 Central line insertion in NICU Intensive Care (Neonatal) Madhavi Parvathareddy National guidance (Matching Michigan project standards) 3 Q1 Car seat assessment in neonates Intensive Care (Neonatal) Pam Cairns/Anoo Jain Local guidance 4 Q1 Newborn Life Support (Joint project with Obstetrics/Midwifery) Intensive Care (Neonatal) Sue Braithwaite/Karen MacDonald-Taylor External accreditation/regulation (CNST Maternity Standard 3.5.2) 2 Q1 Occupational Therapy Provision Occupational Therapy Lisa Mills Identified through patient safety/risk/incident reporting 2 Q3 Clinical Audit Annual Report 2013/14 Page 67 Renal Registry (UKRR) Nephrology Carol Inward National Audit (Quality Accounts) 1 Q1 Renal biopsy Nephrology Jan Dudley National guidance (Specialty Group) 3 Q2 Dialysis line locks Nephrology Jenny Haylor National guidance (NPSA /Toft report) 2 Q1 Epilepsy 12 (Childhood Epilepsy) Neurology Phil Jardine National Audit (NCAPOP) 1 Q1 Paediatric Pneumonia (British Thoracic Society audit programme) Respiratory Deb Marriage National Audit (Quality Accounts) 1 Q3 Medication information contained in Paediatric Rheumatology clinic letters and discharge summaries v RCPCH standards Rheumatology Alison Kelly National guidance 3 Q1 Use of Etanercept in Juvenile Idiopathic Arthritis (JIA) against NICE guidelines Rheumatology AV Ramanan National guidance (NICE TA35) 3 Q1 Use of Tocilizumab in Systemic Juvenile Idiopathic Arthritis (sJIA) versus NICE guidelines Rheumatology AV Ramanan National guidance (NICE TA238) 3 Q1 Recording of core outcome variables for patients with juvenile idiopathic arthritis (JIA) versus national standards Rheumatology AV Ramanan National guidance 3 Q1 Errors in radiology reports using voice recognition software Radiology David Grier Change in practice, evaluation required 3 Q1 Biofeedback in management of dysfunctional voiding Surgery Mark Woodward Evaluation of outcomes post implementation of a new clinic 3 Q1 Human Fertilisation and Embryology Authority (HFEA) statutory compliance Reproductive Medicine David Cahill National guidance (regular audit of compliance with national standard operating procedure) 2 Q4 Outpatient Hysteroscopy Gynaecology Katherine O’Brien/ Naomi Crouch To determine whether clinically suitable patients are being 4 managed as outpatients Q1 Heavy Menstrual Bleeding (NICE QS47) Gynaecology Munawar Hussain/Martin Mills National guidance (NICE QS47) 4 Q1 Female Genital Mutilation in pregnancy Obstetrics/Midwifery Sara-Jane Sheldon Re-audit / joint audit with North Bristol Trust 3 Q2 Magnesium sulphate for neuroprotection in pre-term birth (Joint project with Neonatology) Obstetrics/Midwifery Emma Treloar/Karen Luyt Regional project managed by West of England Academic Health Science Network 3 Q2 Care of Women in Labour, incl. Intermittent Auscultation, Continuous Electronic Fetal Monitoring, Fetal Blood Sampling, Use of Oxytocin Obstetrics/Midwifery Emma Treloar/Jane Farey External accreditation/regulation (CNST Maternity standards 3.2.1 to 3.2.5) 2 Q1 Caesarean Section – Decision to Delivery times (NICE CG132) (Joint project with Obs and Gynae Anaesthesia) Obstetrics/Midwifery Emma Treloar/Stephen Kinsella External accreditation/regulation (CNST Maternity Standard 3.2.6) 2 Q1 Women’s Services Clinical Audit Annual Report 2013/14 Page 68 Intrauterine resuscitation in cases of suspected acute hypoxia (Joint project with Obs and Gynae Anaesthesia) Obstetrics/Midwifery Rachna Bahl/Stephen Kinsella Local guidance (caesarean section guideline) 4 Q1 Shoulder Dystocia Obstetrics/Midwifery Rachna Bahl External accreditation/regulation (CNST Maternity Standard 3.3.6) 2 Q1 Perineal Tear Obstetrics/Midwifery Rachna Bahl/Di Dorrington External accreditation/regulation (CNST Maternity Standard 3.3.5) 2 Q1 Obstetric Haemorrhage Obstetrics/Midwifery Rachna Bahl/Caryn Albury External accreditation/regulation (CNST Maternity Standard 3.3.7) 2 Q1 UNICEF UK Baby Friendly Initiative / Newborn Feeding Obstetrics/Midwifery Joan Beales External accreditation/regulation (UNICEF standards & CNST Maternity Standard 3.5.5) 2 Q1 Examination of the Newborn Obstetrics/Midwifery Anne Duffner External accreditation/regulation (CNST Maternity Standard 3.5.6) 2 Q1 Postnatal care Obstetrics/Midwifery Sara-Jane Sheldon External accreditation/regulation (CNST Maternity Standard 3.3.7) 2 Q2 Support for Parents Obstetrics/Midwifery Louise Howarth External accreditation/regulation (CNST Maternity Standard 3.5.8) 2 Q3 Immediate Care of the Newborn (Joint project with Neonatology) Obstetrics/Midwifery Sara-Jane Sheldon /Anoo Jain External accreditation/regulation (CNST Maternity Standard 3.5.4). 2 Q3 Handover of Care (Onsite) Obstetrics/Midwifery Sara-Jane Sheldon External accreditation/regulation (CNST Maternity Standard 3.4.8) 2 Q3 Title Sub-Specialty Lead Rationale Priority Q Start Blood Transfusion All areas/specialties Tom Latham Transfusion Group Priority 2 Q2 Audit of suspected VTE management All areas/specialties Amanda Clark Commissioning requirement (Links to Quality Schedule) 1 Q2 Audit of patient transfer All areas/specialties Anne Reader Commissioning requirement (Links to Quality Schedule) 1 Q2 Sepsis All areas/specialties Jeremy Bewley Commissioning requirement (CQUIN) 1 Q2 Audit of patient discharge All areas/specialties Anne Reader Commissioning requirement (Links to Quality Schedule) Link to Board Assurance Framework/Corporate Objectives 1 Q2 Medical Records audit All areas/specialties Jane Luker External accreditation/regulation (links to CQC Outcome work) 1 Q2 Nursing documentation audit All areas/specialties Helen Morgan External accreditation/regulation (links to CQC Outcome work) 1 Q2 Non Division Specific Clinical Audit Annual Report 2013/14 Page 69 Appendix E - National audit participation (extract from Quality Report 2013/14) Participation in clinical audits and national confidential enquiries For the purposes of Quality Accounts and Reports, the Department of Health publishes an annual list of national audits and confidential enquiries, participation in which is seen as a measure of quality of local clinical audit programmes. This list is not exhaustive, but rather aims to provide a baseline for trusts in terms of percentage participation and case ascertainment1. The information which follows relates to this list. During 2013/14, 39 national clinical audits and three national confidential enquiries covered NHS services that University Hospitals Bristol NHS Foundation Trust provides. During that period, University Hospitals Bristol participated in 95% (37/39) national clinical audits and 100% (3/3) national confidential enquiries of which it was eligible to participate in. The national clinical audits and national confidential enquiries that University Hospitals Bristol NHS Foundation Trust was eligible to participate in during 2013/14 are as follows: Name of audit / Clinical Outcome Review Programme Eligible Participated Yes Yes Yes No Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Severe sepsis and septic shock Yes Yes Severe trauma (Trauma Audit & Research Network, TARN) Yes Yes Blood and Transplant National Comparative Audit of Blood Transfusion programme Yes Yes Cancer Bowel cancer (NBOCAP) Head and neck oncology (DAHNO) Lung cancer (NLCA) Oesophago-gastric cancer (NAOGC) Yes Yes Yes Yes Yes Yes Yes Yes Heart Acute coronary syndrome or Acute myocardial infarction (MINAP) Cardiac Rhythm Management (CRM) Congenital heart disease (Paediatric cardiac surgery) (CHD) Coronary angioplasty National Adult Cardiac Surgery Audit Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes National Cardiac Arrest Audit (NCAA) Yes Yes National Heart Failure Audit Yes Yes National Vascular Registry Yes Yes Acute Case Mix Programme (CMP) Emergency use of oxygen (British Thoracic Society) Medical and surgical clinical outcome review programme: National confidential enquiry into patient outcome and death National Audit of Seizures in Hospitals (NASH) National emergency laparotomy audit (NELA) National Joint Registry (NJR) Paracetamol overdose (care provided in emergency departments) Long term conditions 1 i.e. the number of individual patents we submit data on compared to how many we should have submitted data on (usually outlined through Hospital Episode Statistics or similar) Clinical Audit Annual Report 2013/14 Page 70 Diabetes (Adult) ND(A), includes National Diabetes Inpatient Audit (NADIA)* Diabetes (Paediatric) (NPDA) Inflammatory bowel disease (IBD) National Chronic Obstructive Pulmonary Disease (COPD) Audit Programme BTS Paediatric bronchiectasis (British Thoracic Society) Renal replacement therapy (Renal Registry) Rheumatoid and early inflammatory arthritis** Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes No Yes Yes Older People Falls and Fragility Fractures Audit Programme (FFFAP) Sentinel Stroke National Audit Programme (SSNAP) Yes Yes Yes Yes Other Elective surgery (National PROMs Programme) Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Women’s & Children’s Health Child health clinical outcome review programme (CHR-UK) Epilepsy 12 audit (Childhood Epilepsy) Maternal, Newborn and Infant Clinical Outcome Review Programme (MBRRACE-UK) Moderate or severe asthma in children (care provided in emergency departments)* Neonatal intensive and special care (NNAP) Paediatric asthma Paediatric intensive care (PICANet) * Organisational aspects only The Trust did not participate in two national audits under the auspices of the British Thoracic Society and is undertaking relevant local audit activity instead. The national clinical audits and national confidential enquiries that University Hospitals Bristol NHS Foundation Trust participated in, and for which data collection was completed during 2013/14, are listed below alongside the number of cases submitted to each audit or enquiry as a percentage of the number of registered cases required by the terms of that audit or enquiry. Name of audit / Clinical Outcome Review Programme % cases submitted Acute Case Mix Programme (CMP) National Audit of Seizures in Hospitals (NASH) National Joint Registry (NJR) Paracetamol overdose (care provided in emergency departments) Severe sepsis & septic shock Severe trauma (Trauma Audit & Research Network, TARN) 1190* 100% (30/30) 98% (49/50) 100% (50/50) 100% (50/50) 68% (200/294) Blood and Transplant National Comparative Audit of Blood Transfusion programme 38* Cancer Bowel cancer (NBOCAP) Head and neck oncology (DAHNO) Lung cancer (NLCA) Oesophago-gastric cancer (NAOGC) 94% (162/173) 90* 80% (144/180) 99% (149/150) Heart Clinical Audit Annual Report 2013/14 Page 71 Acute coronary syndrome or Acute myocardial infarction (MINAP) 985* Cardiac Rhythm Management (CRM) Congenital heart disease (Paediatric cardiac surgery) (CHD) Coronary angioplasty National Adult Cardiac Surgery Audit 100% (792/792) 100% (742/742) 100% (1423/1423) 100% (1481/1481) National Cardiac Arrest Audit (NCAA) 133* National Heart Failure Audit 100% (403/403) National Vascular Registry 98% (145/148) Long term conditions Diabetes (Adult) ND(A), includes National Diabetes Inpatient Audit (NADIA) Diabetes (Paediatric) (NPDA) Inflammatory bowel disease (IBD) 99% (100/101) 1354* 100% (40/40) Older People Falls and Fragility Fractures Audit Programme (FFFAP) Sentinel Stroke National Audit Programme (SSNAP) 345* 100% (121/121) Other Elective surgery (National PROMs Programme) 27% (33/122) Women’s & Children’s Health Moderate or severe asthma in children (care provided in emergency departments) Neonatal intensive and special care (NNAP) Paediatric intensive care (PICANet) 100% (50/50) 100% (2739/2739) 100% (671/671) *No case requirement outlined/unable to establish baseline from HES data The reports of ten national clinical audits were reviewed University Hospital Bristol NHS Foundation Trust in 2013/14. The Trust is taking the following actions to improve the quality of healthcare provided: College of Emergency Medicine (CEM) audits The Medway system has been altered to allow better electronic capture of data relating to consultant review or discussion. Monthly reporting against the CEM quality standard has been introduced to inform further actions required by pinpointing times / days when standards are less likely to be adhered to. National Audit of Dementia A care pathway for frail older people which incorporates people with a dementia will be developed. Access to intermediate care services to allow people with dementia to be admitted to intermediate care directly will be part of this review. A review of the model of care for the older adult admissions wards is to be undertaken. A clinical guideline is being developed to ensure that patients with dementia or cognitive impairment are assessed for the presence of delirium at presentation using a recognised tool (Confusion Assessment Method). An electronic discharge summary for all patients who are 75 years and over will be developed which contains mandatory fields to include abbreviated mental test score, cause of cognitive impairment, symptoms of delirium, and behavioural and psychological symptoms of dementia. National Cancer Audits Significant progress has been made with the lung, bowel and head and neck audits in 2013. All three audits returned their best ever standard of submission in terms of data completeness and quality. Easy format written guidance on data entry has been produced, along with reports that allow MDT coordinators to easily identify and rectify data gaps, and their managers to monitor this. This system has received positive feedback from coordinators and clinicians. Clinical Audit Annual Report 2013/14 Page 72 All national audit submissions have undergone clinical quality assurance prior to submission. Monthly submission has been introduced along with a robust system for identifying ‘rejected’ records enabling these to be quickly fixed. The Trust’s cancer manager continues to work closely with the Somerset Cancer Register to ensure the best use of the register and influence its development. National Diabetes Audit (NADIA) Increased diabetes specialist nursing input was allocated via CQUIN funding to help improve the care that diabetic patients receive as inpatients. National Cardiac Arrest Audit (NCCA) All cardiac arrests are now reported on the Trust incident reporting system (Ulysses Safeguard) to enable learning from these incidents. Falls and Fragility Fractures Audit Programme - National Hip Fracture Database The appointment of a specialist hip fracture nurse (and audit nurse responsible for data) has resulted in a significant improvement in data quality, and patient care as a whole. A business case was approved and implemented to increase orthogeriatrician input, increase trauma theatre allocation and implement direct access beds. National Vascular Registry A written pathway of care for Transient Ischaemic Attacks (TIAs) and non-disabling stroke for Bristol Bath and Weston Vascular Network is being developed to ensure that the agreed protocol for referral is followed to help avoid any unnecessary delay. National Neonatal Audit Project A preterm breast feeding project has been started aiming to improve rates of breastfeeding at discharge. The outcome and action summaries of 205 local clinical audits were reviewed by University Hospital Bristol NHS Foundation Trust in 2013/14; summary outcomes and actions reports are reviewed on a bi-monthly basis by the Trust’s Clinical Audit Group. Details of the changes and benefits of these projects will be published in the Trust’s Clinical Audit Annual Report for 2013/142. 2 Available via the Trust’s internet site from June 2013 Clinical Audit Annual Report 2013/14 Page 73