Name: Alisha H. MRN: 123456 DOB: 06/25/1984 Age: 28 CC
advertisement

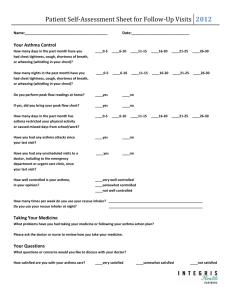
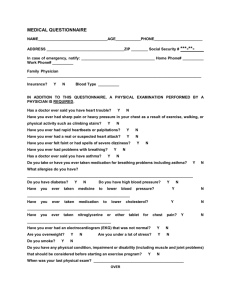
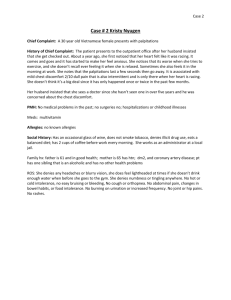
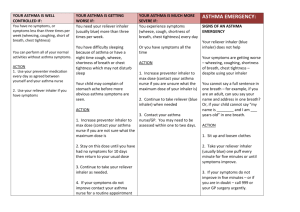
Name: Alisha H. MRN: 123456 DOB: 06/25/1984 Age: 28 CC: Periodic “chest tightness” Subjective: Patient is a pleasant 28 y/o Caucasian female with a history of asthma and anxiety. She presents today with a history of atypical chest pain that has been periodic in nature which her PCP, Dr. D, has diagnosed as asthma. She describes the chest pain as a “tightness” that limits her ability to “move air” and denies radiation of the pain as well as wheezing or loss of consciousness.Patient comes in today stating she wants “better control” of her asthma and to review the results of her pulmonary function test from 7/12/12. Patient states that her first episode of chest pain occurred approximately 10 years ago and went away after a short time without her doing anything. She explains that since then she has periodically experienced similar episodes a couple times a month, often worse in when it is very hot outside or when there are a lot of stressors in her life. On a weekly basis, she states that she has two or three episode a week and experiences nocturnal coughing “a couple” of times per month. She also denies a correlation between exertion and the episodes, but does say that she is unable to participate in normal activities when she is having an attack. Patient states that the pain is a 7/10 with 10 being….during these episodes, but it is a diffuse pain, rather than sharp or in any particular area. She says that time and consciously trying to take deep breaths can help her recover from these episodes and that the pain is typically gone a couple of hours after it starts. Patient denies experiencing heartburn. She has previously been prescribed ProAir from her PCP and had PFTs performed approximately one year ago that showed a “borderline” asthmatic pattern. Patient has not been satisfied with the effectiveness of ProAir what about pertienet ROS that is needed up here??? Ie Cardiac, resp., GI????LMP??? PMH.up here Family Hx: ; ???family history is significant for depression, diabetes mellitus and cardiovascular disease. Denies family history of lung cancer, early COPD or asthma Social Hx: Patient is married and lives with her husband and four year old son Works as an account manager at a magazine; States she smoked approximately 1 pack of cigarettes per day for 3 years but quit smoking 5 years ago; Also states she drinks approximately 1-2 drinks of what???per month; Denies use of illicit drugs. Allergies: Tetanus toxoid reaction? Immunizations: Current Medications: ProAir 180 µg (2 puffs) PRN; Propranolol 160 mg PO BID PMH: Migraine headaches for which she sees a pain management doctor in York pertinent negatives? PSH: Tubal ligation (2010) Objective: Vitals: Temperature: 96.7F P: 76 R: 20 BP: 116/74 Height: 67 inches Weight: 183lbs. BMI: 28.7 General Appearance: Pleasant, well groomed female; alert and oriented X3 Needs oropharynx and neck exam with nodes Chest: No scars, ecchymosis, asymmetry or erythema of chest noted; Chest wall expansion found to be equal, with no accessory muscle use or intercostal retractions noted; A:P ratio is 2:1; No tenderness or fremitus of chestcheck Bates for normal an abnormal findings in fremitus found on palpation; Lung fields are clear to percussion bilaterally; Dry breath sounds found bilaterally in apices and bases; no wheezing/rales/rhonchi/stridor appreciated Heart: RRR no m/g/r/ Skin: Warm, no erythema or cyanosis noted; No contusions, rashes, or bleeding Peripheral Vascular: No edema of the upper or lower extremities noted; Radial and Dorsalis Pedis pulses palpated, present and equal bilaterally, +2/4 Abd Exam??? Labs/Tests: Pulmonary Function Test: Spirometry: Prebronchodilator = moderate airway obstruction (FEV1/FVC = 61%) Postbronchodilator = mild airway obstruction (FEV1/FVC = 78%) Lung Volumes: TLC normal (91%), RV normal (99%) Diffusion: DLCO normal (90%) Assessment: 1) Asthma 2) Anxiety 3) Overweight Differential Diagnosis: Vocal cord dysfunction, Gastroesophageal reflux, Tracheal and bronchial lesions, Chronic Obstructive Pulmonary Disease Plan: 1) Asthma: Due to the insufficient control of her symptoms with only an albuterol rescue inhaler (ProAir), Mrs. H was prescribed Pulmicort 180 µg daily to help control her symptoms. She was also given a renewal of her ProAir for use a rescue inhaler. If her symptoms do not significantly improve she was instructed to inform the office. Mrs. H was scheduled for a follow up in six months and at that time she will also get another set of PFTs. We also discussed talking with her pain management doctor to possibly switching from Propranolol, a beta-blocker, to another medication for her migraine headaches due to the adverse effect beta-blockers can have on asthma. Such as… 2) Anxiety: We discussed breathing techniques to help her control her anxiety. Patient states that she has been working with her PCP on her anxiety issues.does she need to seek counseling? 3) Overweight: Patient was given a handout, “Understanding Adult BMI” and we talked for 5 minutes about exercise and how she can use her albuterol inhaler to treat exercise-induced symptoms if they arise. Additionally, Mrs. H states that she receives an annual physical exam with her PCP that includes a pelvic exam, Pap smear and lab work. Patient denied any additional questions and was informed to call our office if she is not experiencing adequate control of her symptoms. In the event of a severe attack, Mrs. H is to call 911 and see emergent care. Patient agreed to our plan and was scheduled to follow up with our office in six months if no acute issues arise. 25/30 Vanessa G Wittstruck, PA-S 7/23/12 20:32