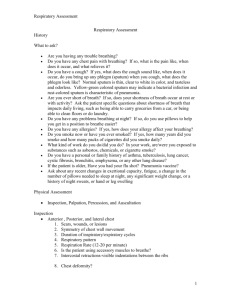
Respiratory – 9 - Student Nurses Association: UCF Orlando Campus
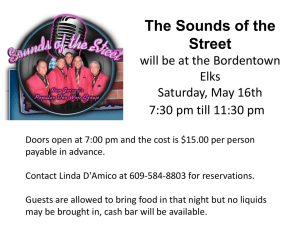
advertisement

Health Assessment – Exam 2 Respiratory – 9 A&P Review Bony Structures Suprasternal notch Sternum Manubrium Manubrial – sternal angle (Angle of Louis): consistent with 2nd rib Xiphoid process Costal Angle (<90°): If greater than 90°, that means thicken chest wall (evidence of barrel chest wall from hypoxia, COPD, etc). Landmarks Vertebra prominence (C7): base of neck Spinous processes Inferior angle of scapula 12th rib Anterior, posterior, and midaxillary lines, midsternal line, MCL Thoracic Cavity Mediastinum Esophagus, trachea, heart, great vessels Lung borders Apices (upper side) 3-4 cm above clavicle Bases Rest on diaphragm at 6th rib Lobes of the Lungs Paired but not symmetric Right: shorter 3 lobes Left: narrower 2 lobes; no middle lobe Anterior: mostly upper/mid lobes Posterior: all lower lobes; oblique fissure Pleura – forms an envelope Parietal: lines chest wall and diaphragm Vacuum, negative pressure holds to chest wall. Positive pressure would make them fall. Pleurisy (pleuritis – caused by infection, causes painful respirations) Trachea and Bronchial Tree Trachea Anterior to esophagus 10-11 cm long in an adult Bifurcates just below the sternal angle (T4-T5): carina, landmark for trach suction Right main stem is shorter and straighter Implications: If a child swallows a nickel, it goes there. Aspirations in right mid/lower lung Bronchial tree Protects alveoli from particulate matter Goblet cells – traps particles Cilia – sweep particles upward Acinus Bronchioles alveolar ducts alveolar sacs alveoli (grape like cluster) Function of Respiration Supply oxygen Remove CO2 Hypoventilation: increased retention of CO2, slow shallow breathing – causes buildup of CO2 in blood Hyperventilation: blows off CO2, rapid deep breathing, causes CO2 to be blown off Maintains homeostasis (pH balance) Maintains heat exchange Involuntary control of respirations In response to cellular demands Mediated by the respiratory center in the brainstem Pons and medulla Major feedback loop is humoral regulation (change in carbon dioxide and oxygen levels in the blood and the hydrogen ion level (less important) Normal stimulus to breathe for most of us is an increase of carbon dioxide in the blood (hypercapnia). A decrease of oxygen in the blood (hypoxemia) also increases respirations but is less effective than hypercapnia. Mechanisms of Respiration Inspiration Diaphragm flattens, lungs expand, chest size increases Vertical and AP diameter increase Expiration Diaphragm relaxes; dome is up, chest recoils Diameters decrease Brainstem increase in CO2 (hypercapnia) + decrease in O2 (hypoxemia) regulates respiratory drive Subjective Data Cough Description: hacking, dry, wet, spasmodic (coughing nonstop for minutes), barking Sputum (does anything come up?): clear (good), rust (TB/Klebsiella), yellow/green (bacteria/pseudomonas – CF), pink frothy (pulmonary edema), hemoptysis (blood from lungs, not blood from chronic irritation of esophagus). Timing: night (ex: allergies to bedding), day, location (allergens), meals. Relief? Associated symptoms? Ex: post ptusive emesis: coughing so hard you vomit Shortness of Breath (SOB): allergens, orthopnea (difficulty breathing when supine), exercise intolerance, apnea, PND (paroxysmal nocturnal dyspnea – different breathing at night, sleep in recliner or propped up) Chest pain r/t breathing (not necessarily cardiac) History of frequent acute symptoms? Chronic lung conditions? Ex: emphysema, TB, cystic fibrosis, allergies, etc. Unplanned weight changes? FHx of lung disease? SHx Occupational/mask? Tobacco? Amount (ppd and pack years) Duration Quit attempts 2nd hand smoke Health Promotion TB testing: last time, results? Smoking cessation Lung protection (ex: masks) Pneumococcal vaccine and flu vaccine Recommended for adults with chronic medical conditions, residents of nursing homes and group car, health care workers, and those who are immunosuppressed. Assessment Techniques Basic: hands, eyes, ears, stethoscope Not necessary for basic patient: PFT, peak flow meter, incentive spirometer, pulse oximeter, x-ray, MRI, CT, VQ perfusion scan, D-dimer (used to rule out hypercoagulability) Inspect Thoracic cage – AP : Transverse diameter is 1 : 2 Shape: pectus excavatum, pectus carinatum (pigeon chest), scoliosis, kyphosis Pectus excavatum- hollowed chest is the most common congenital deformity of the anterior wall of the chest, in which several ribs and the sternum grow abnormally. This produces a caved-in or sunken appearance of the chest. It can either be present at birth or not develop until puberty. Pectus carinatum- opposite of pectus excavatum, characterized by the protrusion of the sternum and ribs. Evidence of scoliosis, kyphosis Musculoskeletal can impact breathing; bad curvature impacts lung expansion Symmetry Unequal chest expansion occurs with marked atelectasis, lobar pneumonia, pleural effusion; with thoracic trauma, such as fractured ribs or with pneumothorax. A lag in expansion occurs with atelectasis, pneumonia, and postoperative guarding. Bulging indicates trapped air as in the forced expiration associated with emphysema or asthma. Respirations – even, labored? Gasping for breath? Abdominal breathing (normal in children) could signal respiratory distress in adults. Noisy breathing occurs with severe asthma or chronic bronchitis Rapid respiratory rates accompany pneumonia, fever, pain, heart disease, and anemia Accessory muscles: flaring, grunting, retractions (working extra hard, intercostal muscles pull) Body positioning: head bobbing + tripod = respiratory distress Facial expressions COPD: tense, strained, tired face. Pursed lips in a whistling position – by exhaling slowly and against a narrow opening, the pressure in the bronchial tree remains positive and fewer airways collapse. Cerebral hypoxia: excessive drowsiness or by anxiety, restlessness, and irritability. hypoxia altered level of consciousness Skin, mucous membrane, nails, nail bed color, and condition Nails: blue/purple = bad Cold environment could be a factor Circumoral cyanosis: blue around mouth Acrocyanosis: blue fingers and toes Cherry red: due to carbon monoxide poisoning Clubbing: nail bed degree is prominent Chronic hypoxia: thick, spongy nail bed Patterns of Respirations Eupnea: 10-20 breaths per minute Apnea: stopped breathing for more than 20 seconds Bradypnea: less than 10 breaths per minute Tachypnea: more than 24 breaths per minute Sighing: done occasionally to purposely expand lungs; if done constantly there may be a psych component Hyperventilation (rate/depth) Hypoventilation: shallow Cheyne-Stokes (waxe/wane): regular pattern (fast/slow); seen in persons with severe heart failure, renal failure, meningitis, drug overdose, ICP A cycle in which respirations gradually wax and wane in a regular pattern, increasing in rate and depth and then decreasing. Breathing periods last 30-45 seconds, with periods of apnea (20 seconds) alternating the cycle. Cycle where see respirations wax/wane in regular pattern- kinda slow, kinda fast Consistent with heart failure, renal failure, meningitis, drug overdose, increase intracranial pressure Occurs normally in infants and aging persons during sleep Biot’s (irregular waxe/wane): due to head trauma, brain abscess, heat stroke, encephalitis A series of normal respirations (3-4) are followed by a period of apnea. The cycle length is variable, lasting anywhere from 10 secs- one minute. Seen with head trauma, brain abscess, heat stroke, spinal meningitis, encephalitis Palpate Symmetric thoracic expansion – around 12th rib Asymmetric expansion occurs with diaphragmatic hernia or pneumothorax. Tenderness, moisture, lumps, masses Tactile fremitus – elicit vibrations (do both sides at the same time) Palms, base fingers, ulnar edge of hands “99” or “Blue Moon” Apices compare bilaterally Vibration increases (i.e. pneumonia) with compression or consolidation and decreases with obstruction (i.e. obstructed bronchus, pneumothorax, emphysema, pleural effusion Decreased fremitus: occurs when anything obstructs transmission of vibrations (i.e. obstructed bronchus, pleural effusion or thickening, pneumothorax, or emphysema). Any barrier that comes between the sound and your palpating hand will decrease fremitus. Increased fremitus: occurs with compression or consolidation of lung tissue (i.e. lobar pneumonia). This is present only when the bronchus is patent and when the consolidation extended to the lung surface. Note that only gross changes increase fremitus. Small areas of early pneumonia do not significantly affect fremitus. Rhonchal fremitus: palpable with bronchial secretions Pleural friction fremitus: palpable with inflammation of pleura Percussion Resonance: ICS Hyper-resonance: over inflated (i.e. emphysema or pneumothorax) Normal for infant or small child; not adults Hypo-resonance (dullness): density Mass? Tumor? Obese? Dull (over diaphragm) or flat (over bone) Abnormal density in the lungs occurs with pneumonia, pleural effusion, atelectasis, or tumor. Lung fields, liver, cardiac borders (anterior) Map diaphragmatic excursion (length/movement) with expiration > inspiration = 3-5 cm posteriorly Purpose: diaphragm function/movement Begin at apices and move down bilaterally every 5 cm Avoid scapula and ribs Listen for resonance to change into dullness and mark spot First: exhale and hold diaphragm is up Second: inhale and hold diaphragm is down High level of dullness and absence of excursion. These occur with pleural effusion (fluid in the space b/w the visceral and parietal pleural) or atelectasis of the lower lobes. Auscultation Presence Note: Clear vs. “don’t hear anything” Silent chest means no air is moving in or out, which is an ominous sign. Immobile diminished sounds Decreased or absent breath sounds occur: When the bronchial tree is obstructed at some point by secretions, mucus plus, or a FB In emphysema as a result of loss of elasticity in the lung fibers and decreased force of inspired air; also, the lungs are already hyperinflated so the inhaled air does not make as much noise. When anything obstructs transmission of sound between the lung and your stethoscope, such as pleurisy or pleural thickening, or air (pneumothorax) or fluid (pleural effusion) in the pleural space. Increased breath sounds occur when consolidation (i.e. pneumonia) or compression (i.e. fluid in the intrapleural space) yields a dense lung area that enhances the transmission of sound from the bronchi. Symmetry: side to side comparison Background noises Be careful, hair sounds like rhonchi. Make sure to wet hairy chests with water prior auscultation. Normal breath sounds Bronchial: tracheal/larynx Loud Bronchovesicular (toward periphery) Major bronchi Vesicular Peripheral lung fields Adventitia Crackles Fine/coarse rales: sounds like rice krispies Moist rhonchi: sounds like snoring, air movement is turbulent Constant or transient atelectasis: don’t last, not pathologic, disappear after first few breaths after sleep Occur in upper lung fields occur with cystic fibrosis; crackles only in lower fields occur with heart failure Wheeze (easiest to hear) Inspiration: signals obstruction Ex: child swallows coin; asymmetrical Expiration: most common; occurs with lower airway obstruction (i.e. asthma or bronchiolitis). When unilateral, it may be foreign body aspiration. Clears with cough? Asthmatic wheezes don’t clear with cough Pleural friction rub: coarse, low-pitch, bradding quality (sounds like 2 pieces of leather rubbing) Ex: pleuritis Stridor: high-pitched inspiratory crowing sound heart without the stethoscope, occurring with upper airway obstruction (i.e. croup, FB aspiration, or acute epiglottitis). Bronchophony: “99” Dull vs. clear Normal: dull, increased lung density, generated by larynx Egophony: “ee-ee-ee” “ee” vs. “aa” A areas of consolidation (i.e. pneumonia) Whispered pectoriloquy Dull vs. clear Normal: dull Developmental Infants and Children Surfactant: surface tension, lipid substance needed to inflate alveoli, produced at 32 weeks gestation. Premature babies need exogenous/artificial surfactant because they cannot expand their lungs. 70 million alveoli (vs. 300 million in adults) Increased risk if exposed to irritants such as second hand smoke Cutting cord activates respirations via change in circulation from adult to fetus Inspect (similar to adult) Shape and symmetry Rounded thorax/belly Barrel shape persisting after age 6 years, which may develop with chronic asthma or cystic fibrosis. Harrison’s groove occurs normally, but also occurs with rickets from the pull of the diaphragm on weakened ribs. Ribs/xiphoid prominent (especially if they’re skinny) Apgar score (3-6 is moderate; 0-2 indicates a several depressed newborn needing full resuscitation, ventilation assistance, and subsequent intensive care) Appearance Pulse Grimace (reflex irritability) Respiratory effort Muscle tone Palpate: look for lumps, masses, crepitus (especially over clavicle if fractured at birth) Crepitus: coarse, crackling sensation palpable over the skin surface. It occurs in subcutaneous emphysema when the air escapes from the lungs and enters the subcutaneous tissue, as after open thoracic injury or surgery. Palpable around fracture clavicle, which may occur with difficult forceps delivery Percussion will be hyper-resonant (normal), limited usefulness – auscultation is better. Obligate nose breathers 3 months; they don’t know how to breath out of their mouth until then Abdominal breathing (vs. thoracic in adults) Respiration rate: 30-40+ (listen for full minute b/c irregular) Bronchovesicular sounds until 5-6 years Fine crackles immediate new period because opening lungs for first tie Note: When listen to pediatric patients, if you hear wheezing or rhonchi – don’t stop. Next put the stethoscope over the nose/mouth and compare the sounds. If they’re the same, signals upper respiratory congestion moved to lungs. This is not a problem. Everything is magnified in peds. Tachypnea of 50-100 per minute in infants during sleep may be an early sign of heart failure. Pregnancy Wider thorax Deeper respirations Elevated diaphragm Increased total circumference Increased tidal volume Increased awareness of need to breathe Aging Rigid thorax: poor chest expansion Decreased vital capacity Prone to atelectasis Acute respiratory failure barrel chest (thickened chest wall; greater than 90 degrees costalsternal angle) Kyphosis (impacts breathing) Easily fatigued, during tests – don’t rush causing them to hyperventilate Decreased chest expansion Increased risk post-op complications due to decreased lung expansions Pathology Name Pneumothorax Pleural Effusion Asthma Condition Assessment Free air in pleural space causes partial or complete lung collapse. Air in pleural space neutralizes the usual negative pressure present; thus lung collapses. Usually unilateral. Pneumothorax can be: 1) Spontaneous: air enters pleural space through rupture in lung wall. 2) Traumatic: air enters through opening or injury in best wall. 3) Tension: trapped air in pleural space increases compressing lung and shifting mediastinum to the unaffected side. Collection of excess fluid in the intrapleural space, with compression of overlying lung tissues. Effusion may contain watery capillary fluid (transudative), protein (exudative), purulent matter (empyemic), blood (hemothorax), or milky lymphatic fluid (chylothorax). Gravity settles fluid in dependent areas of thorax. Presence of fluid subdues all lung sounds. I: unequal chest expansions. If large, tachypnea, cyanosis, apprehension, bulging in interspaces. Pal: Tactile fremitus decreased or absent. Tracheal shift to opposite side (unaffected side). Chest expansion decreased on affected side. Tachycardia, decreased Bp. Per: hyperresonant. Decreased diaphragmatic excursion. A: Breath sounds decreased or absent. Voice sounds decreased or absent. None I: Increased respirations, dyspnea; may have dry cough, tachycardia, cyanosis, abdominal distention. Pal: Tactile fremitus decreased or absent. Tracheal shift away from affected side. Chest expansion decreased on affected side. Per: Dull to flat. No diaphragmatic excursion on affected side. A: Breath sounds decreased or absent. Voice sounds decreased or absent. When remainder of lung is compressed near the effusion, may have bronchial breath sounds over the compression along with bronchophony, egophony, whispered pectoriloquy. I: During severe attack increased resp. rate, SOB with audible wheeze, use of accessory neck muscles, cyanosis, apprehension, retraction of intercostal None Allergic hypersensitivity to certain inhaled allergens (ex: pollen), irritants (ex: tobacco, ozone), microbes, stress, or exercise that produces a complex response Adventitia Bilateral wheezing on expiration, sometimes inspiratory and Bronchitis Lobar Pneumonia TB Bronchal Pulmonary Dysplasia Cystic Fibrosis characterized by bronchospasm and inflammation, edema in walls of bronchioles, and secretion of highly viscous mucus into airways. These factors greatly increase airway resistance, especially during expiration, and produce symptoms of wheezing, dyspnea, and chest tightness. Proliferation of mucus glands in the passageways, resulting in excessive mucus secretion. Inflammation of bronchi with partial obstruction of bronchi by secretions or constrictions. Sections of lung distal to obstruction may be deflated. Bronchitis may be acute or chronic with recurrent productive cough. Chronic bronchitis is usually caused by cigarette smoking. Infection in lung parenchyma leaves alveolar membrane edematous and porous, so RBCs and WBCs pass from blood to alveoli. Alveoli progressively fill up (become consolidated) with bacteria, solid cellular debris, fluid, and blood cells, which replace alveolar air. This decreases surface area of the respiratory membrane, causing hypoxemia. Inhalation of tubercle bacilli into the alveolar wall starts: 1) Initial complex is acute inflammatory response – macrophages engulf bacilli but do not kill them. Tubercle forms around bacilli. 2) Scar tissue forms, lesion calcifies, and shows on x-ray. 3) Reactivation of previously healed lesion. Dormant bacilli now multiply, producing necrosis, cavitation, and caseous lung tissue (cheeselike). 4) Extensive destruction as lesion erodes into bronchus, forming airfilled cavity. Apex usually has most drainage. spaces. Expiration labored, prolonged. If chronic, may have barrel chest. Pal: Tactile fremitus decreased, tachycardia. Per: Resonant. If chronic, may be hyperresonant. A: Diminished air movement. Breath sounds decreased, with prolonged expiration. Voice sounds decreased. I: hacking, rasping cough productive of think mucoid sputum. Chronic dyspnea, fatigue, cyanosis, possible clubbing of fingers. Pal: Tactile fremitus is normal. Per: Resonant A: Normal vesicular. Voice sounds normal. Chronic prolonged expiration. expiratory wheezing. I: Increased resp. rate. Guarding and lag on expansion on affected side. In children – sternal retraction, nasal flaring. Pal: chest expansion decreased on affected side. Tactile fremitus increased if bronchus patent, decreased if bronchus obstructed. Per: Dull over lobar pneumonia. A: breath sounds louder with patent bronchus, as if coming directly from larynx. Voice sounds have increased clarity; bronchophony, egophony, whispered pectoriloquy present. In children – diminished breath sounds may occur early in pneumonia. Usually asymptomatic, showing as positive skin test or x-ray. Progressive TB involve weight loss, anorexia, easily fatigued, lowgrade afternoon fevers, night sweats. May have pleural effusion, recurrent lower respiratory infections. I: cough initially nonproductive, later productive of purulent, yellow-green sputum, may be blood tinged. Dyspnea, orthopnea, fatigue, weakness. Pal: Skin moist at night from night sweats. Per: Resonant initially. Dull over any effusion. A: Normal or decreased vesicular breath sounds. Crackles – fine to medium. Crackles over deflated areas. May have wheeze. Crackles over upper lobes common, persist following full expiration and cough. Congestive Heart Failure Pump failure with increasing pressure of cardiac overload causes pulmonary congestion or an increased amount of blood present in pulmonary capillaries. Dependent air sacs are deflated. Pulmonary capillaries engorged. Bronchial mucosa may be swollen. COPD/ Emphysema Emphysema: Destruction of pulmonary connective tissue (elastin, collagen); characterized by permanent enlargement of air sacs distal to terminal bronchioles and rupture of interalveolar walls. This increases airway resistance, especially on expiration – producing a hyperinflated lung and an increase in lung volume. *cigarette smoking accounts for 8090% of emphysema cases. I: Increased resp. rate, SOB on exertion, orthopnea, paroxysmal nocturnal dyspnea, nocturia, ankle edema, pallor in lightskinned people. Pal: skin moist, clammy. Tactile fremitus normal. Per: Resonant. A: Normal vesicular. Heart sounds include S3 gallop. I: increased AP diameter. Barrel chest. Use of accessory muscles to aid respiration. Tripod position. SOB, esp. on exertion. RD. Tachypnea. Pal: decreased tactile fremitus and chest expansion. Per: Hyperresonant. Decreased diaphragmatic excursion. A: Decreased breath sounds. May have prolonged expiration. Muffled heart sounds resulting from overdistention of lungs. Cardiovascular – 13 A&P Review Structures Endocardium Myocardium: muscular, “pumper” Pericardium: fibrous, protective Positioning Mediastinum: center of chest wall Base: at the top Apex: at the bottom left 5th ICS L. MCL Can change (i.e. in peds it may be in 4th ICS) Dextracardia: things are flipped; heart is on right side Blood Flow Crackles at lung bases. Usually none, occasionally wheeze. Cardiac Output CO = HR x SV (amount of blood pumped by LV in one contraction) Preload: filling/relaxation Afterload: contraction Conduction system (ventricular innervations) SA node AV node Bundle of His R/L bundle branches Subjective PHx Cardiac disease/surgeries? FHx CVD? Who? What Age? Ex: PGF died at 42 from acute MI Congenital (ex: atrial septal defect) or acquired disease (rheumatic fever)? HTN? Obesity? DM? CAD? Sudden death at younger age? SHx Habits? Smoking, drinking, poor nutrition, activity, occupation (ie: desk job = no activity) Non-modifiable risks for heart disease: FHx, gender, age, genetics Modifiable risks: lifestyle, diet, exercise Risk factors for CAD: elevated cholesterol and BP, blood sugar levels above 130 mg/dL or DM, obesity, cigarette smoking, low activity level, and length of any hormone replacement therapy for postmenopausal women. Meds? Cardiac meds, antihypertensives, or med w/ cardiac side effects ROS Chest pain? PQRSTU Palliative: stop movement, rest, nitroglycerine / provocative: exertion, stress Quality: male vs. female M: “Feels like an elephant sitting on chest” crushing/squeezing feeling F: pain in jaw, back of neck, and arm; nausea/vomiting Region and radiation: jaw, shoulder Severity Timing: When did it start? What were you doing? Understanding patient’s perspective: What do you think happened? Associated symptoms: diaphoresis, vomit, nausea Acute MI: necrosis of heart cells Peripheral Leg pain/cramp with or without activity? Distance? Claudication – could be intermittent; cramping pain in the leg is induced by exercise, typically caused by obstruction of the arteries. Skin changes or hair loss on feet or legs? Ex: DM with peripheral artery disease no walking barefoot PAD: thin, shiny skin with no hair. Nails are very thick/deformed. No good circulation. Palpitations: possible due to caffeine Dyspnea [on exertion (DOE)]: out of breath Paroxysmal nocturnal dyspnea (PND) occurs with heart failure. Lying down increases volume of intrathoracic blood, and the weakened heart cannot accommodate the increased load. Typically, the person awakens after 2 hours of sleep with the perception of needing fresh air. Orthopnea: difficulty breathing laying flat use pillows or recliner Cough? Hemoptysis is often a pulmonary disorder but also occurs with mitral stenosis. Fatigue? R/T decreased CO is worse in the evening. Cyanosis or pallor? Occur with MI or low CO as a result of decreased tissue perfusion. Edema? Dependent when caused by heart failure, worse in the evening and better in the morning after elevating legs all night, bilateral (unilateral swelling has a local vein cause) Nocturia? Getting up at night to pee (i.e. congestive heart failure) Health promotion BP checks Cholesterol screening Weight/BMI Activity Nutrition DASH diet Fat intake Objective Precordium/Chest Wall Inspect Heaves or lifts: indicates over activity; look at apex area in the left sternal border Hyperdynamic precordium or active precordium which signals left ventricular hypertrophy (LVH) LVH: diffused left lifting pulse Palpate Thrills: palpable vibration at PMI, apex impulse, apical pulse, 5th ICS MCL. Feels like throat of a purring cat – turbulent blood flow. Heave + thrill = murmur (must auscultate) Carotid Artery Carotid sinus hypersensitivity is the condition in which pressure over the carotid sinus leads to a decreased heart rate and BP, and cerebral ischemia with syncope. The may occur in older adults with hypertension or occlusion of the carotid artery. Apical Pulse Note location, size, amplitude, and duration LV dilation displaces impulse down and to the left and increases size more than one space. A sustained impulse with increased force and duration but no change in location occurs with LV hypertrophy and no dilation (pressure overload) Not palpable with pulmonary emphysema due to overriding lungs. Percuss (limited usefulness) Size and location (not children or obese) Cardiomegaly d/t increased ventricular volume or wall thickness; it occurs with HTN, CAD, heart failure, and cardiomyopathy. Auscultate (5 locations): Aortic, Pulmonic, Erb’s point (where all sounds come together midpoint), Tricuspid, Mitral APE To Man Auscultate Systematically Sitting then lying; then left side-lying to bring the heart more superficial to hear the extra heart sounds better. Diaphragm then bell Note: rate (reg x2 or full minute) and rhythm S1 and S2 (first), S3 and S4 if applicable Murmurs Pulse deficit - get apical and then radial pulse Signifies a weak contraction of the ventricles; it occurs with atrial fibrillation, premature beats, and heart failure. Apical – radial = 6 to 10 Numbers should be close – if greater than 6 to 10 pulse deficit and signifies AF Pericardial friction rub (pericarditis) Scratchy, rough, grading LLSB or apex Leans forward When auscultating, ask patient to hold breath after expiration to cut out respiratory sounds Heart Sounds Closure of valves Turbulence of blood flow First heart sound: S1 “Lub” Closure of AV valve Systole begins Best heard at the apex Second heart sound: S2 “dub” Closure of semilunar (aortic and pulmonic) valves Systole ends Best heard at base Diminished S1 and S2 d/t condition that place an increased amount of tissue between the heart and your stethoscope: emphysema (hyperinflated lungs), obesity, and pericardial fluid. Split S2 S2 is supposed to be one sound, but sometimes splits because aortic valve closed before the pulmonic. Effect of respirations and pressure gradients: Ask patient to take “deep deep breaths” and if the pressure gradient remains constant or fix that is no bueno. Fixed split is unaffected by respirations. Paradoxical split is where the sounds fuse on inspiration and split on expiration. S3 – pathologic Ventricular gallop Vibration due to rapid ventricular filling Occurs after S2 due to volume (fluid) overload, softer Sounds like “Kentucky” or “Slosh-ing-in” (rare) Low pitch – use bell of stethoscope First sign for CHF S4 – pathologic Atrial gallop Atria contract and push blood into non-compliant ventricle; soft sound Occurs presystole (before S1) Sounds like “Tennessee” or “A-stiff-wall” Low pitch use bell at apex AMI? Ominous sign All 4 heart sounds = train wreck Bruits and Hums Abnormal in adults – extra heart sounds (i.e. in atherosclerosis) Palpate 1 side at a time and auscultate with bell for carotid bruits (=S1) Venous hum in supraclavicular fossa = normal in children due to turbulence in jugular venous system. Murmurs Turbulent blood flow resulting in blowing or swooshing sound Causes: Increased velocity (i.e. increased heart rate – when children have an acute illness, exercise, thyrotoxicosis) Decreased viscosity (i.e. anemia or sickle cells) Structural defects Prolapse (incompetent) Stenosis (narrowing) Defective opening: “leaky pipe” Unusual openings in the chambers (dilated chamber, wall defect) Can hear better in thinner patients Can’t hear as well with obese, muscular, or fluid (due to CHF) filled patients. Functional (not pathological) Murmurs Common in kids Increased blood force and velocity against a thin chest wall “Still’s” murmur = innocent murmur More pronounced with a child who has fever, anemia, or supine 5 Ways to Describe Murmurs Loudness Grade I/VI: barely go undiagnosed II/VI: faint III/VI: moderate IV/VI: loud feel thrills V/VI: very loud VI/VI: can be felt touching the skin and can hear it without a stethoscope. Region and Radiation: localized? Radiate? Pitch: High/Low? Timing: when do you hear it? Systole or diastole Crescendo Decrescendo Pan/Holo: entire S1 or S2? Or just one short portion of S1 or S2? End/Mid Quality Blowing Harsh Rumble: like train, especially if S1 or S4 Jugular Venous Distension (JVD) Supine with HOB 30-45° (no pillow). Use tangential lighting over neck and ask patient to look away; external jugular pulse should be visible. Top of the waveform of the internal jugular venous pulsation = height of the venous distention Imaginary horizontal line (parallel to the floor) is then drawn from this level to above the sternal angle. Use 2 rulers First ruler goes on the Angle of Louis 2nd ruler goes from height of EJV parallel to the floor. Find the number that’s vertical where the rulers intersect and that’s the JVD. More than 4-5 cm from sternal angle to imaginary line = elevated venous pressure CHF Heptojugular Reflux (HJR) Supine with HOB at 45° angle Mouth open, breathes normally Moderate pressure is applied over the middle or RUQ abdominal region for 30-60 seconds Height of the neck veins increases by at least 3 cm and the increase is maintained throughout the compression period HJR Look for distention Greater than 3cm = compromised circulation Pulses Sites (arteries) Temporal, carotid, aorta, brachial, radial, ulnar, femoral, popliteal, dorsalis pedis, posterior tibialis Description 0 absent 1+ weak 2+ normal 3+ increased 4+ bounding Name Weak, Thready, 1+ Full, bounding, 3+ Water Hammer (Corrigan), 3+ Pulsus Bigeminus Pulsus Alternans Pulsus Paradoxus Pulsus Bisferiens See page 519 for visual ABNORMAL PULSES Description Associated With Hard to palpate, need to search Decreased cardiac output, peripheral for it, may fade in and out, arterial disease, aortic valve stenosis easily obliterated by pressure. Easily palpable, pounds under Hyperkinetic states (exercise, anxiety, fingertips fever), anemia, hyperthyroidism Greater than normal force, then Aortic valve regurgitation, patent ductus collapses suddenly arteriosus Rhythm is coupled, every other Conduction disturbance (i.e. premature beat comes early, or normal ventricular contraction, premature atrial beat is followed by premature contraction, dysrhythmia). beat. Force of premature beat is decreased because of shortened cardiac filling time. Rhythm is regular, but force When HR is normal, pulsus alternans varies with alternating beats of occurs with severe left ventricular large and small amplitude failure, which in turn is due to ischemic heart disease, valvular heart disease, chronic hypertension, cardiomyopathy, or CHF Beats have weaker amplitude A common finding is cardiac tamponade with inspiration, strong with (pericardial effusion in which high expiration. Best determined pressure compresses the heart and during blood pressure blocks cardiac output); also in severe measurement; reading bronchospasm of acute asthma decreases (> 10 mmHg) during inspiration and increases with expiration. Each pulse has two strong Aortic valve stenosis plus regurgitation, systolic peaks, with a dip in AF between. Best assess at carotid artery. Inspection Temperature Is there a difference between R/L? Sores or lesions Edema Measure bilat Pitting: 1+ (mild) 4+ (deep) Color Pallor Rubor – red Cyanosis – blue Brawny (v. stasis) – brown Varicosities Auscultate for bruits over abdomen Pincer grasp for AAA (abdominal aortic aneurysm) Developmental Pregnancy Increase HR, blood volume (by 30-40%), cardiac output Edema Varicosities r/t decrease in arterial pressure BP lowest 2nd trimester then increases (especially in 3rd trimester) Preeclampsia: pregnancy induced hypertension (PIH) Lie left lateral to decrease BP due to oxygenation PIH: Greater than 30 mmHg increase systolic or greater than 15 mmHg increase diastolic Aging Lifestyle (smoking, diet, alcohol, exercise and stress) Increased systolic BP d/t stiffening of large arteries arteriosclerosis difficulty feeling pulses Left ventricular wall thickens increased workload Decreased response to exercise (orthostasis) Increased incidence arrhythmias and ectopic beats S3 is associated with heart failure and is ALWAYS abnormal over age 35. Infant Initial murmurs PDA – patent ductus arteriosis 10-15 hours after birth, mixing arterial and venous blood PFO – patent foramen ovale 1 hour after birth Treatment: meds or surgery ASD/VSD Truncus arteriosis + Transposition of Great Vessels emergency d/t no oxygenated blood Coarctation of aorta Tetraology of Fallot Stenosis HR 1 minute R = L ventricle size to 1 year and then L:R is the same as adult 2:1 Positioned horizontal with apex at 4th ICS 1 umbilical vein, 2 umbilical arteries Cyanosis at or just after birth signals oxygen desaturation of congenital heart disease. Important signs of heart failure: persistent tachycardia (>200 in newborns, >150 in infants), tachypnea, liver enlargement, engorged veins, gallop rhythm, and pulsus alternans. Respiratory crackles (rales) are an important sign in adults, but not in infants. Apex displacement r/t Cardiac enlargement shift to the left Pneumothorax shifts away from affected side Diaphragmatic hernia shifts usually to the right b/c this heart occurs more often on the left. Dextrocardia (a rare anomaly in which the heart is located on the right side of the chest) Diagnostics EKG Holter – 24 hr EKG Ambulatory BP EST – exercised stress test Chemical stress test – injection Echocardiogram – ultrasound of heart Angiography – note any areas of blockages Cardiac enzymes – lab test to rule out MI Allen test – radial and ulnar artery patency The hand is elevated and the patient/person is asked to make a fist for about 30 seconds. Pressure is applied over the ulnar and the radial arteries so as to occlude both of them. Still elevated, the hand is then opened. It should appear blanched (pallor can be observed at the finger nails). Ulnar pressure is released and the color should return in 7 seconds. If color does not return or returns after 7–10 seconds, the test is considered negative and the ulnar artery supply to the hand is not sufficient. The radial artery therefore cannot be safely pricked/cannulated. Homan’s Test – rule out deep vein thrombosis (DVT) leg circumference, >1 cm difference D-dimer Ankle/Brachial Index (ABI): < 0.9 = PVD) Doppler A/V (C)HF Causes AMI HTN Valvular disease Thyroid disease S/S Skin-ashen, diaphoretic SOB/DOE, orthopnea, paroxysmal nocturnal dyspnea (PND) Crackles Hypotension Edema, ascites Nausea/vomiting Anxiety Change in level of consciousness JVD S3, tachy, deviated PMI Decreased urinary output Gastrointestinal – 15 Karen c/o abdominal pain P: What brought on the pain? Q: How does it feel? Sharp, stabbing, dull? R: Region or radiation S: Scale out of 1 to 10 T: How long does it last? When does it occur? U: What do you think it means? Subjective Weight changes? Is it planned? Diet? Anorexia: in elderly, loss of appetite (not psychiatric) Could be r/t GI disease, pregnancy, or psychological Appetite? Dysphagia? Difficulty swallowing – solids? Liquids? Seen in disorders of the throat/esophagus Food intolerance? Ex: lactose intolerance (common in Asians) (50% of Mexican Americans and 80% of AA) Symptoms: what can you tolerate? What happens? Do you use antacids? Is there belching (eructation), bloating, heart burn? Abdominal pain May be visceral from an internal organ (dull, general, poorly localized); parietal from inflammation of overlying peritoneum (sharp, precisely localized, aggravated by movement); or referred pain. Acute pain requiring urgent diagnosis occurs with appendicitis, cholecystitis, bowel obstruction, or a perforated organ. Chronic pain of gastric ulcers occurs on an empty stomach, pain of duodenal ulcers occurs 23 hours after a meal and is relieved by more food. Nausea/Vomiting Frequency? Timing? Hematemesis: bloody vomit; occurs with stomach or duodenal ulcers and esophageal varices. Associated symptoms? Colicky pain, diarrhea, fever? R/T food poisoning, GI disease, meds, and early pregnancy Bowel habits Frequency? Constipation? Color: black stools may be tarry due to occult blood (melena) from GI bleeding or non-tarry from iron medications. Gray stools occur with hepatitis. Consistency? Any bleeding? Changes Bleeding Hematochezia (frank) – lower GI bright blood (i.e. hemorrhoid) Melena or tarry (occult) – upper GI dark blood PHx? Surgeries related to GI system? (i.e. appendectomy, cholestectomy) FHx? CA, polyps, IBD, IBS Medication Antacids (i.e. pepto) NSAIDS r/t peptic ulcer disease FE+ (cause constipation) ETOH (alcohol) – ask how much is consumed Hemorrhoids – when people have enlarged veins in the rectum Pruritis ani – anal itching (could be caused by hemorrhoids or coffee, tea, and citrus can irritate the anus) Fistulas – abnormal passageway between organs and vessels Ex: tunnel between anal gland and access on skin. Nutritional assessment: What are they eating? 24 hour diet recall is important. Tobacco? ETOH? Caffeine? Developmental Infants/Children Breast milk vs. formula Whole milk at 1 year Introduction to solid foods – what age? Fe+ formula supplement Pica: when children eat nonfoods like dirt and grass Teens Eating patterns: regular meals? Snacks? Junk food? Exercise habits? Exercise is often hyperactive. Body image: “What/how do you think your body looks like?” Anorexia nervosa: patient refuses to maintain body weight; extreme fear of gaining weight. Boys need 4000 cal/day, girls need 20% less Aging Adults Pernicious anemia: vitamin B12 due to lack of intrinsic factor. Weight changes – start to lose weight Bowel preoccupation: ask about bowel patterns, constipation, and fluid/fiber intake. Achalasia Decreased esophageal peristalsis and LES constriction: esophagus becomes weak and is less able to transport food. Esophageal emptying is delayed, and if fed in a supine position – increased risk for aspiration. Dysphagia constipation r/t lack of liquid Constipation is caused by decreased physical activity, inadequate intake of water, a lowfiber diet, side effects of meds, IBS, bowel obstruction, hypothyroidism, and inadequate toilet facilities. Salivation decreases, causing a dry mouth and a decreased sense of taste Pregnancy N/V r/t hormone changes Heart burn (pyrosis) r/t esophageal reflux Decreased gastric motility constipation and hemorrhoids Bowel sounds are diminished Objective Patient preparation: Have adequate lighting to visualize abdomen Empty bladder to listen (Specimen?) Warm room, stethoscope, and hands Cold hands = tensing Abdomen: supine with knee bent Rectal: Male: Left lateral recumbent or standing forward flexed Female: Left lateral or lithotomy Quadrants Epigastrum, Hypogastrum (Suprapubic), Periumbilical RUQ: liver gallbladder, duodenum, head of pancreas, right kidney & adrenal gland, hepatic flexure of colon, part of ascending colon and transverse colon. LUQ: Stomach, spleen, left lobe of liver, body of pancreas, left kidney & adrenal gland, and splenic flexure of colon, part of tranverse and descending colon RLQ: Cecum, appendix, right ovary and tube, right ureters, and right spermatic cord LLQ: Part of descending colon, sigmoid colon, left ovary and tube, left ureter, and left spermatic cord. CVA: costovertebral angle Retroperitoneal Inspect Auscultate Percuss Palpate Inspection Demeanor Relaxed vs. agitated Abdomen Contour Scaphoid: concave Flat Rounded Protuberant Distended (convex) Fat Fluid (ascites) Flatus: gas Feces Fetus Fatal (malignancy): cancer Fibroids Pulsations: may see aortic in thin people (normal) Marked pulsation occurs with widened pulse pressure (i.e. HTN, aorta insufficiency, thryrotoxicosis) and aortic aneurysm. Waves of peristalsis: marked visible peristalsis with a distended abdomen indicated intestinal obstruction. Skin: Lesions/rash/color/scars Striae: stretch marks (d/t rapid weight gain, pregnancy, ascites); look purple-blue with Cushing syndrome. Color Redness: localized inflammating Jaundice Skin glistening and taut ascites Cutaneous angiomas (spider nevi) occur with portal hypertensions or liver disease. Prominent, dilated veins occur with portal hypertension, cirrhosis, ascites, or vena cava obstruction. Veins are more visible with malnutrition as a result of thinned adipose tissue. Poor turgor accompanies GI disease and occurs with dehydration. Symmetry: should be symmetric bilaterally Bulges? Masses? Hernia – protrusion of abdominal viscera through abnormal opening in muscle wall. Umbilicus Everted with ascites or underlying mass. Deeply sunken with obesity. Enlarged, everted with umbilical hernia Bluish periumbilical color occurs with intra-abdominal bleeding (Cullen sign) Rectal Anal fissures Hemorrhoids Rectal discharge Prolapse Papilloma (condyloma): warts caused by HPV Imperforate anus: no anus After birth, the meconium (first poop) must be defecated, and in IA it can’t. Surgery required. Auscultate Bowel Sounds (BS) Press lightly with warmed diaphragm All 4 quadrants begin RLQ (ileocecal) then go clockwise BS always here normally Note: Character & Frequency Normal (5-30x/min) Hyperactive: loud, high-pitched, rushing, tinkling sounds that signal increased motility. Borborygmus, stomach growling Hypoactive or absent: follow abdominal surgery or with inflammation of peritoneum Absent (0 x5’) have to listen for 5 minutes in each quadrant to be able to say that. Vascular Sounds Press more firmly Vascular Sounds Bruits (normal in children) heard in patients with heart failure and hypertension. Aorta Renal Iliac Femoral Percuss All 4 quads Tympany predominates; dull = solid Dulls occurs over distended bladder, adipose tissue, fluid, or a mass. Hyperresonance is present with gaseous distention. Liver Span, resonance to dull. Then tympany to dull; typical 6-12 cm enlarged liver span indicates hepatomegaly. Percuss CVAT - direct or indirect. Should not be tender – sharp pain occurs with inflammation of the kidney or paranephric area. Percuss splenic dullness – 9-11th ICS L MAL A dull note forward of midaxillary line indicates enlargement of the spleen, as occurs with mono, trauma, and infection. A change in percussion from tympany to a dull sound with full inspiration is a positive spleen percussion sign, indicating splenomegaly. This method will detect mild to moderate enlargement before spleen becomes palpable as in mono, malaria, and hepatic cirrhosis. Special procedures Fluid wave test (to differentiate ascites from gaseous distention) S/S: distended abdomen, bulging flanks, and an umbilicus that is protruding and displaced downward. Ascites occurs with heart failure, portal HTN, cirrhosis, hepatitis, pancreatitis, and CA. Shifting dullness Positive with a large volume of ascitic fluid; it will not detect less than 500 mL of fluid. Palpate Palpate for: enlargements and masses Note: Size, location, shape, consistency, surface, mobility, pulsatility, tenderness, guarding, rigidity, and masses. Involuntary rigidity is a constant, board-like hardness of the muscles. It is a protective mechanism accompanying acute inflammation of the peritoneum. It may be unilateral, and the same area usually becomes painful when the person increases intra-abdominal pressure by attempting a sit up. Tenderness occurs with local inflammation, inflammation of the peritoneum or underlying organ, and with an enlarged organ whose capsule is stretched. Nephroblastoma: tumor in kidney (Wilm’s); non-tender mass; DO NO PALPATE 6 % of all childhood cancers Light then Deep 1cm > 5-8cm Use palmar surface fingers; clockwise motion around abdomen Bimanual technique Use in patients with large abdomen (obesity) Retroperitoneal organs Liver (GB) Bimanual technique Duck bill: used to palpate liver 1-2 cm below costal margin Alternative Hooking Technique to palpate the lower margin of liver Murphy’s sign: “take a deep breath” Inspiration depresses liver/GB for palpation under costal margin When test positive, as the descending liver pushes into the inflamed gallbladder onto the examining hand, the person feels sharp pain and abruptly stops inspiration midway. Aorta Palpate just to L of umbilicus w/ opposing fingers Normal= 2.5 to 4 cm wide “AAA” Abdominal Aortic Aneurysm: aorta develops weakness and becomes enlarged. Kidneys/Adrenal Bimanual (AP) technique Slide hands laterally May palpate R lower pole No changes felt with deep inspiration Spleen Bimanual AP, left hand on the left side of 11th to 12th rib. Ask patient to take a breath Only palpable when 3x normal size Spleen enlarges with mononucleosis, trauma, leukemias, and lymphomas. A large spleen is friable and can rupture easily with over palpation. Roll side lying right Palpation Hints “I’m going to inspect this now.” Tender area last Voluntary guarding vs. involuntary rigidity Keep Knees bent Ticklish? Do self-palpation and join them Anus, Rectum & Prostate Position: lateral recumbent (L side/R knee flexed) Dorsal lithotomy Forward over table Anus Check sphincter tone (anal wink) Gloved index finger w/ lubricant Check for hemorrhoids (int/ext) Prostrate Valsalva; when they take a deep breath, bear down, and check prostate. Prostate @ 2.5x4 cm Smooth Rubbery Non-tender Heart shaped Check for masses Rectum Examine stool Color/consistency Guaiac-occult blood: testing for blood in the stool Abnormal: Jelly-inflammation (i.e. when one intestine telescopes into another) Bright red (hematochezia)-lower GI Tarry (melena) DARK- upper GI Black-Fe+, Pepto Gray/tan-hepatobilliary Greasy/fatty-malabsorption Called steatorrhea Developmental Changes Infants/Children Umbilical = 2A 1V Jelly stool (intussuception) Large liver & most organs palpable For years and younger: Protuberant (pot belly) sitting/lying After four: flat laying supine. BS only, no vascular sounds on auscultation; don’t percuss over spleen Diastasis recti: separation of rectus muscles with a visible bulge along the midline; normal variation; more common in black infants – refer if it lasts more than 6 years. Umbilical hernia appears 2-3 weeks, reaches maximum size at 1 month, and disappears by 1 year. Refer any umbilical hernia larger than 2.5 cm, one that continues to grow after 1 month, or one lasting more than 2 years in a white baby and more than 7 years for a black baby. Scaphoid abdomen in a child is associated with dehydration or malnutrition. Younger than 7 years, the absence of abdominal respirations occurs with inflammation of the peritoneum. Aging Adult Inc. fatty deposits abdomen and hips Muscle atrophy = organs easily palpable liver can be lower, kidneys easy to palpate Referred Pain Special Procedures Rebound tenderness? Peritonitis accompanied with appendicitis (Blumberg’s sign) palpate at 90 degree angle at opposite side of pain. “Karate chop” Normal response: no pain at the release of pressure Pain on release of pressure confirms rebound tenderness, which is a reliable sign of peritoneal inflammation (this accompanies appendicitis). Cough tenderness that is localized to a specific spot also signals peritoneal inflammation – refer pt. with suspected appendicitis for CT. Suspect appendicitis: Obturator Sign: Lie supine lift their right leg up at 90 degree angle and you will hold at their ankle and rotate it internally and externally. Abnormal response is pain. Iliopsoas Sign: Have patient on left side and move leg back. When the iliopsoas muscle is inflamed (which occurs with an inflamed or perforated appendix), pain in felt in the RLQ. Shifting dullness? Ascites Lay them flat then shift them to their side and you will feel fluid upon percussion Signs for liver disease: Jaunidce eyes ictericsclera Bilirubinuria Other Pathologies Umbilical hernia, do sit-up to see if it is a hernia. Diastasis recti Gastroschisis, born with intestine out. Volvulus, really bad tangle Intussusception, two intestines telescope into each other. Omphalocele Important to know Different Signs. Different changes that occur with PEDS and ADULTS Eyes – 7 A&P Parallel axes (conjugate movement) are important because the human brain can only one image. The muscle fibers of the iris contract the pupil in bright light and to accommodate for near vision; they dilate the pupil in dim light and accommodate for far vision. Subjective Data C/C: acuity changes? Blurring? Clouding (cataract)? Floaters? Blind spots? Night blindness? Halos? PHx Vision difficulty? Floaters are common with myopia or after middle age due to condensed vitreous fibers. Usually not significant, but acute onset of floaters (shade or cobwebs) occurs with retinal detachment. Happens in HTN, diabetic retinopathy, and dirty contacts. Halos around lights occur with acute narrow-angle glaucoma. Scotoma: a blind spots surrounded by an area of normal or decreased vision, occurs with glaucoma, optic nerve disorders, and migraines. Night blindness occurs with optic atrophy (decreased visual field), glaucoma, or vitamin A deficiency. Pain? Some common eye diseases cause no pain (i.e. cataract, glaucoma) Photophobia: the inability to tolerate light. Sudden onset of eye symptoms (pain, floaters, blind spot, loss of peripheral vision) is an emergency. Strabismus? Diplopia? Strabismus: deviation in the axis of the eye; unequal placement of the eyes Esotropia: inward deviation Exotropia: outward deviation Diplopia: the perception of two images of a single object Redness? Swelling? Watering? Discharge – color, amount, crusting/matting? Lacrimation and epiphora (excessive tearing) are due to irritants or obstruction in drainage of tears. Xerophtalmia = dry eyes Purulent discharge is thick and yellow. Crusts form at night. Assess hygiene practices and knowledge of cross contamination. Past history of ocular problems (i.e. allergies) and surgeries Allergens cause irritation of conjunctiva or cornea (i.e. makeup, contact lens solution) Surgery (i.e. Lasix, radiocaratonomy, lens replacements) Glaucoma: increased intraocular pressure Use of glasses or contact lenses With the use of corrective lenses, does your vision change? Contacts are a FB; take them out regularly. Self-care behaviors Last vision test Environment condition: work-related eye disease (i.e. an auto mechanic with a FB from metal working or radiation damage from welding). Medications? Some medications affect the eyes (i.e. prednisone may cause cataracts or increased intraocular pressure; beta blockers are used for ocular migraines and also used for HTN). Additional history for peds Any vaginal infections in the mother at time of delivery? Genital herpes and gonorrhea vaginitis have ocular sequelae for the newborn. HPI (PQRSTU) Objective – Physical Exam Far vision Snellen chart: E or picture chart 3 - 6 years old: 20/30 By 7- 6 years old: 20/20 Remove only reading glasses because they will blur distance vision. Note hesitancy, squinting, leaning forward, and misreading letters. The larger the denominator, the poorer the vision. If vision is poorer than 20/30, refer to an ophthalmologist or optometrist. Impaired vision may be due to refractive error, opacity in the media (cornea, lens, vitreous), or disorder in the retina or optic pathway. Picture cards (Allen Test) 2-5 years old 15 ft 3/7 = normal “How many fingers am I holding up?” Use if lower than the largest letter/picture Refer kids if…. < 20/50 age 3 either eye < 20/40 age 4 either eye > 1 line difference between eyes Screen x 2 before referral Near vision Hand held vision screener @ 14” from eyes 14/14 in each eye, read without hesitancy and without moving the card closer or farther away is a normal result. Presbyopia starts at age 40 (occurs in 50% of people) due the decrease in power of accommodation with aging; takes you longer to focus (loss accommodation for near vision); suggested when the person moves the card farther away. Confrontation test – checks fields of vision Gross measure of peripheral vision If the person is unable to see the object as the examiner does, the test suggest peripheral field loss. In an older adult, this screens for glaucoma. Acutely diminished visual fields occur with diseases of the retina and stroke. Color Blindness Assessment Ishihara’s test Primary colors: Red, Yellow, Green, Blue Male predominance: X-Linked Recessive Trait Corneal Light Reflex (Hirschberg Test): Checks for strabismus or eso/exotropia Shine a light toward person’s eyes, note the reflection of light on the corneas; it should be in the exact same spot on each eye. Asymmetry of the light reflex indicates deviation in alignment from eye muscle weakness or paralysis. If you see this – perform cover test. Cover test: checks for strabismus or eso/exotropia Detects small degrees of deviated alignment by interrupting the fusion reflex that normally keeps the two eyes parallel – cover an eye and stare at an object Normal response is uncovered eyeball has a steady fixed gaze If one eye jumps to fixate on the designated point, it was out of alignment before. If muscles aren't mature/strong, covered eye would "wander" A phoria is a mild weakness noted only when fusion is blocked. Tropia is more severe – a constant malalignment of the eyes. Diagnostic positions test: checks neuromuscular function Lead the eyes through the 6 cardinal positions of gaze and it will elicit any muscle weakness during movement. H pattern: up and down, left and right Left and right checks for nystagmus (eyes twitch when you look at extremes and also while moving horizontally) Then 45° angle Normal response is parallel tracking of the object with both eyes. If eye movement is not parallel Failure to follow in a certain direction indicates weakness of extraocular muscle or dysfunction of cranial nerve innervating it. Note any nystagmus a fine oscillating movement seen around the iris. Mild nystagmus at an extreme lateral gaze is normal; any other position is note. Occurs with disease of the semicircular canals in the ears, a paretic eye muscle, multiple sclerosis, or brain lesions. You should not see a white rim of sclera between the lid and the iris. Lid lag – occurs with hyperthyroidism. Inspection Brows Unequal or absent movement with nerve damage. Scaling occurs with seborrhea. Lashes/eyelids Incomplete closure creates risk for corneal damage. Palpebral fissures (opening b/w lids) are horizontal in non-Asians, whereas Asians normally have an upward slant. Ptosis: drooping of upper lid Eyeballs African Americans normally may have a slight protrusion of the eyeball beyond the supraorbital ridge. Exophthalmos: protruding eyes Enopthalmos: sunken eyes Conjunctiva (mucous membranes) and sclera: (white part) General reddening occurs in vascular disorders Cyanosis of the lower lids is abnormal Pallor near the outer canthus of the lower lids may indicate anemia (the inner canthus normally contains less pigment). African Americans occasionally have a gray-blue or “muddy” color to the sclera. In darkskinned people, you may see small brown macules (like freckles) on the sclera – this is normal. AA’s may have yellowish fatty deposits beneath the lids away from the cornea (don’t confuse this with jaundice). Scleral icterus: an even yellowing of the sclera extending up to the cornea, indicating jaundice. Note: tenderness, FB, discharge, or lesions. Lacrimal ducts Excessive tearing may indicate blockage of the nasolacrimal duct. Watch for any regurgitation of fluid out of the puncta, which confirms duct blockage. Note: puncta red, swollen, and tender to pressure Cornea/lens There should be no cloudiness A corneal abrasion causes irregular ridges in reflected light, producing a shattered look to light rays. Iris/pupil Size (3-5 mm); decreases in response to light Anisocoria: having pupils of two different sizes May be normal or could indicate CNS injury Note any irregular shape – normally they’re round. Reflexes Consensual light reflex: if a stimulus is presented to one pupil (i.e. a bright light) and it causes the pupil to constrict and dilate – the other pupil will have the same reflex simultaneously. Pupillary light reflex: normal constriction of the pupils when bright light shines on the retina. Subcortical reflex arc the person has no conscious control over it Abnormal findings: dilated pupils, dilated & fixed pupils, unequal or no response to light, Direct light reflex: occurs when one eye is exposed to bright light, the pupil constricts Fixation: reflex direction of the eye toward and object attracting a person’s attention. The image is fixed in the center of the visual field (fovea centralis). It consists of very rapid ocular movements to put the target back on the fovea and somewhat slower movements track the target and keep its image on the fovea. These movements are impaired by drugs, alcohol, fatigue, and inattention. Accommodation: adaption of the eye for near vision – observed by convergence of the eyeballs and pupillary constriction. Absence of constriction, convergence, or asymmetric response is abnormal. Red Reflex: reflects off retina 'Red eye' in pictures PERRLA Pupils Equal Round Reactive to Light Accommodation Fundoscopic Exam How to: Right Hand (hand holding opthalmoscope) Your right eye (where you should hold opthalmoscope) toview Their right eye Left hand on brow What you're looking for Optic disk: round, distinct, cream-orange, nasal side Arteries:Veins width should be 2:3 or 4:5 Macula (straight back, dark color): want 2DD (2 disk diameter) temporal to disk Papilledema - inc. ICP Cotton wool spots - diabetic retinopathy Retinal Hemorrhage Developmental Considerations Infants and children Birth – 2 weeks: blink to bright light 2 – 4 weeks: fixate on objects 1 month: track light or bright objects 3 – 4 months: fixate, track, and reach for objects Establishes binocularity and can fixate on a single image with both eyes simultaneously. 6 – 10 months: track in all directions Peripheral vision is intact in newborn; macular is absent (develops by 4 months and matures by 8). 80% of neonates are born farsighted; this gradually decreases by 7 – 8 years old. Eyeball reaches adult size by age 8 Aging adults Consistency changes from that of a soft plastic to rigid glass (d/t loss of elasticity). Lacrimal glands involute, causing decreased tear production and a feeling of dryness and burning. Pupil size decreases By age 70 – the normally transparent fibers of the lens begin to thicken and yellow senile cataract. Floaters appear d/t debris that accumulates because the vitreous is not renewed as continuously as the aqueous humor. Common causes of decreased visual functioning: Cataract formation (lens opacity resulting for a clumping of proteins in the lens) Glaucoma (increased intraocular pressure) Affects men at higher rates than women Most common type: chronic open-angle glaucoma; gradual loss of peripheral vision Primary open-angle glaucoma affects blacks 3-6 times more than whites, and is 6 times more likely to cause blindness in blacks than in whites. Macular degeneration (loss of central vision, the area of clearest vision) Most common cause of blindness Women more affected than men Peripheral vision is not affected Blindness In whites (older than 40) – leading cause is age-related macular degeneration, followed by cataracts. In blacks–cataracts and open-angle glaucoma. In Hispanics – open-angle glaucoma Common Abnormalities Eyes: Pseduostrabismus: Eye aren't equal but it's okay Epicathal fold excess on Asians, disappears with age Bush field spot: white around pupil, common in children with down’s syndrome Retinoblastoma! Seeing white in flash in a camera: light is not bouncing back = could mean cancer! Glaucoma Increased pressure in the anterior chamber Tonometry pressure testing Red Eye Conjuctivitis d/t varicella Subjuctival hemorrhage: most likely caused by trauma Hyphema: blood in anterior chamber of eye – trauma Pseudostrabismus-epicanthal fold excess; more common in Asians; others disappear with age. Brush field spot; NI variant? Common in Down syndrome White spot in picture of eye means cancer for ALL ages. We always want a red reflux. Retinal blastoma Blood in anterior chamber of eye- hyphema; can come from straining, getting hit. Ectropion-bottom eyelid drops down Entropion-bottom eyelid curls up. Xanthelasma-cholesterol in the eyelid Chalazion- cyst in the eyelid Hordeoulum- stye- infection in hair follicle of eyelid Basal cell carcinoma Exophthalmus- bulging eyes Coloboma- misshapen iris; dilated pupil Aniscoria-uneven pupils; head trauma, stroke, etc Pinguecula-growth in sclera Pterygium-growth into eye that can affect vision Ptosis-drooping of the upper lid Ears, Nose, Mouth, Throat (Chapter 15 & 16) – 16 Ears Case: Bobby 4 y.o. Bobby is brought into the clinic for c/o right ear pain for 2 days cc: OD pain x 2 d R otalgia x 2 day A &P Eustachian tube In children, it is more straight and short, so they have increased ear infections Babies should not lay flat while bottle feeding because they have eustachian tube dysfunction. The effects of gravity and sucking draw the nasopharyngeal contents directly into the middle ear. Labyrinth Vertigo: inflammation of labyrinth – creating a staggering gait and a strong, spinning, whirling sensation. Focused PHx/ROS Infections? (i.e. OM: otitis media, OE: Otitis externa) OM: obstruction of the eustachain tube or passage of the nasopharyngeal secretions into the middle ear. 90% of children younger than 2 years have had at least 1 case Predisposing factors: absence of breast feeding in the first 3 months, exposure to tobacco smoke (passive or gestational), daycare attendance, male gender, pacifier use, seasonability, and underlying diseases. Side effect: middle ear effusion can impair hearing, placing a child at risk for delayed cognitive development. Discharge? (otorrhea – suggests infected canal or perforated ear drum) External otitis: purulent, sanguineous, or watery discharge Acute otitis media with perforation: purulent discharge Typically with perforation – ear pain occurs first, stops with a popping sensation, then drainage occurs. Cholesteatoma: dirty yellow/gray discharge, foul odor. Earaches? Otalgia may be directly due to ear disease or may be referred pain from a problem in teeth or oropharynx. Virus/bacteria from URI may migrate up the Eustachian tube to involve middle ear. Trauma may rupture TM. Hearing loss? Adaptive devices? Children at risk for hearing deficit include those exposed to maternal rubella or to maternal ototoxic drugs in utero; premature infants; low-birth weight infants; trauma or hypoxia at birth; and infants with congenital liver or kidney disease. Vertigo – true rotational spinning r/t dysfunction of labyrinth Objective: feels like room spins; subjective: person feels like he/she spins. Make sure to distinguish vertigo from dizziness or light-headedness Ear Tubes or other surgery? Tinnitus: ringing (Meniere’s, ototoxic meds—Lasix, trauma)? Self-care? Clearing with q-tips impact cerumen, causing hearing loss Environmental noise? Objective External Inspection Alignment, Size, Shape, Symmetry Microtia: ears smaller than 4 cm vertically Macrotia: ears larger than 10 cm Edema occurs with infection or trauma Skin: Note any eczema, seborrhea, SCC (squamous cell carcinoma), decubiti (ulcer), sebaceous crust, chondrodermatitis, tophi Reddened, excessively warm skin indicates inflammation. Crusts and scaling occur with otitis externa and with eczema, contact dermatitis, and seborrhea. Enlarged tender lymph nodes in the region indicate inflammation of the pinna or mastoid process. Masses, nodes, nodules, furuncles--cyst under the skin Darwin’s tubercle: small painless nodule at the helix; congenital variation and not significant. Tenderness @ pinna and tragus Pain with movement occurs with otitis externa and furuncle. Pain at the mastoid process may indicate mastoiditis or lymphadenitis of the posterior auricular node. Mastoiditis can cause hearing loss. External Auditory Meatus: should be clear of swelling, redness, and discharge Drainage (otorrhea) is abnormal A sticky yellow discharge accompanies otitis externa, or it may indicate otitis media if the drum has ruptured Hygiene Otoscopic Examination Developmental considerations Child (less than three years): pull pinna down and back Adult: (because taller) up and back to help straighten the S-shape of the canal External canal – note color, lesions, masses and discharge Redness and swelling occur with otitis externa, the canal may be completely closed with swelling. Purulent otorrhea suggests otitis externa or otitis media if the drum has ruptured. Frank blood or clear watery drainage (cerebrospinal fluid leak) after trauma suggests basal skull fracture and warrants immediate referral. Cerebrospinal fluid feels oily and tests positive for glucose. Abnormal findings: FB, exostosis, polyp, furuncle Tympanic Membrane Color and Characteristics Yellow-amber color of the drum occurs with serous otitis media Red color occurs with acute otitis media Note absent or distorted landmarks Landmark: umbo Air/fluid level or air bubbles behind the drug indicate serous otitis media Position Normal: flat, slightly pulled at center, and flutters when the person performs the Valsavla maneuver (avoid in older person disrupts equilibrium), or insufflation (avoid in pt with URI proper infectious matter into middle ear) Abnormal Retracted drum due to vacuum in middle ear Bulging drum from increased pressure; no cone of light; cannot see umbo Eardrum does not move Integrity of Membrane – intact Perforation shows as a dark oval or as a larger opening on the drum. White patch may indicate scarring Insufflator: attaches to otoscope to push a little air and makes tympanic membrane move Words to know Malleus (manubrium of) Umbo (tip of manubrium of malleus) Reflected cone of light (looking for it when shining light in your ear) Right ear: cone of light is at 5 o clock Left ear: cone of light is at 7 o clock Hearing Audiometry Whisper (voice) Passing: 3/6 numbers/letters Abnormal: person is unable to hear whispered items. A whisper is a high-frequency sound and is used to detect high-tone loss. Watch: hearing the click of a watch Tuning Fork Weber: tuning fork on top of head Sound lateralizes to > Good ear: sensorineural (CN VIII ) loss Bad ear: conductive loss Rinne: tuning fork on mastoid bone, will time it. When patient does not hear anymore, move it to their ear. AC [Air conduction] 2x > BC [Bone conduction] = nl; Ratio 2:1*** ex/ 30 seconds to feel, 60 seconds to hear If bone conduction is greater, you have a conductive hearing loss BC > AC = Conductive loss AC > BC but overall reduced = Sensorineural loss If Weber test lateralizes to one side, do Rinne to confirm Startle Conductive Mechanical obstruction: cerumen, FB, rupture, OM/E, ETD--Eustachian Tube D... Acoustic neuroma--brain tumor that grows in the inner ear Tympanometry: presence of fluid in the middle ear, mobility of the middle ear system, and ear canal volume Developmental Considerations Infants and Children Maternal rubella infection occurs during the first trimester damage of the organ of Corti and impair hearing. Eustachian tube is relatively short and wider and more horizontal easier for pathogens from the nasopharynx to migrate to the middle ear increases risk for ear infections Low set ears are found with trisomy 13, 15, 21. Large, prominent ears, misshapen ears, and creases on earlobes are nonspecific but occur with certain syndromes and with underlying ear structure abnormalities. Pre-auricular skin tags may occur alone or with other facial anomalies. Use a pneumatic bulb to assess the vibratility – normally membrane moves inward with puff of air and outward with a slight release. An abnormal response is no movement of the eardrum. Drum hypomobility indicates effusion or a high vacuum in the middle ear. For the newborn’s first 6 week, drum immobility is the best indicator of middle ear infection. Look for FBs increased risk for trauma The incidence of meningitis, measles, mumps, OM, and any illness with persistent high fever may increase risk for hearing deficit. The adult Otosclerosis: common cause of conductive healing loss in young adults b/w the ages of 20 and 40; gradual hardening fixation of stapes in oval window impeding transmission of sound progressive deafness Aging adult Accumulation of cerumen d/t coarse/stiff cilia reduces hearing Impacted cerumen (occurs in 57% of older adults) is associated with hearing loss. Blocks conduction from hearing aids Presbycusis: gradual sensorineural loss causes by nerve degeneration in the inner ear that slowly progresses after the 5th decade; accentuated when unfavorable background noise is present (i.e. music, dishes clattering, or at a noisy party). Abnormal Findings External Ear Frostbite: reddish blue discoloration and swelling of auricle after exposure to extreme cold. Vesicles or bullae may develop, the person feels pain and tenderness, and ear necrosis may ensue. OE (swimmer’s ear): infection of outer ear, with severe painful movement of the pinna and tragus, redness and swelling of pinna and canal, scanty purulent discharge, scaling, itching, fever, and enlarged tender regional lymph nodes. Hearing is normal or slightly diminished. More common in hot, humid weather. Swimming causes canal to become waterlogged and well; skinfolds are set up for infection. Prevent by using rubbing alcohol or 2% acetic acid eardrops after every swim. Branchial Remnant and Ear Deformity: a facial remnant or leftover of the embryologic branchial arch usually appears as a skin tag. Occurs most often in the preauricular area, in front of the tragus. When bilateral, there is increased risk for renal anomalies. Cellulitis: inflammation of loose, subcutaneous connective tissue. Shows as thickening and induration of auricle with distorted contours. Lumps and Lesions Sebaceous cyst: Common location is behind lobule, in the postauricular fold. A nodule with central black punctum indicated blocked sebaceous gland. It is filled with waxy sebaceous material and is painful if infected. Tophi: small, whitish yellow, hard, nontender nodules in or near helix or antihelix; contain greasy, chalky material of uric acid crystals and are a sign of gout. Chondrodermatitis Nodularis Helicus: painful nodules develop on the rim of the helix (where this is no cushioning subcutaneous tissue) as a result of repetitive mechanical pressure or environmental trauma (sunlight). They are small, indurated, dull red, poorly defined, and very painful Keloid: overgrowth of scar tissue, which invades original site of trauma. It is more common in dark-skinned people, although it also occurs in whites. In the ear it is most common at lobule at the site of a pierced ear. Carcinoma: ulcerated, crusted nodule with indurated base that fails to heal. Bleeds intermittently. Must refer for biopsy. Usually occurs on the superior rim of the pinna, which has the most sun exposure. May occur also in ear canal and show chronic discharge that is either serosanguineous or bloody. Ear Canal Excessive cerumen: produced or impacted because of narrow, tortuous canal or poor cleaning method. Even when canal is 90-95% blocked, hearing stays normal; when cerumen expands after swimming or showering, person has ear fullness and sudden hearing loss. OE: severe swelling of canal, inflammation, tenderness. FB Osteoma: single, stony hard, rounded nodule that obscures the drum; nontender; overlying skin appears normal. Attached to inner third, the body part, of canal. Benign, but refer for removal. Exostosis: more common than osteoma. Small, bony hard, rounded nodules of hypertrophic bone, covered with normal epithelium. They arise near the drum, but usually do not obstruct the view of the drum. They are usually multiple and bilateral. They may occur more frequently in cold-water swimmers. The condition needs no treatment, although it may cause accumulation of cerumen, which blocks the canal. Polyp: arises in canal from granulomatous or mucosal tissue; redder than surrounding skin and bleeds easily; bathed in foul, purulent discharge; indicates chronic ear disease. Benign, but refer for excision. Furuncle: exquisitely painful, reddened, infected hair follicle. It may occur on the tragus on the cartilaginous part of ear canal. Regional lymphadenopathy often accompanies a furuncle. Tympanic Membrane (page 346) Nose Subjective Discharge Altered smell – anosmia Sense of smell diminishes with cigarette smoking, chronic allergies, aging Smoking Frequent colds (upper respiratory infections) Allergies or sinus pain “seasonal” rhinitis if due to pollen; “perennial” if allergen is dust Misuse of OTCs irritate the mucosa and cause rebound swelling. Epistaxis (nose bleeds) – occurs with trauma, vigorous nose blowing, FB Trauma – can cause deviated septum, which may cause nares to be obstructed Objective Inspection Lesions (BCC--basal cell carcinoma; more deadly than SCC although doesn't look worse, SCC) impetigo, deformities, discharge, asymmetry, and inflammation Absence of sniff indicates obstruction (i.e. nasal polyps, rhinitis) Nasal speculum: look for deviation, perforation, or bleeding Deviated septum looks like a hump or shelf in one nasal cavity. Perforation is seen as a spot of light from penlight shining in the other naris. Epitaxis commonly comes from the anterior septum; Kiesselbach plexus is the most common site. Turbinates: note any swelling, tender to touch, vascular Polyps (benign growths that accompany chronic allergy) are smooth, pale gray, avascular, mobile, and nontender. Nasal cavity: normal red color, smooth moist surface Note any swelling, discharge, bleeding, FB Rhinits: nasal mucosa is swollen and bright red with an upper respiratory infection Discharge is common with rhinitis and sinusitis, varying from watery and copious to thick, purulent, and green-yellow. With chronic allergy, mucosa looks swollen, boggy, pale, and gray. Palpation Sinuses Sinus areas are tender to palpation in persons with chronic allergies and acute infection (sinusitis) Pathology Rhinitis Acute vs. Allergic Acute: Purulent, Red turbinates, Unilateral (possibly d/t FB), Allergic, Clear, Pale boggy, Itchy, watery eyes, lines above their nose r/t always wiping Sinusitis Polyps (gray) Epistaxis (nosebleeds) Caused by trauma, vigorous nose blowing, foreign body Mouth & Throat Subjective Sores or lesions? Sore throat? Untreated strep throat may lead to the complication of rheumatic fever Bleeding gums? Dental problems? Toothache? Dentures? Correct fit? Vocal hoarseness (dysphonia)? R/T overuse of voice, URI, chronic inflammation, lesions, or a neoplasm Dysphagia? Occurs with pharyngitis, GERD, stroke & other neurological disorders, and esophageal cancer. Taste alterations? Self-care behaviors Dental care/check-ups? (should be every six months for cleaning as you get older) Dental appliances (braces, dentures, bridges)? Lesions may arise form ill-fitting dentures, or the presence of dentures may make the eruption of new lesions. TOBACCO? ETOH? Chronic tobacco use leads to tooth loss, coronal and root caries, and periodontal disease in older adults. Increase risk for oral and pharyngeal cancers Objective Inspection: Lips: Color, moisture, texture, vermilion border (border all the way around the lips) Abnormals: Angular cheilitis (perleche) (cracking on the side of the mouth) HSV I--herpes simplex virus 1 (typically oral; 2 is not oral but can be there SCC Cyanosis (hypoxemia and chilling), cherry red lips/nose/cheecks (CO poisoning- late sign), acidosis (aspirin poisoning or ketoacidosis) Gums: Color, swelling, atrophy, bleeding Dark lines gums = lead poisoning Teeth: Color, spacing, hygiene, occlusion Discolored teeth appear brown with excessive fluoride use, yellow with tobacco use. Grinding down of tooth surface; plaque – soft debris; caries – decay. Malocclusion (poor biting relationship), protrusion of upper or lower incisors Gingivitis hyperplasia, crevices between teeth and gums, pockets of debris. Gums bleed with slight pressure indicates gingivitis. Dark line on gingival margins occurs with lead and bismuth poisoning. Tongue: Sublingual/frenulum: Color, Texture, Coatings Palpate salivary glands Beefy red, glossy (B12 deficiency) should be pink and even Furrows (= dehydration) Black hairy (meds) Tremors (could possibly be from hyperthyroid Enlarged tongue occurs with mental retardation, hypothyroidism, acromegaly; a small tongue accompanies malnutrition. Dry mouth occurs with dehydration, fever; tongue has deep vertical fissures. Saliva is decreased when taking anti-cholinergic medications Excess saliva and drooling occur with gingivostomatitis and neurologic dysfunction A fine tremor of the tongue occurs with hyperthyroidism; a coarse tremor occurs with cerebral palsy and alcoholism. Tonsils: Color (Exudate: whiteness), Crypts Size : large child & atrophy w/ age rating tonsils 1+ visible 2+ 50% 3+ touches uvula 4+ kissing each other (painful) Bifurcated uvula – more common in American Indians Deviation to the side or absent movement indicates nerve damage, which also occurs with poliomyelitis and diphtheria. Bucca mucosa – pink, smooth, moist Dappled brown patches are present with Addison’s disease Orifice of Stensen’s duct looks red with mumps Koplik spots are an early warning sign of measles. Palate (hard and soft palate) Soft “Ahhh…” CN IX & X Uvula should go up Hard Appears yellow with jaundice (in blacks with jaundice – it may appear yellow, muddy yellow, or green-brown). Oral Kaposi sarcoma is the most common early lesion in people with AIDS Torus palatinus: benign growth arises after puberty and is a more common finding in American Indians, Inuits, and Asians. A high-arched palate is usually normal in the newborn, but very narrow or high arch also occurs with Turner’s syndrome, Ehlers-Danlos syndrome, Marfan’s syndrome, and Treacher Collins syndrome or develops in the mouth-breather in chronic allergies. Abnormals Angioedema: swelling of mouth and eyes Leukoplakia: side of whiteness, normal Geographic tongue: nothing wrong Glossitis: bright, red, can be enlarged, glossy Thrush: tongue is red and inflamed, white patches (can get it from fungal infection, which you can get from antibiotics) Black hairy tongue r/t antibiotics Ankyloglossia: short tongue syndrome - frenulum is too short, may have difficulty with bottle feeding; can limit protrusion and impair speech development Strep vs. Mono Petechiae soft palate strep Aphthous ulcers: ulcers inside mouth Sialolith (stones) Breath Halitosis: bad breath; can be caused by sinus, caries, strep Ketosis: sweet smell, occurs in diabetic ketoacidosis Acetone breath smell occurs in children with malnutrition or dehydration. Ammonia breath occurs with uremia Musty odor with dental or respiratory infections Alcohol odor with alcohol ingestion or chemicals Mouse-like smell with diphtheria S/S infection Red Pus Fever Dysphagia Developmental Child Obligate nose breathers Inability to suction out nose is bad, because they cannot breathe through mouth. Nasal flaring in the infant indicates respiratory distress Choanal atresia: inability to pass catheter through nasal cavity – requires immediate intervention Natal teeth (baby teeth that develop in uterine) vs. Epstein’s pearls (white cysts on gum line) Discolored teeth appear yellow or yellow-brown with infants taking tetracycline or whose mothers took the drug during the last trimester; appear green or black with excessive iron ingestion, although this reverses when iron is stopped. Cleft palate / lip Teeth Begin 6 m-2 ½ yr. (age in mo's – 6 = approx. # teeth they should have) 20 Deciduous lost by 6-12 yr. of age Baby Bottle tooth decay: consistent bottle drinkers are missing top front teeth, because of sugar in milk and juice (this also increases risk for middle ear infections) Tooth eruption is delayed with Down syndrome, cretinism, rickets. Prolonged thumb sucking (after age 6 or 7) may affect occlusion. Bruxism (teeth grinding) occurs in sleep from dental problems or nervous tension. Pregnancy Hyperplasia: swelling, increased blood flow/supply that goes everywhere (normal) Caries = myth Rhinitis Aging Decreased saliva production dry mouth (xerostomia) Dry mouth also causes by side effect of many drugs (i.e. antidepressants) Decreased taste Possibly r/t medications People add extra salt and sugar to food. Diminished smell may decrease the person’s ability to detect food spoilage, natural gas leaks, or smoke from a fire. Osteoporosis SQ wasting dental problems (i.e. dentures could not fit as well as possible)