Medicines management workshop
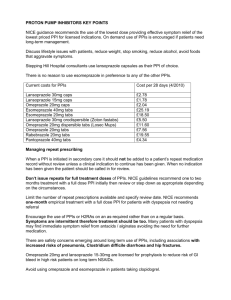
advertisement
Prudent Healthcare Medicines management workshop Proton Pump Inhibitors 1. Products Proton pump inhibitors (PPIs) are listed in British National Formulary (BNF) section 1.3.5. They include: Lansoprazole (Zoton®) Omeprazole (Losec®) Esomeprazole (Nexium®) Pantoprazole (Protium®) Rabeprazole sodium (Pariet®) Combination products are also available. These are: Vimovo® (naproxen + esomeprazole) Axorid® (ketoprofen + omeprazole) (The hyperlink links to one manufacturer’s summary of product characteristics (SPC) for one formulation/ strength of the drug. The SPCs for alternative manufacturer’s/ formulations/ strengths can be searched for at eMC) 2. Indications Proton pump inhibitors inhibit gastric acid secretion. Indications vary between products and according to dosage. The licensed indications of PPIs include: Treatment of gastric and duodenal ulcers Eradication of Helicobacter pylori Dyspepsia Gastro-oesophageal reflux disease Prevention and treatment of NSAID-associated ulcers Reduce degradation of pancreatic enzyme supplements in patients with cystic fibrosis Zollinger-Ellison syndrome Prepared by Anne Hinchliffe, Public Health Wales March 2014 v1.0 Page 1 “A proton pump inhibitor should be prescribed for appropriate indications at the lowest effective dose for the shortest period; the need for long-term treatment should be reviewed periodically” 1 3. National Institute for Health and Care Excellence (NICE) 3.1. Clinical guidelines recommending use of PPIs Management of dyspepsia in primary care (CG17) Acute upper GI bleeding (CG141) In addition, prescribing a PPI to provide gastro-intestinal protection when prescribing other medicines e.g. NSAIDs, low dose aspirin, SSRIs, is mentioned in a number of NICE clinical guidelines, examples include rheumatoid arthritis (CG79), low back pain (CG88), osteoarthritis (CG177), stroke (CG68) and depression with a chronic physical health problem (CG91). 3.2. Do not do recommendation From CG141 (ID: 1078) Do not offer acid-suppression drugs (PPIs or H2-receptor antagonists) before endoscopy to patients with suspected non-variceal upper gastrointestinal bleeding. 4. Medicines and healthcare products regulatory agency (MHRA) drug safety updates Hypomagnesaemia with long-term PPI usage Prolonged use of PPIs has been associated with hypomagnesaemia. Healthcare professionals should consider measuring magnesium levels before starting PPI treatment and repeat measurements periodically during prolonged treatment, especially in those who will take a PPI concomitantly with digoxin or drugs that may cause hypomagnesaemia (e.g., diuretics). [Drug Safety Update Vol. 5, Issue 9. April 2012] Increased risk of fracture with long term PPI usage There is epidemiological evidence of an increased risk of fracture with long-term use of PPIs. Patients at risk of osteoporosis should be treated 1 BNF edition 66, September 2013-March 2014, [page 55] Prepared by Anne Hinchliffe, Public Health Wales March 2014 v1.0 Page 2 according to current clinical guidelines to ensure they have an adequate intake of vitamin D and calcium. [Drug Safety Update Vol. 5, Issue 9: April 2012] Interaction between clopidogrel and omeprazole/ esomeprazole Use of either omeprazole or esomeprazole with clopidogrel should be discouraged. The current evidence does not support extending this advice to other PPIs. [Drug Safety Update Vol. 3, Issue 9. April 2010] 5. Additional health issues Decreased gastric activity, due to any means-including PPIsincreases gastric counts of bacteria normally present in the gastrointestinal tract. Treatment with acid reducing drugs leads to an increased risk of gastrointestinal infections such as salmonella, campylobacter or Clostridium difficile FDA Drug Safety Communication 2012: Clostridium difficile and PPIs Potential to mask malignant gastro-intestinal disease PPIs may be encouraging unhealthy lifestyle choices e.g. high fat diet, excessive alcohol consumption, over-eating, smoking, if patients are overcoming the unpleasant GI consequences from these behaviours by taking a PPI rather than modifying their behaviour to avoid the symptoms 6. All Wales Prescribing Indicators In 2011-12 there were two national prescribing indicators for PPIs. These were: Defined daily doses per 1000 prescribing units PPI items of low acquisition cost as a percentage of all PPIs Further information on national prescribing indicators and their analysis from 2011-12 to 2014-15 can be found in the online AWMSG library Cwm Taf had traditionally high rates of low acquisition cost PPI prescribing; this has been supported by the Cwm Taf formulary Prepared by Anne Hinchliffe, Public Health Wales March 2014 v1.0 Page 3 7. Resources to support change 7.1. All Wales Therapeutics and Toxicology Centre (AWTTC) All Wales proton pump inhibitor and dyspepsia resource pack 2013 CEPP All Wales Audit: Reducing the use of high acquisition cost proton pump inhibitors 2011-2013 Patient information leaflet: Proton Pump Inhibitors for the treatment of dyspepsia and heartburn English/ Welsh Stopping medicines- proton pump inhibitors WeMeReC e-notes 2010 7.2. NICE shared learning database The way to medicines optimisation is through the stomach - tackling high prescribing levels using the NICE dyspepsia guideline to review proton pump inhibitor (PPI) prescribing. 7.3. Cwm Taf Health Board The Cwm Taf Medicines Management Practice Unit works with GP practices in Cwm Taf to encourage clinically and cost effective prescribing. The Unit was involved in the development of the CEPP All Wales audit and guidelines on PPI prescribing (hyperlink above). These were sent to GP practices in Cwm Taf. A PowerPoint presentation on dyspepsia management was also made available to practices. A multidisciplinary audit pack was developed for use by community pharmacy and formed part of the community pharmacy contractual requirement in Cwm Taf for 2011/12 (attachment 1). Despite this work the total quantity of PPIs prescribed continues to rise year on year. Attachment 1Community Pharmacy PPI audit.doc Prepared by Anne Hinchliffe, Public Health Wales March 2014 v1.0 Page 4