Jr. Internal Medicine Clerkship - East Tennessee State University
advertisement

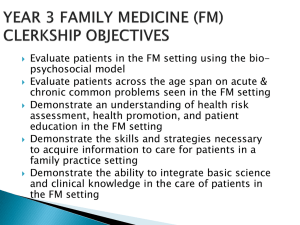
Third Year Internal Medicine Clerkship 2015 - 2016 Syllabus Department of Internal Medicine Quillen College of Medicine East Tennessee State University Dr. Charles A. Stuart Interim Chair, Department of Internal Medicine Dr. Aaysha Kapila – Course Director Dr. Rupal Shah – Co-Director Yvette Font Clerkship Coordinator (rev. 9/22) 1|Page 2015 – 2016 JUNIOR INTERNAL MEDICINE CLERKSHIP SYLLABUS CONTACT INFORMATION WELCOME A. Importance of clerkship B. Clerkship Goals C. Clerkship Objectives ROLES AND RESPONSIBILITIES A. Assessment of Student B. Assessment of Faculty and Course C. Faculty Responsibilities D. Student Responsibilities E. Documentation of Required Experiences F. Clerkship Specific Procedures/Patient Log G. Professional Expectations for Students H. Social Networking I. Policy on HIPPA Training, Violations and Disciplinary Actions J. Medical Student Duty Hours K. Student Illness L. Student Absences M. Inclement Weather Policy N. Appropriate Dress O. Identification Badges P. Student Contact Phone Numbers SCHEDULES A. Clerkship Site Assignments B. Student Education Conferences C. Quiz schedule D. Department of Medicine Grand Rounds E. Cardiac Rehabilitation ASSESSMENTS A. Clerkship Grading B. Clerkship Grade Scale C. NBME Exam Policy D. Student Computer Usage During Electronically Administered Quizzes/Exams Policy TIPS FOR LEARNING A. Top 10 Ways to Excel on the Internal Medicine Clerkship LEARNING RESOURCES A. Textbooks for reading B. References and Materials (Optional) C. Student Procedures for Special Services (ADA) D. Tutoring E. Counseling APPENDICES A. History and Physical Template 3 3 3 3 4 5 5 5 5 6 7 8 9 9 10 11 11 12 12 12 12 13 13 13 13 13 13 14 14 14 15 15 15 16 16 16 16 16 17 17 17 18 2|Page B. COM Intuitional Objectives C. Entrustable Professional Activities JR. INTERNAL MEDICINE CLERKSHIP Dr. Aaysha Kapila: Course Director: 423-224-8425 (beeper) kapilaa@etsu.edu Yvette Font: Clerkship Coordinator, 423-439-6381 font@etsu.edu Johnson City Medical Center VA Medical Center Holston Valley Medical Center Bristol Regional Medical Center Academic Affairs Ms. Tawana Holland Ms. Anetha Wright Ms. Rita Forrester Ms. Jane Lipscomb Ms Cathy Peeples 423-431-6431 423-926-1171 ext. 7358 423-224-5075 423-844-6650 423-439-6311 WELCOME! Welcome to the Junior Medicine Clerkship. We hope you will enjoy the time you share with us. We are proud of our reputation as dedicated medical educators and hope you enjoy the knowledge and experience you will gain while rotating with the Department of Internal Medicine. The Junior Clerkship experience in Internal Medicine consists of six weeks of inpatient medicine divided into two three week rotations at two of our three sites: VA Medical Center, Johnson City Medical Center or Holston Valley Medical Center. This will provide you the opportunity to experience different hospital settings. A. Importance of this course During this six-week clerkship, you will acquire fundamental skills, reinforce and expand your knowledge, and develop personally and professionally. We hope that this experience inspires you to learn and experience more of what Internal Medicine has to offer. Internists care for a broad spectrum of patients, ranging in age from adolescents to the ever-growing elderly population. While expanding your medical knowledge, you will also be solidifying basic clinical skills such as patient interviewing, physical examination, and communication through case presentations and written documentation. This time is also a major opportunity to improve more advanced skills such as physical diagnosis, clinical reasoning, and developing physician-patient relationships. B. Clerkship Goals The Internal Medicine curriculum goals are to assist students in acquiring a foundation of knowledge regarding the practice of medicine, and assist students in mastering basic interpersonal skills relevant to the management of patients with medical illness. 1. Student will develop a solid foundation of medical knowledge regarding the care and management of patients presenting with a variety of medical diseases. This will include formulating a diagnosis, patient care plan, medical diagnostic procedures, adherence to evidence-based guidelines and follow up care that includes both medical and psychological support. 3|Page 2. Students will effectively participate as team members while maintaining a professional demeanor that includes communication with fellow students, residents, attending physicians and patient’s family members. C. Clerkship Objectives: Course / Clerkship Objectives: At the conclusion of this rotation the student will be able to: Meets EPAsee appendix B Educational Method(s) gather a history and perform a physical examination incorporating ethical, social, and diversity perspectives to provide culturally competent health care. prioritize a differential diagnosis following a clinical encounter for common conditions seen in Internal Medicine. EPA 1 Clinical Experienceinpatient EPA 2 Clinical Experienceinpatient recommend and interpret common diagnostic and screening tests for conditions frequently seen in Internal Medicine. EPA 3 -Clinical Experienceinpatient; - Conference document and discuss orders for common conditions seen in Internal Medicine. EPA 4 appropriately write prescriptions by recognizing and avoiding errors utilizing information resources to place the correct order/perscription and maximize therapeutic benefit and safety for patients document a clinical encounter in the patient record (electronic or written format) EPA 4 Clinical Experienceinpatient Clinical Experienceinpatient provide an accurate and concise oral presentation of a clinical encounter of a patient in the inpatient setting form clinical questions and retrieve evidence to advance patient care EPA 6 give or receive a patient handover to transition care responsibility in an inpatient setting demonstrate the ability to collaborate as a member of an interprofessional team in an inpatient setting EPA 8 recognize a patient requiring urgent or EPA 10 EPA 5 EPA 7 EPA 9 Assessment Method(s) -Clinical Documentation Review; -Participation -Clinical Documentation Review; -Exam-Institutionally Developed-writtem; -Exam-Nationally Normed/Subject -Clinical Documentation Review; -Exam-Institutionally Developed-writtem; -Exam-Nationally Normed/Subject -Clinical Documentation Review Clinical Documentation Review Clinical Experienceinpatient Clinical Experienceinpatient -Clinical Experienceinpatient; -Self-directed learning Clinical Experienceinpatient Clinical Experienceinpatient Clinical Documentation Review Oral Patient Presentation -Clinical -Participation; -Clinical Documentation Review; -Oral Patient Presentation Participation Participation 4|Page emergent care demonstrate knowledge of the elements necessary for informed consent for tests and procedures and impact on patient/family perform required Clerkship and College of Medicine procedures under direct supervision. demonstrate an understanding of system based practice and the students role in a culture of patient safety and continuous quality improvement 2. Experienceinpatient; -Conference Clinical Experienceinpatient -Exam-Nationally Normed/Subject EPA 12 -Demonstration; -Preceptorship EPA 13 Clinical Experienceinpatient -Participation; -Clinical Performance Checklist -Participation; -Exam-Nationally Normed/Subject EPA 11 -Participation; - Exam-Nationally Normed/Subject ROLES AND RESPONSIBILITIES IN LEARNING A. COM: ASSESSMENT OF STUDENT The clerkship director and coordinator manage the assessment process for all the clerkship students. QCOM uses an on-line assessment system, New Innovations (NI), to assess each student’s performance. Individual faculty assessment of each student will be combined into the Clerkship Director’s final composite assessment form for each student. The final composite will contain faculty comments and the final course grade. Students will be notified when their final assessment is available in NI to view. This should be approximately 3 weeks following the conclusion of the clerkship. Final grades will be posted into the ETSU Banner system and become the official grade for the student’s transcript. An integral part of the assessment process is the Mid-clerkship Review with the clerkship director which all students will have. It is the student’s responsibility to complete their portion of the Mid-Clerkship Review form and to arrange for a faculty member they have worked closely with during the clerkship to review and complete the faculty portion of the form prior to the Mid-Clerkship Review. During the Midclerkship Review the clerkship director will review and discuss the completed form with the student. The completed form will remain with the Clerkship throughout the rotation. The Mid-Clerkship Review form can be found in the Administrative Forms folder in New Innovations under my Favorites/Department Manuals or it may be provided to the student by the clerkship coordinator. The Mid-Clerkship Review form can be found in the Administrative Forms folder in New Innovations under Intranet or it may be provided to the student by the clerkship coordinator. B. COM: EVALUATION OF FACULTY AND COURSE The on-line system is also used for the students to evaluate the faculty and the course. This evaluation tool is used to provide information to the clerkship administration about the teaching/learning process with the intent of improving learning. Student feedback is essential for curriculum planning. Students will be notified electronically when these required evaluations are available to complete. Timely completion of evaluations is required. Individual clerkships may also request students to evaluate its’ Resident Physicians using the on-line system, also with the intent of improving learning. C. FACULTY RESPONSIBILITIES: 5|Page Observe each student perform components of a history and physical exam on a patient some time during their inpatient rotation. During the inpatient rotation a strong emphasis on the development of clinical skills is a necessity. Review student’s histories and physical exams to include assessments and plans. Review the written record and assess that the student is able to present each case succinctly. (Students at the VA will write notes in Word Document so that the notes can be cut and pasted if needed by residents or attendings to insert into the patient record.) Submit an assessment via New Innovations of each student after the completion of the ward rotation. D. STUDENT RESPONSIBILITIES: 1. Attend Orientation at 8 a.m. on first Monday of the clerkship. This is a live interactive orientation conducted by one of the co-clerkship directors and coordinator, which is designed to outline the course and expectations as well as tips on how to succeed. Included in the orientation will be a discussion regarding professionalism and its vitality in medicine. 2. Admit at least 12 patients during the 6 week ward service. Perform a complete history and physical exam on these patients. Assist the PGY-1 with entering admission orders into the hospital order entry system. Leave history, physical exam and assessment on patients chart to be countersigned by the attendings. Copies of the H&P should be made and submitted to the attending for critique. An H&P template will be emailed to you for assistance with structure and content. In addition, one formal H&P will be submitted to the clerkship office for review and evaluation. It will be counted as 10% of your total grade. 3. Write daily progress (SOAP) notes on patients you are covering to be co-signed by attendings. Each student will be responsible for two patients while on rotation during any one given time. 4. Attend morning report and/or attending rounds daily and be prepared for patient presentations or admission H&P’s from the previous night. 5. Take Overnight call – no more than 1 in 7 days (average over 6 weeks) If you are assigned to the VAMC you will be expected to take one week of night float. Students should be aware that night float begins on Sunday night at 7 p.m. and ends Friday morning at 7 a.m. STUDENTS MAY WEAR SCRUBS DURING THE WEEK OF NIGHT FLOAT AT WELL AS NIGHTS ON CALL AT JCMCH OR HOLSTON VALLEY. STUDENTS AT ALL SITES MAY STOP TAKING FLOOR CALLS AND ADMISSIONS AT MIDNIGHT ON NIGHTS PRIOR TO QUIZ DATES. PLEASE COMMUNICATE WITH YOUR ATTENDINGS AND SENIOR RESIDENTS. 6. Maintain a professional demeanor that includes communication with fellow students, residents, faculty, staff and patient’s family members. 7. Attend Student Education Conference each Thursday afternoon from 1-5 p.m. in VAMC, Bldg 1. 8. Complete a comprehensive patient interview followed by a case presentation with their assigned attending who will assess a grade. Grading forms will be distributed at orientation and can also be obtained online in New Innovations. This grade will count as 15% of their overall clerkship grade. 9. Complete a patient log (hard copy) as well as enter in New Innovations. At mid-rotation the student must review the log with his or her attending to make sure the requirements are being met. Any deficiencies must be noted and completed by the end of the rotation. 10. Complete a Mid-Clerkship Self-Assessment. During the Mid-clerkship Review the clerkship director will review and discuss the completed form, accomplishment and documentation of 6|Page required procedures and/or patient types, and duty hours issues with the student. The MidClerkship Review form can be found in the Administrative Forms folder in New Innovations under Intranet or it may be provided to the student by the clerkship coordinator. 11. Complete an assessment of the faculty and clerkship at the end of the rotation. Student input is instrumental to creating a positive experience for students. Student responses are taken into consideration by each department. 12. Access: http://www.etsu.edu/com/intmed/educationprograms/juniormed/lecture.aspx The prerecorded lectures can also be retrieved by accessing the Department of Internal Medicine website – “clerkships” – “junior medicine” – “student lecture series” E. COM: DOCUMENTATION OF REQUIRED EXPERIENCES Required College of Medicine Procedures and Clerkship Specific Procedures and/or Patient Types LCME Accreditation standard ED-2 requires that core clinical requirements are identified for all students to accomplish. This has been done at both the clerkship level and the College of Medicine level. Students are expected to demonstrate performance (not observing or assisting) the following procedures by the end their M3 year in order to graduate from the Quillen College of Medicine. Class of 2016 Required College of Medicine Procedures 2015-16 Quillen College of Medicine Required Procedures QCOM: Arterial puncture - perform (also Surgery Clerkship requirement) QCOM: Aseptic technique-demonstrate (also Surgery Clerkship requirement) QCOM: Bacterial culture-collect, perform and interpret results (also Surgery Clerkship requirement) QCOM: EKG-perform QCOM: Foley catheter- perform insertion (also Surgery Clerkship requirement) QCOM: Glucose test finger stick-perform and interpret (also Community Medicine & RPCT Clerkship requirement) QCOM: Injection-intramuscular -perform (also Family Medicine & RPCT Clerkship requirement) QCOM: Injections-subcutaneous - perform QCOM: KOH Prep-perform (OB Clerkship requirement) QCOM: Nasogastric tube insertion - perform (also Surgery Clerkship requirement) QCOM: Pap smear-perform (also OB Clerkship requirement) QCOM: Prostate Exam-perform QCOM: Spirometry-perform and interpret results (also Community Medicine & RPCT Clerkship requirement) QCOM: Stool guaiac testing-perform QCOM: Suturing-successfully demonstrate (also Surgery & OB Clerkship requirements) QCOM: Tube Thoracotomy (live or in sim lab) (also Surgery Clerkship requirement) QCOM: Urine clean catch - instruct patient and obtain (also Community Medicine & RPCT clerkship requirement) QCOM: Urine dipstick test-perform & interpret results (also Community Medicine & RPCT clerkship requirement) QCOM: Venipuncture - perform (also Surgery Clerkship requirement) QCOM: Wet mount-perform (Wet prep, GBS, FFN requirement for OB clerkship) The above procedures can to be performed any time during the M3 year and documented into New Innovations under the Global setting in the Case Logger, however please note some are also Clerkship requirements and must be accomplished during that specific clerkship. F. Clerkship Specific Procedures Patient Log 7|Page Each clerkship has also identified required and/or suggested procedures to be performed and/or patient types for all students to experience during the clerkship. Clerkship specific procedures/patient types are also to be documented in New Innovations, indicating if they observed, assisted or performed a skill and where the experience occurred. Required procedures must be “performed”. Only those procedures documented as “performed,” not observed or assisted, will count toward meeting the requirements. Students are to document all clerkship identified experiences in the Case Logger module of New Innovations by the end of the clerkship. Only the electronic log will be accepted as evidence of meeting the requirements. The ability to log diagnosis or procedures into New Innovations closes at midnight the last Friday of the clerkship rotation. Those students who do not document in New Innovation accomplishing all clerkship specific required procedures/patient types by the end of the clerkship will have their final numeric grade lowered by 5%. 2015-16 Internal Medicine Required Procedures # Required Interpret a Gram stain 1 Interpret an EKG Interpret and report urinalysis results 1 1 Perform a complete history and physical Read and interpret a peripheral blood smear 12 1 Encouraged Diagnosis Abdominal Pain Anemia Alcohol/ Drug Related Problem Arthritis Bleeding Disorder Coronary Artery Disease Diabetes Gastrointestinal Bleeding Hepatitis Hypertension Neuromuscular Disease Pleural Effusion COPD/Asthma CVA Electrolyte Abnormality Heart Failure HIV Lung Nodule/Mass Pancreatitis Pneumonia Renal Failure Thyroid Disorder Vasculitis Syncope/Arrhythmia Urinary Tract Infection Clerkships must provide students with adequate exposure to a variety of learning opportunities. If a student is having difficulty in securing an opportunity to perform a required procedure or see a required patient type they should request assistance from the clerkship director, preceptors, residents or fellow students in identifying opportunities. If the student is still not able to secure a required procedure experience they should inform the clerkship director and request to complete in a simulated environment. It is the student’s responsibility to be proactive in seeking out the identified required educational experiences. A clerkship may provide the student a paper copy of the required experiences specific to that clerkship and require that each accomplished experience be validated by the observing faculty. This documentation assures the requirements of the clerkship are met by each student and builds the student’s portfolio. A single observer cannot validate all of a student’s documentation. Students are expected to enter their documentation at least weekly into New Innovations and document at least 1/3 of the required clerkship procedures/patient types by the clerkship midpoint. Students’ progress will be monitored by the Clerkship Director and Coordinator in addition to Academic Affairs. G. COM: PROFESSIONAL EXPECTATIONS FOR STUDENTS Student behavior is expected to be professional in all areas at all times. 8|Page Professionalism Students shall demonstrate the behaviors befitting an ethical professional at all times. Students shall: exhibit respect, compassion, humility, altruism, duty, and honesty with patients, patient’s families, staff, faculty, members of the healthcare team, fellow students, and themselves. be punctual, reliable, and conscientious in completing academic and patient care responsibilities. recognize limitations in knowledge and pursue appropriate activities to effectively address learning needs. demonstrate personal accountability and admit professional mistakes. adhere to legal and ethical principles related to patient consent and confidentiality. demonstrate awareness and sensitivity to age, gender, race, ethnicity, culture, spiritual beliefs, socioeconomic background, family support, sexual orientation, and healthcare beliefs in interactions with others. demonstrate professionalism in dress, hygiene, and demeanor. utilize appropriate boundaries within the patient/physician relationship. For the vast majority of students these expectations are natural and intuitively known. However, a limited number of specific unprofessional behaviors are identified below. Of course, it is impossible to delineate each and every aspect of professionalism. Consequently, the final decision of what constitutes unprofessional behavior lies with faculty preceptors and the clerkship director. Faculty preceptors may report any unprofessional actions of concern on their assessment of student form or to the clerkship director prior to the end of the rotation. The student may be assigned a grade of R, which requires a review by the Student Promotions Committee. Students many fail a clerkship based solely on unprofessional behavior. Examples of Unprofessional Behavior Include: Absence from duty without excuse. Substance abuse either on duty or off duty which effects performance while on duty (in addition, legal or criminal action, will be dealt with as an infraction of professional behavior). False witness in any statement in a chart or document related to the practice of medicine. Failure to safeguard patient’s rights. Willful neglect of patients. Expressions of prejudice in any form (this includes verbal comments or behaviors expressing prejudice based on age, sex, sexual orientation, race, religion, nationality, origin, or disability). Inappropriate personal behavior in professional settings including abusive language, unprofessional appearance or sexual misconduct. Use of patient's chart or record for any purpose other than rendering health care (i.e., criticism of colleagues, demeaning remarks toward the patients). Non-compliance with HIPAA guidelines (Refer to QCOM’s HIPAA and Social Medical Policies for additional information.) Acute or chronic neglect of professional/educational schedule. Failure to comply with the hospital or clinic bylaws. Willful failure to comply with the reasonable professional directions of an attending physician or faculty preceptor. Texting or sleeping during didactic, clinical or laboratory activities. H. COM: Social Networking Guidelines The Quillen College of Medicine recommends that students exercise caution in using social networking sites such as Facebook, MySpace, and Twitter. Items that represent unprofessional behavior posted by students on such networking sites are not in the best interest of the University or Quillen College of Medicine and may result in disciplinary action up to and including termination. Students are expected to exhibit a high degree of professionalism and personal integrity consistent with the pursuit of excellence in the conduct of his or her responsibilities. They must avoid identifying their connection to the University or QCOM if their online activities are inconsistent with University and QCOM values or could negatively impact the University's or College of Medicine’s reputation. 9|Page If using social networking sites, students should use a personal e-mail address as their primary means of identification. Their University e-mail address should be used in accordance with university policy: http://www.etsu.edu/oit/policies/acceptableuse.aspx#Intro . Students who use these websites must be aware of the critical importance of privatizing their websites so that only trustworthy friends have access to the websites/applications. In posting information on personal social networking sites, students must not present themselves as an official representative or spokesperson for the college of medicine, any affiliated hospital or clinic, or the University. Patient privacy must be maintained and confidential or proprietary information about the University or hospitals must not be shared online. Patient information is protected under the Health Insurance Portability and Accountability Act (HIPAA). Students have an ethical and legal obligation to safeguard protected health information and posting or e-mailing patient photographs is a violation of the HIPPA statute. I. COM: Policy on Student HIPAA Training, Violations and Disciplinary Action The Health Insurance Portability and Accountability Act (HIPAA) is federal legislation which protects the health information of individuals. Medical students will routinely be exposed to Protected Health Information (PHI) during clinical rotations. As part of their orientation to medical school students will receive HIPAA training which will be periodically updated. HIPAA violations can result in significant federal penalties for both individuals and organizations. Quillen College of Medicine regards HIPAA violations as serious offenses. Discussion of patient cases in educational conferences and among students for educational purposes is not a HIPAA violation. However, if such PHI was disseminated beyond these settings, it would likely be a HIPAA violation. Use of PHI in research requires approval of an Institutional Review Board (IRB). Medical students who do not know if a particular use of PHI is appropriate should ask their supervisor. Level of Violation Examples of HIPAA Violations (these are not inclusive) Review and Minimum Disciplinary Action Level I Level II Level II Unauthorized copying of medical records Leaving PHI in a public area Discussing PHI in a non-secure area Posting PHI on any social networking site Removing medical records from a hospital or clinic without proper authority Unapproved accessing of PHI when the student is not involved in the care of the particular patient Intentional assisting another person in gaining unauthorized access to PHI Inappropriate sharing of ID/Password with another person Removing medical records from a hospital or clinic without proper authority Unapproved accessing of PHI when Verbal counseling Written warning in student’s permanent file and Retraining Multiple careless Level I violations shall be subject to progressive disciplinary action which may include a failing grade in the course/clerkship and/or dismissal from QCOM Verbal counseling Written reprimand in student’s file and Retraining A single incident may result in suspension, a failing grade in the course/clerkship and/or dismissal from QCOM Verbal counseling Written reprimand in student’s file and Retraining A single incident may result in suspension, 10 | P a g e Level III the student is not involved in the care of the particular patient Intentional assisting another person in gaining unauthorized access to PHI Inappropriate sharing of ID/Password with another person Disclosure or abusive use of PHI Tampering with or unauthorized destruction of information Unauthorized delivery of PHI to any third party a failing grade in the course/clerkship and/or dismissal from QCOM Immediate dismissal Violations should be reported to the Executive Associate Dean for Academic Affairs immediately for consideration by the Student Promotions Committee which will make an action recommendation. The student may appeal the recommendation of the Student Promotions Committee to the Executive Associate Dean for Academic Affairs. Final determination will be made by the Dean based on the committee’s recommendation. J. COM: MEDICAL STUDENT DUTY HOURS Medical student assignments, including the nature and content of activities and the number of duty hours required, must be determined by the educational value of the assignment. All assignments must provide meaningful educational value. Excessive work hours and fatigue can impact medical student learning just as it impacts patient care. 1. Duty hours consist of hours required In hospital or clinic/office. In didactic education (lectures, conferences, etc.). In any mandatory educational activity. 2. At home call is not included in duty hours determinations. 3. Student study at home is not counted as duty hours. 4. Medical student duty hours should not exceed on average 80 hours / week. 5. IN-HOUSE NIGHT CALL is permitted under the following conditions: Is a valuable educational experience. Facilitates being a member of healthcare team. Adequate rest facilities available in hospital. Occurs no more frequently than once every week. Call will not precede day of an exam or quiz. If student feels fatigued after the call, he/she is to be excused for an appropriate length of time from rounds, classes, etc. Any didactic materials should be made available to the student. It is the responsibility of the student to effectively communicate with team members regarding their need for a period of post-call rest. The student should not leave normal student responsibilities without such communication. Hours of in-house call count toward 80 hours total. Students are to log their duty hours weekly into New Innovations for each clerkship period for documentation purposes. Duty hour compliance will be monitored by Academic Affairs on a periodic basis. Students who feel they are consistently expected to work more than 80 hours per week should notify the clerkship director. If the issue is not resolved the student should contact the Executive Associate Dean for Academic Affairs. K. COM: STUDENT ILLNESS In the event of illness, the student must contact on the day of absence the preceptor/resident they are assigned to work with that day. The student is to update the Clerkship Coordinator upon their return to work. L. COM: STUDENT ABSENCES 11 | P a g e During Jr. Clerkship rotations there is no annual leave / time off. Students will work the schedule of the location they are assigned to during the clerkship. ETSU COM Administrative office closures do not necessitate student time off. All requests for absence from the clerkship rotation must be requested in advance on the Request for Leave form prior to the date(s) needed for justifiable circumstances. The Request for Leave form is located in the Administrative Forms folder in NI, on the Intranet. Additional call may be required for time away for other approved educational activities. All absences will be reported on the final composite assessment completed by the clerkship. No Requests for Leave will be granted for scheduled exam times. M. COM: INCLEMENT WEATHER POLICY The official radio station for reporting the status of classes and other activities of the College of Medicine during inclement weather is WETS-FM 89.5. All students - including all medical students - are to govern themselves according to the status as reported by this station for the University. In the event of missed classes due to inclement weather, makeup classes may be required on Saturdays. N. COM: APPROPRIATE DRESS It is the consensus of the faculty and administration of the Quillen College of Medicine that students should maintain a neat, clean personal appearance and dress in a professional manner at all times. Since students are intimately involved with patients and members of the health care team, wearing reasonable clothing and avoiding extremes of dress is imperative. Individual clerkships may have more specific criteria. GUIDELINES: All students shall wear their white lab coats, unless the department indicates otherwise. General attire must be clean and neat at all times. Appropriate attire is considered to be dress shirts, dresses, pantsuits, blouses, skirts, sport coats, dress slacks, and shirts with collars. Jeans, tennis shoes, shorts, skirts three inches of more above the knee, tube tops, low cut tank tops, t-shirts, midriff tops, sundresses without a jacket or blazer, see-through and low cut blouses, sweatpants, sweatshirts, and leather attire are considered inappropriate attire. When patient care responsibilities necessitate physical contact do not wear large bulky jewelry or jewelry that may inadvertently cause injury to patients. Hair should be neatly arranged in such a manner that it does not fall on patients and cannot be grabbed by a patient. Facial hair should be neatly groomed to present a professional image. Perfume, cologne, or other fragrance products should be moderately used to avoid being offensive or causing discomfort to others. Undergarments should not be visible through outer clothing. OSHA requires that shoes must be closed-toed in the patient care areas (no flip-flops or sandals). Shoes should be of reasonable height and comfortable enough for the student to be able to respond to any type of emergency in a healthcare setting. Visible body piercing must be conservative and jewelry must be small in size. CDC requires that fingernails be kept clean and short for patient care and for the proper fit of gloves or other protective equipment. Artificial Nails are not permitted. Scrubs need to be covered when leaving patient care areas. COMPLIANCE: All students are expected to comply with these guidelines. If a faculty preceptor deems the student’s attire is inappropriate, the student will be counseled appropriately and may be sent home to correct attire before returning to their duties. O. COM: IDENTIFICATION BADGES Students are to wear their College of Medicine Identification badges at all times while on any clinical rotation. 12 | P a g e Students are to wear their hospital issued identification badge at all times during any clinical rotation which requires the student to be present in that particular facility. o It is the student’s responsibility to keep their VA credentials current in accordance with VA policy during their M3 and M4 year. Students may not participation in any rotation occurring at the VAMC without a valid VAMC identification badge. P. COM: STUDENT CONTACT PHONE NUMBERS The student is responsible for providing a local area code contact phone number or pager number for use by rotation coordinators. If contact information has changed, the change should be made in Banner, which will update information in New Innovations. 3. SCHEDULES A. CLERKSHIP SITE ASSIGNMENTS are posted in New Innovations for each rotation and distributed at clerkship orientation. B. STUDENT EDUCATION CONFERENCE (SEC) The SEC or Academic Half Day will be held each Thursday afternoon in an effort to help bolster medical knowledge as well as help students develop their medical management skills. Faculty and residents will be responsible for facilitating each session that will consist of up to date audio lectures followed by a “Washington Manual” review session. The class will culminate in a case conference Week 1: Week 1. Week 2: Week 2: Week 3: Week 4: C. CHF, ACS, A fib, EKG’s Asthma, COPD Fever/Infection DVT/PE CVA/Seizure Disorder DKA QUIZ SCHEDULE: Week 2: Week 3: Week 4: Week 5: Cardio and Pulmonary Hematology and ID (midterm review forms due) Gastroenterology and Neurology Endocrine and Nephrology (written H&P’s due) D. DEPARTMENT OF MEDICINE “GRAND ROUNDS” CONFERENCE Every Tuesday at 8 a.m. at the Votaw Auditorium located at the ETSU Physicians and Associates building there is “Grand Rounds.” Please inquire with your attending at each specific training site regarding attendance. If you are directed to attend the “Grand Rounds” then you will report back to your respective sites following its conclusion at 9 a.m. E. CARDIAC REHABILITATION As a component of Internal Medicine, students will attend a lecture given by Dr. Timir Paul – 13 | P a g e ETSU Physicians, Cardiologist. The goals of cardiac rehabilitation lecture are to introduce the student to how rehabilitation can improve patient functioning through: reduction, modification and/or elimination of the health risks associated with chronic disease, and restoration, maintain and/or improvement of the patient's physical function and quality of life. 4. ASSESSMENTS A. CLERKSHIP GRADING – The Clerkship graded activities and NBME exam policy are under revision and will be distributed as soon as available. Item weight Faculty observation 35% Quizzes 20% Graded H&Ps 10% NBME 35% Your final grade will be based on a 100 point scale. There is no certain score you have to achieve on the NBME exam, however, performing well on it helps your chances of obtaining the highest possible grade. Students are excused from clinical duties the day before the NBME end of course exam and the day of the exam. Faculty Observations: Individual faculty assessments based on observation of each student will be combined into the final composite assessment form for each student. The final composite containing faculty comments and ratings are the basis of this component of the final grade. Particular focus will be on student’s clinical acumen while on the inpatient service. History & Physical Examination: The written H&P is due by week 5 (during the Student Education Conference on Thursday.) The H&P will be graded and returned to each student prior to the final quiz. This H&P should be formal and legibly written or typed. The H&P should be as detailed as possible particularly in the assessment and plan section. Points will be deducted if: 1) the chief complaint is omitted, 2) the assessment and plan is not appropriately detailed, including differential diagnosis, or 3) an explanation of reasoning is missing. The template to be used can be found in the Appendix. *Please remember that the mid-term review does not count toward your final grade but serves only as a tool to help gauge progress at the mid-point of the rotation. B. COM: CLERKSHIP GRADE SCALE A=100-90 (Excellent) B=89-80 (Good) C=79-70 (Adequate) D= below 70 (Remediate part of the course) F=Below 70 (After attempted remediation = repeat the course) I=Incomplete R=Review by Student Promotions Committee For Specialties Clerkship only: P (Pass) =70 and above F=Below 70 (Repeat the course). Any grade less than a C requires a deficiency grade sheet to be submitted to the COM Registrar’s office outlining the issues and remediation plan. All will be discussed at the next regularly scheduled Student Promotions Committee meeting. 14 | P a g e D = Requires review and approval of the remediation plan by the Student Promotions Committee. A “D “ grade indicates that in the judgment of the course faculty, an additional period of prescribed remediation (assuming no deficiencies in other courses), if successfully completed, will qualify a student for a grade of C*. If a grade of D is not successfully remediated in the time period allotted by the faculty and/or the Student Promotions Committee, a grade of F will be assigned. I = Incomplete, requires completion of work within 12 months or grade will automatically be changed to an F. A grade of “I” may be given in cases wherein students, for an acceptable reason, have been unable to complete all of the required work in a course. An incomplete grade must be removed within twelve months after it has occurred or it will automatically be changed to F. If the student removes the incomplete within the time period, the instructor may assign any appropriate grade according to the quality of the work completed for the entire course. R =Review by Student Promotions Committee; If for some appropriate reason a course faculty wishes to insure that the performance of a student is discussed at a Student Promotions Committee (SPC) meeting, a grade of R (review) may be assigned. Following the consideration by the SPC, the R will be changed to the appropriate grade. C. COM: NBME EXAMINATION POLICY NBME End of clerkship exams will be administered the last day of the clerkship. Specific time and location information will be provided by each clerkship. If a student is not present at the announced location and time the exam is to begin, that student will have to make special arrangements to take the exam at another time/location and will receive a grade of “I” for the rotation. No Requests for Leave will be granted for scheduled exam times. Students must bring a laptop computer with Ethernet capability and related cables for the exam. The exam cannot be taken wirelessly. No food or drinks of any type are permitted in the exam area. Books, all electronic devices, including cell phones, and other personal items, including baseball caps, are not permitted in the exam area. These items should be left at home, in lockers or cars. Examinations will be proctored by staff and/or faculty from the department responsible for administering the examination. Students will be required to sign in. ETSU ID cards are required. Students may leave the room to attend to personal needs. They may not remove any items from the exam room and may not talk with classmates while out of the room. D. COM: STUDENT COMPUTER USAGE DURING ELECTRONICALLY ADMINISTERED QUIZZES/ EXAMS POLICY This policy has been developed to address the problem of students appearing for computer administered quizzes or exams without a laptop computer that meets the specifications set forth in the QCOM Student Catalog. Every student is responsible for having a functioning laptop computer that meets these specifications. Currently, mobile devices (e.g., iPads) are not compatible with the testing environment. Any student who experiences computer problems should meet with the IT Manager (Daniel McLellan) to attempt to resolve the problem in advance of a scheduled quiz/exam. It is understood that some technical issues may not be resolved and that last minute issues may arise. If a student experiences issues immediately prior to the quiz/exam, they should bring their laptop to the quiz/exam for examination by the IT Manager. Only those students who contact the IT Manager no later than the day prior to the quiz/exam for a known problem, or who present their malfunctioning laptop the day of the quiz/exam, or who experience technical issues during the quiz/exam will be provided a laptop for the quiz/exam by the College of Medicine. Failure to adhere to this policy will result in consequences related to both the grade assigned and professionalism assessment. The student’s quiz/exam score will be reduced by 10 points and a 15 | P a g e Professionalism Report form will be submitted for any student who requests use of a College of Medicine computer but had failed to contact the IT Manager prior to the quiz/exam day or to present their malfunctioning laptop the day of the quiz/exam. 5.TIPS FOR LEARNING TOP 10 WAYS TO EXCEL ON THE INTERNAL MEDICINE CLERKSHIP 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Find out what your preceptors expect of you. Meet and try to exceed their expectations. Go the extra mile for your patients. You will benefit as much as they will. Go the extra mile for your team. Additional learning will follow. Read consistently and deeply. Include what you learn in your discussions with your team and in your notes. Follow through on every assigned task. Ask good questions. Educate your team members about what you learn whenever possible. Speak up – share your thoughts in teaching sessions, share your opinions about your patients’ care, constructively discuss observations about how to improve the education you are receiving and the systems around you. Actively reflect on your experience. The more you put in, the more you will get out. Be caring and conscientious and strive to deliver outstanding quality to your patients as you learn as much as you can from every experience. Treat every member of the health care team, the clerkship team, and every patient with respect. Answer your pager and email in a reasonable time frame. Make sure your handwriting is legible and ensure every note includes your name, role, and pager. Adapt and be professional. An open mind is expected. Be pro-active – seek out learning opportunities. Ask questions. Be flexible – each day will be different. 6. LEARNING RESOURCES A. Textbooks for Reading: all are available for loan during the clerkship and can be obtained from the office of the Clerkship Secretary Dr. Berk’s Pre-Test Medicine: Self-Assessment and Review Harrison’s Principles of Internal Step Up To Medicine Cecil’s Essentials of Medicine – 7th Edition Bates History and Physical Examination – 11th Edition B. References and Materials to read: (Optional) Balady GJ, Williams MA, Ades PA, et al. Core Components of Cardiac Rehabilitation/Secondary Prevention Programs: 2007 Update: A Scientific Statement from the American Heart Association and AACVPR. Journal of Cardiopulmonary Rehabilitation and Prevention. 2007;27:121-129. Balady GJ et al. Core components of cardiac rehabilitation/secondary prevention programs: 2007 update: Circulation. 2007;115(20):2675-2682. N.K. Wenger. Current Status of Cardiac Rehabilitation. Journal of the American College of Cardiology. 51(2008), pp. 1619–1631. 16 | P a g e Hammill BG, Curtis LH, Schulman KA, Whellan DJ. Relationship Between Cardiac Rehabilitation and Long-Term Risks of Death and Myocardial Infarction Among Elderly Medicare Beneficiaries. Circulation. 121(2010); pp 63-70. Suaya JA, Stason WB, Ades PA, et al. Cardiac Rehabilitation and Survival in Older Coronary Patients. J. Am. Coll. Cardiol. 2009;54;25-33. Geol K, Lennon RJ, Tilbury RT et al, Impact of Cardiac Rehabilitation on Mortality Following Percutaneous Coronary Intervention. Circulation. 2011;123:2344-2352. Many books are available from our COM Library portal at http://www.etsu.edu/medlib., including board review resources. Appropriate use of electronic material is governed by copyright and Intellectual Property Laws. C. COM: STUDENT PROCEDURES FOR SPECIAL SERVICES (ADA) ABSENT A LETTER FROM DISABILITY SERVICES, STUDENTS ARE NOT ELIGIBLE FOR ACCOMMODATION It is the policy of ETSU to accommodate students with disabilities, pursuant to federal law, state law and the University’s commitment to equal educational access. Any student with a disability who needs accommodations, for example arrangement for examinations or seating placement, should inform the instructor at the beginning of the course. All students seeking accommodation for disabilities are to contact Ms. Linda Gibson, M.Ed., Director, ADA Coordinator for Disability Services at East Tennessee State University (439-8346). Faculty accommodation forms are provided to students through Disability Services in the D. P. Culp center, Suite A. D. COM: TUTORING The Office of Student Affairs will make tutors available to any QCOM student. Contact Student Affairs at 439-2037. E. COM: COUNSELING Confidential academic and personal counseling are available through the Professional and Academic Resource Center – PARC (Mr. Phil Steffey, 232-0275 or pager 854-0342.) 17 | P a g e APPENDIX A IM H&P TEMPLATE APPENDIX B: BULLETED LIST OF EXPECTED BEHAVIORS FOR PRE-ENTRUSTABLE AND ENTRUSTABLE LEARNERS LINK TO COLLEGE OF MEDICINE INSTUTIONAL OBJECTIVES HTTP://WWW.ETSU.EDU/COM/MSEC/DOCUMENTS/INSTITUTIONALEDUCATIONALOBJEC TIVES_LATESTVERSION.PDF 18 | P a g e INTERNAL MEDICINE HISTORY AND PHYSICAL TEMPLATE Identifying Data Name, Date of Birth, Account number (dictation identifying information as required by site) Primary care doctor Chief Complaint: (in patient’s own words) History of Present Illness (HPI) Course Onset Duration Intensity Exacerbating factors Remitting Factors Signs and symptoms associated From whom information obtained Last meal Under the influence of drugs or alcohol Poor historian/Good historian Other pertinent info for example: If cardiovascular: risk factors- obesity, htn, hpl, family history, smoking, diabetes, male >45yo Past Medical History Childhood and Adult diseases (medical, surgical, ob-gyn, psych) Blood transfusion history (antibodies?- if known) Hospitalizations Past Surgical History Prior surgery types, complications, approximate date Current Medications Name, dosage and whether adherent, last time taken, recent adjustments or additions, include over the counter vitamins and minerals Allergies Drugs, contrast media, latex, foods (include the reaction to differentiate adverse reaction from allergy) Social/Sexual History Social: Smoking (pk-yr history), ETOH, caffeine, substance abuse, education level, occupation (current and past), marital status, children, lifestyle (activity level, eating habits), religion, type of support from family, living environment, recent changes Sexual: Sexual orientation (if applicable) menstruation information for females, ED for males? birth information, contraception, libido, symptoms/issues Special Needs Assessment Sleep assessment- sleep apnea screen (use CPAP? daytime sleepiness) Hearing aid- does patient have hearing aid or difficulty hearing- has with them? Vision- does patient wear glasses- have with them? Does patient use cane or walker prior to hospitalization? Fallen in the past year? Depression screen- SIGECAPS Pain Management- have pain normally, how controlled/ problems with requiring additional medications, any signs of abuse/dependence (loss of family support, legal issues, Dysphagia screen-Problems with choking or swallowing prior to hospitalization? Chronic Foley- last time changed Oxygen requirements- Home oxygen? Continuous? Nocturnal? Reading comprehension- literacy level, problems with reading Review of Systems (in patient terms) GENERAL/CONSTITUTIONAL: overall general health changes, fever, chills, fatigue, weakness, changes in sleep, sweats, appetite changes, weight gain or weight loss. HEAD, EYES, EARS, NOSE AND THROAT: Head- headache, trauma, migraines 1|Page Eyes –pain, redness, loss of vision, double or blurred vision, flashing lights or spots, dryness, the feeling that something is in the eye, vision correction issue. Ears, nose, mouth and throat. -Ringing in the ears, loss of hearing, nosebleeds, loss of sense of smell, dry sinuses, sinusitis, post nasal drip, sore tongue, bleeding gums, sores in the mouth, loss of sense of taste, dry mouth, dentures or removable dental work, frequent sore throats, hoarseness or constant feeling of a need to clear the throat when nothing is there, waking up with acid or bitter fluid in the mouth or throat, food sticking in throat when swallows or painful swallowing, new lumps or bumps in neck/thyroid area noted CARDIOVASCULAR: chest pain, irregular heartbeats, sudden changes in heartbeat or palpitation, shortness of breath, difficulty breathing at night, swollen legs or feet, heart murmurs, high blood pressure, cramps in his legs with walking, pain in his feet or toes at night or varicose veins. RESPIRATORY: chronic dry cough, coughing up blood, coughing up mucus (purulent? Amount?), waking at night coughing or choking, repeated pneumonias, wheezing or night sweats, occupational exposures, TB history/testing, pain with deep breath, shortness of breath, fast breathing. GASTROINTESTINAL: decreased appetite, nausea, vomiting, vomiting blood or coffee ground material, heartburn, regurgitation, frequent belching, stomach pain relieved by food, yellow skin, generalized itching, diarrhea, constipation, gas, blood in the stools, black tarry stools or hemorrhoids, colonoscopy and results GENITOURINARY: difficult urination, pain or burning with urination, blood in the urine, cloudy or smoky urine, frequent need to urinate, urgency, needing to urinate frequently at night, inability to hold the urine, discharge from the penis, kidney stones, rash or ulcers, sexual difficulties, impotence or prostate trouble, exposure to sexually transmitted diseases, abnormal PAP smears, changes in menstruation or bleeding, discharge, pain with intercourse MUSCULOSKELETAL: arm, buttock, thigh or calf cramps, joint or muscle pain. Muscle weakness or tenderness. Joint swelling, neck pain, back pain or major orthopedic injuries, limited movement in any joints SKIN AND BREASTS: easy bruising, skin redness, skin rash, hives, sensitivity to sun exposure, tightness, nodules or bumps, hair loss, color changes in the hands or feet with cold, breast lump, breast pain or nipple discharge. NEUROLOGIC: headache changes, dizziness, fainting, lightheadedness, muscle spasm, loss of consciousness, sensitivity, tingling or pain in the hands and feet or memory loss, seizures, shaking/tremor, problems with speech. PSYCHIATRIC: depression, thoughts of suicide? nervousness, panic attacks, attention problems, hallucinations (visual or auditory), delusions, substance abuse, not sleeping for >3 days, and if so reason, changes in personality, previous treatment for psychiatric issues ENDOCRINE: intolerance to hot or cold temperature, flushing, fingernail changes, increased thirst, increased urination, increased salt intake or decreased sexual desire. HEMATOLOGIC/LYMPHATIC: anemia, pallor, bleeding tendency or clotting tendency, lumps or bumps neck, armpits or groin area Physical Examination General Appearance Development Nourishment Body habitus Deformities Attention to grooming Comprehension and language skills (also noted in history) Vital signs Temperature, height and weight (if question repeat) Respiration Pulse – regular, irregular or irregularly irregular (as in atrial fibrillation – A fib) Blood pressure (BP) – both arms - check for orthostatic hypotension by taking blood pressure with patient sitting - (if orthostatic hypotension considered-obtain BP lying, sitting, standing and in legs (if coarc aorta considered) HEENT Head Shape, scars and size Eyes External eye structures-Visual acuity – use pocket-sized visual cards, color chart Extra ocular movements (EOM) and convergence Pupillary light reflex (direct and consensual) and accommodation Visual fields by confrontation Ophthalmoscopy Ears External canals-Gross hearing (rub fingers together next to ears) Weber test – place tuning fork in middle of forehead Rinne test – place tuning fork behind ear on mastoid process Otoscopy – look 2|Page at tympanic membrane Nose External nares (polyps, condition of mucosa), turbinates, septum (deviation from the Center – from fracture) Sinuses (tap them for tenderness, particularly over the maxillary sinus) Throat Lips (pale – anemia, cold sore – viral infection) Buccal mucosa (pale – anemia) Gingiva (gums) – bleeding, hypertrophy (thick and swollen due to taking Dilantin) Teeth – presence, state of repair, dentures Hard and soft palates – clefts, masses Tonsils – (red, swollen with exudates – tonsillitis) Floor of mouth – (ranula – stone in duct of sub maxillary gland) Gag reflex Neck Scars, masses Anterior and posterior cervical nodes Carotid artery pulse (also, auscultate for a bruit first) Observe jugular vein for distention (increased jugular venous pressure – JVP) Check for tracheal position in midline and for free movement of trachea Palpate thyroid gland for enlargement and nodules Chest Anterior Inspect sternum (marked central depression of sternum – pectus excavatum, pigeon breast – pectus carinatum) Inspect ribs (point tenderness – fracture of rib) Inspect for scars and for symmetrical movement of chest wall with breathing Palpate for symmetrical movement of chest wall on breathing and for tactile fremitus Percussion for resonance, dullness, flatness, tympany Auscultation for breath sounds Posterior Inspect for scars, contour, symmetrical motion on breathing, shape and appearance Palpate for symmetrical motion on breathing and for tactile fremitus Percussion for resonance, dullness, flatness, tympany and for movement of diaphragm on both sides Auscultation – breath sounds, rales (crepitations), egophony, bronchophony, whispered pectoriloquy and rubs Breasts Inspect and palpate Dimpling of skin (peau d’orange – cancer) Tenderness – infection All quadrants and tail process of Spence Axillary nodes, areolae -Discharge (galactorrhea, blood and pus) Chest wall pain – very tender costchondral junctions (Tsetse’s Syndrome) Heart Sitting and lying down (examine all 4 areas – mitral, tricuspid, pulmonary, and aortic) Inspect – scars (midsternal scar – CABG), pulsations Palpate – Point of maximal impulse (PMI), heaves, thrills, lifts Auscultate - heart sounds, rubs, gallops (S3 and S4) and murmurs Location refers to where the heart murmur is usually auscultated best. There are four places on the anterior chest wall to listen for heart murmurs; each of the locations roughly corresponds to a specific part of the heart and should be auscultated with the patient lying supine. The four locations are: • Aortic region - the 2nd right intercostal space. • Pulmonic region - the 2nd left intercostal spaces. • Tricuspid region - the 5th left intercostal space. • Mitral region - the 5th left mid-clavicular intercostal space. Additional maneuvers can be performed for additional auscultation: • Left lateral decubitus. With the patient sitting upright, with the patient leaning forward and exhaling. Radiation refers to where the sound of the murmur radiates. The general rule of thumb is that the sound radiates in the direction of the blood flow. Intensity refers to the loudness of the murmur, and is graded according to the Levine scale, from 1 to 6 1. The murmur is only audible on listening carefully for some time. 2. The murmur is faint but immediately audible on placing the stethoscope on the chest. 3. A loud murmur readily audible but with no palpable thrill. 4. A loud murmur with a palpable thrill. 5. A loud murmur with a palpable thrill. The murmur is so loud that it is audible with only the rim of the stethoscope touching the chest. 6. A loud murmur with a palpable thrill. The murmur is audible with the stethoscope not touching the chest but lifted just off it. Pitch may be low, medium or high and is determined by whether it can be auscultated best with the bell or diaphragm of a stethoscope. Quality refers to unusual characteristics of a murmur, such as blowing, harsh, rumbling or musical. A mnemonic to remember what characteristics to look for when listening to murmurs is SCRIPT: Site, Configuration (shape), 3|Page Radiation, Intensity, Pitch and quality, and Timing in the cardiac cycle. The use of two simple mnemonics may help differentiate systolic and diastolic murmurs; PASS and PAID. Pulmonary and aortic stenoses are systolic while pulmonary and aortic insufficiencies (regurgitation) are diastolic. Mitral and tricuspid defects are opposite. Abdomen-Lying flat Inspect – scars, masses, contour, venous pattern Auscultate – bowel sounds, bruits Percussion – all four quadrants – if pain elicited in any quadrant be gentle on palpation so as not to have the patient suffer unnecessary pain Palpate and percussion (a) Superficial and deep palpation (all 4 quadrants) (b) Liver and Spleen for consistency and size (c) Hepato-jugular reflex (d) Shifting dullness (e) Fluid wave (f) Masses and hernias – include inguinal area Rectal exam-sphincter tone, rashes, hemorrhoids? obvious bleeding amount, or occult blood testing results Genitourinary Peripheral vascular Palpate Carotid pulse – also auscultate for a bruit first Radial pulse Femoral pulse – also auscultate for bruit Popliteal pulse Dorsalis pedis (DP) pulse Posterior tibial (PT) pulse Musculoskeletal Inspect and palpate Bones, joints and spine CVA tenderness Sacroiliac tenderness Sacral edema -Muscle atrophy, muscle strength Tenderness, warmth, swelling and redness of joints, as well as for stability and also for whether a joint effusion is present Range of motion (ROM) of joints (perform only if there is a joint problem) – elbows – wrists – fingers Chest – spine (thoracic and lumbar) kyphosis, scoliosis Hips – knees – ankles Neurologic Mental status Level of consciousness Orientation to time (date), place (where are you?), and person (your name) Memory - remember 3 words (recent memory), well-known past event (remote memory) Insight and judgment – reaction to a simple problem Affect – emotional response to an event Intellectual ability – series of 7s (100 – 7) Speech, language and comprehension (a) Aphasia – acquired disturbance of language 1. Motor – expressive 2. Sensory – receptive (b) Dysarthria – disturbance of speech due to problems with articulation of sounds (MMSE) or SLUMS exam – used in geriatric patients Cranial nerves I – not tested II – visual acuity, visual fields by confrontation (already done under Eyes) III, IV and VI – extra-ocular movements (EOM), light reflex (direct and consensual), nystagmus (already done under Eyes) V – sensory and motor of face (a) Sensory – test ophthalmic, maxillary and mandibular divisions (b) Motor – ask patient to bite down hard – feel contraction of masseter muscles VII – smile, ask patient to close eyes tightly and don’t let you open them, wrinkle Forehead (bilaterally innervated) VIII – hearing, Weber and Rinne tests (already done under Ears) IX – X – gag reflex (already done under Throat) XI – shrug shoulders – palpate both trapezii muscles and feel contraction, push chin against Examiner’s fingers of one hand and examiner feels contraction of sternocleidomastoid Muscles with his other hand XII – stick out tongue – it should be in midline; if to either side, it points to the side of the l Lesion (already done under Throat) Motor system Test muscle strength and resistance to passive motion (part of Musculoskeletal Examination, but fits in here much better) Reflexes – biceps, triceps, brachioradialis, knee jerk (KJ), ankle jerk (AJ) Babinski reflex Inspect for (a) Tremor - involuntary shaking (b) Fasciculations - irregular, involuntary muscle twitching (c) Spasticity – involuntary increased muscle tone with progressive stretching of muscle (d) Rigidity – involuntary increased muscle tone throughout range of motion of muscle (e) Atrophy - loss of muscle mass (f) Flaccidity – floppiness of muscle (g) Chorea – involuntary twisting and writhing motion (h) Myoclonus – involuntary shock-like motion of muscles with extreme twisting of joints (i) Dystonia–involuntary, persistent, fixed contraction of muscle 4|Page Sensory system Pain and temperature (use sharp side of pin) Light touch (use dull side of pin) (NB – pain and light touch are performed together on hands and lower forearm as well as on feet and lower leg) Two-point discrimination Position sense and vibration (testing posterior or dorsal column) – hold lateral aspects of both great toes and both thumbs and move up and down – ask patient to close eyes and identify movement as up or down Romberg test – stand with feet together, arms stretched forward, eyes open and have patient close eyes (be careful to be ready to catch patient if patient begins to fall) – if patient losses balance or sways with eyes open, cerebellar disease is probably present; if this occurs with eyes closed, but not when eyes are open, then position sense is impaired Cerebellum Finger to nose test - eyes open (if eyes closed, testing position sense) Heel to knee (shin) – eyes open (if eyes closed, testing position sense) Alternating movements Gait Posture-Walking – normally, on toes, on heels and in tandem Assessment and Plan The assessment starts with a summary statement. In the summary statement, put foreground issues first (i.e. presenting complaint and important findings from your history, physical, and data sections) and then state the background issues (age, pertinent past medical history). The assessment should include a discussion of the differential diagnosis and your clinical reasoning. Divide your differential diagnosis into categories of “likely”, “less likely”, “less likely but immediately life-threatening”, and “unlikely” diagnoses. . List the most likely diagnoses first. As you weigh your differential diagnosis, you should support your reasoning with findings from your history, physical, and work-up, and information you gathered from your reading. The assessment is a discussion of your patient, NOT a reiteration of your reading. This is your opportunity to show how you are thinking about a case. References should be used for every patient and noted at the end of your write-up. All problem lists in the History and Physical should be problem-based, not organ system-based, In some cases, the problem will be a symptom (abdominal pain); in other cases, when a diagnosis is established by the data you have already collected, it will be a diagnosis (pancreatitis). For example, the headers for your discussion in the problem list would be: 1. Pancreatitis or Abdominal Pain not Gastrointestinal- abdominal pain Or 1. Pneumonia not Respiratory/Pulmonary- shortness of breath or pneumonia The goal is as you progress through the hospitalization you will be able to further reason out the possible differential diagnosis listed initially in your assessment and develop a firm diagnosis by discharge. Each day you can discuss what aspects of the initial assessment are no longer valid and continue to refine Each medication should have a problem associated with it. If it is stable and not going to impact the hospitalization, it does not need to be carried through as a problem on daily SOAP notes. These should include only the active problems being treated. A plan/intervention should be developed under each problem listed. If it is stable and no intervention required, document this information Code Status includes any discussion information and who was present for decision, living will? Prophylaxis- DVT and GI (if not needed for either document reason) Disposition- planned disposition of patient at time of discharge Immunization Status: up to date on immunizations? 5|Page