Population Science Strategy: Towards a Creative Transformation of
advertisement
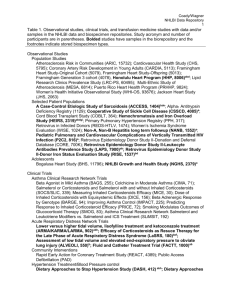
Final 11/12/13 Population Science Strategy: Towards a Creative Transformation of Epidemiology 2013 Council/BEE Working Group Charge Within the context of budgetary constraints, the overarching goal of the NHLBI Council/BEE Working Group on Epidemiology and Population Science is to define how Epidemiology and Population Science research can be optimized by taking advantage of new tools/methods. In order to meet this goal, the Working group will strive to address the following questions: 1) What should be the NHLBI’s long-term strategy for population science? a. What scientific questions should be the primary focus, with the goal of improving the health of the population and addressing contemporary disease burden? b. What types of project domains and methods best enable us to address the primary scientific questions of interest? i. Propose a conceptual framework for the domains of epidemiology, such as population vs. clinical; mega-scale vs. standard-scale; outcomes/health services vs. etiological/discovery ii. Propose possible approaches to balance the NHLBI’s support across domains 2) How should the NHLBI take advantage of new opportunities for epidemiology to address the key scientific questions, and what should the balance be between developing new opportunities and supporting well-established population science? a. What gaps exist in NHLBI’s current portfolio of population science need to be filled in order to meet the needs outlined above? b. What should the balance be between supporting a large portfolio of investigatorinitiated grants or link onto or expand other existing infrastructures? c. How should NHLBI increase its links with other ICs/agencies? d. How should training of scientists be incorporated into the NHLBI’s current and future portfolio of population sciences? e. What approaches should be used to leverage new data sources such as electronic health records (EHRs), existing registries, and other data sources to capture outcomes and risk factors/predictors? How should the NHLBI support research to evaluate the quality of information obtained from these new data sources and track this over time? For which of the primary scientific questions of interest are these approaches best suited? 3) What question or research priorities can be advanced by better integrating clinical epidemiology and clinical trials? a. What are the best practical approaches for integrating clinical trials with clinical epidemiology within the context of the US health care system? b. What methodological constructs can be learned from experiences in other countries (e.g. Scandinavia) and from other funding agencies (e.g. AHRQ DeCIDE, NIH Collaboratory, FDA Mini-Sentinel)? What are the gaps that need to be addressed? Which of these constructs are transferable to the US health care system and NHLBI? c. Under what circumstances does this integration improve efficiency? d. How should the NHLBI proceed with this, and if so, how can it promote the streamlining of efficient clinical trials conduct? e. What proportion of the resources should be directed in this way? Final 11/12/13 4) How should the NHLBI quantify the success of individual projects in epidemiology and population science? a. How should we measure the success of new projects or approaches? b. What is the appropriate comparator group? 5) Provide recommendations to the NHLBI director about what to do with the existing NHLBI-contract funded cohort studies to improve their ability to address the scientific questions of primary interest. a. How should the NHLBI rebalance its population-studies portfolio in terms of % contracted-funded cohort studies compared with investigator-initiated research or new initiatives? b. To what extent should the cohorts continue to exist independently, as compared with becoming consolidated as part of a synthetic whole? If the cohorts should mostly exist as a synthetic whole: i. What should the objectives be of such a synthetic cohort? ii. What are the key scientific hypotheses that can be addressed? iii. What kind of scientific governance is most appropriate? c. What should be the balance between the cohorts continuing to collect new data versus curate existing data? If new data collections are done: i. How should optimal timing and intensity be determined? ii. Should, and if so how, can novel data collections (e.g., mobile phones, electronic health records, and other technologies) be incorporated and evaluated?